Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8932
Peer-review started: June 29, 2021
First decision: July 15, 2021
Accepted: August 3, 2021
Article in press: August 3, 2021
Published online: October 16, 2021
Processing time: 107 Days and 23.4 Hours
Severe eyelid edema and blood accumulation in the submandibular space after preauricular fistula surgery is rarely reported.
We report a 4-year-old girl with eyelid edema and swelling of the submandibular region after preauricular fistula resection under general anesthesia. When drug treatment failed, neck computed tomography examination was performed, which confirmed severe bleeding in the submandibular space. Later, exploration and ligation of the superficial temporal artery were performed under general anesthesia to stop the bleeding. The child was successfully treated, and there were no abnormalities over 1 year of follow-up.
When severe bleeding occurs after preauricular fistula surgery, superficial temporal artery rupture should be considered as a cause.
Core Tip: In clinical practice, infection and recurrence of preauricular fistula after operation are very common. However, eyelid edema and swelling of the submandibular area are very rare, and the possibility of superficial temporal artery bleeding should be considered when anti-inflammatory and antiallergic therapies are ineffective. This can be verified by computed tomography, and exploration and thorough hemostasis are keys to resolving the problem and avoiding more serious consequences.
- Citation: Tian CH, Chen XJ. Severe bleeding after operation of preauricular fistula: A case report. World J Clin Cases 2021; 9(29): 8932-8937
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8932.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8932
Preauricular fistula is one of the most common congenital auricular abnormalities, and its incidence rate is around 1%-2% worldwide[1]. Once fistula infection occurs, cysts and fistulas need to be removed completely to control infection and prevent complications. Till now, postoperative recurrence has been the most common reported clinical problem[2]. Preauricular fistula arises due to failure of fusion of the primitive tubercles that form the pinna, and it is a dominant genetic disease with incomplete penetrance[3,4]. Common clinical complications reported include postoperative hematoma, wound dehiscence, wound infection, and abscess. A more serious complication is facial nerve injury[5]. Here, we present a case of a 4-year-old patient who developed severe bleeding after preauricular fistula operation, which caused serious facial and eyelid edema, blood accumulation in the submandibular space and submental space, and dyspnea. The patient was successfully treated through immediate management.
A 4-year-old girl began to develop swelling of the right eyelid during the operation and the submandibular area 6 h after the operation, accompanied by mild dyspnea.
The patient underwent right preauricular fistula resection under general anesthesia. Six hours after the operation, the patient's right face and right upper and lower eyelids were obviously swollen, and the right submaxillary areas were swollen (Figure 1). She received intravenous dexamethasone injection (5 mg) and oral cetirizine hydrochloride syrup (5 mg); yet, her symptoms did not improve.
The patient was found to have a preauricular fistula on her right side after birth. She was admitted to hospital with recurrent swelling and redness in front of her right ear for more than half a year. Four months prior to presentation, the local hospital had performed incision, drainage, and dressing change.
The patient’s father also had a preauricular fistula, but it had never become inflamed.
The patient's body temperature was 37.0 °C. She had tachypnea (respiratory rate: 42 breaths/min) and tachycardia (heart rate: 125 beats/min). Her blood pressure was 97/68 mmHg and oxygen saturation on pulse oximetry was 91% at ambient air. Her right face and right upper and lower eyelids were obviously swollen, and the right submaxillary areas were swollen (Figure 1). The local skin temperature was elevated.
Whole blood cell examination showed that the white blood cell count was normal (8.37 × 109/L), and the percentage of neutrophils was normal (70.00%).
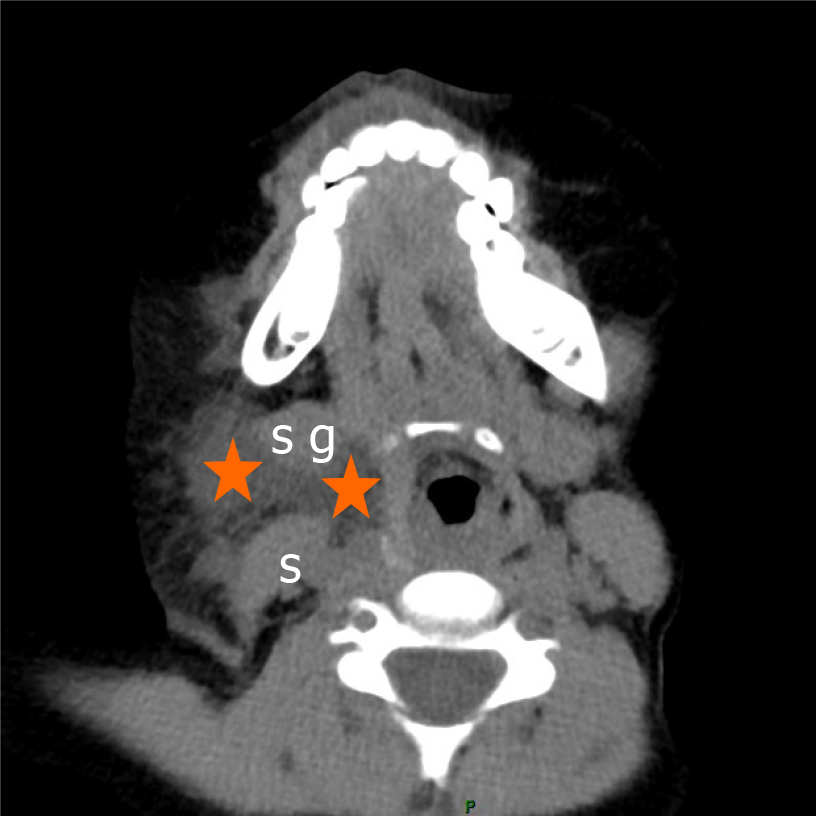
Neck computed tomography (CT) showed low density soft tissue shadow in the right submandibular space, laryngeal shift to the left, and subcutaneous tissue thickening (Figure 2).
Under the guidance of color Doppler ultrasound, we punctured the swollen area under the jaw with a coarse needle, and the blood clot was punctured. Infection and suppuration were ruled out.
Bleeding after operation of preauricular fistula.
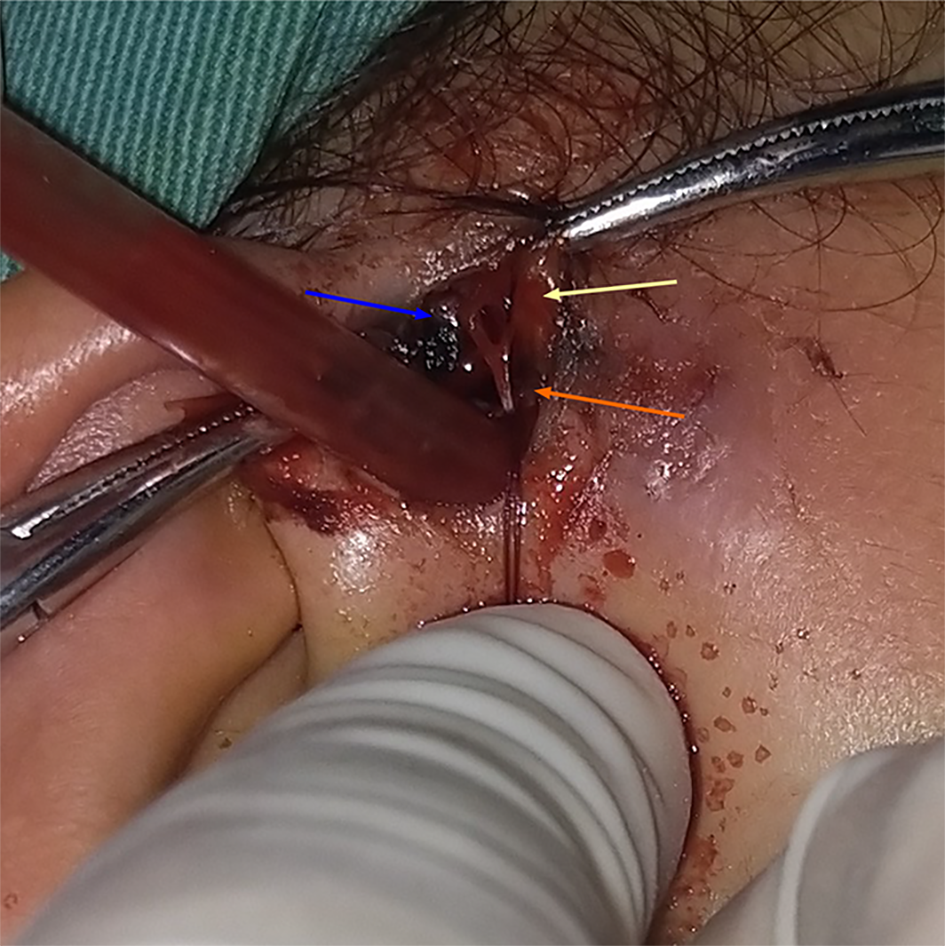
An emergency operation was performed under general anesthesia; rupture and bleeding of the right superficial temporal artery were confirmed (Figure 3). The upper and lower ends of the blood vessels were ligated to stop the bleeding, and a pressure bandage treatment was applied.
The day after surgery, the patient’s immediate symptoms improved significantly. On the fifth day, the patient was cured and discharged. She showed no abnormality during the 1-year follow-up.
Van Heusinger described preauricular fistula first in 1864 and considered it as a benign congenital malformation of the preauricular soft tissues[6]. No treatment is required if no infection occurs. Once there is infection, surgical intervention is needed. It is rare for such a serious hemorrhage to spread up and down along the front edge of parotid gland and the surface space of the masseter muscle, resulting in severe eyelid edema and bleeding in the submandibular neck space.
In this case, a small amount of methylene blue was injected into the fistula orifice during the operation. Methylene blue leakage was then observed after incision of the skin and subcutaneous tissue. Extended resection was performed around the fistula.
Eyelid and right facial swelling were initially found. Hormone and antiallergic treatments were administered in a timely manner but had little effect. The disease progressed again, and the patient had mild dyspnea. We confirmed the intraoperative hemorrhage by CT examination and carried out the intraoperative exploration and hemostasis in time. If the bleeding had developed further, dyspnea may have worsened and led to the severe consequences of asphyxia and death.
The reasons were as follows: (1) Intraoperative injection of methylene blue: Most of the infected preauricular fistulas were broken and incomplete. Injection of methylene blue will lead to remarkable blue staining in the operation cavity, making it impossible to distinguish the boundary between the fistulas and the surrounding normal tissues; (2) During the operation, the responsible vessels were not carefully identified: The superficial temporal artery was bleeding in the deep part of the front end during the operation procedure but it was not given enough attention; and (3) No pressure bandage was applied after the operation: Especially for preauricular fistula with infection, a large defect in the operation cavity may be left after the operation. It is difficult to completely eliminate the dead cavity by closing and suturing the operation cavity only. Failure to apply a pressure bandage will leave the hidden danger for postoperative bleeding unaddressed.
Most of the patients who undergo preauricular fistula surgery are children. Most also have a history of fistula infection, or even incision and drainage of pus. The superficial temporal artery in children is relatively superficial, and, compared with adults, its anatomic relationship is close to skin and helix. As a result, the boundary of the fistula is unclear and the superficial temporal artery can be easily injured, leading to bleeding. Some studies have shown that the recurrence rate of preauricular fistula with infection was higher than that without infection, and the recurrence rate of patients with infection and incision drainage was higher than that of patients with infection and without incision drainage[7,8]. Tang et al[9] surmised that complete excision of the sinus tract was more difficult owing to the fibrosis and edema associated with postinfection inflammation and scarring. The patient described herein happened to have had fistula infection in the past and had received incision and drainage treatment. In order to prevent recurrence, we performed extended resection.
We suggest that for patients with infection, surgery is best performed after the inflammation has been completely controlled for 2 wk. For patients with persistent infection, methylene blue should not be injected during the operation. Methylene blue is difficult to remove after leakage, resulting in unclear lesion boundaries, very slight distinguishment of the anatomical level, and even residual fistula recurrence. It has been reported that the use of methylene blue in preauricular fistula surgery cannot reduce the risk of postoperative recurrence[10].
During the operation, we should pay attention to the fine steps of the operative procedure and ensure complete removal of the fistula. At the same time, attention should be given to the preservation of the surrounding normal tissue as much as possible, in order to reduce the risk of superficial temporal artery injury and also reduce the local defect after operation, which is conveniently close to the operation cavity. Bleeding should be stopped completely. The blood vessels should be explored clearly in any case of active bleeding. Bipolar electrocoagulation should be used to stop the bleeding, and, if necessary, both ends of the blood vessels can be sutured. For severe infection cases, drainage skin can be placed in the operation cavity. It is better to use bandage pressure after the operation, which can help to further close the dead space and reduce the hidden danger of postoperative bleeding.
This case left us a profound lesson. We searched the literature and found no report of severe bleeding after preauricular fistula operation. Therefore, we share this case as a reference to avoid serious consequences when similar situations occur.
We thank Wang XL, MD (Department of Ultrasonic Medicine, Suzhou Hospital of Anhui Medical University, Suzhou, Anhui Province, China) and Shao SH (Department of Imaging, Suzhou Hospital of Anhui Medical University, Suzhou, Anhui Province, China) for their help in the diagnosis. We also thank the patient’s mother for granting permission to publish this report.
Manuscript source: Unsolicited manuscript
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Apiratwarakul K, Salimi M S-Editor: Yan JP L-Editor: A P-Editor: Wu RR
| 1. | Isaacson G. Comprehensive management of infected preauricular sinuses/cysts. Int J Pediatr Otorhinolaryngol. 2019;127:109682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 2. | Choo OS, Kim T, Jang JH, Choung YH. The clinical efficacy of early intervention for infected preauricular sinus. Int J Pediatr Otorhinolaryngol. 2017;95:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Tan T, Constantinides H, Mitchell TE. The preauricular sinus: A review of its aetiology, clinical presentation and management. Int J Pediatr Otorhinolaryngol. 2005;69:1469-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 54] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Fourman P, Fourman J. Hereditary deafness in family with ear-pits (fistula auris congenita). Br Med J. 1955;2:1354-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Tan B, Lee TS, Loh I. Reconstruction of preauricular soft tissue defects using a superiorly based rotation advancement scalp flap - A novel approach to the surgical treatment of preauricular sinuses. Am J Otolaryngol. 2018;39:204-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Chami RG, Apesos J. Treatment of asymptomatic preauricular sinuses: challenging conventional wisdom. Ann Plast Surg. 1989;23:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Rataiczak H, Lavin J, Levy M, Bedwell J, Preciado D, Reilly BK. Association of Recurrence of Infected Congenital Preauricular Cysts Following Incision and Drainage vs Fine-Needle Aspiration or Antibiotic Treatment: A Retrospective Review of Treatment Options. JAMA Otolaryngol Head Neck Surg. 2017;143:131-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Gur E, Yeung A, Al-Azzawi M, Thomson H. The excised preauricular sinus in 14 years of experience: is there a problem? Plast Reconstr Surg. 1998;102:1405-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Tang IP, Shashinder S, Kuljit S, Gopala KG. Outcome of patients presenting with preauricular sinus in a tertiary centre--a five year experience. Med J Malaysia. 2007;62:53-55. [PubMed] |
| 10. | Bruijnzeel H, van den Aardweg MT, Grolman W, Stegeman I, van der Veen EL. A systematic review on the surgical outcome of preauricular sinus excision techniques. Laryngoscope. 2016;126:1535-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |