Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9990
Peer-review started: June 26, 2021
First decision: July 14, 2021
Revised: July 16, 2021
Accepted: July 29, 2021
Article in press: July 29, 2021
Published online: November 16, 2021
Processing time: 136 Days and 12.5 Hours
Abdominal lymphangiomatosis is a rare benign condition accounting for less than 1% of all the cases of lymphangiomatosis. Management usually involves radical surgical excision; however, depending upon the extent of involvement, patient condition, and absence of complications, conservative management can be also considered.
We present the case of a 32-year-old male who presented with short onset abdominal pain and melena. Physical examination findings were within normal limits, except for left lower abdominal tenderness. Upper gastrointestinal endoscopy was within normal limits. Abdominal and pelvic ultrasound and computed tomography (CT) scan revealed numerous, variably-sized cystic lesions within the abdominal cavity, exclusively and extensively affecting the small bowel mesentery with sparing of the retroperitoneum. The diagnosis was confirmed by CT and cytological examination. Radical surgical excision was technically impossible in this patient because of the extensive involvement of the mesentery; therefore, the patient was managed conservatively.
Extensive and exclusive small bowel mesentery involvement in abdominal lymphangiomatosis is rare. Imaging modalities play an important role in establishing the diagnosis and conservative management can be considered when surgery is technically impossible.
Core Tip: Abdominal lymphangiomatosis is rare, accounting for less than 1% of all cases of lymphangiomatosis. The retroperitoneum is the typical site affected in abdominal lymphangiomatosis. Other than the retroperitoneum, the mesentery and omentum can also be affected. Here, we report a case of extensive mesenteric lymphangiomatosis without retroperitoneal involvement. Surgical excision was technically impossible in our case due to the extensive and exclusive involvement of the small bowel mesentery and the patient was managed conservatively.
- Citation: Alhasan AS, Daqqaq TS. Extensive abdominal lymphangiomatosis involving the small bowel mesentery: A case report. World J Clin Cases 2021; 9(32): 9990-9996
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9990.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9990
Lymphangiomatosis is a rare benign condition that affects the lymphatic system[1,2]. Usually, younger children are affected by this condition; however, in rare cases, adults can also be diagnosed with lymphangiomatosis. The exact etiology of lymphangiomatosis has not been fully established; however, since children are more commonly affected, it is postulated that lymphangiomatosis could be a congenital disease[3]. In some cases, certain secondary underlying conditions, such as a history of abdominal trauma, surgery, radiation, or underlying obstruction of the lymphatic ducts owing to inflammation or infection, can precipitate lymphangiomatosis[4]. Lymphangiomatosis can occur anywhere in the body except for the brain, as it lacks the lymphatic system[5]. Approximately 95% of lesions occur in the neck and axillary regions, whereas the remaining 5% can arise elsewhere[6]. Herein, we report a rare case of extensive cystic lymphangiomatosis exclusively involving the small bowel mesentery without involvement of the retroperitoneum in a 32-year-old male. We also highlight the importance of imaging modalities and present a review of literature on this entity.
A male patient aged 32 years presented with mild dull diffuse abdominal pain and two episodes of melena.
The symptoms started 1 wk prior to presentation, with recurrent abdominal pain and two episodes of melena.
The patient had no significant prior medical or surgical history.
The patient had no family history that was related to the present illness.
General examination findings were within normal limits. Vital signs were also normal. Abdominal examination revealed mild to moderate abdominal distension with mild left lower quadrant tenderness.
Complete blood count and coagulation profile were within normal limits. The serum creatinine level was 0.91 mg/dL, liver and cholestasis parameters were unremarkable, and albumin level was 4.1 g/dL.
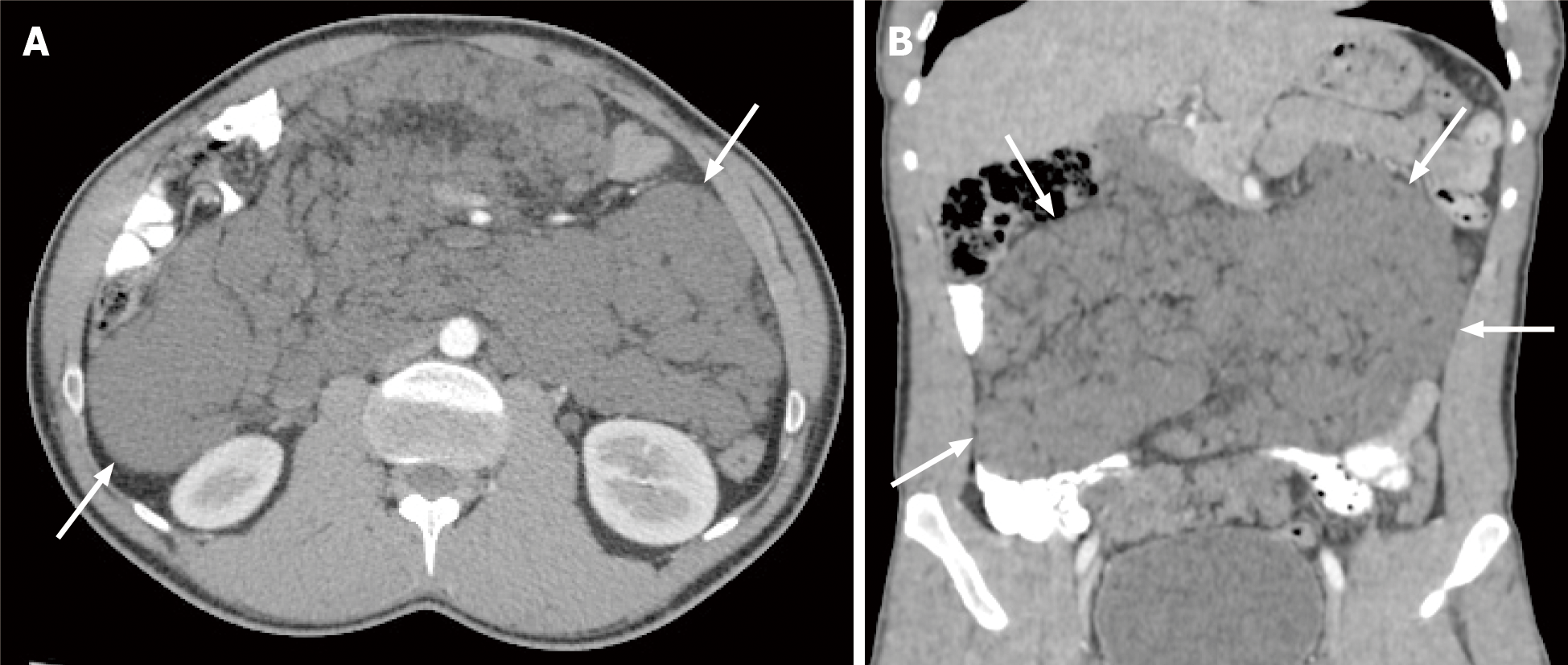
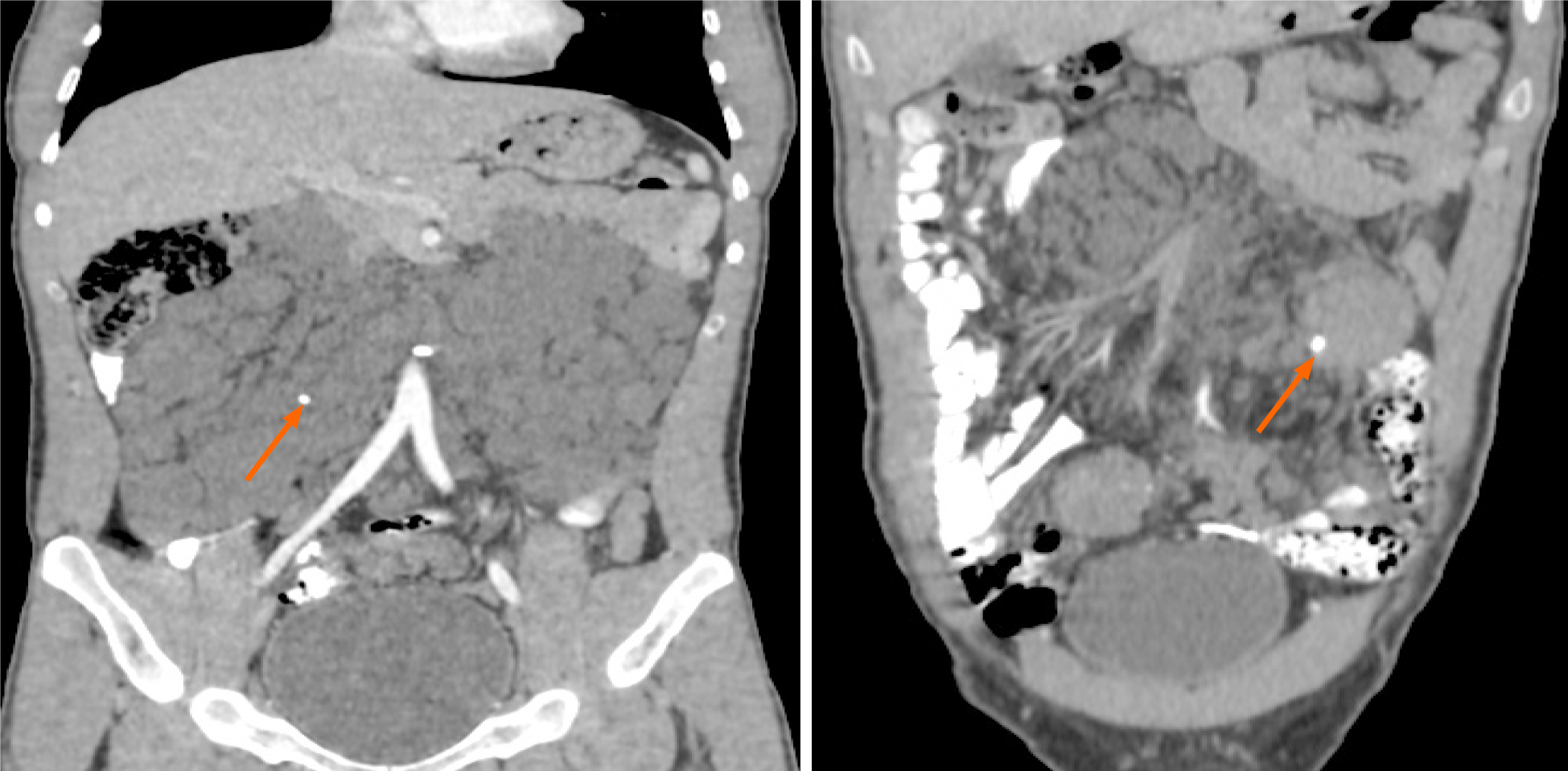
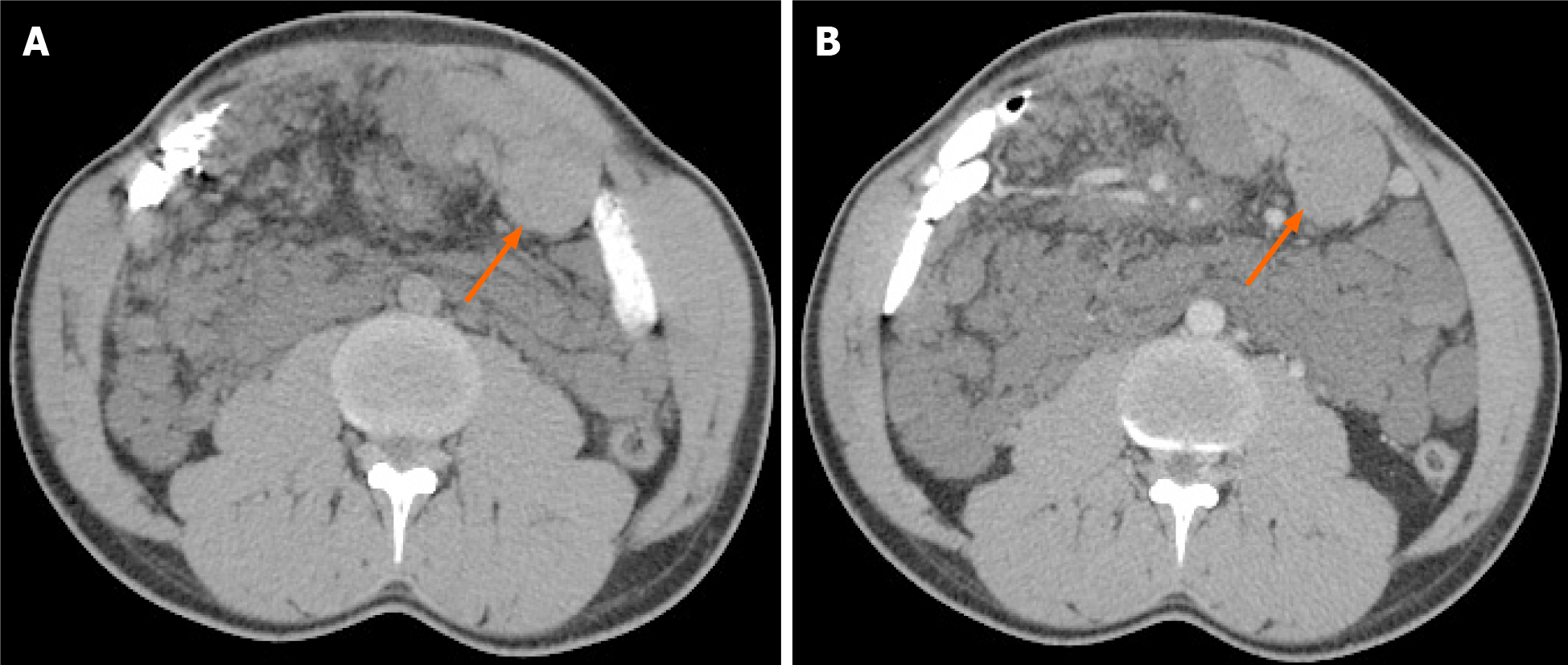
Abdominal radiography did not show air-fluid levels or free air. Abdominal ultrasound reported the presence of multiple anechoic cystic lesions within the abdominal cavity. Some of the cystic lesions at the left lower quadrant showed low level internal echoes. An abdominal computed tomography (CT) scan revealed numerous confluent cystic lesions of variable size showing fluid density 0-10 Hounsfield units (HU) with no enhancing walls (Figure 1). The lesions were extensive, involving the small bowel mesentery and encasing the mesenteric vessels. The largest lesions were seen peripherally, while the smaller lesions were more central in location. The largest lesion measured approximately 4.6 cm at its longest axis. No enhancement was seen within these lesions on post-contrast CT images. The jejunal loops were displaced superiorly and to the left side, while the ileal loops were displaced inferiorly and towards the right side. Despite the mass effect on the small bowel loops, there were no signs of intestinal or colonic obstruction. A few small, round calcifications were present within these lesions (Figure 2). No cystic lesions were seen within the mesocolon, retroperitoneum, gastro-hepatic, peri-gastric, or peri-splenic spaces. No lung, mediastinal, liver, kidney or bone lesions were seen. At the left lower quadrant of the abdomen, some of the lesions showed intra-cystic hemorrhage with a spontaneous density of 53 HU. (Figure 3).
Upper gastrointestinal (GI) endoscopy was performed and revealed no significant abnormality. Ultrasound-guided fine needle aspiration obtained from one of the large cystic lesions was performed with no subsequent adverse events. Gross examination showed clear fluid. Cytology revealed few mature lymphocytes and was negative for chyle. The culture was also negative. Flow cytometry showed few B and T lym
The final diagnosis of the present case was extensive and exclusive mesenteric cystic lymphangiomatosis.
The patient received symptomatic treatment with 1 g of oral paracetamol three times per day for 1 wk. Radical surgical excision was technically impossible in our case due to the extensive involvement of the small bowel mesentery.
The patient reported no pain after 1 wk of using oral paracetamol three times per day and was asymptomatic during short-term follow-up.
Lymphangiomatosis is a rare benign disease characterized by proliferative lymphatic malformations. The lesions are composed of spaces lined with endothelium and encompassed connective tissue stroma composed of lymphatic tissue, smooth muscle, and round cells[1]. In most cases, the disease is diagnosed during the initial 2 years of life and the disease is rarely diagnosed after reaching adulthood[1,3]. The disease is not familial and does not depend on patient gender[2]. Abdominal lymphangiomatosis is very rare, representing less than 1% of all lymphangiomatosis cases. The retroperitoneum is the typical site affected in abdominal lymphangiomatosis. Other than the retroperitoneum, the mesentery and omentum can also be affected[7]. In our case, the patient had extensive involvement of the small bowel mesentery with no involvement of the retroperitoneum.
There are no specific signs or symptoms for abdominal lymphangiomatosis. Also, there are no specific laboratory diagnostic tests to confirm the disease. Although nonspecific palpable abdominal mass, pain, or abdominal distensions could be presenting features, different patients might present with different sets of symptoms and signs. In most cases, the lesions are usually fluid-filled sacs, and incidental diagnosis is made after imaging study of the abdomen, such as ultrasound or CT. Some of the patients might present with acute abdomen, GI bleeding in the form of melena or hematemesis, intestinal obstruction, or even bowel perforation in severe cases[8,9]. Rarely, life-threatening complications might arise, such as rupture, torsion of the cyst, volvulus, or severe GI bleeding leading to shock[9].
Literature search revealed only a few cases of abdominal lymphangiomatosis in adult patients presenting with GI bleeding[1,10,11]. Our case described a male patient aged 32 years, without any significant prior medical or surgical history, with complaints of mild, dull, diffuse abdominal pain, and two episodes of melena for 1 wk. An existing hypothesis suggests that trauma can precipitate GI bleeding, due to hemorrhage in these cystic lymphatic lesions. The bleeding in these cystic lymphatic lesions can results in the development of an abnormal venolymphatic communication or hemangioma within the lesion[7,12].
Radiological investigations play an important role in the diagnosis of abdominal lymphangiomatosis. Although plain abdominal X-ray cannot diagnose abdominal lymphangiomatosis, it can be useful in the diagnosis of complications, such as intestinal obstruction or displacement of bowel loops owing to the mass effect of the cystic lesions. Ultrasonography typically demonstrates purely anechoic cystic lesions or lesions with low level internal echoes if complicated by internal bleeding or infection. CT can provide additional details, such as size, specific anatomical location, extent of organs affected, and presence or absence of complications (i.e. hemorrhage or infection), and allows differentiation from other pathologies, such as complicated ascites. CT scans usually reveal uni- or multi-locular low density cysts with no perceptible wall, as in our case. The lesions usually contain fluid or chyle with a density ranging from −10 HU to 0 HU. If internal bleeding occurs, density might increase, as demonstrated in our case. In some rare cases, calcification might also be present, as also shown in our case[13]. Magnetic resonance imaging is another important diagnostic tool. Cystic lesions typically have low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging. Cysts containing high chyle might present with high signal intensity on T1-weighted images and moderate signal intensity on T2 weighted images[14].
Although typical radiological findings, in combination with cytological examination might be sufficient to establish a diagnosis, histopathological and/or immunohistochemical examinations could be helpful. The cell lining of the cystic lesions in abdominal lymphangiomatosis are immunologically reactive to cytokeratin and does not show positive reaction for factor VIII. The most reliable method of demonstrating the endothelium in lymphangiomatosis is positive staining with CD31 and Prox1[7,15].
Radical excision of the abdominal cystic lesions is considered an ideal treatment option by some authors, even if diagnosed incidentally in asymptomatic patients due to the risk of complications, such as intestinal obstructions[9]. In this case, radical surgical excision was technically impossible due to the extensive involvement of the mesentery. Regarding radical excision of the cystic lesions, some authors, such as Kochman et al[16], have reported that radical surgical excision should be avoided, especially in asymptomatic patients without any complications. Other authors have suggested other treatment options, such as marsupialization, percutaneous drainage of the cystic lesions, intra-cystic injection of biological response modifiers and sclerotherapy agents[17,18].
Abdominal lymphangiomatosis is quite rare and the evidence regarding the ideal choice of treatment is meager. The treatment options should take in consideration individual patient status, such as symptoms, number, size and location of the lesions, presence of complications, and risk of future complications. Our patient was managed symptomatically, as radical surgical excision was not feasible because of extensive involvement of the mesentery. In addition, there were no signs of intestinal obstruction or other complications. The patient reported a good response to self-prescribed oral paracetamol to control the pain. Paracetamol has been traditionally considered a safer alternative to non-steroidal anti-inflammatory drugs. As a result, the treating physician advised the patient to continue with the recommended dose of paracetamol for 1 wk. The patient did not receive any other treatment. The patient’s melena and abdominal pain subsided eventually, and no further treatment was offered as the patient became asymptomatic. Among the few cases of abdominal lymphangiomatosis reported in the literature, abdominal pain, anemia, protein-losing enteropathy, and GI bleeding were the most common presenting symptoms. However, one patient presented with symptoms of intestinal (ileal) perforation. Chan et al[12] presented a case of lymphangiomatosis involving both the mesentery and retroperitoneum in a male patient aged 51 years with melena, whom they managed conservatively. Surgical laparotomy was subsequently performed to obtain tissue for histopathologic examination.
In conclusion, extensive and exclusive small bowel mesentery involvement in abdominal lymphangiomatosis is rare. Imaging modalities, especially CT scans, play an important role in the diagnosis. Conservative management can be considered when surgery is technically impossible.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Medicine, research and experimental
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang XJ, Yi XL S-Editor: Yan JP L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Lin RY, Zou H, Chen TZ, Wu W, Wang JH, Chen XL, Han QX. Abdominal lymphangiomatosis in a 38-year-old female: case report and literature review. World J Gastroenterol. 2014;20:8320-8324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Alqahtani A, Nguyen LT, Flageole H, Shaw K, Laberge JM. 25 years' experience with lymphangiomas in children. J Pediatr Surg. 1999;34:1164-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 233] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Hanagiri T, Baba M, Shimabukuro T, Hashimoto M, Takemoto H, Inoue A, Sugitani A, Shirakusa T. Lymphangioma in the small intestine: report of a case and review of the Japanese literature. Surg Today. 1992;22:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Suthiwartnarueput W, Kiatipunsodsai S, Kwankua A, Chaumrattanakul U. Lymphangioma of the small bowel mesentery: a case report and review of the literature. World J Gastroenterol. 2012;18:6328-6332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 52] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Stopinski J, Stephan S, Staib I. [Intra-abdominal cystic lymphangioma and mesenteric cysts as a cause of abdominal discomfort]. Langenbecks Arch Chir. 1994;379:182-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Roisman I, Manny J, Fields S, Shiloni E. Intra-abdominal lymphangioma. Br J Surg. 1989;76:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 121] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Aprea G, Guida F, Canfora A, Ferronetti A, Giugliano A, Ciciriello MB, Savanelli A, Amato B. Mesenteric cystic lymphangioma in adult: a case series and review of the literature. BMC Surg. 2013;13:A4. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Giuliani A, Romano L, Coletti G, Walid A Fatayer M, Calvisi G, Maffione F, Muolo C, Vicentini V, Schietroma M, Carlei F. Lymphangiomatosis of the ileum with perforation: A case report and review of the literature. Ann Med Surg (Lond). 2019;41:6-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Jang JH, Lee SL, Ku YM, An CH, Chang ED. Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean J Radiol. 2009;10:319-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Amadori G, Micciolo R, Poletti A. A case of intra-abdominal multiple lymphangiomas in an adult in whom the immunological evaluation supported the diagnosis. Eur J Gastroenterol Hepatol. 1999;11:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Takami A, Nakao S, Sugimori N, Ishida F, Yamazaki M, Nakatsumi Y, Saito M, Otake S, Nakamura S, Matsuda T. Management of disseminated intra-abdominal lymphangiomatosis with protein-losing enteropathy and intestinal bleeding. South Med J. 1995;88:1156-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Chan WYS, Kwan KEL, Teo LT. A rare case of retroperitoneal and mesenteric lymphangiomatosis. Radiol Case Rep. 2020;15:11-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Cutillo DP, Swayne LC, Cucco J, Dougan H. CT and MR imaging in cystic abdominal lymphangiomatosis. J Comput Assist Tomogr. 1989;13:534-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Rajiah P, Sinha R, Cuevas C, Dubinsky TJ, Bush WH Jr, Kolokythas O. Imaging of uncommon retroperitoneal masses. Radiographics. 2011;31:949-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 171] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 15. | Hornick JL, Fletcher CD. Intraabdominal cystic lymphangiomas obscured by marked superimposed reactive changes: clinicopathological analysis of a series. Hum Pathol. 2005;36:426-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Kochman ML, Wiersema MJ, Hawes RH, Canal D, Wiersema L. Preoperative diagnosis of cystic lymphangioma of the colon by endoscopic ultrasound. Gastrointest Endosc. 1997;45:204-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Grunewald TGP, Damke L, Maschan M, Petrova U, Surianinova O, Esipenko A, Konovalov D, Behrends U, Schiessl J, Wörtler K, Burdach S, von Luettichau I. First report of effective and feasible treatment of multifocal lymphangiomatosis (Gorham-Stout) with bevacizumab in a child. Ann Oncol. 2010;21:1733-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Rostom AY. Treatment of thoracic lymphangiomatosis. Arch Dis Child. 2000;83:138-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |