Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9122
Peer-review started: March 19, 2021
First decision: July 26, 2021
Revised: July 30, 2021
Accepted: September 16, 2021
Article in press: September 16, 2021
Published online: October 26, 2021
Processing time: 215 Days and 19.5 Hours
Accessory and cavitated uterine mass (ACUM) is an uncommon form of connate Müllerian anomaly seen in young and nulliparous women, which presents as chronic periodic pelvic pain and severe dysmenorrhea. The entity is often underdiagnosed due to a broad differential diagnosis, including rudimentary uterine horn, true cavitated adenomyosis and degenerating fibroids.
A 22-year-old woman who presented with severe dysmenorrhea and was initially misdiagnosed with cystic adenomyosis. Gynecological examination and ultrasonography were performed. The patient underwent laparoscopic excision of the mass and histopathological examination confirmed the diagnosis. Postoperatively, the patient did well, with no further dysmenorrhea.
ACUM is difficult to diagnose. A correct diagnosis can be made only after excision and histopathological evaluation. Surgical excision is necessary and can be carried out by laparoscopy.
Core Tip: We present a case of accessory cavitated uterine mass (ACUM) treated with laparoscopic excision. The patient had no further dysmenorrhea after operation. ACUMs are generally underdiagnosed and often reported as juvenile cystic adenomyomas. Early surgical treatment including laparoscopic or open lump removal could prevent prolonged suffering in these young women. ACUM is considered a new variety of Müllerian anomaly.
- Citation: Hu YL, Wang A, Chen J. Diagnosis and laparoscopic excision of accessory cavitated uterine mass in a young woman: A case report. World J Clin Cases 2021; 9(30): 9122-9128
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9122.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9122
An accessory cavitated uterine mass (ACUM) was first reported in 1998 by Potter and Schenken[1], and is a uncommon variety of uterine lesions, found in young women, which is a non-communicating, accessory cavity with normal endometrium located in the uterus of normal shape and function. This uterine anomaly is categorized as U6 (“still unclassified”) in the ESHRE/ESGE classification, which is related to female gubernaculums dysfunction[2,3]. A recent study revealed that most cases of non-communicating accessory uterine cavities and juvenile, or isolated, cystic adeno
The criteria used to diagnose an ACUM are as follow: isolated cyst-like mass; normal uterine cavity, tubes and ovaries; exeresis of the mass with a pathology assessment; accessory cavity bordered by endometrial epithelium with glands and stroma; chocolate-brown-colored liquid content; and no adenomyosis (if hysterectomy has been performed), but there may be small foci in myometrium near the mass[4].
ACUMs are commonly underdiagnosed because of the extensive differential diagnosis, including other uterine malformations, cavitated adenomyosis, cystic adenomyosis and primary dysmenorrhea. Ultrasonography, magnetic resonance imaging (MRI) and hysterosalpingography are conducive to the diagnosis so as to quickly choose the best management strategy[6-8].
Here, we present a patient with ACUM diagnosed using the recommended ACUM criteria[4,5]. This patient was a 22 years old woman who suffered from recurrent pelvic pain after menses and was initially misdiagnosed as a left adnexa mass. Laparoscopic excision of the ACUM was performed in the patient.
A 22-year-old single woman had a history of periodic pain in the left lower abdomen after menses for more than a year, accompanied by a small amount of irregular vaginal bleeding lasting for approximately one week.
During the preceding months, the pain (in the left lower abdomen) had worsened and sometimes necessitated the use of non-steroidal anti-inflammatory drugs (NSAIDs). Transvaginal ultrasonography (TVU) showed a left adnexal cystic-solid mass, which was considered to be an inflammatory lesion. Following anti-inflammatory therapy and symptomatic treatment, the mass did not decrease. Thus, the patient was transferred to our hospital for further management.
The patient denied the history of gynecologic disease and operation. She had attained menarche at 12 years of age and had not experienced dysmenorrhea. Her menstrual pattern was normal.
The patient and her family had no history of gynecologic and other diseases.
Gynecological examination showed that the uterus was enlarged, and a mass of approximately 4cm in diameter was palpable on the left side of the uterus.
Laboratory examinations, including the serum tumor markers, were all within normal limits.
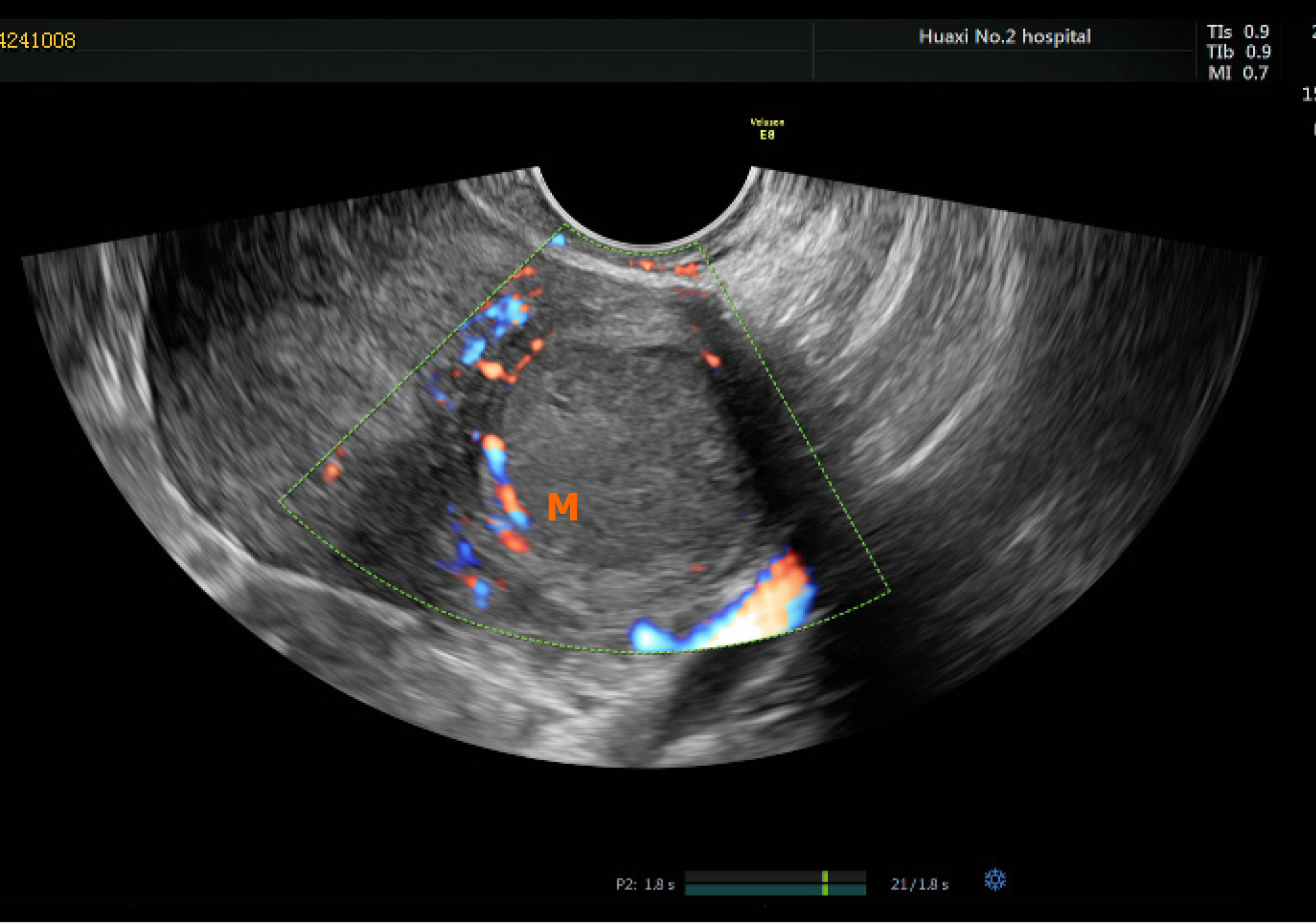
TVU showed a normal endometrial cavity and normal uterus size. A cystic dark area 3.0 cm × 2.9 cm × 3.9 cm in size was observed on the left muscle wall, which was thought to be a uterine myoma with liquefaction or an endometriosis lesion. There was no obvious mass echo in bilateral adnexa area (Figure 1).
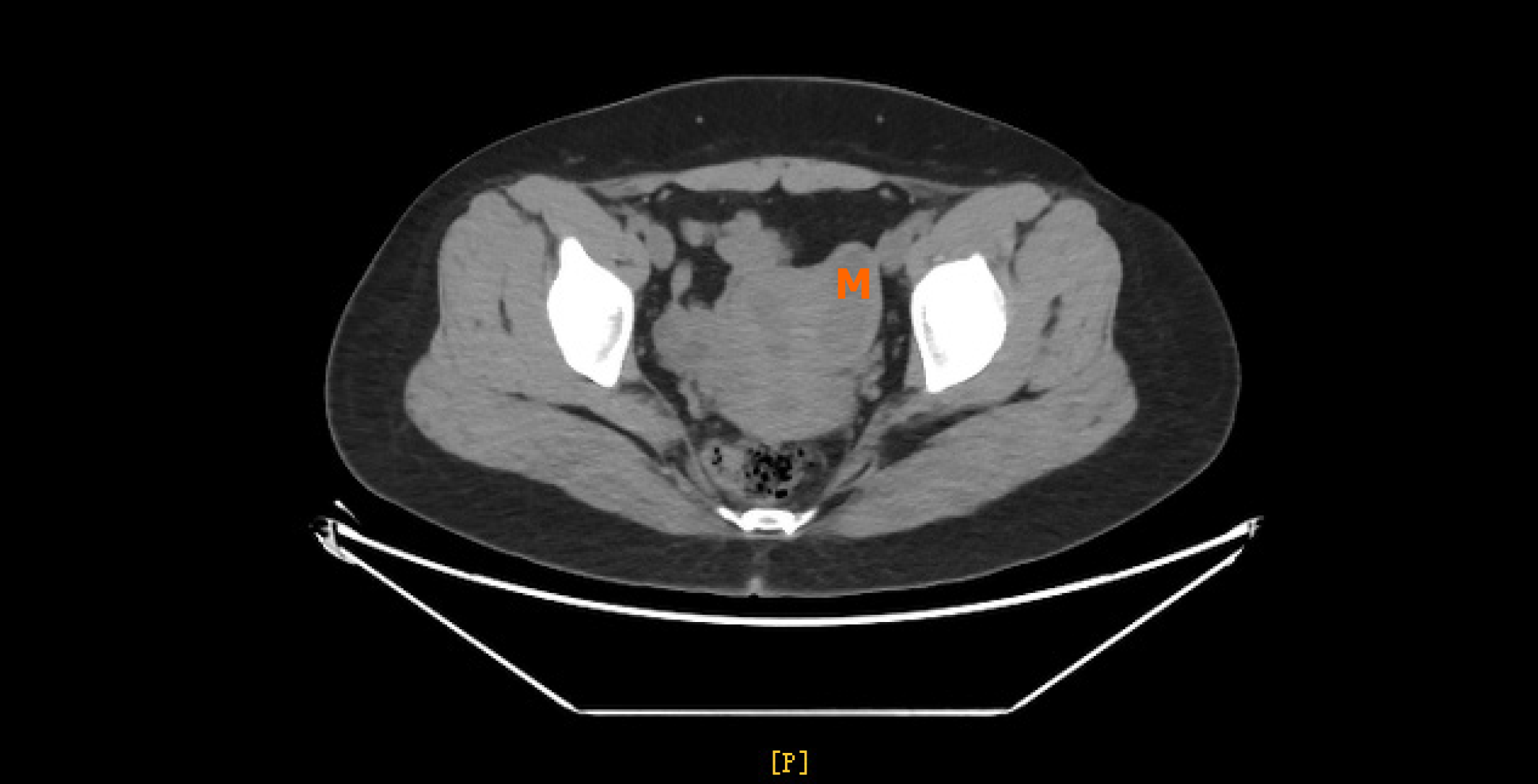
Pelvic contrast-enhanced computed tomography (CT) was then performed, which revealed a cystic lesion on the left posterior wall of the uterus, which protruded to the left horn and serosa of the uterus (Figure 2). Cystic adenomyosis or uterine malformation was suspected, considering the age of the patient and no other findings, the former diagnosis is unlikely. A radiologist, who had been researching on genital tract malformations, considered that the patient had an ACUM.
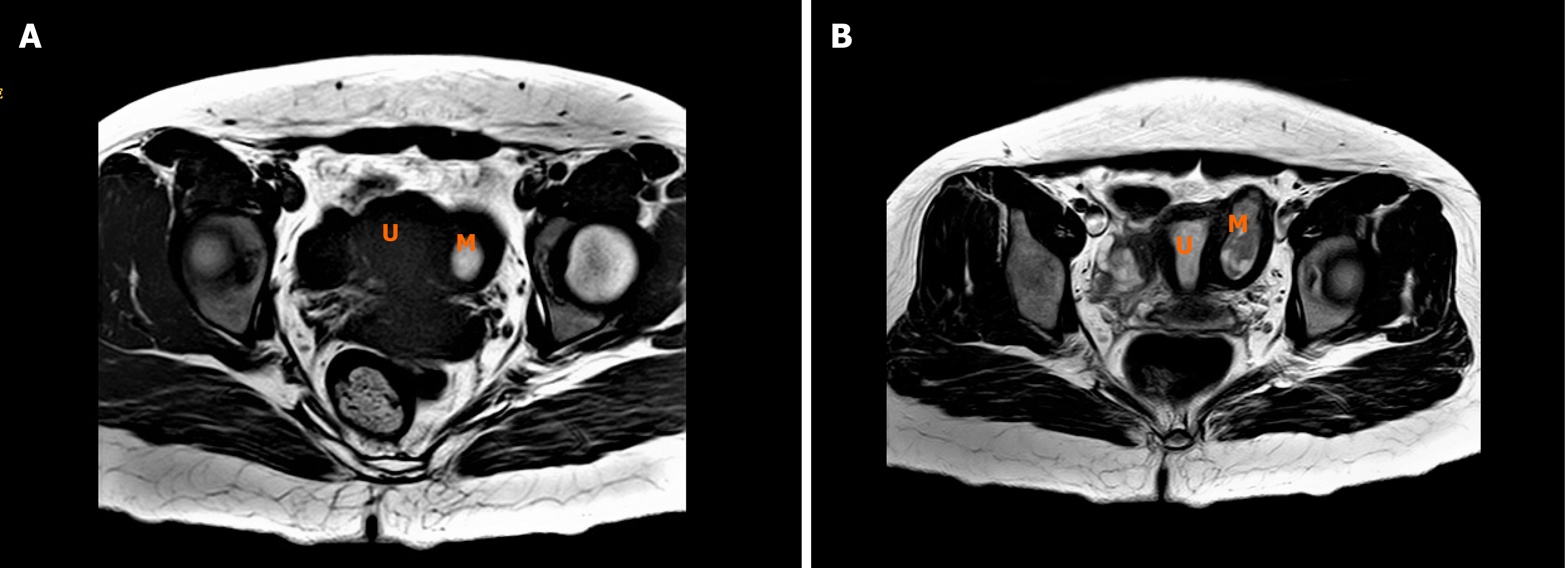
Thus, the patient underwent a preoperative pelvic MRI, which showed a round, cystic lump on the left side of the myometrial wall adjacent to the left uterine horn, that was not contiguous with the endometrial cavity (Figure 3A). MRI showed T1 hyperintensity, T2 heterogeneous hyperintensity components in the ACUM cavity, suggesting hemorrhage. (Figure 3B). Furthermore, the endometrium and myometrium are normal. And the adnexa were otherwise normal.
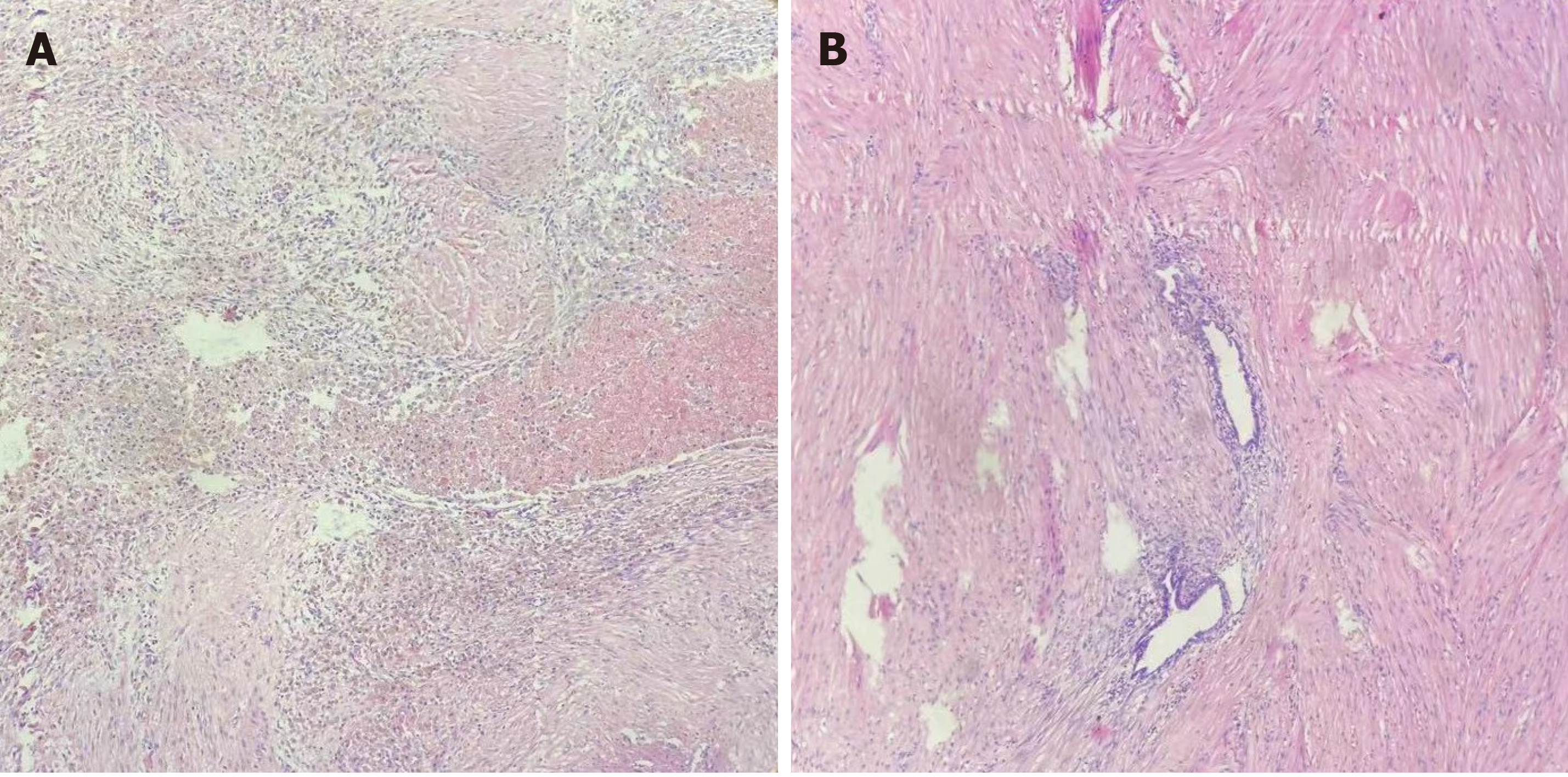
Examination of the histopathological specimen confirmed an accessory uterine mass with a cystic hemorrhagic cavity lined endometrium, surrounded by a layer of myometrium-like smooth muscle around the ACUM (Figure 4).
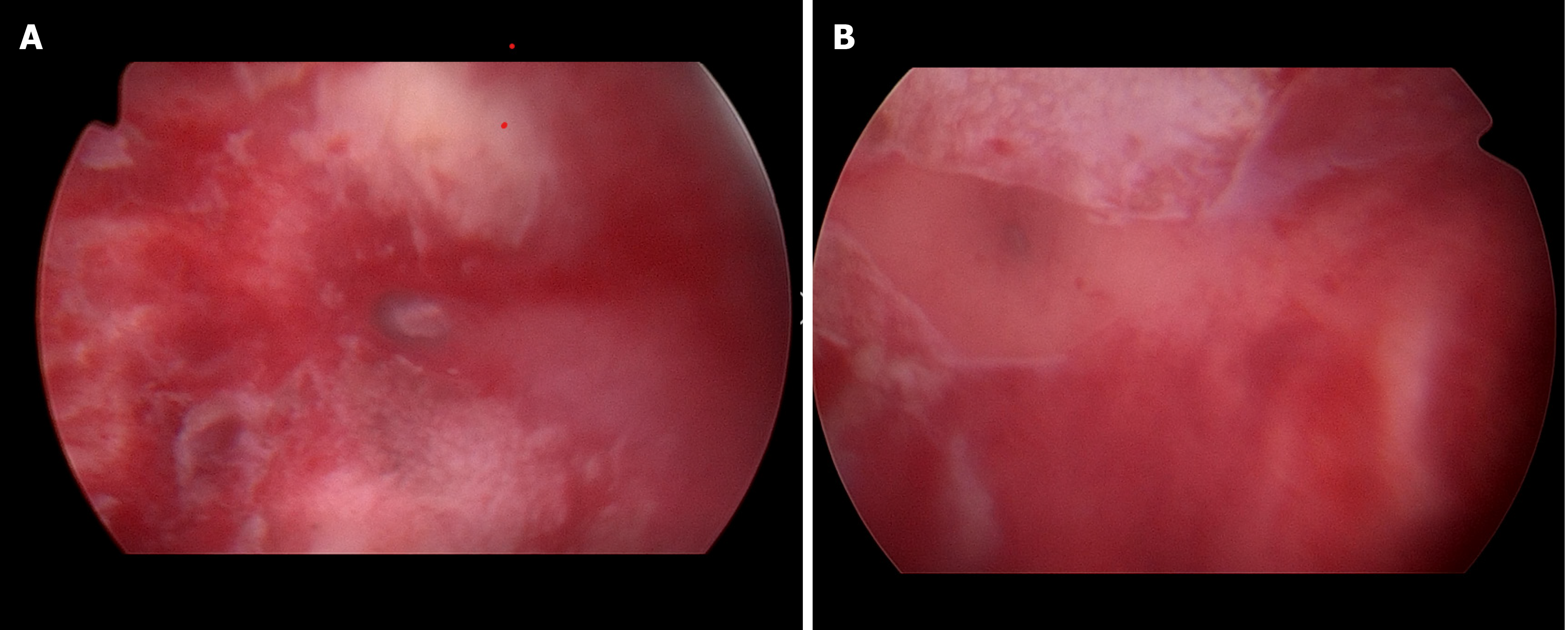
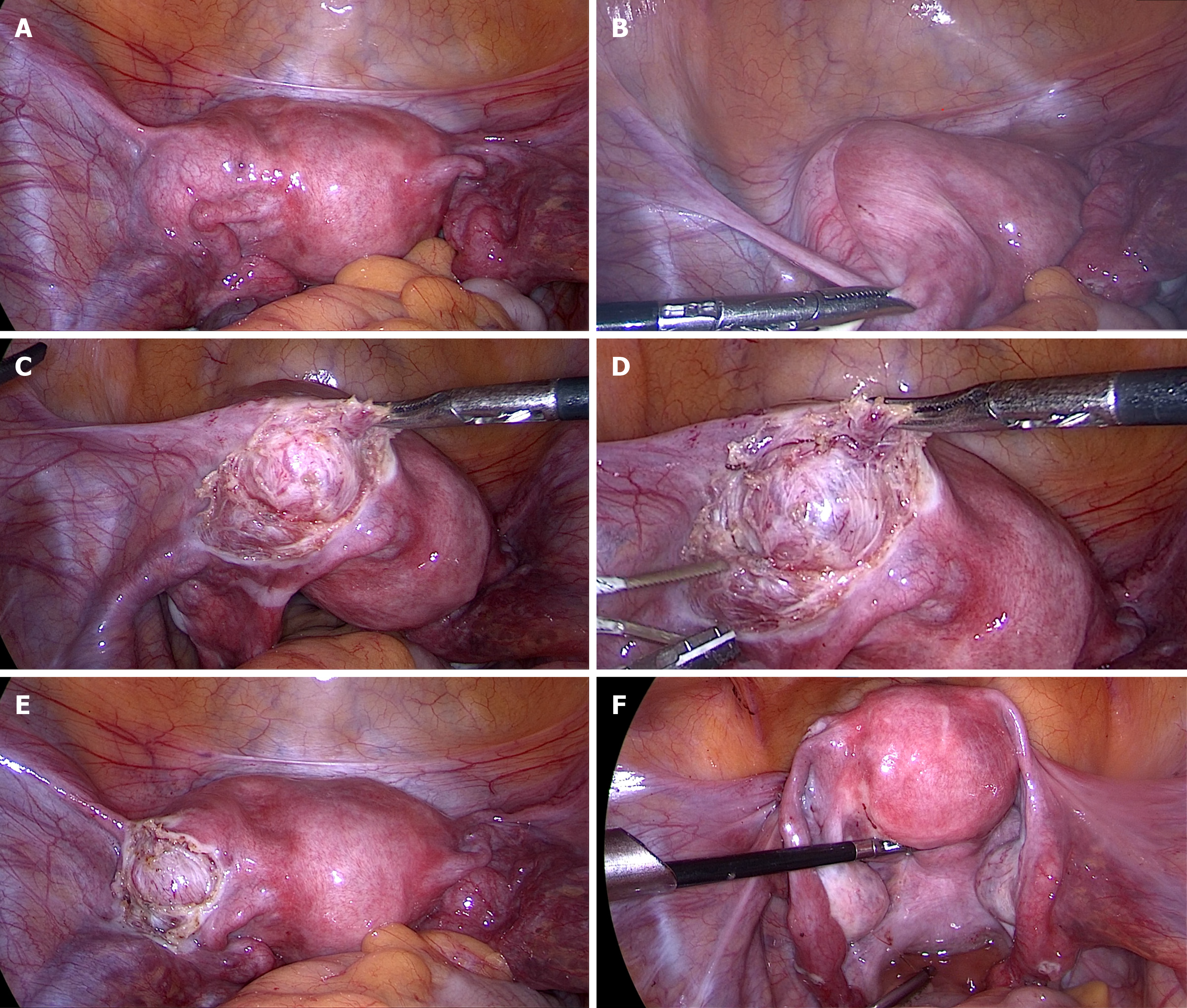
With a diagnosis of intramural mass, hysteroscopy combined with laparoscopic exploration was performed. Hysteroscopy showed a normal uterine cavity, no abnormalities in bilateral cornua uteri and both ostia were visible, and there was no sign of endometriosis pelvic peritoneum (Figure 5). A laparoscopy was performed, the uterine contour was irregular, a mass in the left myometrial wall near the insertion point of the ligament was visualized. Dissection of the mass was carried out using an ultracision-harmonic scalpel. A small incision was made at the top of the lesion, through the left broad ligament, and then a series of blunt and sharp dissections were performed. After the mass was thoroughly dissected, it was completely resected without entering the true cavity. Put the mass into a specimen bag and extracted it from the peritoneal cavity through a trocar. The defect was then sutured using absorbable sutures, and the left round ligament repaired with silk suture. And washed the pelvic cavity thoroughly (Figure 6).
The post-operative course was normal and the patient was discharged from hospital on the third post-operative day. The patient is currently asymptomatic.
A review of the existing literature revealed other more than 40 cases of ACUM recorded by different authors. Seemingly, ACUM is less rare than previously believed. If ACUMs were more correctly diagnosed, they could be more appropriately treated, which would prevent these young women suffering persistent pain[5]. Thus, prompt diagnosis of the atypical uterine malformation is the key to adequate treatment.
With regard to the diagnostic methods for ACUM, as mentioned above, the crux is clinical suspicion based on recurrent symptoms, knowledge of this disease, patient age, and the search for a mass using transabdominal ultrasonography or TVU and the clinical data on the common location of ACUMs. The mass is generally single and isolated[4], usually located on the anterior left or right side of the uterus, below the insertion of the round ligament on the uterine horn. However it may not be accurate, as two ACUMs were identified in one patient[5], and in another patient the mass was located in the anterior myometrium[7].
Reports have illustrated the symptoms, imaging techniques, and surgical management of ACUM. For women with an ACUM, clinical manifestation and imaging might be misleading and may incorrectly suggest other Müllerian abnormalities. In our case, as reported by others in the literature, the main symptoms were recurrent pelvic pain, despite the use of NSAIDs.
Ultrasonography is a useful imaging method to rule out other causes of pelvic pain, such as adenomyosis, pelvic inflammatory diseases, genital tract malformations. Conventional ultrasound might not identify specific sorts of Müllerian duct anomalies. MRI has been considered to be the optimal imaging method to identify endometriosis and Müllerian malformations[8]. In our patient, Ultrasound thought the mass was a uterine myoma with liquefaction or an endometriosis lesion. Fortunately, MRI showed the anatomical nature of ACUM, an accessory uterine mass which did not communicate with the normal uterine cavity. For the management of ACUM, we recommend that surgical excision is necessary and is the only way to definitely diagnose ACUM. Laparoscopic excision is effective, safe and minimally invasive, which is the preferable choice.
ACUM is a rare, underdiagnosed pathology. For a asymptomatic ACUM, it is difficult to distinguish the mass from other disorders, and most women with this disease suffer relentless pelvic pain. Therefore, timely surgical management for suspected case is necessary and can be carried out via laparotomy or laparoscopy. The correct diagnosis can be made only after resection of the lesion and histopathological evaluation.
The authors thank the patient who kindly allowed her disease data to be used for this report.
Manuscript source: Unsolicited manuscript
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Attia G, Dev B S-Editor: Ma YJ L-Editor: A P-Editor: Xing YX
| 1. | Potter DA, Schenken RS. Noncommunicating accessory uterine cavity. Fertil Steril. 1998;70:1165-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 2. | Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Brölmann H, Gianaroli L, Campo R. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013;28:2032-2044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 423] [Cited by in RCA: 455] [Article Influence: 37.9] [Reference Citation Analysis (1)] |
| 3. | Acién P, Sánchez del Campo F, Mayol MJ, Acién M. The female gubernaculum: role in the embryology and development of the genital tract and in the possible genesis of malformations. Eur J Obstet Gynecol Reprod Biol. 2011;159:426-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Acién P, Acién M, Fernández F, José Mayol M, Aranda I. The cavitated accessory uterine mass: a Müllerian anomaly in women with an otherwise normal uterus. Obstet Gynecol. 2010;116:1101-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Acién P, Bataller A, Fernández F, Acién MI, Rodríguez JM, Mayol MJ. New cases of accessory and cavitated uterine masses (ACUM): a significant cause of severe dysmenorrhea and recurrent pelvic pain in young women. Hum Reprod. 2012;27:683-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Peyron N, Jacquemier E, Charlot M, Devouassoux M, Raudrant D, Golfier F, Rousset P. Accessory cavitated uterine mass: MRI features and surgical correlations of a rare but under-recognised entity. Eur Radiol. 2019;29:1144-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Kriplani A, Mahey R, Agarwal N, Bhatla N, Yadav R, Singh MK. Laparoscopic management of juvenile cystic adenomyoma: four cases. J Minim Invasive Gynecol. 2011;18:343-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Jain N, Verma R. Imaging diagnosis of accessory and cavitated uterine mass, a rare mullerian anomaly. Indian J Radiol Imaging. 2014;24:178-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |