Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9878
Peer-review started: June 18, 2021
First decision: August 18, 2021
Revised: August 27, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: November 16, 2021
Processing time: 144 Days and 14.6 Hours
Proximal femoral nails (PFNs) are the most common method for the treatment of unstable intertrochanteric femoral fractures (IFFs), but postoperative bed rest is required. There is a large amount of blood loss during the operation. Osteoporosis in elderly patients may cause nonunion of fractures and other complications. Arthroplasty can give patients early weight bearing and reduce financial burden, but whether it can replace PFNs remains controversial.
To compare the clinical outcomes of arthroplasty and PFNs in the treatment of unstable IFFs in elderly patients.
A search was conducted in the PubMed, Embase, and Cochrane Library databases and included relevant articles comparing arthroplasty and PFN. The search time was limited from January 1, 2005 to November 1, 2020. Two investigators independently screened studies, extracted data and evaluated the quality according to the inclusion and exclusion criteria. According to the research results, the fixed effect model or random effect model were selected for analysis. The following outcomes were analyzed: Harris Hip score, mortality, complications, operation time, blood loos, hospital stay, weight-bearing time, fracture classification and type of anesthesia.
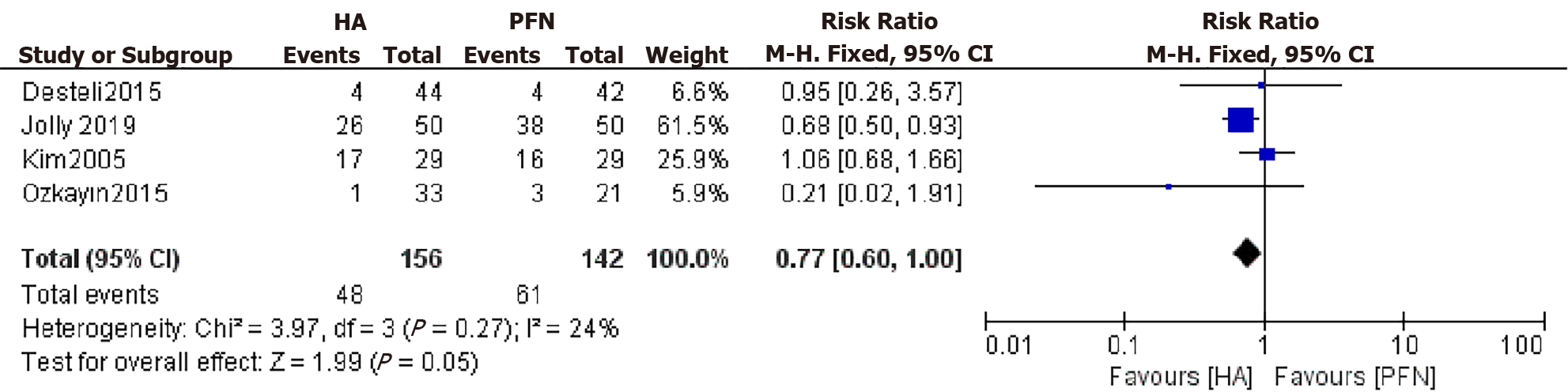
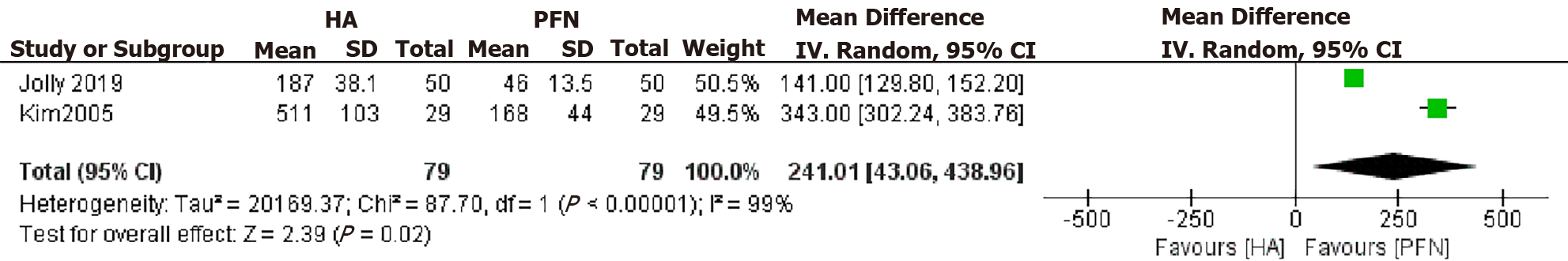
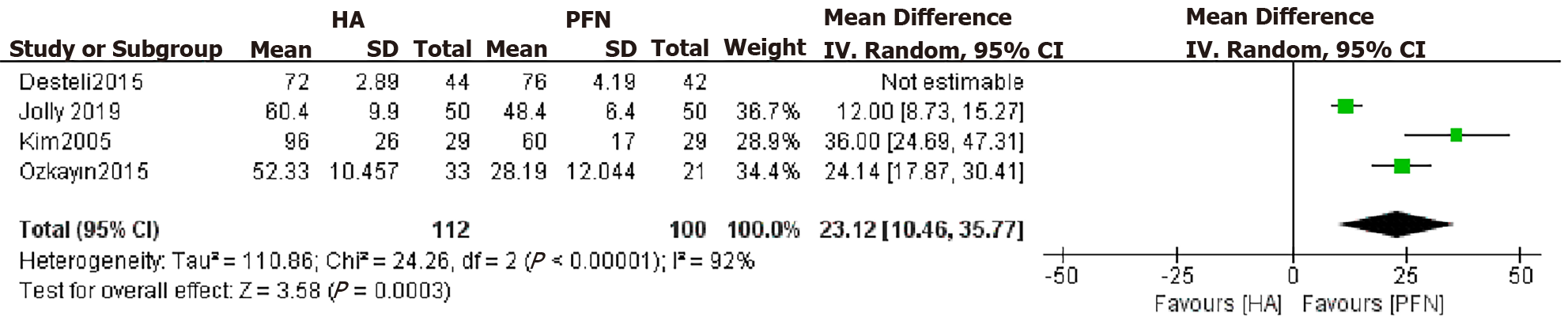
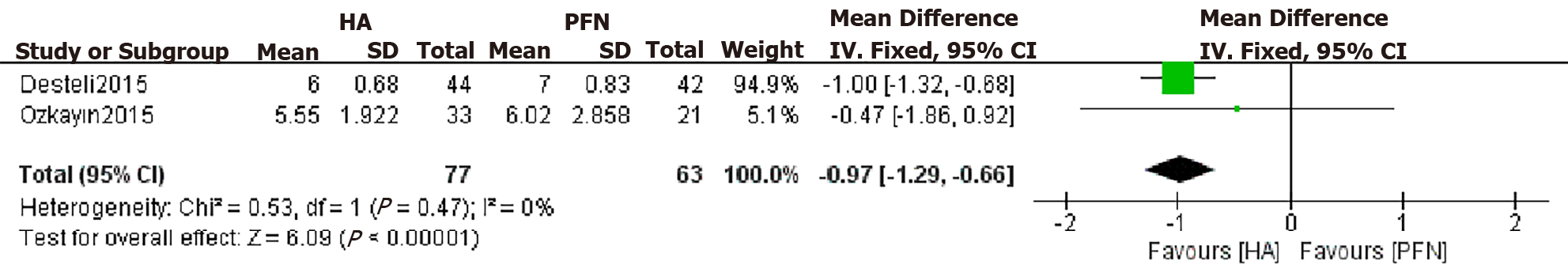
We analyzed four randomized controlled trials that met the requirements. A total of 298 patients were included in these studies. According to the AO/OTA classification, there are 20 A1 types, 136 A2 types, 42 A3 types and 100 unrecorded types. Primary outcome: The Harris Hip Score at the final follow-up of the PFN group was higher [mean difference (MD): 9.01, 95% confidence interval (CI): 16.57 to 1.45), P = 0.02]. There was no significant difference between the two groups in the rate of overall mortality [risk ratio (RR): 1.44, P = 0.44] or the number of complications (RR: 0.77, P = 0.05). Secondary outcomes: blood loss of the arthroplasty group was higher (MD: 241.01, 95% CI: 43.06–438.96, P = 0.02); the operation time of the PFN group was shorter (MD: 23.12, 95%CI: 10.46–35.77, P = 0.0003); and the length of hospital stay of the arthroplasty group was shorter [MD: 0.97, 95% CI: 1.29 to 0.66), P < 0.00001]. There was no difference between the two groups in the type of anesthesia (RR: 0.99). There were only two studies recording the weight-bearing time, and the time of full weight bearing in the arthroplasty group was significantly earlier.
Compared with PFN, arthroplasty can achieve weight bearing earlier and shorten hospital stay, but it cannot achieve a better clinical outcome. Arthroplasty cannot replace PFNs in the treatment of unstable IFFs in elderly individuals.
Core Tip: This review compared the clinical outcomes of arthroplasty and proximal femoral nails (PFNs) in the treatment of unstable intertrochanteric femoral fractures (IFFs) in elderly patients. Many people believe that arthroplasty can replace PFNs for unstable IFFs in elderly patients. However, there is no consensus. Some researchers have carried out reviews of the research, but the results were different. Therefore, we conducted this meta-analysis. We reviewed four randomized controlled trials about this topic and found that arthroplasty cannot achieve better results than PFNs in the clinic. Arthroplasty is not the first choice for the treatment of unstable IFFs in elderly patients.
- Citation: Chen WH, Guo WX, Gao SH, Wei QS, Li ZQ, He W. Arthroplasty vs proximal femoral nails for unstable intertrochanteric femoral fractures in elderly patients: A systematic review and meta-analysis. World J Clin Cases 2021; 9(32): 9878-9888
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9878.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9878
Intertrochanteric femoral fracture (IFF) is a common type of hip fracture and is extracapsular in nature. The incidence of IFFs accounts for 3.51% of systemic fractures, and IFFs are more common in elderly individuals[1]. AO/OTA classification is commonly used in clinical practice. Among the different types of IFFs, 31A1 and A2.1 are considered stable fractures, while the rest are unstable. With the increase in the human lifespan and the arrival of a globally aging society, the incidence of the disease is also increasing yearly. Thus, to achieve good stability and activity, surgeons are more willing to choose surgical treatment. Because strong internal fixation can promote the early recovery of limb function and reduce the occurrence of complications, surgical treatment has gradually become the preferred treatment[2]. The proximal femoral nail (PFN) is more consistent with the anatomical shape of the femur and provides better stability, so most clinicians choose PFNs to treat unstable IFFs[3-5]. However, for elderly patients, osteoporosis often increases the failure rate of surgery[6] and leads to many complications and poor prognosis[7]. As a result, some people focus on artificial hip joint replacement, which can be used as a better treatment for some elderly patients with IFFs[8].
Arthroplasty can allow patients to achieve full weight bearing early, thus reducing the complications of long-term bed rest[9,10]. Studies have shown that bilateral hemiarthroplasty treatment of unstable IFFs can achieve good therapeutic effects[11]. However, there are also significant complications related to arthroplasty, such as bone marrow mud syndrome, a large amount of bleeding, prosthesis loosening, and wound infection[12].
Many scholars have conducted clinical studies to find evidence to prove that arthroplasty can replace PFNs in treating unstable IFFs in elderly patients, but there is no consensus[13-15]. Therefore, we conducted this meta-analysis and systematic review of RCTs to determine whether arthroplasty can achieve better results than PFNs in the treatment of unstable IFFs at an advanced age (> 60 years).
This article was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[16]. The primary search was conducted in PubMed, Embase and Cochrane Library databases by two investigators independently. They used the keywords and synonyms listed in Table 1 to aggregate all of the relevant published studies. Each investigator reviewed all titles, abstracts, and full texts of the potentially related studies.
| Database | Methodology | Results |
| PubMed | {[(hip fracture) or (intertrochanteric fracture)] or (femoral fracture)} and [(aged or elderly) or senile] and {[(Arthroplasty, Replacement, Hip or Hemiarthroplasty or Prosthesis Implantation) or (total hip replacement)] or (hip replacement)} and (randomized). Filters: From 2005 to 2020 | 430 |
| EMBASE | ('femur intertrochanteric fracture'/exp or 'hip fracture'/exp or 'femoral fracture'/exp) and ('aged'/exp OR 'elderly'/exp) and ('hip replacement'/exp or 'hip hemiarthroplasty'/exp or 'total hip replacement'/exp or 'arthroplasty'/exp) and (‘randomized’) and [(2005-2020)/py] | 239 |
| Cochrane Library | [(hip fracture) or (intertrochanteric fracture) or (femoral fracture)] and (aged or elderly or senile) and (Arthroplasty or Hemiarthroplasty or Prosthesis Implantation or hip replacement). Custom year range: 2005 to 2020 | 554 |
Studies were selected according to the inclusion and exclusion criteria. The inclusion criteria were all RCT studies on arthroplasty and PFNs in the treatment of elderly patients with IFFs. Through reading the literature, we found that there were few reports before 2005on the clinical effects of PFN. Therefore, the research publication time was limited to between 2005 and 2020. The exclusion criteria were non-RCT studies, cadaver studies, biomechanical studies, conference abstracts, case reports, editorial reviews, patients aged ≤ 60 years, inconsistent publication time, and studies not written in English. The primary outcomes were the Harris Hip Score (HHS) at the final follow-up time, the rate of postoperative overall mortality and the number of complications. Secondary outcomes were blood loss, operation time, length of hospital stay, weight-bearing time and type of anesthesia.
RevMan 5.4 software, provided by the Cochrane Collaboration Network, was used for statistical analysis. The relative risk (RR) was used as the effect analysis statistic for two categorical variables, and the mean difference (MD) was used for continuous variables. The heterogeneity of the included results was determined using the I2 test. If there was no statistical heterogeneity among the research results, the fixed effect model was used for meta-analysis; otherwise, the random effect model was used after excluding the influence of obvious clinical heterogeneity. Significant clinical heterogeneity was treated by subgroup analysis, sensitivity analysis, or descriptive analysis. The test level of meta-analysis was set as P = 0.05.
The Cochrane Collaboration Risk of Bias Tool was used to evaluate the quality of the RCTs by two independent investigators.
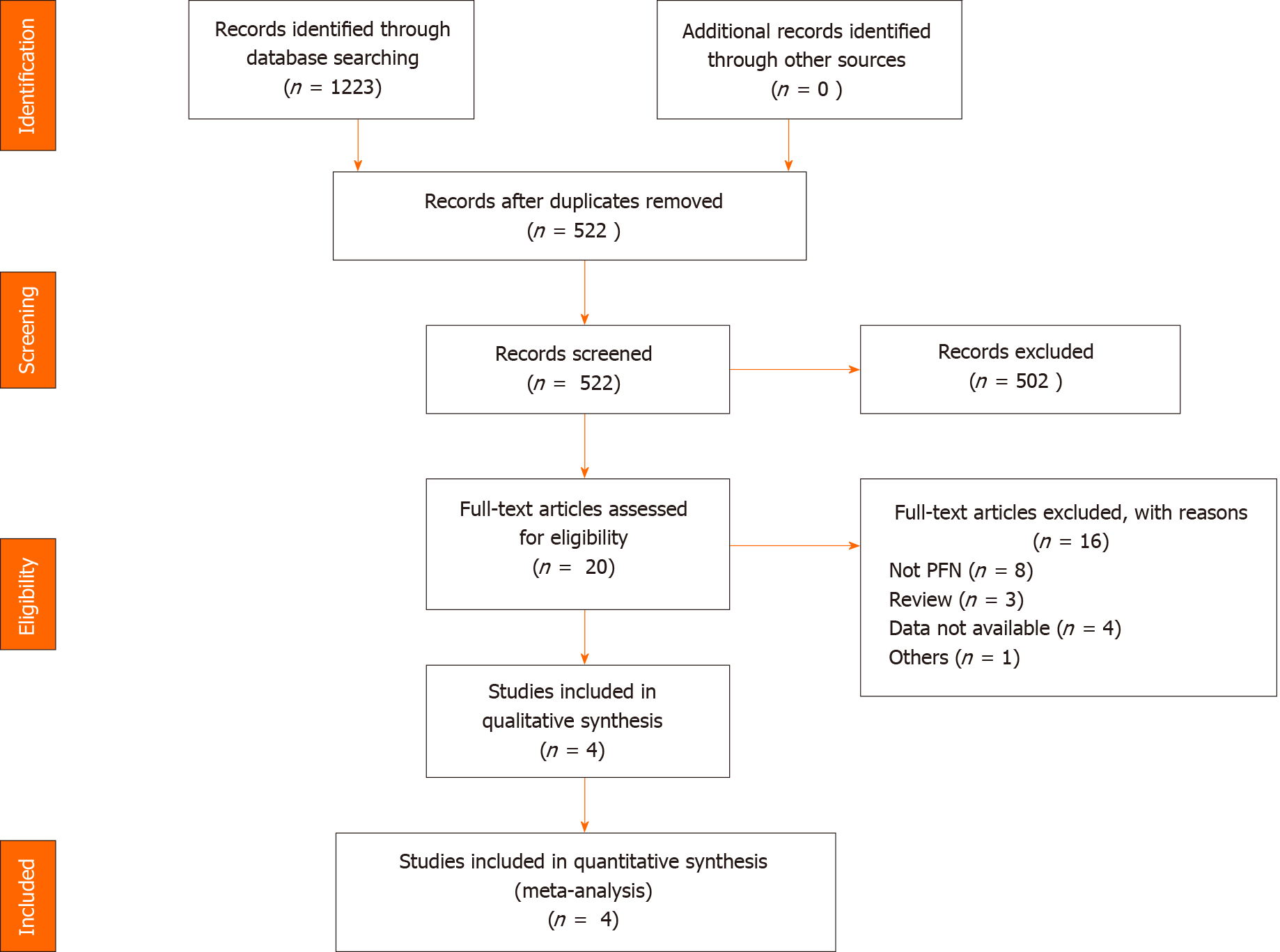
The literature was searched by two investigators and screened strictly by reading the title, abstract, or full text of the article according to the inclusion and exclusion criteria. A total of 1223 studies were obtained, and 502 were excluded by reading the titles and abstracts, and 20 relevant studies were identified for further evaluation. After screening the full texts, 16 studies were excluded. Ultimately, four RCTs were identified for the meta-analysis[14,15,17,18] (Figure 1).
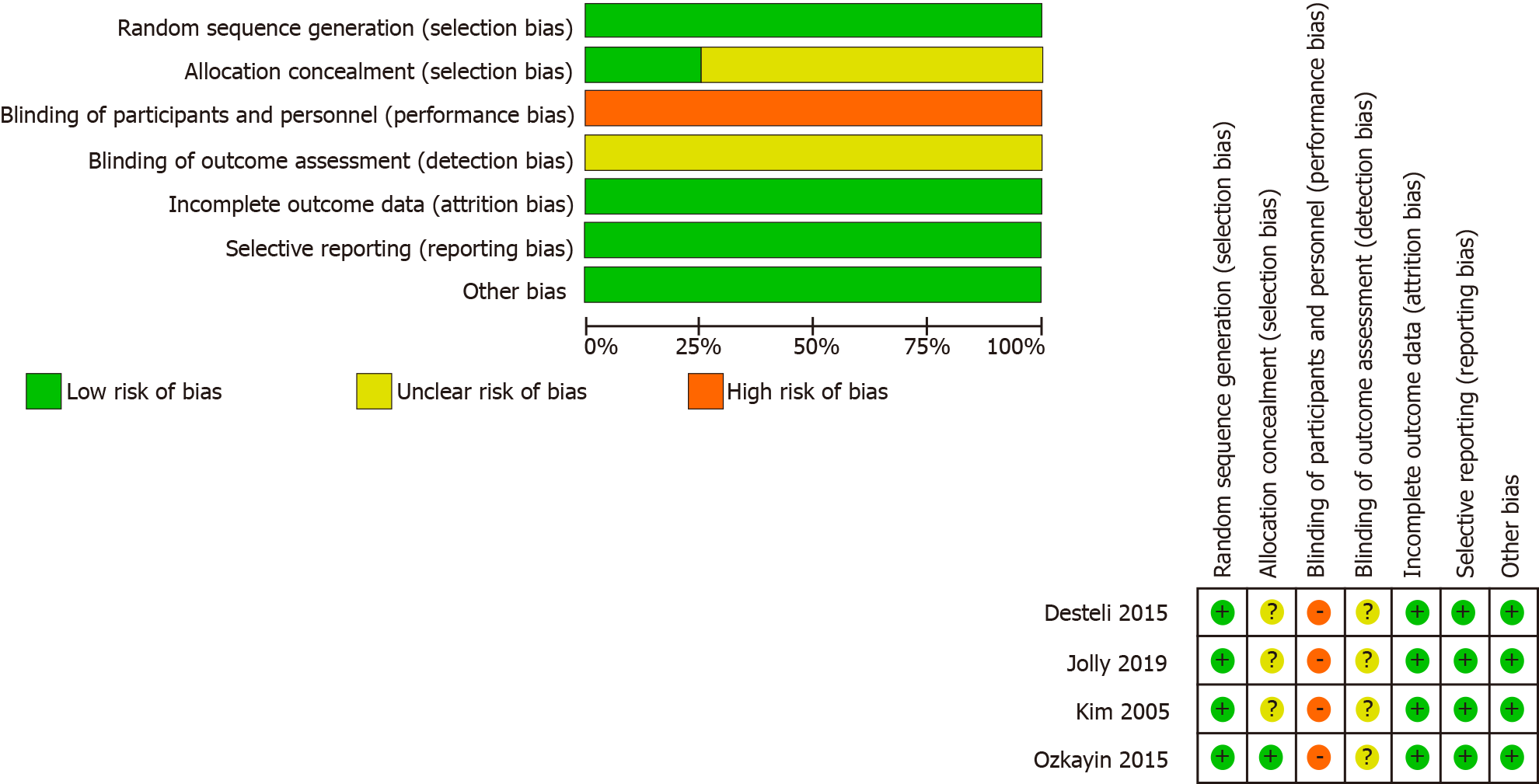
The results of bias risk assessment in RCTs are shown in Figure 2. None of the included RCTs reported blinding of the surgeons, participants, or assessors. The checklist is in the additional file.
The basic characteristics of the included studies are shown in SupplementaryTables 1 and 2. There were 298 patients, forming the arthroplasty group (n = 156) and PFN group (n = 142).
All the patients in the four studies were aged > 60 years, and most of them were 75–85 years old. There was no significant difference in age between any of the studies. There was no significant difference between the arthroplasty and PFN groups in the sex ratio in three studies. However, the number of IFFs in women was greater than that in men in two studies, which may be related to osteoporosis and bone strength reduction caused by decreased estrogen levels[19,20].
Three studies reported the fracture types of the included patients. In the arthroplasty group, there were 10 patients with type A1 fractures, 73 with type A2 and 23 with types A3. In the PFN group, there were 10 patients with type A1, 63 with type A2 and with types A3 fractures. The number of stable fractures was small, and the corresponding data were not provided in the original literature, so they are not excluded in the analysis. The three studies did not list the incidence of outcomes for different classifications; therefore, subgroup analysis could not be conducted.
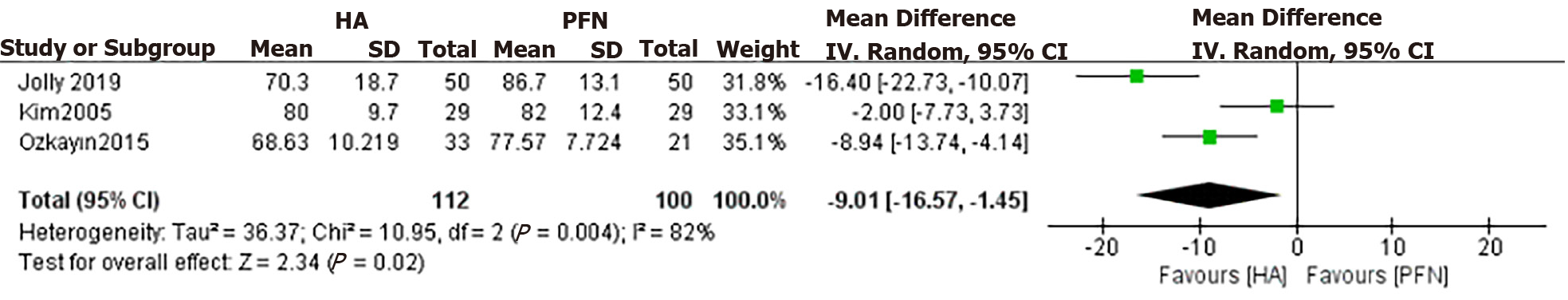
HHS: The HHS at the end of follow-up was compared between the arthroplasty and PFN groups. Three studies mentioned the HHS and included the mean and standard deviation (SD). The results of the fixed effect model showed that there was statistical heterogeneity among studies (P = 0.004, I2 = 82%), so we chose the random effect model for analysis. There was a significant difference in HHS between the arthroplasty and PFN groups [MD = 9.01, 95% confidence interval (CI): 16.57 to 1.45), P = 0.02]. The score of the PFN group at the end of follow-up was higher than that of the arthroplasty group. All the studies included were followed up for > 12 mo. Except for Jolly[18], the other three studies were followed up for > 24 mo. Moreover, in terms of hip function, the arthroplasty group did not achieve better results (Figure 3).
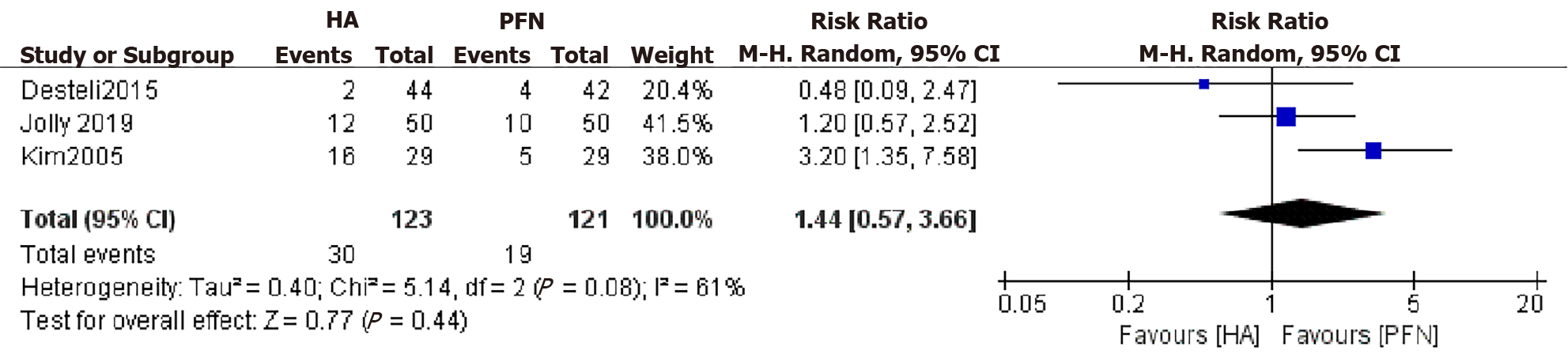
Mortality: The rate of overall mortality was assessed by three studies. The results of the fixed effect model showed that there was heterogeneity among studies (P = 0.08, I2 = 61%), so we chose the random effect model for analysis. There was no significant difference between the two groups (RR: 1.44, 95% CI: 0.57–3.66, P = 0.44) (Figure 4).
Complications: The four studies documented complications, including superficial infection, deep infection, implant failure, respiratory infection, and venous thromboembolism. There was no significant difference between the two groups (RR: 0.77, 95% CI: 0.60–1.00, P = 0.05) (Figure 5).
Blood loss: Blood loss was compared between the arthroplasty and PFN groups. Two studies recorded the intraoperative bleeding volume. The results of the fixed effect model showed that there was statistical heterogeneity among studies (P < 0.00001, I2 = 99%), so we chose the random effect model for analysis. There was a significant difference between the two groups (MD: 241.01, 95% CI: 43.06–438.96, P = 0.02). The blood loss of the arthroplasty group was higher than that of the PFN group (Figure 6).
Operation time: The operation times for the arthroplasty and PFN groups were compared in the four studies. The results of the fixed effect model showed that there was statistical heterogeneity among all studies (P < 0.00001, I2 = 97%). After discussion, we excluded a study that had a greater impact on heterogeneity and used a random effect model for analysis. There was a significant difference in operation time between the arthroplasty and PFN groups (MD: 23.12, 95% CI: 10.46–35.77, P = 0.0003). The operation time of the PFN group was significantly shorter than that of the arthroplasty group. A longer operation time and more intraoperative bleeding was found to easily lead to more potential complications and affect the patient’s postoperative recovery (Figure 7).
Hospital stay: The lengths of hospital stay for the arthroplasty and PFN groups were compared. Two studies mentioned the days and included the mean and SD. The results of the fixed effect model showed that there was a significant difference in the length of hospital stay between the arthroplasty and PFN groups [MD: 0.97, 95% CI: 1.29 to 0.66), P < 0.00001]. The length of stay in the arthroplasty group was significantly shorter than that in the PFN group (Figure 8).
Weight-bearing time: Only two studies recorded the weight-bearing time. One recorded full weight-bearing time, and the other recorded walking with a walker. In addition, their units were different. Thus, we did not combine the results of the two papers. Jolly[18] documented that the mean time of full weight bearing in the PFN group was 10.1 ± 3.5 wk, while the mean time in the arthroplasty group was 3.2 ± 4.7 wk. Kim[14] documented that the time of walking with a walker in the PFN group was 8.8 ± 2.9 d, while that in the arthroplasty group was 7.8 ± 1.6 d. The weight-bearing time of the arthroplasty group was significantly shorter than that of the PFN group. The time of weight bearing reflects the time of postoperative bed rest. Shorter postoperative bed rest and hospital stay can reduce the complications caused by long-term bed rest, but a large amount of intraoperative blood loss and excessive operation time are not conducive to patients’ self-repair.
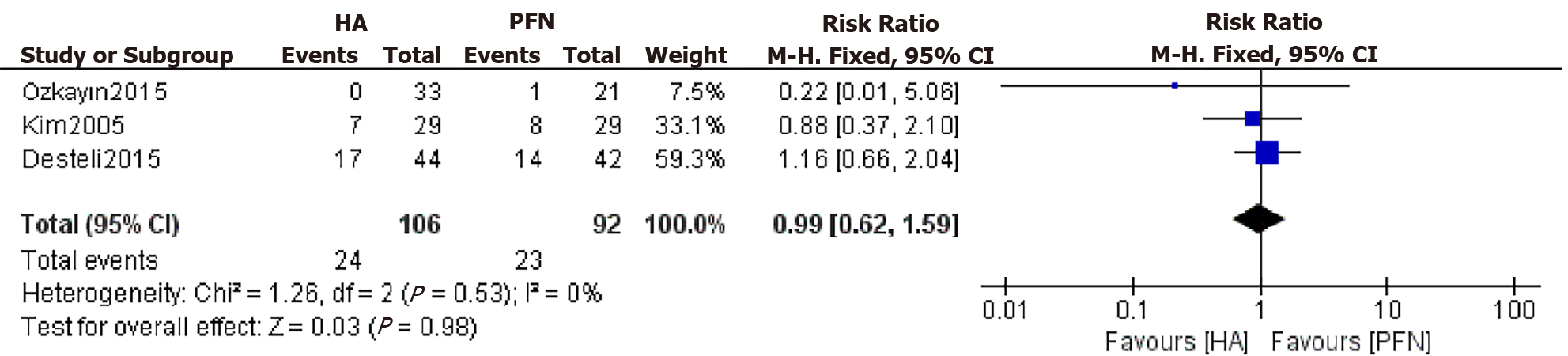
Type of anesthesia: The type of anesthesia is a preoperative factor. Three studies recorded the type of anesthesia. The results showed that there was no significant difference between the arthroplasty and PFN groups, meaning that the anesthetic will not affect the therapeutic effect (RR: 0.99, 95% CI: 0.62–1.59, P = 0.98) (Figure 9).
The incidence rate of intertrochanteric fracture accounts for 50% of hip fractures[21]. Most intertrochanteric fractures are comminuted and unstable because of the lower bone strength in elderly people. It is difficult to achieve satisfactory results in conservative treatment, while surgical treatment can reduce complications and contribute to rehabilitation training. Therefore, we conducted a meta-analysis of RCTs and evaluated the clinical outcomes of elderly patients with unstable IFFs who underwent PFN or arthroplasty. In this meta-analysis, the type of anesthesia and fracture classification did not affect the clinical outcome. In the AO/OTA classification of IFFs, types A1 and A2.1 were considered stable fractures, while the rest were considered unstable fractures. In this study, the number of unstable fractures accounted for 60% of the included study reports. However, since the study reports did not list the incidence of adverse events in different classifications, no subgroup analysis was conducted. Compared with the PFN group, the arthroplasty group had earlier time to weight bearing, shorter hospital stay, more intraoperative bleeding, and longer operation time. There were no significant differences in postoperative complications or overall mortality between the two groups. The HHS at the final follow-up was significantly better in the PFN group than in the arthroplasty group.
The recovery of hip function is the most important concern of clinicians and patients. The HHS is the most common score in the clinical evaluation of hip function. The higher the score, the better the function. It comprehensively evaluates the affected limb from the four aspects of deformity, range of motion, pain and function to judge the degree of patients returning to normal activities of life. Among the four studies, only Desteli[15] used EQ-5D and mobility scores, while other studies used HHS. With the exception of Jolly[18], which was followed up for 12 mo, all other studies were followed up for > 24 mo, and the final HHS of all the studies was higher in the PFN group than in the arthroplasty group, indicating that with fracture healing, when the internal fixation was stable, the limb function provided by arthroplasty was not superior to PFNs. Arthroplasty does not provide significantly better hip function than PFNs. This is different from the report of Tu et al[21], who meta-analyzed the HHS of two RCTs and two retrospective comparative control trials, and showed that there was no significant difference between arthroplasty and PFNs. We think this may be due to the different types of studies included by us and them; additionally, retrospective studies may have patient selection bias.
Postoperative overall mortality is an important factor for the prognosis of hip fracture, and a point of concern to patients and their families. Most elderly patients have medical diseases of other systems, and they are more likely to die under the stimulation of trauma and surgery. Some studies record that arthroplasty of IFFs in elderly patients can reduce mortality by reducing bed time[9]. In contrast, some studies have reported that the postoperative mortality of the arthroplasty group is significantly higher than that of internal fixation[22,23]. In this study, a total of three articles reported overall mortality during the follow-up period, and the results showed that there was no significant difference between the arthroplasty and PFN groups, indicating that arthroplasty cannot reduce the incidence of postoperative mortality. It is important to note that although the difference was not significant, the number of deaths in the joint replacement group increased with the extension of follow-up time, which is consistent with other studies in the past 3 years[18,21,24].
There are many postoperative complications of unstable IFFs in elderly patients, including bedsores, respiratory infections, superficial wound infections, deep infections, deep vein thrombosis (DVT), periprosthetic fractures, nonunion of fractures, urinary tract infections, and dislocations of the prosthesis. Some of the postoperative complications were reported in the four studies included here. After meta-analysis, we found that there was no significant difference between arthroplasty and PFNs. This is consistent with the results of a previous study[8]. Arthroplasty may reduce the incidence of long-term bed rest complications such as DVT and bedsores by reducing the time spent in bed, but it cannot reduce the overall incidence of postoperative complications.
Operation time and blood loss are important indicators to evaluate the quality of the surgery and judge the prognosis. The operation time is usually proportional to the amount of intraoperative blood loss. The longer the operation time, the more blood loss there is, which increases cardiovascular and respiratory complications and risk of wound infection. In this study, the intraoperative blood loss and operation time of the arthroplasty group were significantly greater than those of the PFN group, which is consistent with the results of another previous study[13]. Before 2005, arthroplasty was not widely used in the clinical treatment of IFFs. Many doctors are less proficient in arthroplasty, which results in longer operation time and more blood loss than traditional internal fixation methods. Notably, the average amount of bleeding reported by Kim was as high as 511 mL and close to three times that reported by Jolly[18] in 2019. We think that this is related to the technical level and proficiency of the surgeons. In particular, the surgical technique of calcar-replacement prosthesis is more advanced. When dealing with more comminuted unstable fractures, it is more difficult to fix. Sometimes it even needs to be fixed with steel wire and the amount of bleeding and operation time are also significantly increased. Authen[25] points out that doctors with less surgical experience have higher rates of adverse events than experienced doctors have. This may be the reason for the high heterogeneity of the outcomes in this study.
The weight-bearing time greatly affects the overall length of hospital stay. Salpakoski[26] noted that walking after internal fixation is more difficult than walking after joint replacement. Kim[14] and Jolly[18] also reported that the arthroplasty group had an earlier loading time. The two articles included in this study reported the times of full and half weight bearing. The arthroplasty group was capable of weight bearing significantly earlier than the PFN group was. Similarly, the length of hospital stay in the arthroplasty group was significantly shorter. These differences are related to many factors. Arthroplasty can allow patients to get out of bed early; promote the recovery of limb function; avoid complications such as bedsores caused by long-term bed rest[27,28]; significantly reduce the length of hospital stay and the economic burden of patients; help patients recover their mental health and return to normal life; and quickly improve their quality of life. This is why, in recent years, an increasing number of clinicians have considered arthroplasty to treat unstable IFFs in elderly patients. Moreover, osteoarthritis of the hip in elderly patients is a major factor for clinicians to consider when using arthroplasty in the treatment of IFFs.
The most important limitation of the study is that the number of RCTs was slightly lower, so the strength of the evidence was inadequate. Other limitations are the experience of surgeons and the blinding of inclusion studies, which may influence the heterogeneity. There was significant heterogeneity in several important parameters and the cause of this heterogeneity was often not identified and controlled for. It is likely that heterogeneity arose from the different patient populations and center experiences. Since the original literature does not provide relevant data, we cannot discuss the difference between different types of fractures. It is necessary for our further study to collect more high-quality RCTs for analysis.
As a classic method for the treatment of unstable IFFs, PFNs have been widely recognized in clinical practice. Their clinical effect is definite, and the disadvantages of needing to lie in bed after surgery also exist all the time. Therefore, in recent years, some researchers have been trying to find evidence from clinical studies, aiming to use arthroplasty to replace PFNs in the treatment of unstable IFFs. However, while there are differences in the results reported in the literature, there is no conclusion thus far. The results of this study indicate that, compared with PFNs, although arthroplasty can shorten bed time and hospital stay, it cannot reduce postoperative complications and mortality of elderly patients with unstable IFFs; moreover, the operation time and blood loss are significantly increased. PFNs were associated with better limb function after stabilization of fracture healing with longer follow-up. Therefore, joint replacement is not a substitute for PFNs in the treatment of elderly patients with unstable IFFs.
Proximal femoral nails (PFNs) and arthroplasty are common methods for the treatment of intertrochanteric femoral fractures (IFFs), but there is no consensus on which treatment is better for elderly patients with unstable fractures.
At present, many retrospective studies have compared and analyzed the clinical efficacy of arthroplasty and PFNs in the treatment of unstable IFFs, but the results differed. To explore whether arthroplasty can really replace PFNs as the preferred treatment, we conducted this study.
To compare the clinical outcomes of arthroplasty and PFNs in the treatment of unstable IFFs in elderly patients and determine whether arthroplasty can replace traditional PFNs.
Through meta-analysis and systematic review, we summarized the randomized controlled trials (RCTs) in the past 20 years. According to the inclusion and exclusion criteria, the results of four RCTs were finally included for analysis. According to the data given in the literature, the Harris Hip Score (HHS), mortality, complications, blood loss, operation time and hospital stay, weight-bearing walking time and anesthesia of the two methods were analyzed and compared.
The joint replacement group had earlier weight-bearing walking time and shorter hospital stay, but the HHS, bleeding volume and operation time in the PFN group were better. There were no significant differences in mortality, complications and anesthesia between the two groups.
Based on available evidence, arthroplasty cannot replace PFNs in the treatment of unstable IFFs in elderly patients.
More high-quality clinical studies are needed to judge whether joint replacement can replace PFNs as the first choice for the treatment of unstable IFFs in elderly patients.
We thank all authors for their helpful conversations about this manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kakoulidis P S-Editor: Wang JJ L-Editor: Kerr C P-Editor: Guo X
| 1. | Lu Y, Uppal HS. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr Orthop Surg Rehabil. 2019;10:2151459319859139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 2. | Dehghan N, McKee MD. What's New in Orthopaedic Trauma. J Bone Joint Surg Am. 2020;102:1137-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Ballal MS, Emms N, Thomas G. Proximal femoral nail failures in extracapsular fractures of the hip. J Orthop Surg (Hong Kong). 2008;16:146-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Ertürer RE, Sönmez MM, Sarı S, Seçkin MF, Kara A, Oztürk I. Intramedullary osteosynthesis of instable intertrochanteric femur fractures with Profin® nail in elderly patients. Acta Orthop Traumatol Turc. 2012;46:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Koval KJ. Intramedullary nailing of proximal femur fractures. Am J Orthop (Belle Mead NJ). 2007;36:4-7. [PubMed] |
| 6. | Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P 3rd, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85:1673-1681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 374] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 7. | Camurcu Y, Cobden A, Sofu H, Saklavci N, Kis M. What Are the Determinants of Mortality After Cemented Bipolar Hemiarthroplasty for Unstable Intertrochanteric Fractures in Elderly Patients? J Arthroplasty. 2017;32:3038-3043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Kumar P, Rajnish RK, Sharma S, Dhillon MS. Proximal femoral nailing is superior to hemiarthroplasty in AO/OTA A2 and A3 intertrochanteric femur fractures in the elderly: a systematic literature review and meta-analysis. Int Orthop. 2020;44:623-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Grimsrud C, Monzon RJ, Richman J, Ries MD. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplasty. 2005;20:337-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Park MS, Cho HM, Kim JH, Shin WJ. Cementless bipolar hemiarthroplasty using a rectangular cross-section stem for unstable intertrochanteric fractures. Hip Int. 2013;23:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Feehan LM, Tang CS, Oxland TR. Early controlled passive motion improves early fracture alignment and structural properties in a closed extra-articular metacarpal fracture in a rabbit model. J Hand Surg Am. 2007;32:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Singh V, Bhakta P, Zietak E, Hussain A. Bone cement implantation syndrome: a delayed postoperative presentation. J Clin Anesth. 2016;31:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Nie B, Wu D, Yang Z, Liu Q. Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: A meta-analysis. Medicine (Baltimore). 2017;96:e7446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Kim SY, Kim YG, Hwang JK. Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg Am. 2005;87:2186-2192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 80] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Desteli EE, İmren Y, Erdoğan M, Aydagün Ö. Quality of Life Following Treatment of Trochanteric Fractures with Proximal Femoral Nail versus Cementless Bipolar Hemiarthroplasty in Elderly. Clin Invest Med. 2015;38:E63-E72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17367] [Article Influence: 1085.4] [Reference Citation Analysis (1)] |
| 17. | Özkayın N, Okçu G, Aktuğlu K. Intertrochanteric femur fractures in the elderly treated with either proximal femur nailing or hemiarthroplasty: A prospective randomised clinical study. Injury. 2015;46 Suppl 2:S3-S8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Jolly A, Bansal R, More AR, Pagadala MB. Comparison of complications and functional results of unstable intertrochanteric fractures of femur treated with proximal femur nails and cemented hemiarthroplasty. J Clin Orthop Trauma. 2019;10:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Semba RD, Garrett E, Johnson BA, Guralnik JM, Fried LP. Vitamin D deficiency among older women with and without disability. Am J Clin Nutr. 2000;72:1529-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Moreira ML, Neto LV, Madeira M, Lopes RF, Farias MLF. Vitamin D Deficiency and Its Influence on Bone Metabolism and Density in a Brazilian Population of Healthy Men. J Clin Densitom. 2018;21:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Tu DP, Liu Z, Yu YK, Xu C, Shi XL. Internal Fixation versus Hemiarthroplasty in the Treatment of Unstable Intertrochanteric Fractures in the Elderly: A Systematic Review and Meta-Analysis. Orthop Surg. 2020;12:1053-1064. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Yang ZB, Wu PH, Wong PK, Huang ZY, Fu M, Liao WM, He AS, Kang Y. Better Prognosis of Senile Patients with Intertrochanteric Femoral Fracture by Treatment with Open Reduction Internal Fixation than by Hip Arthroplasty. J Invest Surg. 2018;31:431-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Kesmezacar H, Oğüt T, Bilgili MG, Gökay S, Tenekecioğlu Y. [Treatment of intertrochanteric femur fractures in elderly patients: internal fixation or hemiarthroplasty]. Acta Orthop Traumatol Turc. 2005;39:287-294. [PubMed] |
| 24. | Ju JB, Zhang PX, Jiang BG. Hip Replacement as Alternative to Intramedullary Nail in Elderly Patients with Unstable Intertrochanteric Fracture: A Systematic Review and Meta-Analysis. Orthop Surg. 2019;11:745-754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Authen AL, Dybvik E, Furnes O, Gjertsen JE. Surgeon's experience level and risk of reoperation after hip fracture surgery: an observational study on 30,945 patients in the Norwegian Hip Fracture Register 2011-2015. Acta Orthop. 2018;89:496-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 26. | Salpakoski A, Kallinen M, Kiviranta I, Alen M, Portegijs E, Jämsen E, Ylinen J, Rantanen T, Sipilä S. Type of surgery is associated with pain and walking difficulties among older people with previous hip fracture. Geriatr Gerontol Int. 2016;16:754-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Kuru T, Olçar HA. Effects of early mobilization and weight bearing on postoperative walking ability and pain in geriatric patients operated due to hip fracture: a retrospective analysis. Turk J Med Sci. 2020;50:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Iosifidis M, Iliopoulos E, Panagiotou A, Apostolidis K, Traios S, Giantsis G. Walking ability before and after a hip fracture in elderly predict greater long-term survivorship. J Orthop Sci. 2016;21:48-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |