Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9174
Peer-review started: April 13, 2021
First decision: June 24, 2021
Revised: July 9, 2021
Accepted: September 10, 2021
Article in press: September 10, 2021
Published online: October 26, 2021
Processing time: 190 Days and 16.4 Hours
Choriocarcinoma is a subtype of gestational trophoblastic disease, gestational trophoblastic neoplasia. Patients with brain metastasis are rare and information on the optimal treatment and patient outcome is limited. In order to improve the prognosis of this disease, accurate and timely treatments are very important for the patient of brain metastasis by choriocarcinoma.
A 17-year-old unmarried girl was misdiagnosed with a cerebral hemangioma with intracranial hemorrhage in a local hospital after presentation with severe head pain. She underwent craniotomy three times for treatment. The pathological results of posterior intracranial hematoma showed choriocarcinoma, and the patient was diagnosed as choriocarcinoma (21 points in stage IV). After uterine artery embolization, etoposide, methotrexate, actinomycin D, cyclophosphamide, and vincristine chemotherapy for 7 cycles, and whole brain radiotherapy, the patient achieved remission. She has been followed for 2 years with no signs of tumor recurrence.
For female patients of childbearing age with an intracranial hematoma, the possibility of brain metastasis by choriocarcinoma should be considered. It is necessary to obtain a detailed history, including menstruation, beginning age of first sex, contraception, etc. The level of β-human chorionic gonadotropin should be tested at the beginning, and a stratified treatment should be administered according to the International Federation of Gynecology and Obstetrics staging and World Health Organization prognostic scoring systems.
Core Tip: A 17-year-old unmarried girl was misdiagnosed with a cerebral hemangioma with intracranial hemorrhage in a local hospital after presentation with severe head pain. The patient was treated with craniotomy three times. The pathological results of posterior intracranial hematoma showed choriocarcinoma, and the patient was diagnosed as choriocarcinoma (21 points in stage IV). For female patients of childbearing age with an intracranial hematoma, the possibility of brain metastasis by choriocarcinoma should be considered. It is necessary to obtain a detailed sexual history, include menstruation, beginning age of first sex, contraception, etc. The level of β-human chorionic gonadotropin should be tested at the beginning, and a stratified treatment should be administered according to the International Federation of Gynecology and Obstetrics staging and World Health Organization prognostic scoring systems.
- Citation: Huang HQ, Gong FM, Yin RT, Lin XJ. Choriocarcinoma misdiagnosed as cerebral hemangioma: A case report . World J Clin Cases 2021; 9(30): 9174-9181
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9174.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9174
Gestational trophoblastic neoplasia (GTN) is a group of malignant tumors characterized by abnormal growth of trophoblastic tissue, which can occur after a molar or non-molar pregnancy. Choriocarcinoma, a subtype of gestational trophoblastic disease first described in 400 BC by Hippocrates, is a rare and aggressive neoplasm[1] that can easily metastasize via the hematogenous pathway to multiple organs, such as uterus, vagina, lung, kidney, brain, liver, etc.[2]. GTN patients with brain metastasis are rare and information on the optimal treatment and patient outcome is limited[3]. However, since this type of tumor shows a high cure rate, early diagnosis and subsequent treatment are important. In this report, we present a rare case of choriocarcinoma with brain metastasis in a 17-year-old girl with intracerebral hemorrhage at initial presentation, which may provide a clinical references for aiding in diagnosing and treating brain metastases of choriocarcinoma, especially in adolescent women.
A 17-year-old girl with no disease history initially presented to a local community hospital for the acute onset of intense cephalagia, emesis, and left hemiplegia with normal mental state with bilateral pupils equal and reacting.
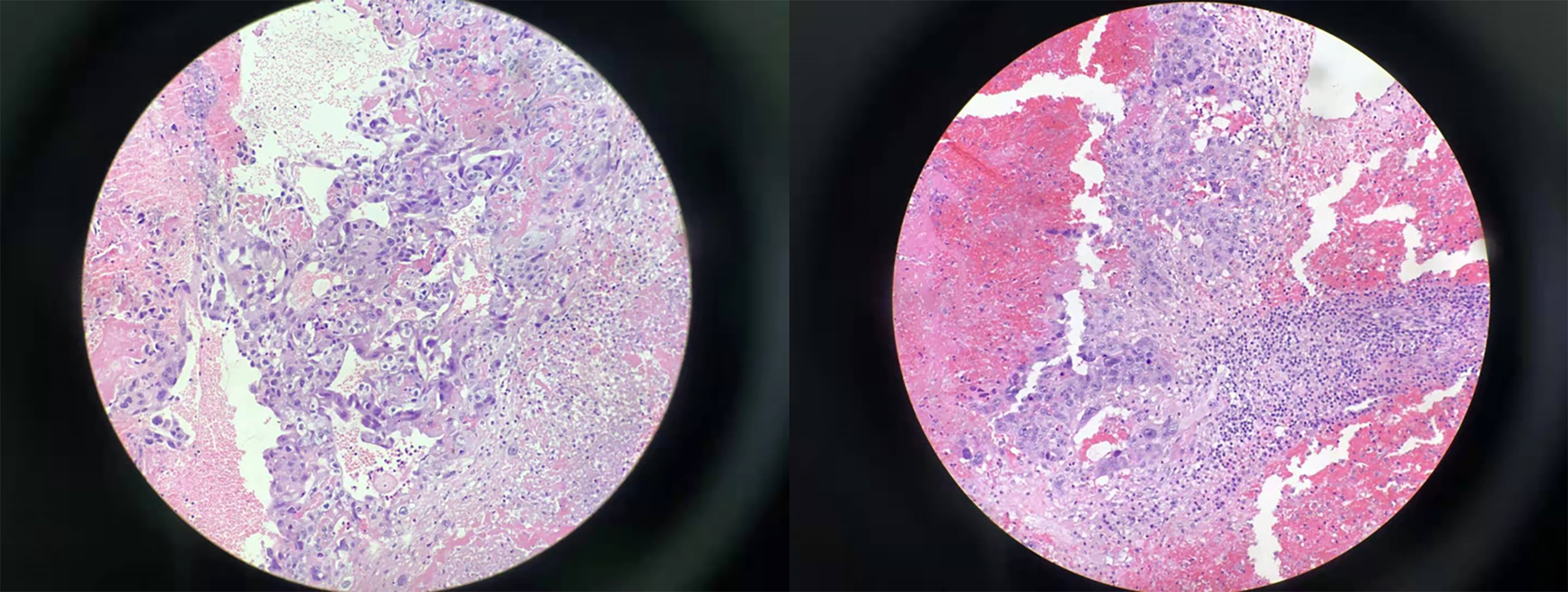
Computed tomography (CT) scan of the brain showed the right frontal parietal lobe intracerebral hemorrhage of the patient at the local hospital, and the patient underwent evacuation of hematoma by emergency craniotomy. Nine days after the first surgery, the patient complaint of severe headache, accompanied by jet vomiting, and the vomit was gastric contents. The patient underwent another evacuation of hematoma by craniotomy. Five days after the second operation, a third attack of headache and vomiting began, and the patient underwent the third evacuation of hematoma by craniotomy to control the hemorrhage. Postoperative pathological examination showed foam-like histiocyte proliferation, and tumor cells were found in the hemorrhagic and necrotic tissues (Figure 1). Immunohistochemical results: pan-cytokeratin (+), epithelial membrane antigen (+), human chorionic gonadotropin (HCG) (+), granulocyte chemotactic protein-3 (+, focal area), Sal-like protein 4 (+), octamer binding transcription factor 3/4 (-), and placental alkaline phosphatase (-), supporting metastatic choriocarcinoma. After confrontation, the patient admitted to having a sexual history and having had an abortion 2 years ago. She hid her medical history for fear that her parents would find out. Laboratory findings revealed that serum β-HCG level was more than 200000 U/mL. Based on all these findings, choriocarcinoma was strongly indicated. She received mannitol dehydration and brain protective treatment, and was then transferred to a general hospital for further treatment, at which time she was transferred to our center.
The patient’s menstrual cycle was regular and she declared no history of sexual intercourse or abortion. No history of hypertension could be identified.
No personal and family history available.
On presentation in our hospital, the patient was in a normal mental state with bilateral pupils equal and reacting. The muscle strength of left limb was grade III, the right limb grade V. The physical examination showed there was a bluish violet nodule with a diameter of about 6 cm at the cervix.
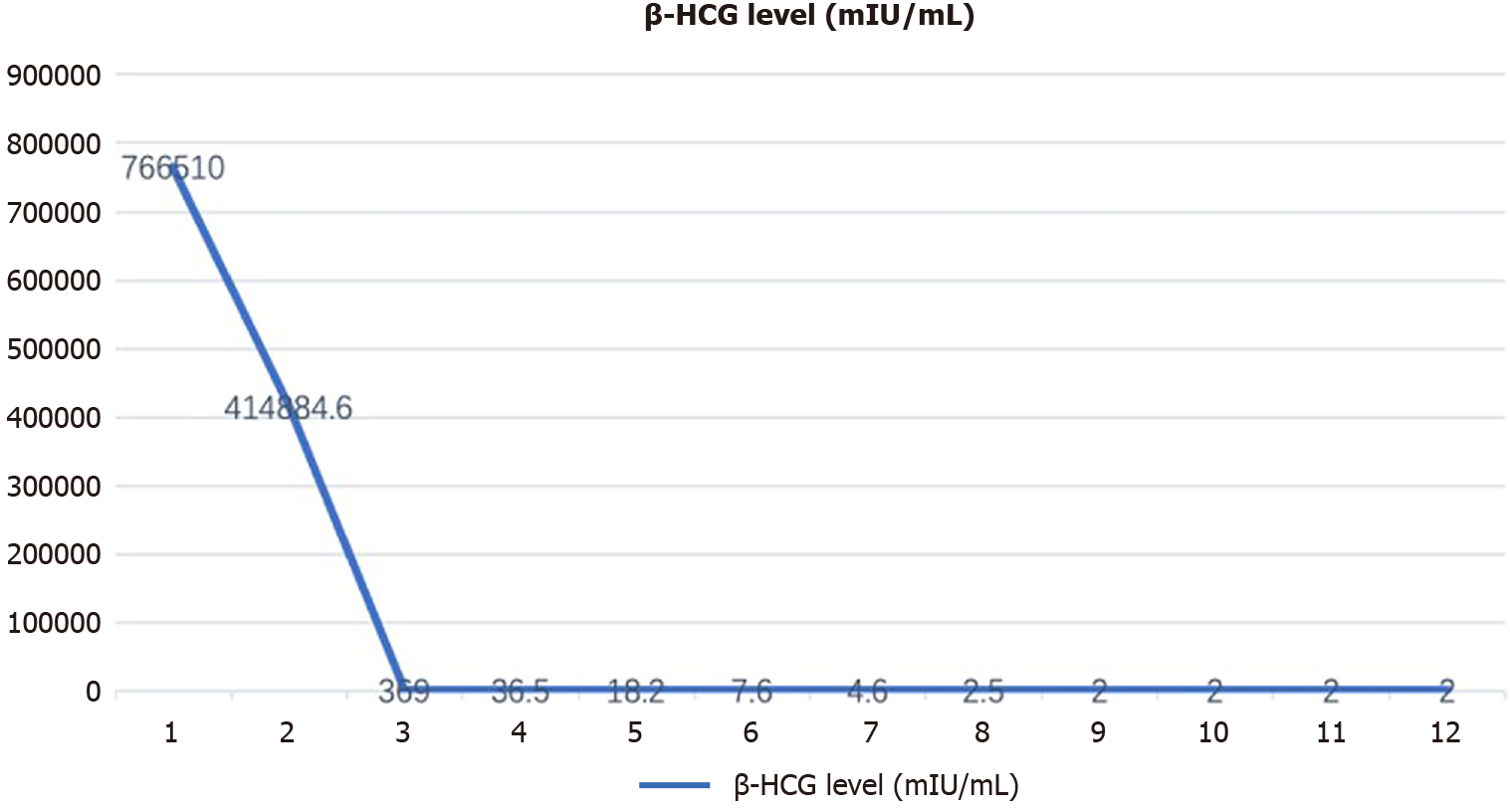
The blood level of β-HCG was 766510.0 mIU/mL (normal value, < 2.0 mIU/mL).
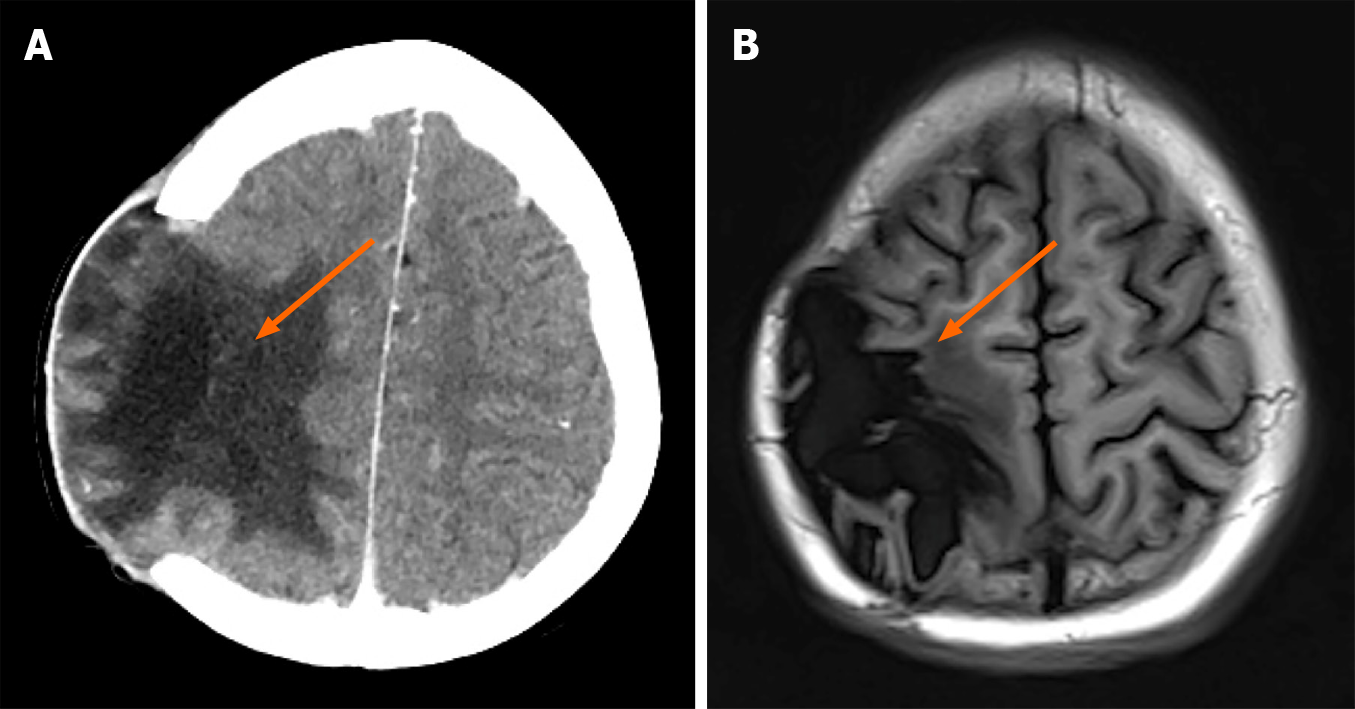
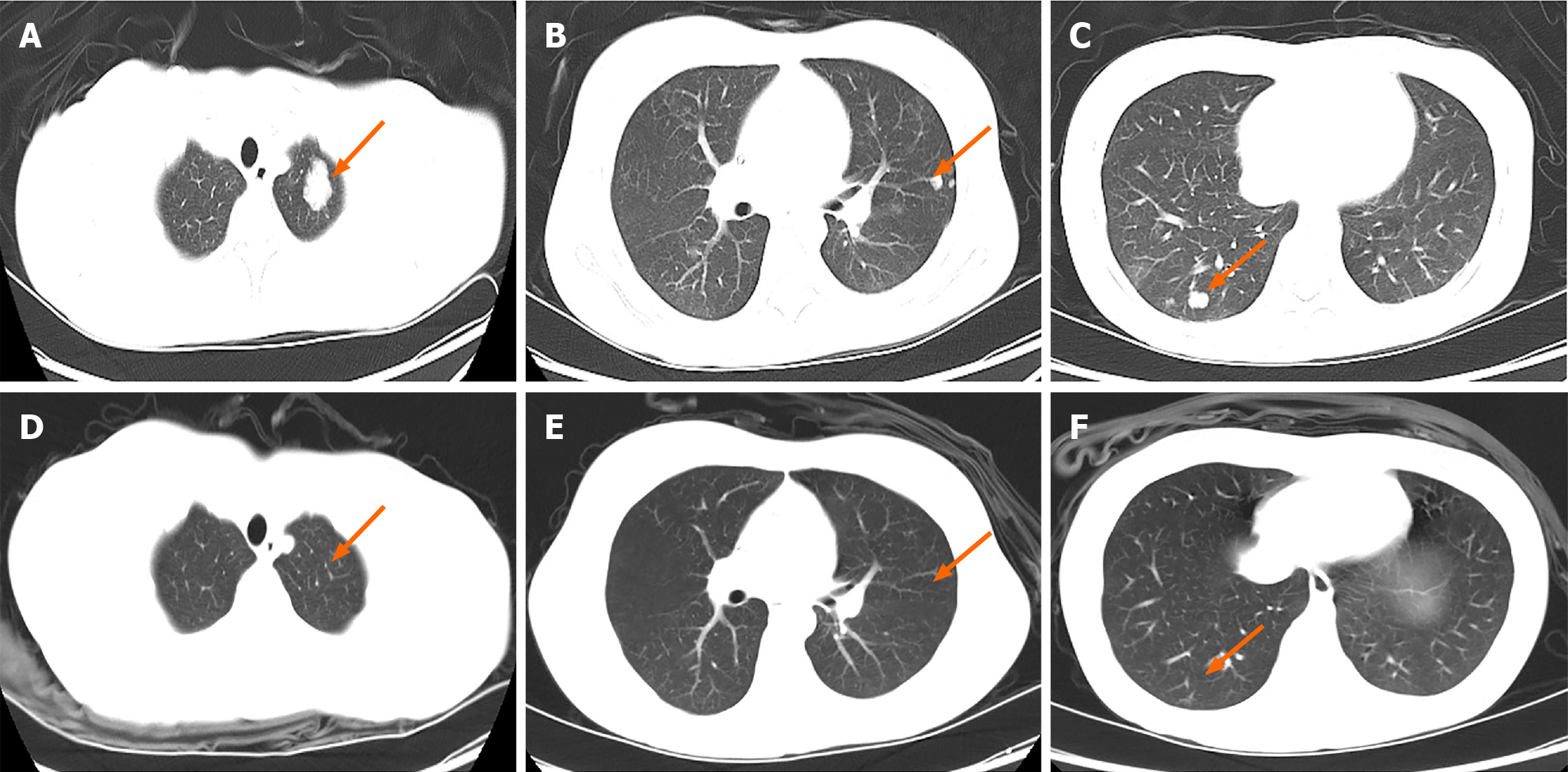
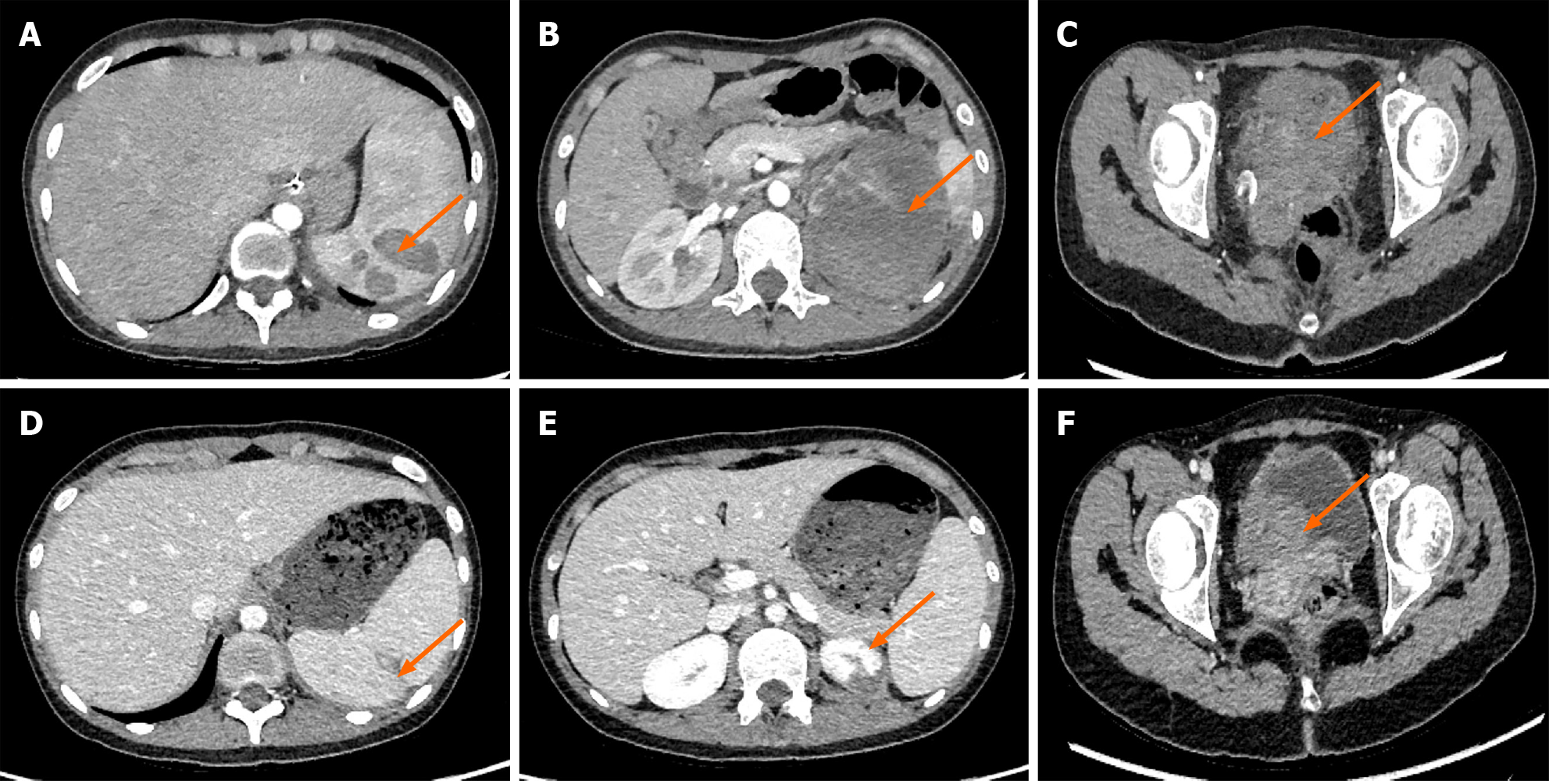
Brain CT with contrast enhancement showed the right parietal lobe in the area of the previous operations had obvious edema, and local softening foci were formed. The adjacent meninges and brain were swollen, indicating residual tumor at the surgical area. Chest CT showed multiple round nodules and masses of variable sizes in both lungs, with scanty amounts of right pleural effusion, compatible with lung metastasis. Abdomen CT showed an abnormal, high and low mixed density in the spleen and kidneys, and the cervical was enlarged with uneven and enhancement CT value.
On the basis of clinical and laboratory investigations, the patient was diagnosed with choriocarcinoma, International Federation of Gynecology and Obstetrics (FIGO) stage IV and score of the Prognostic Scoring Index modified by the FIGO score was 21 (extreme high risk).
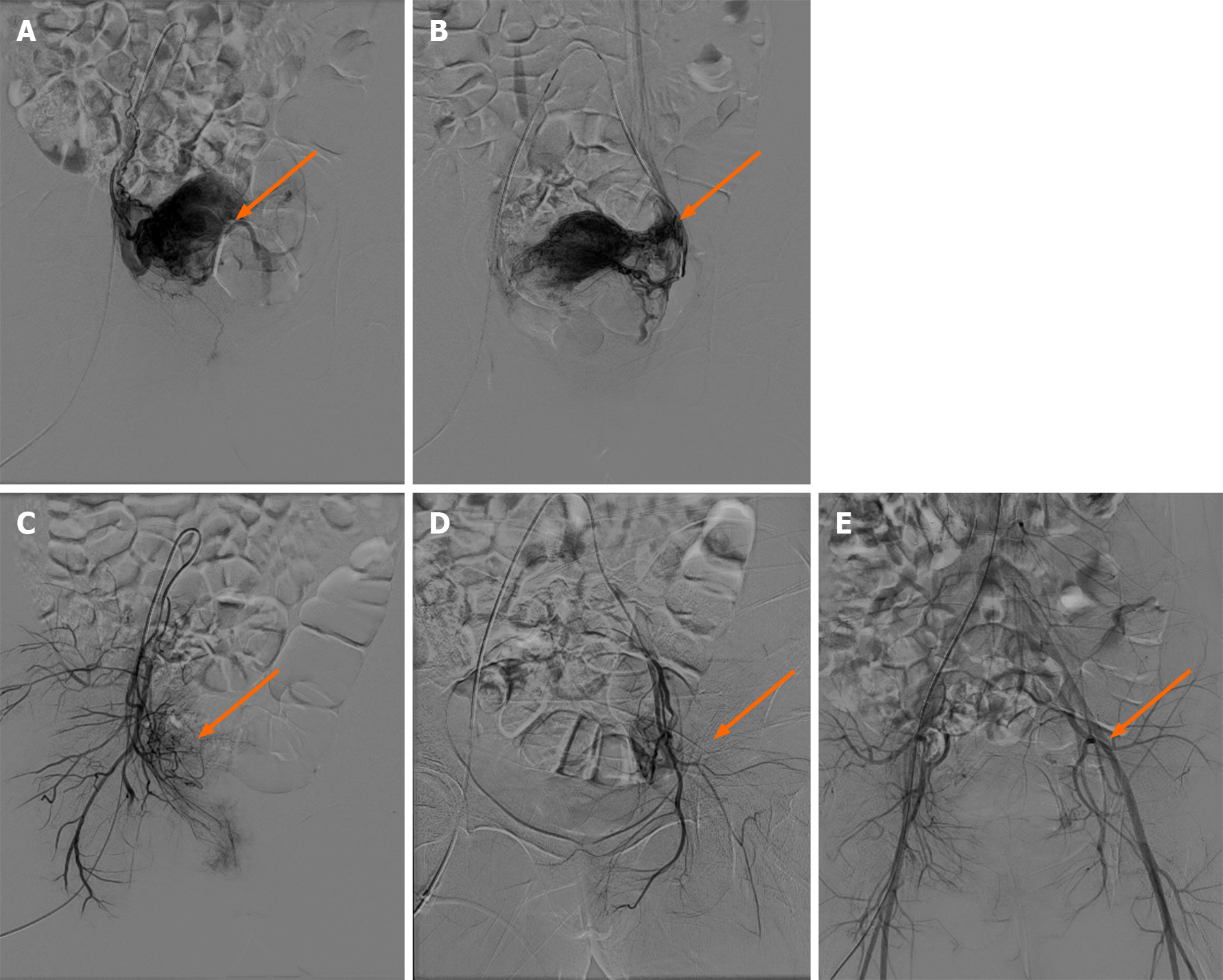
The patient underwent a multidisciplinary approach to treatment which consisted of a modified multi-agent chemotherapy regimen of etoposide, methotrexate, actinomycin D, cyclophosphamide and vincristine (EMA-CO) with higher doses of methotrexate. The regimen was as follows: methotrexate 100 mg/m2, followed by methotrexate 200 mg/m2 over 12 h day 1, etoposide 100 mg/m2 and dactinomycin 0.5 mg days 1 and 2, calcium folate 15 mg intramuscular injection every 12 h days 2 and 3, alternating with cyclophosphamide 600 mg/m2 and vincristine 2 mg day 8, every 14 days. During the first chemotherapy regimen, the patient suddenly had vaginal bleeding. Physical examination found a large amount of blood in the vagina and the bluish violet nodule on the cervix had ruptured. After vaginal gauze packing, there was still active bleeding. Uterine artery embolization was performed to selectively embolize the bleeding vessel and successfully control uterine hemorrhage (Figure 2). The patient underwent a blood transfusion to compensate for blood loss. Because of the brain metastasis and indications of residual tumor at the brain operation area, the patient underwent whole-brain radiotherapy with 50 Gy in 25 fractions. Usually patients with lung metastasis or disease in the pulmonary vasculature might have a combination of hemoptysis, shortness of breath, or pleuritic chest pain; however, the patient fortunately had no sign of those symptoms, and after the treatments, the lung CT showed favorable therapeutic response.
Serumβ-HCG decreased logarithmically to normal levels after the 7th chemotherapy regimen (Figure 3). The patient then completed 4 consolidation courses of chemotherapy. The results of lung CT, brain magnetic resonance imaging (MRI), and chest radiograph after treatments all showed favorable therapeutic response (Figures 4, 5 and 6). However, the patient still experienced alopecia, I° liver dysfunction, I-II° canker sore, I-II° nausea and vomiting, and II° granulocytopenia.
Long-term follow-up with evaluation of serum β-HCG levels every 3 mo and CT of her chest and MRI of her brain every 6 mo showed no evidence of disease. The patient has been followed up for 14 mo at the outpatient clinic. She complained of no self-conscious discomfort and the β-HCG value has been maintained in the normal range. The muscle strength of her limbs was almost normal. The patient consented to publication of the case.
Metastatic brain tumors are not frequently the cause of the intracerebral hemorrhage in the young, which is usually caused by arteriovenous malformations and aneurysms. About 10%-20% of brain metastases cases are found in choriocarcinoma, which most often manifests as an intracerebral or subdural hematoma because of the innate capacity of trophoblastic cells to invade vessel walls[4].
The pathological mechanism of choriocarcinoma metastasis to the brain is still controversial, and the formation mechanism may have the following points: (1) Vascular injury mechanism: microthrombotic injury of blood vessels, vascular endothelial scar formation, resulting in changes in vascular hydrodynamics, and hematoma formation[5]; (2) After the destruction of arterial blood vessels, tumor cells invade cerebral blood vessels through vascular nutrient tubes. However, vascular trophoblast tubes in experimental animals and humans are rare[6]; and (3) Tumor crossing mechanism: tumor cells have the ability to bind closely with endothelial cells at the terminal deposition site, and even destroy endothelial cells. With the growth of endothelial cells, they eventually cross and destroy arterial blood vessels[7]. No matter which of the three mechanisms mentioned above, microthrombosis is the earliest. More scholars now agree with the theory of tumor traversing mechanism because histopathologists have found that tumor cells proliferate in hemangioma cells and invaded the inner elastic membrane in various tumors. In conclusion, the biological characteristics of brain metastatic tumor cells play a very important role in the formation of brain metastatic hemangioma.
The strategy to treat patients who have GTN and brain metastases is with intravenous multidrug chemotherapy; however, the 2013 Cochrane review could not come to a conclusion on what the most effective multidrug chemotherapy regime was to treat high-risk GTN. The EMA-CO combination is most commonly used with an increased dose of Methotrexate from 300 to 1000 mg/m2 in the case of brain metastases (EMA-CO CNS), as recommended by the FTDRC[8]. According to our center's data on previous cases of GTN with brain metastasis, increasing the methotrexate (MTX) dose to 1.0 g/m2 results in unbearable side effects in patients. Patients who are administered low-dose 5-FU and actinomycin D chemotherapy with intermittent intrathecal MTX (15 mg) injection (2–3 times per cycle) until β-HCG is absent in the cerebrospinal fluid, with or without radiotherapy based on the efficacy of chemotherapy, have a remission rate of 75%[9,10]. These patients experience fewer side effects and can tolerate chemotherapy. The patient in this report received EMA-CO combination with usual dose of Methotrexate chemotherapy and showed a good prognosis. Reported by Soper et al[11], treating brain metastases from choriocarcinoma by using systemic intravenous chemotherapy (although alternative regimens to EMA-CO) with surgery or stereotactic brain radiation without the need for whole brain radiation and intrathecal chemotherapy is successful. HCG is key to effective management of gestational trophoblastic disease as the choriocarcinomas are malignant HCG-producing epithelial tumors. HCG is comprised of an α subunit and a β subunit that confers specificity. β-HCG is a good predictive indicator of prognosis and recurrence[12]. However, apart from clinical and radiological signs, the key diagnostic feature of choriocarcinoma is an elevated serum β-HCG. Elevation of β-HCG in the serum of a patient with a history of normal or abnormal pregnancy suggests the diagnosis of choriocarcinoma[12].
Because of the characteristics of trophoblast cell growth, it is easy for choriocarcinoma lesions to hemorrhage throughout the therapy. In this case, the patient presented with hemorrhages at both the cervix and the brain. Conservative treatment for choriocarcinoma hemorrhagic lesions should first be considered due to chemosensitivity. Arterial embolization has also proven to be an effective nonsurgical way to treat acute and massive genital bleeding in gestational trophoblastic disease, providing specific occlusion of the uterine vessels. Transcatheter angiographic embolization is an accepted treatment modality to control recurrent massive genital bleeding and can avoiding of hysterectomy and preserve fertility[13].
The literature advises that early diagnosis and treatment can significantly improve the prognosis of this disease[14]. In this case brain metastases were already present at time of diagnosis, which worsened the long-term prognosis of the choriocarcinoma. This highlights the importance of increasing awareness of the disease on the part of general practitioners, midwives, and emergency medicine staff, as they are most likely to receive the first presentations of patients with choriocarcinoma, and this will to ensure timely diagnosis and will improve prognosis and reduce morbidity[15]. Because of the Chinese traditional dichotomy, Chinese parents do not allow their daughters to have premarital sex, and therefore, adolescent girls often hide their sexual life history, and doctors in China always ignore their intercourse history. Therefore, there are no reliable data on the age of sexual debut in Chinese women, and the proportion of young women aged 15-19 years who had experienced sexual activity with a partner ranged from 4.5% among rural respondents to 10.8% among urban respondents[16]. In women at childbearing age, metastatic choriocarcinoma must be considered in the differential diagnosis of intracerebral hemorrhage because of its multiple clinical and radiological presentations. It is difficult to differentiate the imaging appearances from those due to cerebrovascular disease[17].
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jeong KY, Schulten HJ S-Editor: Wang JL L-Editor: Filipodia P-Editor: Li X
| 1. | Seckl MJ, Fisher RA, Salerno G, Rees H, Paradinas FJ, Foskett M, Newlands ES. Choriocarcinoma and partial hydatidiform moles. Lancet. 2000;356:36-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 203] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 2. | Bonnet L, Raposo N, Blot-Souletie N, Faruch Bilfeld M, Chollet F, Mazière J, Olivot JM, Albucher JF. Stroke Caused by a Pulmonary Vein Thrombosis Revealing a Metastatic Choriocarcinoma. Circulation. 2015;131:2093-2094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Piura E, Piura B. Brain metastases from gestational trophoblastic neoplasia: review of pertinent literature. Eur J Gynaecol Oncol. 2014;35:359-367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Savage P, Kelpanides I, Tuthill M, Short D, Seckl MJ. Brain metastases in gestational trophoblast neoplasia: an update on incidence, management and outcome. Gynecol Oncol. 2015;137:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Ashalatha R, Moosa A, Gupta AK, Krishna Manohar SR, Sandhyamani S. Cerebral aneurysms in atrial myxoma: a delayed, rare manifestation. Neurol India. 2005;53:216-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Sedat J, Chau Y, Dunac A, Gomez N, Suissa L, Mahagne MH. Multiple cerebral aneurysms caused by cardiac myxoma. A case report and present state of knowledge. Interv Neuroradiol. 2007;13:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Radoi MP, Stefanescu F, Arsene D. Brain metastases and multiple cerebral aneurysms from cardiac myxoma: case report and review of the literature. Br J Neurosurg. 2012;26:893-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Deng L, Zhang J, Wu T, Lawrie TA. Combination chemotherapy for primary treatment of high-risk gestational trophoblastic tumour. Cochrane Database Syst Rev. 2013;CD005196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Song L, Li Q, Yin R, Wang D. Choriocarcinoma with brain metastasis after term pregnancy: A case report. Medicine (Baltimore). 2018;97:e12904. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Hiramatsu Y, Masuyama H, Ishida M, Murakami K, Sakurai M. Term delivery choriocarcinoma patient with brain and lung metastases successfully treated by etoposide, methotrexate, actomycin D, cyclophosphamide and vincristine (EMA-CO) chemotherapy. Acta Med Okayama. 2005;59:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Soper JT, Spillman M, Sampson JH, Kirkpatrick JP, Wolf JK, Clarke-Pearson DL. High-risk gestational trophoblastic neoplasia with brain metastases: individualized multidisciplinary therapy in the management of four patients. Gynecol Oncol. 2007;104:691-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Ngan HYS, Seckl MJ, Berkowitz RS, Xiang Y, Golfier F, Sekharan PK, Lurain JR, Massuger L. Update on the diagnosis and management of gestational trophoblastic disease. Int J Gynaecol Obstet. 2018;143 Suppl 2:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 236] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 13. | Frati A, Ducarme G, Wernet A, Chuttur A, Vilgrain V, Luton D. Uterine artery embolization as treatment for life-threatening haemorrhage from a cervical choriocarcinoma: a case report. Eur J Obstet Gynecol Reprod Biol. 2008;141:87-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Wreczycka-Cegielny P, Cegielny T, Oplawski M, Sawicki W, Kojs Z. Current treatment options for advanced choriocarcinoma on the basis of own case and review of the literature. Ginekol Pol. 2018;89:711-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Ma Y, Xiang Y, Wan XR, Chen Y, Feng FZ, Lei CZ, Yang XY. The prognostic analysis of 123 postpartum choriocarcinoma cases. Int J Gynecol Cancer. 2008;18:1097-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Zhao FH, Tiggelaar SM, Hu SY, Xu LN, Hong Y, Niyazi M, Gao XH, Ju LR, Zhang LQ, Feng XX, Duan XZ, Song XL, Wang J, Yang Y, Li CQ, Liu JH, Lu YB, Li L, Zhou Q, Liu JF, Zhao N, Schmidt JE, Qiao YL. A multi-center survey of age of sexual debut and sexual behavior in Chinese women: suggestions for optimal age of human papillomavirus vaccination in China. Cancer Epidemiol. 2012;36:384-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 17. | Lappin JM, Darke S, Duflou J, Kaye S, Farrell M. Fatal Stroke in Pregnancy and the Puerperium. Stroke. 2018;49:3050-3053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |