Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9935
Peer-review started: July 19, 2021
First decision: August 19, 2021
Revised: August 28, 2021
Accepted: September 8, 2021
Article in press: September 8, 2021
Published online: November 16, 2021
Processing time: 113 Days and 16.3 Hours
Foreign body aspiration mainly occurs in children, which can cause a severe concurrent syndrome and even death without timely treatment. As a rare foreign body, aspiration of lime is seldom reported, and most cases involve a small amount of hydrated lime. Although the symptoms are usually severe, the prognosis is good after suitable treatment. Experience of treatment for lime aspiration is lacking, and this report provides novel evidence for treatment of mass burnt lime aspiration using bronchoscopy.
We report an adult with a large amount of burnt lime aspiration. Because of delay in clearance of the inhaled lime in the trachea and bronchus at the local hospital, he suffered several severe complications, including complete occlusion of the right primary bronchus, aeropleura, aerodermectasia, pneumomediastinum, secondary infection and hypoxemia at 4 d after injury. After transferring to our department, bronchoscopy was immediately carried out to clear the lime in the major airway, using foreign body forceps, biopsy forceps, puncture needle, and hairbrush. The patient’s condition recovered rapidly and at 3-months’ follow-up, he demonstrated good recovery of the bronchus and lung parenchyma.
After mass lime aspiration, flexible fiberoptic bronchoscopy is suggested as early as possible, using clamping, flushing or cryotherapy.
Core Tip: Aspiration of lime is seldom reported, especially in adults, and most cases involve small amounts of hydrated lime. We report an adult with a large amount of burnt lime aspiration. Because of delay in clearance of the inhaled lime in the airway, he suffered severe complications. Bronchoscopy was immediately carried out to clear the lime by mechanical methods such as clamping, washing and freezing. The treatment target was to release airway obstruction. After removal of most of the lime, the condition improved rapidly, and follow-up showed good recovery.
- Citation: Li XY, Hou HJ, Dai B, Tan W, Zhao HW. Adult with mass burnt lime aspiration: A case report and literature review. World J Clin Cases 2021; 9(32): 9935-9941
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9935.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9935
Foreign body aspiration mainly occurs in children, and can cause a severe concurrent syndrome and even death without timely treatment. As a rare foreign body, aspiration of lime is seldom reported, and most cases involve a small amount of hydrated lime. Although the symptoms are usually severe, the prognosis is good after suitable treatment. We report an adult with a large amount of burnt lime aspiration. Because of delayed clearance of the inhaled lime in the trachea and bronchus at the local hospital, he suffered several severe complications, including complete occlusion of the right primary bronchus, aeropleura, aerodermectasia, pneumomediastinum, secondary infection and hypoxemia at 4 d after injury. After transferring to our department, bronchoscopy was immediately carried out to clear the lime by mechanical methods such as clamping, washing and freezing. After removal of most of the lime in the airway, the condition improved rapidly, and follow-up showed good recovery. There is a lack of experience of treatment for lime aspiration. To our knowledge, searches of databases, including PubMed, Wanfang and China National Knowledge Infrastructure (CNKI), have only revealed six reports including eight cases (seven adolescents and one adult) who suffered lime aspiration, and most of them inhaled hydrated lime. Bronchoscopy is suggested as early as possible after mass lime aspiration, and the treatment target is mainly to clear the airway. Moreover, electroexcision or laser dissection should be avoided to clean the lime. Instead, we suggest combining several mechanical methods, such as clamping, flushing and cryotherapy. The prognosis is usually good when treatment is timely.
A 24-year-old man was transferred to our department with the complaint of dyspnea for 5 d after burnt lime aspiration after an accidental high fall.
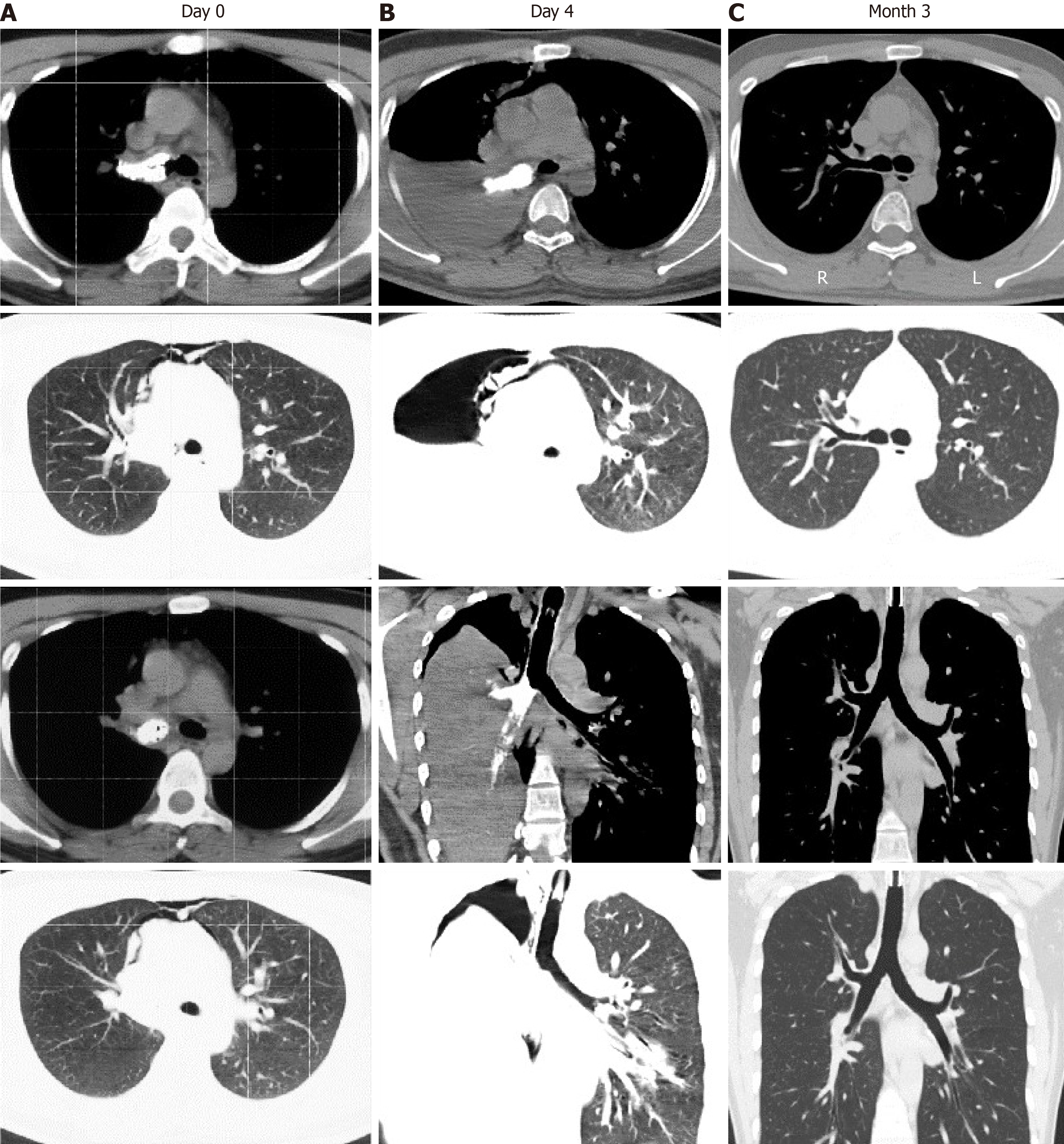
The patient fell head down 5 d before admission from a height of 2 m into a truck of burnt lime and inhaled a large amount. He had severe dyspnea and was immediately admitted to a local hospital. Computed tomography (CT) showed a high-intensity mass in the right principle bronchus, and pneumomediastinum (Figure 1). Blood gas analysis demonstrated severe hypoxemia [partial pressure of oxygen (PaO2) 70 mmHg, fraction of inspired oxygen (FiO2) 50%]. Bronchoscopy and mechanical ventilation were carried out. Because of limited conditions, clearance of lime from the airway was not performed. The patient’s condition became more severe with additional symptoms such as disturbance of consciousness and fever (maximum 38.0°C). Follow-up CT at 1 d before admission showed a high-intensity mass in the right primary bronchus, right pulmonary atelectasis, right aeropleura, and pneumomediastinum. Blood gas analysis demonstrated severer hypoxemia (PaO2 48 mmHg, FiO2 100%). He then underwent closed drainage of the right thorax and was transferred to our department.
The patient had no history of illness.
The patient had no medical history.
The patient had dysphoria and was delirious. His body temperature was 39.5°C, respiratory rate 35–40 breaths/min, blood pressure 130/65 mmHg, pulse oxygen saturation (SpO2) 60% (FiO2 100%), missed respiratory sound in the right lung, crude respiratory sound in the left lung, no visible injury of the body skin, and conjunctival suffusion.
Blood gas analysis demonstrated severer hypoxemia (PaO2 48 mmHg, FiO2 100%).
CT showed a high-intensity mass in the right principle bronchus and pneumomediastinum (Figure 1A). Follow-up CT showed a high-intensity mass in the right primary bronchus, right pulmonary atelectasis, right aeropleura, and pneumomediastinum.
Aspiration airway injury with respiratory failure caused by burnt lime aspiration.
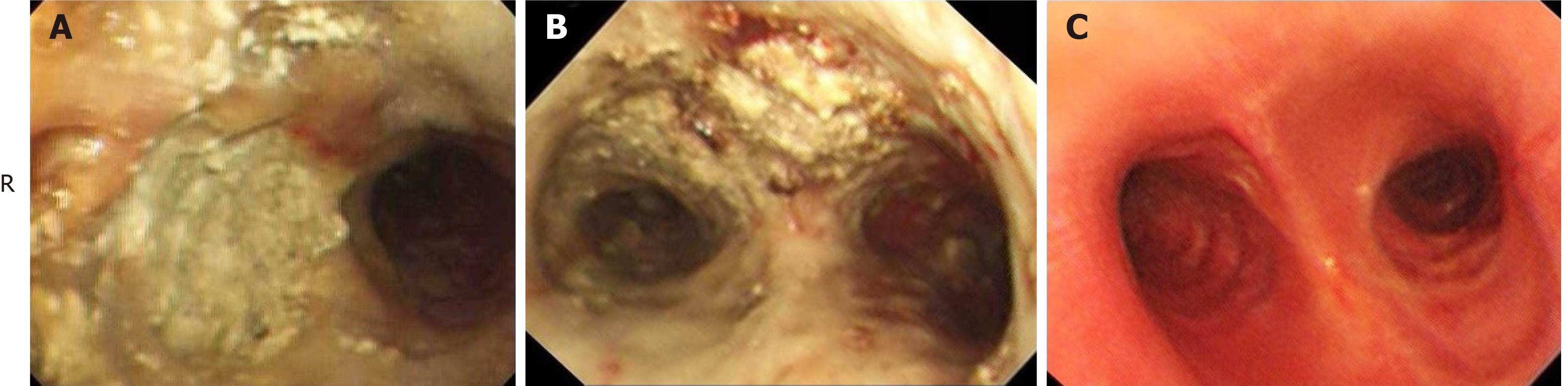
Bronchoscopy showed that the mucosa of the trachea and left bronchus had hyperemia, edema and erosion; the lime powder was deposited diffusely on the mucosa; and the entry of the right principle bronchus was completely obstructed by the lime (Figure 2A). Using foreign body forceps, biopsy forceps, puncture needle, and hairbrush, the lime deposits were loosened and removed. Three hours later, the right primary bronchus was reopened (Figure 2B), and the patient’s oxygenation immediately improved. Although some lime powder was also deposited on the mucous membrane, we did not clean it in case of membrane impairment. After therapy, hypoxia was immediately recovered as identified by blood gas analysis (PaO2 154 mmHg, FiO2 50%). After bronchoscopy, methylprednisolone 40 mg/d intravenously was administered for 3 d. At day 2 after admission, the ventilator was removed. At day 8 after admission, re-examination of the blood gas analysis showed PaO2 79 mmHg (without oxygen uptake). After extracting the tracheotomy tube, the patient left hospital.
Three months after treatment, follow-up bronchoscopy showed cicatricial adhesion at the posterior wall of the pharynx and aryepiglottic fold, restricted abduction of bilateral vocal cords, and disappeared right pyriform sinus and most of the nasal septum. The mucosa at all bronchial levels was smooth and no stenosis or occlusion was found in the bronchi (Figure 2C). Chest CT demonstrated anatomical recovery of the bronchi and lung (Figure 1C).
To our knowledge, searches of databases, including PubMed, Wanfang and CNKI, have revealed only six reports including eight cases (seven adolescents and one adult) who suffered lime aspiration. Most of them inhaled hydrated lime and all received endoairway treatment within 3 d. The conditions of these cases were severe and seven patients underwent bronchoscopy, endotracheal intubation or tracheotomy with mechanical ventilation[1-6]. Among them, seven cases were treated with bronchoalveolar lavage, and one was also treated with foreign body extraction under rigid bronchoscopy. The postoperative prognosis was good, and only one case developed distal bronchial stenosis.
The present case was different; the adult patient inhaled a large amount of lime powder and received airway intervention after 5 d. The patient was treated with tracheotomy and mechanical ventilation, as well as foreign body forceps, biopsy forceps, puncture needles, brush and repeated alveolar irrigation under bronchoscopy, and dozens of lime particles were removed by forceps. Our treatment target was to keep the airway open and not to completely remove the lime. The prognosis was good.
The consequence of lime aspiration is different from those of normal one, especially for burnt lime. The reaction from CaO (burnt lime) to CaO(OH) (hydrated lime) can generate a large amount of heat, which could impair the bronchial mucosa, increase gland secretion, and even cause necrotizing fasciitis. The secretions, indeciduous necrotizing fasciitis and lime blocks are easy to obstruct the airway, causing lethal conditions, which frequently occur at 3–5 d after aspiration[3]. As a result, for patients with large amounts of lime aspiration (especially burnt lime), early tracheoscopy and lime clearance are necessary.
Lime aspiration is usually accompanied by impairment of the oral cavity and respiratory tract; the lime powder can also obstruct the distal segments of the bronchi; and an artificial airway has usually been constructed before bronchoscopy. All these factors restrict the use of rigid bronchoscopy. In the review of the references, all cases used flexible bronchoscopy and one jointly used both the flexible and rigid approaches[3].
According to the location of the foreign body, a rigid or flexible fiberoptic bronchoscope is selected for its removal from the airway[7]. Rigid bronchoscopy is often used for the removal of foreign bodies in the main airway, which has the advantages of maintaining airway ventilation, treatment of hemoptysis, shorter interventional time, and acquisition of large biopsy specimens. However, it may cause damage to the larynx, trachea and bronchi. Selection of the mode of operation is mostly based on touch, and success of the procedure is determined by experience of the operator. The disadvantages of rigid bronchoscopy are that it is not easy to teach or popularize, it has a long operation time and high demand for anesthesia, and has surgical complications[8]. Compared with rigid bronchoscopy, flexible fiberoptic bronchoscopy is a fast, economic and safe procedure that does not require general anesthesia[9]. At present, rigid bronchoscopy combined with flexible fiberoptic bronchoscopy is also used to remove airway foreign bodies[10].
The methods for removing foreign bodies using bronchoscopy are varied depending on the characteristics of the foreign bodies[11-13]. According to the size, shape and texture of the foreign body, various forceps[14], fetching baskets[15] and balloon catheters[16] can be selected. For soft and fragile foreign bodies, frozen electrodes are often used[17-19]. Different interventional treatment techniques can be used according to different chemical characteristics of the foreign bodies. For example, inhalation of tablets often causes local airway inflammation and airway obstruction, so balloon dilatation, argon plasma coagulation and airway stents are often used to relieve airway obstruction[20]. Airway burns can be caused by high temperature physical burns and chemical injuries, and are often diagnosed by bronchoscopy and early alveolar lavage[21]. For airway stenosis caused by chronic granulomatous changes caused by long-term foreign body residues, airway dilatation can be performed by foreign body forceps, holmium laser, freezing, balloon dilatation and other techniques[22,23]. Some rare benign airway diseases, such as tracheobronchopathia osteochondroplastica[24], complicated by severe airway stenosis and recurrent obstructive infection, endoscopic excision and laser ablation are often used to release the airway obstruction. Because of the chemical reaction properties of burnt lime, electroexcision and laser dissection are not suitable[25,26]. Because the texture of the lime particles in the bronchi was soft, it was hard to clamp the particles. Instead, we loosened the lime particles using a puncture needle, cryotherapy and a brush, then clamped the large particles using biopsy and foreign body forceps, and flushed and removed the small particles. The aim of treatment was only to release the airway obstruction; therefore, there was no need to remove all the lime particles on the mucosa, which would fall off naturally and be discharged by coughing.
After aspiration of some chemicals (such as ammonia and oil-based substances), pulmonary fibrosis is generated[27-29]. In the present case, although edema and erosion were seen in the bronchial mucosa at the acute stage, the mucosa recovered completely and showed no pulmonary fibrosis during 3 months’ follow-up. Chlorine inhalation can cause airway inflammation, airway remodeling and stenosis[30]. In the eight previous reports, only one 2-year-old child suffered stenosis of the right medium–lower lobar bronchus[3], which indicates that the bronchi are more susceptible to foreign body aspiration than in adults.
For patients with suspected airway foreign bodies, CT is currently recommended to diagnose and determine the location and size of the foreign bodies[31,32]. For patients with airway foreign bodies complicated with respiratory failure, it is essential to ensure ventilation. Some patients were treated with bronchoscopy under laryngeal mask general anesthesia[33]. Most patients were treated with endotracheal intubation or tracheostomy ventilation combined with endotracheal interventional therapy, and some patients were even treated with endotracheal interventional therapy assisted by extracorporeal membrane oxygenation[34].
Flexible fiberoptic bronchoscopy is suggested as early as possible after lime aspiration, and the treatment target is mainly to keep the airway open and not to completely remove the lime. Moreover, electroexcision or laser dissection should be avoided to remove the lime. Instead, we suggest combining several mechanical methods, such as clamping, flushing and cryotherapy. The prognosis of the patients is usually good when treatment is timely.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Respiratory System
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eccher A S-Editor: Wang JL L-Editor: Kerr C P-Editor: Li JH
| 1. | Gao AP, Bian YQ. [One case report of emergency nursing for child with lime water aspiration]. Huli Xuebao. 2006;13:17. [DOI] [Full Text] |
| 2. | Cao GS, Zhang YL. [Observation for rescuing child with mass particle foreign body aspiration using airway flush]. Zhongguo Jijiu Yixue. 2003;23:201. [DOI] [Full Text] |
| 3. | Wang J, Liu DB, Huang ZY, Qiu SY, Tan ZY. [A successful emergency treatment for child with respiratory failure after lime powder aspiration]. Zhonghua Er Bi Yanhou Toujing Waike Zazhi. 2008;43:792-793. [DOI] [Full Text] |
| 4. | Guo FH, Zhao FM. [One case report of severe lime empyrosis]. Heilongjiang Yiyao Kexue. 2002;25:115. [DOI] [Full Text] |
| 5. | Gao XA. [One case report of acute lung pneumonedema after lime aspiration]. Zhongguo Shiyong Erke Zazhi. 2002;17:503. [DOI] [Full Text] |
| 6. | Lu LC, Guo DY, Qu D, Liu MR. [One case report of treatment of aspirative lung injury by local mediation via fiber bronchoscope]. Qiqihar Yixueyuan Xuebao. 2007;27:1358. [DOI] [Full Text] |
| 7. | Ma W, Hu J, Yang M, Yang Y, Xu M. Application of flexible fiberoptic bronchoscopy in the removal of adult airway foreign bodies. BMC Surg. 2020;20:165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Moura e Sá J, Oliveira A, Caiado A, Neves S, Barroso A, Almeida J, Ferraz JM. Tracheobronchial foreign bodies in adults--experience of the Bronchology Unit of Centro Hospitalar de Vila Nova de Gaia. Rev Port Pneumol. 2006;12:31-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Batra H, Yarmus L. Indications and complications of rigid bronchoscopy. Expert Rev Respir Med. 2018;12:509-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Sancho-Chust JN, Molina V, Vañes S, Pulido AM, Maestre L, Chiner E. Utility of Flexible Bronchoscopy for Airway Foreign Bodies Removal in Adults. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Wu L, Sheng Y, Xu X, Chen Z, Wang Q, Wang Z, Yin Y. Flexible Bronchoscopy Combined with Rigid Bronchoscopy for Treatment of Scarring in the Bronchus Caused by a Foreign Body. Case Rep Med. 2019;2019:4616298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Casalini AG, Majori M, Anghinolfi M, Burlone E, D'Ippolito R, Toschi M, Pisi G, Barantani D, Ghasempour D, Monica M. Foreign body aspiration in adults and in children: advantages and consequences of a dedicated protocol in our 30-year experience. J Bronchology Interv Pulmonol. 2013;20:313-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Sehgal IS, Dhooria S, Ram B, Singh N, Aggarwal AN, Gupta D, Behera D, Agarwal R. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care. 2015;60:1438-1448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 123] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 14. | Afzal M, Al Mutairi H, Chaudhary I. Fractured tracheostomy tube obturator: A rare cause of respiratory distress in a tracheostomized patient. World J Anesthesiol. 2013;2:30-32. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Endoh M, Oizumi H, Kanauchi N, Kato H, Ota H, Suzuki J, Watarai H, Nakamura M, Sadahiro M. Removal of foreign bodies from the respiratory tract of young children: Treatment outcomes using newly developed foreign-body grasping forceps. J Pediatr Surg. 2016;51:1375-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Strychowsky JE, Roberson DW, Martin T, Smithers J, Herrington H. Proximal bronchial balloon dilation for embedded distal airway foreign bodies. Laryngoscope. 2016;126:1693-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Fang YF, Hsieh MH, Chung FT, Huang YK, Chen GY, Lin SM, Lin HC, Wang CH, Kuo HP. Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One. 2015;10:e0118993. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Tale S, Meitei SP, Prakash V, Negi A, Mishra M, Sindhwani G. Bronchoscopic Cryotherapy for Acute Hypoxemic Respiratory Failure in Three Mechanically Ventilated Patients: A Case Series. Indian J Crit Care Med. 2021;25:94-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Kazachkov M, Vicencio A. Foreign body removal is getting "cooler". Pediatr Pulmonol. 2016;51:886-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Zhang L, Yin Y, Zhang J, Zhang H. Removal of foreign bodies in children's airways using flexible bronchoscopic CO2 cryotherapy. Pediatr Pulmonol. 2016;51:943-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 21. | Keshishyan S, Mohan A, Ahmed S, Dhillon SS, Patil M, Harris K. Airway Obstruction Caused by Iron Pill Aspiration: An Interventional Pulmonology Approach to Prevent Surgery. Heart Lung Circ. 2018;27:e89-e92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Reid A, Ha JF. Inhalational injury and the larynx: A review. Burns. 2019;45:1266-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Liao QN, Fang ZK, Chen SB, Fan HZ, Chen LC, Wu XP, He X, Yu HP. Pleomorphic adenoma of the trachea: A case report and review of the literature. World J Clin Cases. 2020;8:6026-6035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Riva G, Girolami I, Luchini C, Villanova M, Valotto G, Cima L, Carella R, Riva M, Fraggetta F, Novelli L, Eccher A. Tracheobronchopathia Osteochondroplastica: A Case Report Illustrating the Importance of Multilevel Workup Clinical, Endoscopic and Histological Assessment in Diagnosis of an Uncommon Disease. Am J Case Rep. 2019;20:74-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Li S, Wu L, Zhou J, Wang Y, Jin F, Chen X, Liu J, Chen Z. Interventional therapy via flexible bronchoscopy in the management of foreign body-related occlusive endobronchial granulation tissue formation in children. Pediatr Pulmonol. 2021;56:282-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Dong YC, Zhou GW, Bai C, Huang HD, Sun QY, Huang Y, Han YP, Li Q. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med. 2012;51:2515-2519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | Ali R, Mittal G, Sultana S, Bhatnagar A. Ameliorative potential of alpha-ketoglutaric acid (AKG) on acute lung injuries induced by ammonia inhalation in rats. Exp Lung Res. 2012;38:435-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Yampara Guarachi GI, Barbosa Moreira V, Santos Ferreira A, Sias SM, Rodrigues CC, Teixeira GH. Lipoid pneumonia in a gas station attendant. Case Rep Pulmonol. 2014;2014:358761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Stathis G, Priftis KN, Moustaki M, Alexopoulou E. Non-resolving Findings in a Long-term Radiographic Follow-up of an Infant with Acute Paraffin Oil Aspiration. J Clin Imaging Sci. 2014;4:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Hoyle GW, Svendsen ER. Persistent effects of chlorine inhalation on respiratory health. Ann N Y Acad Sci. 2016;1378:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 31. | Pitiot V, Grall M, Ploin D, Truy E, Ayari Khalfallah S. The use of CT-scan in foreign body aspiration in children: A 6 years' experience. Int J Pediatr Otorhinolaryngol. 2017;102:169-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 32. | Huang HJ, Fang HY, Chen HC, Wu CY, Cheng CY, Chang CL. Three-dimensional computed tomography for detection of tracheobronchial foreign body aspiration in children. Pediatr Surg Int. 2008;24:157-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Suzen A, Karakus SC, Erturk N. The role of flexible bronchoscopy accomplished through a laryngeal mask airway in the treatment of tracheobronchial foreign bodies in children. Int J Pediatr Otorhinolaryngol. 2019;117:194-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Anton-Martin P, Bhattarai P, Rycus P, Raman L, Potera R. The Use of Extracorporeal Membrane Oxygenation in Life-Threatening Foreign Body Aspiration: Case Series, Review of Extracorporeal Life Support Organization Registry Data, and Systematic Literature Review. J Emerg Med. 2019;56:523-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |