Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9722
Peer-review started: February 16, 2021
First decision: May 4, 2021
Revised: May 7, 2021
Accepted: August 25, 2021
Article in press: August 25, 2021
Published online: November 16, 2021
Processing time: 266 Days and 13.8 Hours
Lateral internal sphincterotomy is still the approach of choice for the treatment of chronic anal fissure (CAF) with internal anal sphincter (IAS) hypertonia, but it is burdened by high-risk postoperative faecal incontinence (FI). Sphincter saving procedures have recently been reconsidered as treatments to overcome this risk. The most employed procedure is fissurectomy with anoplasty, eventually associated with pharmacological sphincterotomy.
To evaluate whether fissurectomy and anoplasty with botulinum toxin injection improves the results of fissurectomy and anoplasty alone.
We conducted a case-control study involving 30 male patients affected by CAF with hypertonic IAS who underwent fissurectomy and anoplasty with V-Y cutaneous flap advancement. The patients were divided into two groups: Those in group I underwent surgery alone, and those in group II underwent surgery and a botulinum toxin injection directly into the IAS. They were followed up for at least 2 years. The goals were to achieve complete healing of the patient and to assess the FI and recurrence rate along with manometry parameters.
The intensity and duration of post-defecatory pain decreased significantly in both groups of patients starting with the first defecation, and this reduction was higher in group II. Forty days after surgery, we achieved complete wound healing in all the patients in group II but only in 80% of the patients in group I (P < 0.032). We recorded 2 cases of recurrence, one in each group, and both healed with conservative therapy. We recorded one temporary and low-grade postoperative case of “de novo” FI. Manometry parameters reverted to the normal range earlier for group II patients.
The injection of botulinum toxin A in association with fissurectomy and anoplasty with a V-Y advancement flap improves the results of surgery alone in patients affected by CAF with IAS hypertonia.
Core Tip: Surgical sphincterotomy is still the approach of choice for the treatment of chronic anal fissure with internal anal sphincter hypertonia, even if it is burdened by a high risk of postoperative faecal incontinence. For this reason, sphincter-saving surgical procedures have recently been reconsidered to overcome this risk. In our work, we consider fissurectomy with anoplasty, and we wonder if the association with pharmacological sphincterotomy with botulinum toxin A injection may improve the outcomes in patients affected by chronic anal fissure with hypertonic internal anal sphincter. Therefore, this study aims to evaluate the results of the associated procedures in terms of reduction of faecal incontinence risk and recurrence rate and improvement of overall results in comparison with conventional sphincterotomy.
- Citation: D'Orazio B, Geraci G, Famà F, Terranova G, Di Vita G. Botulinum toxin associated with fissurectomy and anoplasty for hypertonic chronic anal fissure: A case-control study. World J Clin Cases 2021; 9(32): 9722-9730
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9722.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9722
Chronic anal fissures (CAFs), which are refractory to dietary, hygienic, and pharmacological therapy, require a surgical approach. A hypertonic internal anal sphincter (IAS) is associated with 40%-60% of CAFs[1-4]. To date, the role and genesis of the augmented IAS tone remains unknown; in fact, we wondered whether it is a cause or a consequence of CAF. During the last few decades, the treatment of this disease aimed to reduce IAS tone with medical and surgical approaches, and lateral internal sphincterotomy (LIS) currently represents the preferred approach.
This latter stands apart for its low rate of postoperative complications as well as its high rate of success, which reaches approximately 95%; furthermore, it allows a fast resolution of clinical symptoms since the first postoperative defecation, leading to complete healing within approximately 4-6 wk. Nevertheless, the greatest disadvantage of the abovementioned procedure is the high rate of faecal incontinence (FI) occurrence, which accounts for 30%-40% of cases. A meta-analysis from 2013 evaluated the long-term incidence of FI after LIS and showed an overall continence alteration risk of 14%[5].
Sphincter-saving procedures have been recently reconsidered as a valuable alternative to reduce the risk of FI in both children and adults[6]. Among the latter, fissurectomy and anoplasty with a V-Y advancement flap have been employed by our team for a few years, with outstanding results[1,7].
The aim of our study was to examine whether fissurectomy and anoplasty with botulinum toxin A (BT) injection improves the results of surgery alone in patients affected by CAF with IAS hypertonia. Therefore, we conducted a case-control study between two groups of patients who underwent fissurectomy and anoplasty with or without BT injection.
This case-control study involved 30 male patients, all affected by idiopathic and nonrecurrent CAFs with hypertonic IAS. Fifteen underwent fissurectomy and anoplasty from April 2018 until January 2019 (group I), and 15 underwent fissurectomy and anoplasty with BT injection from 2011 until 2015 (group II). The two groups were matched for demographic and clinical data (Table 1).
The exclusion criteria for the study were the presence of multiple fissures, fistulas in ano, syphilis, inflammatory bowel disease, anal abscess, malignant disease, and previous proctology surgery. All patients were followed up for at least 2 years after the surgical procedure. The patients’ outcome data were retrieved from a prospectively monitored database.
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol for this study was submitted to the Ethical Committee of our institution, which did not consider it necessary to approve. Written informed consent was obtained from all study participants.
Preoperative manometric evaluation was performed after a reasonable period of suspension of all medical therapies influencing IAS tone, and it was carried out by a manometric sensor using station pull-through as described in our previous work[7]. Then, we performed postoperative manometric evaluations at 12 and 24 mo.
Data collected on healthy subjects by our anorectal pathophysiological laboratory showed that normal values of maximum resting pressure (MRP) and maximum squeeze pressure (MSP) were 68.1 ± 12.3 mmHg and 112 ± 36.2 mmHg, respectively[7]. Ultraslow wave activity (USWA) was detected in only 10% of healthy patients. The normal range of MRP, according to Jones et al[8], was 45-85 mmHg; therefore, CAF without hypertonic IAS was defined as those with MRP values < 85 mmHg.
All patients underwent fissurectomy and anoplasty with V-Y skin flap advancement lying in a gynaecological position under spinal or general anaesthesia.
The sentinel skin tags, and hypertrophied anal papilla located at the dentate line were excised, if present; the tissue at the base of the fissure was curetted until clean IAS muscle fibres were reached. Technical details concerning the surgical procedure have already been widely explained in a previous work from our group[9,10].
Once fissurectomy was performed, patients in group II underwent a local injection of 30 UI of BT (Botox, Allergan Westport, Ireland)[11] directly into the IAS. Each patient received a total of 30 UI of BT: 15 UI injected at 3 h in gynaecological position and 15 UI injected at 9 h. None of the patients were taking concomitant oral medication that could interfere with the action of BT (e.g., aminoglycoside, baclofen, dantrolene, diazepam), and we did not register any case of hypersensitivity to any component of BT. Metronidazole was administered intravenously at a dose of 500 mg 1 h before surgery; subsequently, it was administered per os at a dosage of 250 mg three times a day for 7 d. During the first 2 weeks after the surgery, the patients took variable doses of psyllium fibres. A laxative preparation (sennosides) was admini
Complete healing was defined as complete epithelialization of the advancement skin flap. Recurrent CAFs were defined as those that occurred after the complete healing of the previous wound. Both the duration and intensity of post-defecatory pain were evaluated; the intensity was evaluated with a visual analogue scale.
FI was assessed preoperatively and 6, 12 and 24 months after surgery according to Pescatori’s grading system[12]: A incontinence for flatus and mucus; B for liquid stool; C for solid stool; 1 for occasional; 2 for weekly; and 3 for daily. Patients were discharged within 24 h after surgery; afterwards, they were examined until they healed completely, and they were also followed up until 24 months after the surgical procedure. Regardless of the scheduled appointments, patients were seen on request.
Continuous variables were expressed as the mean ± SD, qualitative data as absolute frequencies, and MRP values were also given as the median and range. Student’s t-test with Welch correction was used to analyse the differences in pain score and pain duration at each registration point. Values of P < 0.05 were considered statistically significant.
This study included 30 men. At the time of the surgical procedure, the median age of the patients was 35 years in group I and 29 years in group II (range 18-61). We did not report any significant differences between the two groups of patients regarding bowel function, preoperative FI, intensity and duration of post-defecation pain, IAS tone or USWA detection. Demographic data of the patients in the study and clinical features of CAFs are reported in Table 1.
We achieved complete wound healing within 40 d for all patients in group II and for 80% of those in group I (P < 0.032). All patients in group I reached complete healing within 50 d.
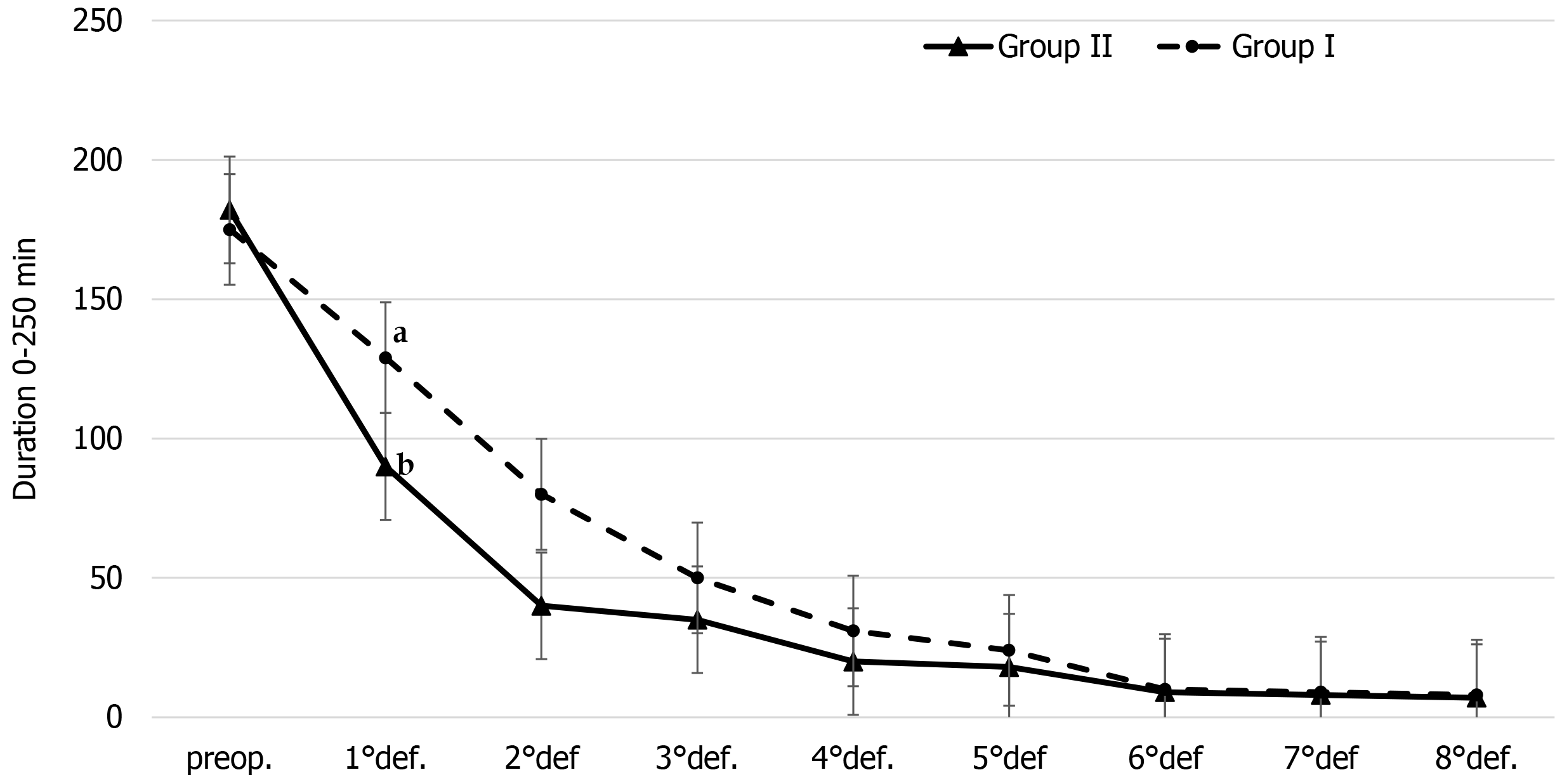
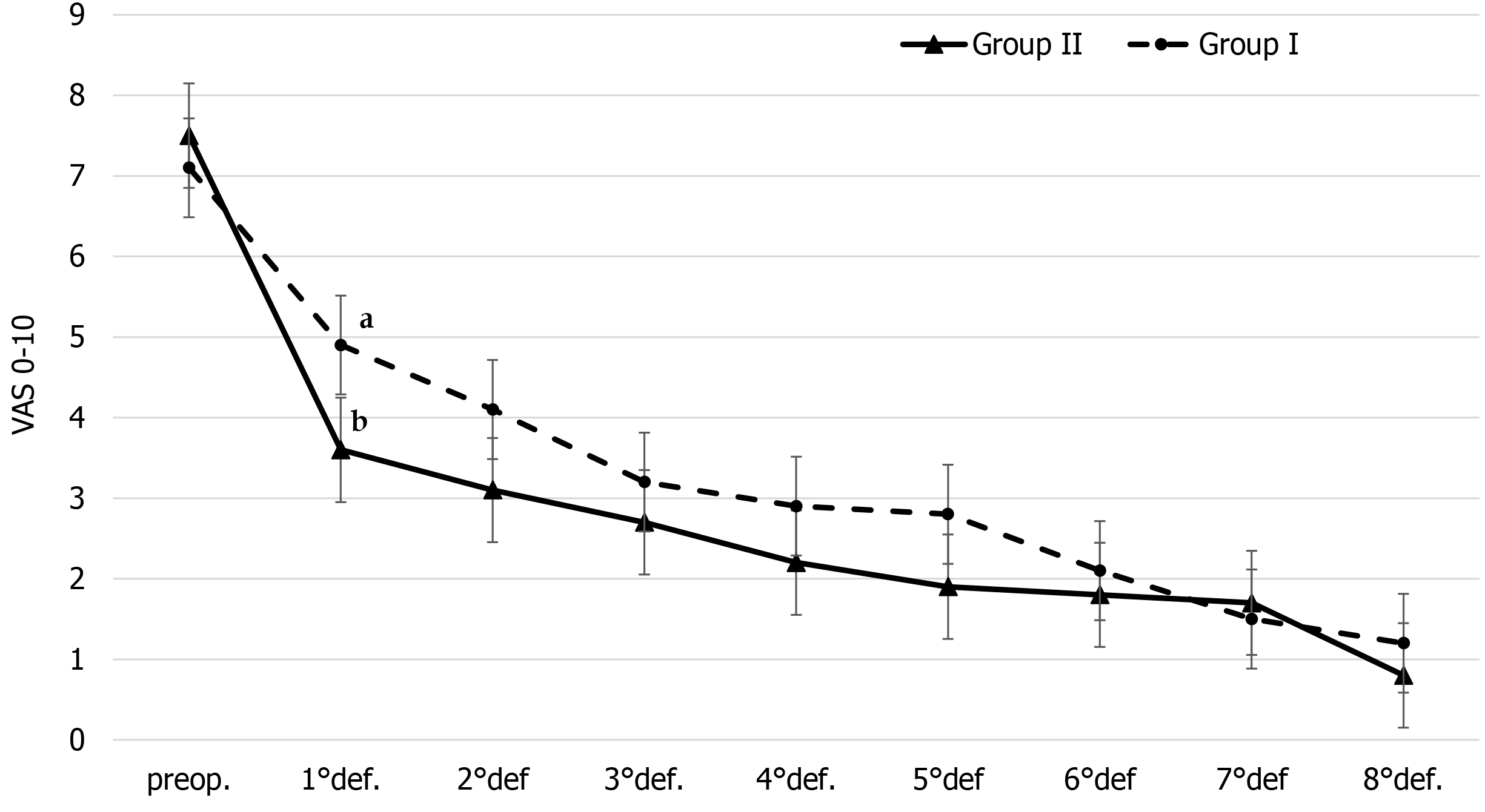
The intensity and duration of post-defecatory pain were significantly reduced in comparison to the preoperative values starting with the first postoperative defecation in both groups; they were greatly reduced in group II patients (P < 0.0001) (Figure 1), while we observed less reduction in both the intensity (P < 0.0095) and duration (P < 0.014 in group I) of pain in group I patients (Figure 2).
None of the patients complained about itching, bleeding, or pain 40 d after surgery. Analgesic consumption decreased significantly after the first defecation.
We recorded 2 cases of preoperative FI, one in each group of patients and both of grade A1 according to Pescatori’s grading system[12]. In group II, FI worsened 1 month after surgery, while at 3 months after the procedure, its grading was similar to that of the preoperative FI. We observed only 1 case of postoperative “de novo” FI in group II, which was temporary and of grade A1.
We observed only 2 cases of recurrence, one in each group of patients. The site of recurrence was different from the primary location; both occurred within 2 years of surgery and were characterized by the persistence of IAS hypertonia. Both patients underwent medical treatment consisting of implementation of fibre in the diet, employment of local products containing nifedipine or lidocaine and anal dilators. The patients responded to conservative therapy with complete healing.
Preoperative values of MRP were significantly higher than those of healthy subjects in both groups of patients (P < 0.001), while MSP values were only slightly increased (P = NS).
In both groups of patients, MSP values at 12 and 24 mo after surgery did not significantly differ from the preoperative values or those of healthy subjects. In group I patients, MRP values at 12 mo after surgery were significantly lower than the preoperative values (P < 0.02), while they were still increased compared with healthy subjects (P < 0.005). At 24 months after surgery, MRP values were similar to those of healthy subjects (P = NS).
In group II patients, MRP values at 12 months after surgery were significantly lower than the preoperative values (P < 0.001), while they were still increased compared to healthy subjects (P < 0.01). At 24 months after surgery, MRP values were similar to those of healthy subjects (P = NS). Preoperative detection of USWA in both groups was significantly higher than that in healthy subjects (P < 0.001). This value decreased significantly after 12 months and was within the normal range after 24 months.
There were no cases of urinary retention, anal stenosis or keyhole deformity. No necrosis of the transposed flap was reported. We did not observe any local complications related to the injection of the BT. The few postoperative complications recorded were of slight severity and in no case required further surgery; in particular, two infections were detected in the donor site, and a partial breakdown of the flap occurred in 1 case.
This study shows that the association of BT injection with fissurectomy and anoplasty improves the results compared with the surgery procedure alone. In fact, we observed a faster and greater reduction in both the intensity and duration of post-defecatory pain as well as a quicker healing of wounds and normalization of IAS tone in patients treated with BT injection. Regarding FI occurrence, we recorded a worsening of preoperative cases and 1 “de novo” postoperative case in group II.
The role of hypertonic IAS in the pathogenesis of this disease is still unclear. Various studies, both in vivo and with corpses[13,14], demonstrate that small arterial branches arising from the rectal artery pass through the IAS to ensure blood supply to the transition zone so that a hypertonic IAS might worsen the blood perfusion and prevent the healing process, leading to the genesis of CAF. However, hypertonic IAS is present only in 40%-60%[1-4] of CAFs, and as some research has indicated, the healing process takes place regardless of the IAS pressure. Pascual et al[3] showed that there were no significant differences concerning anal pressure, assessed with manometry or endoanal ultrasound, between healed and non-healed CAFs. Furthermore, surgical procedures, such as fissurectomy and anoplasty with flap advancement, lead to the resolution of CAF without interfering with the IAS tone, and even years after the procedure, we might record a normalization of IAS tone concurrently with CAF healing[15].
Considering the above findings, LIS should be reconsidered given the high incidence of FI resulting from the entity of the IAS section and, above all, considering that FI worsens naturally with ageing.
Fissurectomy is the most employed procedure to preserve the structural and functional integrity of the IAS. The fissurectomy itself produces wound debridement and removes the brady-trophic scar tissue, from which fresh wound edges and an acute fissure arise. This surgical procedure has been performed alone[16-18] or in association with pharmacological sphincterotomy to improve its outcome[19-25] and reduce its complications. After surgical fissurectomy, which may or may not be followed by chemical sphincterotomy, we observed complete second intention healing even after 10 weeks, with a rate of failure up to 34%. The rate of recurrence and healing failure of fissurectomy might be a consequence of the naked ischaemic area left at the wound site; therefore, the use of a flap to cover up this area is designed to relocate healthy and blood-supplied tissue coming from different arterial districts[26-36]. Another advantage of using a flap may be represented by the boosting effect on cutaneous circumference of the anal canal, which reduces the risk of splitting. Lastly, the employment of drugs enables the reduction of IAS tone and leads to an improvement in the blood supply of the naked area[37-39].
This study shows that the association of BT injection with a sphincter-saving procedure enables a temporary reduction of the IAS tone, improving the outcomes.
Lateral internal sphincterotomy is still the approach of choice for the treatment of chronic anal fissure (CAF) with internal anal sphincter (IAS) hypertonia, but it is burdened by high-risk postoperative faecal incontinence.
Sphincter-saving procedures have been recently reconsidered as treatments to overcome this risk.
The aim of our study was to evaluate whether fissurectomy and anoplasty with botulinum toxin injection improves the results of fissurectomy and anoplasty alone.
We conducted a case-control study involving 30 male patients affected by CAF with hypertonic IAS who underwent fissurectomy and anoplasty with V-Y cutaneous flap advancement. The patients were divided into two groups: Those in group I underwent surgery alone, and those in group II underwent surgery and a botulinum toxin injection directly into the IAS. They were followed up for at least 2 years.
The intensity and duration of post-defecatory pain decreased significantly in both groups of patients starting with the first defecation, and this reduction was higher in group II. Forty days after surgery, we achieved complete wound healing in all the patients in group II but only in 80% of the patients in group I (P < 0.032). We recorded 2 cases of recurrence, one in each group, and both healed with conservative therapy. We recorded one temporary and low-grade postoperative case of “de novo” faecal incontinence. Manometry parameters reverted earlier to the normal range in group II patients.
The injection of botulinum toxin A in association with fissurectomy and anoplasty with a V-Y advancement flap improves the results of surgery alone in patients affected by CAF with IAS hypertonia.
Further studies with larger samples of patients are necessary to ensure a greater foundation for our findings. The outcomes of this study might be considered a starting point to consider the sphincter-saving procedure, eventually associated with pharmacological sphincterotomy, as the treatment of choice for all patients affected by chronic anal fissure regardless of the internal anal sphincter tone.
We thank Prof. Piero Luigi Almasio from the University of Palermo (Promise Department) for his valuable contribution to the statistical analysis of this work.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsimogiannis K S-Editor: Yan JP L-Editor: Filipodia P-Editor: Li JH
| 1. | Patti R, Famà F, Barrera T, Migliore G, Di Vita G. Fissurectomy and anal advancement flap for anterior chronic anal fissure without hypertonia of the internal anal sphincter in females. Colorectal Dis. 2010;12:1127-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Bove A, Balzano A, Perrotti P, Antropoli C, Lombardi G, Pucciani F. Different anal pressure profiles in patients with anal fissure. Tech Coloproctol. 2004;8:151-6; discussion 156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Pascual M, Pera M, Courtier R, Gil MJ, Parés D, Puig S, Andreu M, Grande L. Endosonographic and manometric evaluation of internal anal sphincter in patients with chronic anal fissure and its correlation with clinical outcome after topical glyceryl trinitrate therapy. Int J Colorectal Dis. 2007;22:963-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Anaraki F, Foroughifar T, Laleh Hossein S, Etemad O. Evaluation of outcomes in fissurectomy and V-Y advancement flap for the treatment of chronic anal fissure. JCOL. 2018;38:132-136. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Garg P, Garg M, Menon GR. Long-term continence disturbance after lateral internal sphincterotomy for chronic anal fissure: a systematic review and meta-analysis. Colorectal Dis. 2013;15:e104-e117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 6. | Aigner F, Conrad F. Fissurectomy for treatment of chronic anal fissures. Dis Colon Rectum. 2008;51:1163; author reply 1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Patti R, Territo V, Aiello P, Angelo GL, Di Vita G. Manometric evaluation of internal anal sphincter after fissurectomy and anoplasty for chronic anal fissure: a prospective study. Am Surg. 2012;78:523-527. [PubMed] |
| 8. | Jones OM, Ramalingam T, Lindsey I, Cunningham C, George BD, Mortensen NJ. Digital rectal examination of sphincter pressures in chronic anal fissure is unreliable. Dis Colon Rectum. 2005;48:349-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | D'Orazio B, Geraci G, Famà F, Cudia B, Martorana G, Sciumé C, Corbo G, Terranova G, Bonventre S, Di Vita G. Long term outcomes of fissurectomy and anoplasty for chronic anterior anal fissure without hypertonia: low recurrences and continence conservation. Ann Ital Chir. 2020;9. [PubMed] |
| 10. | D’Orazio B, Geraci G, Sciumé C, Cudia B, Di Vita G. Surgical sphincter saving approach for chronic anal fissure without internal anal sphincter hypertonia: is it effective? Policlinico Sez. Med. 2020;127:1-00. [DOI] [Full Text] |
| 11. | D'Orazio B, Geraci G, Martorana G, Sciumé C, Corbo G, Di Vita G. Fisurectomy and anoplasty with botulinum toxin injection in patients with chronic anal posterior fissure with hypertonia: a long-term evaluation. Updates Surg. 2020;73:1575-1581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Pescatori M, Anastasio G, Bottini C, Mentasti A. New grading and scoring for anal incontinence. Evaluation of 335 patients. Dis Colon Rectum. 1992;35:482-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 223] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Klosterhalfen B, Vogel P, Rixen H, Mittermayer C. Topography of the inferior rectal artery: a possible cause of chronic, primary anal fissure. Dis Colon Rectum. 1989;32:43-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 144] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Schouten WR, Briel JW, Auwerda JJ. Relationship between anal pressure and anodermal blood flow. The vascular pathogenesis of anal fissures. Dis Colon Rectum. 1994;37:664-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 195] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Patti R, Guercio G, Territo V, Aiello P, Angelo GL, Di Vita G. Advancement flap in the management of chronic anal fissure: a prospective study. Updates Surg. 2012;64:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Schornagel IL, Witvliet M, Engel AF. Five-year results of fissurectomy for chronic anal fissure: low recurrence rate and minimal effect on continence. Colorectal Dis. 2012;14:997-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Zeitoun JD, Blanchard P, Fathallah N, Benfredj P, Lemarchand N, de Parades V. Long-term Outcome of a Fissurectomy: A Prospective Single-Arm Study of 50 Operations out of 349 Initial Patients. Ann Coloproctol. 2018;34:83-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Sileri P, Stolfi VM, Franceschilli L, Grande M, Di Giorgio A, D'Ugo S, Attina' G, D'Eletto M, Gaspari AL. Conservative and surgical treatment of chronic anal fissure: prospective longer term results. J Gastrointest Surg. 2010;14:773-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Witte ME, Klaase JM, Koop R. Fissurectomy combined with botulinum toxin A injection for medically resistant chronic anal fissures. Colorectal Dis. 2010;12:e163-e169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Baraza W, Boereboom C, Shorthouse A, Brown S. The long-term efficacy of fissurectomy and botulinum toxin injection for chronic anal fissure in females. Dis Colon Rectum. 2008;51:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Scholz T, Hetzer FH, Dindo D, Demartines N, Clavien PA, Hahnloser D. Long-term follow-up after combined fissurectomy and Botox injection for chronic anal fissures. Int J Colorectal Dis. 2007;22:1077-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Arthur JD, Makin CA, El-Sayed TY, Walsh CJ. A pilot comparative study of fissurectomy/diltiazem and fissurectomy/botulinum toxin in the treatment of chronic anal fissure. Tech Coloproctol. 2008;12:331-6; discussion 336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Engel AF, Eijsbouts QA, Balk AG. Fissurectomy and isosorbide dinitrate for chronic fissure in ano not responding to conservative treatment. Br J Surg. 2002;89:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Andicoechea Agorría A, Del Casar Lizcano JM, Barbón Remis E, Jara Quezada JH, Fernández Fernández JC, Sánchez Sánchez MDR, Quintela Baizán I, Vivoso Piñero F. Treatment of a chronic anal fissure with a botulin toxin A injection and fissurectomy. Rev Esp Enferm Dig. 2019;111:672-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Giordano P, Gravante G, Grondona P, Ruggiero B, Porrett T, Lunniss PJ. Simple cutaneous advancement flap anoplasty for resistant chronic anal fissure: a prospective study. World J Surg. 2009;33:1058-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Samson RB, Stewart WR. Sliding skin grafts in the treatment of anal fissures. Dis Colon Rectum. 1970;13:372-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Owen HA, Edwards DP, Khosraviani K, Phillips RK. The house advancement anoplasty for treatment of anal disorders. J R Army Med Corps. 2006;152:87-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Kenefick NJ, Gee AS, Durdey P. Treatment of resistant anal fissure with advancement anoplasty. Colorectal Dis. 2002;4:463-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Nyam DC, Wilson RG, Stewart KJ, Farouk R, Bartolo DC. Island advancement flaps in the management of anal fissures. Br J Surg. 1995;82:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 62] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Singh M, Sharma A, Gardiner A, Duthie GS. Early results of a rotational flap to treat chronic anal fissures. Int J Colorectal Dis. 2005;20:339-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Patel SD, Oxenham T, Praveen BV. Medium-term results of anal advancement flap compared with lateral sphincterotomy for the treatment of anal fissure. Int J Colorectal Dis. 2011;26:1211-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Hancke E, Suchan K, Völke K. Anokutaner Advancement-Flap zur sphinkterchonenden chirurgischen Therapie der chronischen Analfissur. Coloproctology. 2020;42:270-276. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Abramowitz L, Bouchard D, Souffran M, Devulder F, Ganansia R, Castinel A, Suduca JM, Soudan D, Varastet M, Staumont G; GREP: Groupe de Recherche En Proctologie de la Société Nationale Française de Colo‐Proctologie; CREGG: Club de Réflexion des cabinets et Groupe d’Hépato‐Gastroentérologie. Sphincter-sparing anal-fissure surgery: a 1-year prospective, observational, multicentre study of fissurectomy with anoplasty. Colorectal Dis. 2013;15:359-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Chambers W, Sajal R, Dixon A. V-Y advancement flap as first-line treatment for all chronic anal fissures. Int J Colorectal Dis. 2010;25:645-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Sobrado Júnior CW, Hora JAB, Sobrado LF, Guzela VR, Nahas SC, Cecconello I. Anoplasty with skin tag flap for the treatment of chronic anal fissure. Rev Col Bras Cir. 2019;46:e20192181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Sahebally SM, Walsh SR, Mahmood W, Aherne TM, Joyce MR. Anal advancement flap vs lateral internal sphincterotomy for chronic anal fissure- a systematic review and meta-analysis. Int J Surg. 2018;49:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 37. | D'Orazio B, Sciumé C, Famà F, Bonventre S, Martorana G, Corbo G, Calí D, Terranova G, Vita GD, Geraci G. Surgical Sphincter Saving Approach and Topical Nifedipine for Chronic Anal Fissure with Hypertonic Internal Anal Sphincter. Chirurgia (Bucur). 2020;115:585-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Patti R, Famà F, Tornambè A, Asaro G, Di Vita G. Fissurectomy combined with anoplasty and injection of botulinum toxin in treatment of anterior chronic anal fissure with hypertonia of internal anal sphincter: a pilot study. Tech Coloproctol. 2010;14:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 39. | Pinto-Lopes R, Thahir A, Halahakoon VC. An Analysis of the Decision-Making Process After "Decision not to Operate" in Acutely Unwell, High-Risk General Surgery Patients. Am J Hosp Palliat Care. 2020;37:632-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |