Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8901
Peer-review started: June 9, 2021
First decision: July 15, 2021
Revised: July 20, 2021
Accepted: August 27, 2021
Article in press: August 27, 2021
Published online: October 16, 2021
Processing time: 128 Days and 7.4 Hours
Imperforate hymen is a rare obstructive anomaly of the female reproductive tract. It is associated with complications, such as cyclical abdominal pain, urinary retention, and pelvic mass.
A 13-year-old girl presented several times to the emergency room with lower abdominal pain for a year. She received conservative treatment, such as pain control, at each visit. She visited our gynecological clinic for worsening pain, and a 14-cm hematocolpos was found on ultrasonography. She was finally diagnosed with an imperforate hymen with hematocolpometra. Hymenectomy was performed, which resulted in event-free regular cyclical menstruation.
Imperforate hymen should be considered in a premenarcheal adolescent girl with periodic abdominal pain.
Core Tip: Imperforate hymen is a rare obstructive disease of the female reproductive tract. Unlike other congenital anomalies, an imperforate hymen can be diagnosed late in the adolescence. It is important to suspect imperforate hymen in premenarcheal adolescent girls with cyclical abdominal pain.
- Citation: Jang E, So KA, Kim B, Lee AJ, Kim NR, Yang EJ, Shim SH, Lee SJ, Kim TJ. Delayed diagnosis of imperforate hymen with huge hematocolpometra: A case report. World J Clin Cases 2021; 9(29): 8901-8905
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8901.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8901
Imperforate hymen is a rare anomaly of the reproductive tract with a prevalence of approximately 0.1% in female newborns[1]. Although an imperforate hymen usually does not accompany other genitourinary tract anomalies, it is associated with severe complications if detected late[2]. Adequate treatment is necessary because complications, such as endometriosis, subfertility, infection, hydronephrosis, and renal failure, can occur in rare cases[3,4]. We report the case of a 13-year-old girl with a huge hematocolpometra and an imperforate hymen.
A 13-year-old girl visited our clinic with periodic lower abdominal pain.
The patient visited the emergency room several times over the previous year due to lower abdominal pain. At each visit, she received conservative treatment, such as pain control. She complained of urinary frequency but no nausea, vomiting, diarrhea, or fever. The lower abdominal pain persisted for 7 d each month with worsening severity of pain over the year. She had not attained menarche.
There was no history of past illnesses.
The personal and family histories were unremarkable.
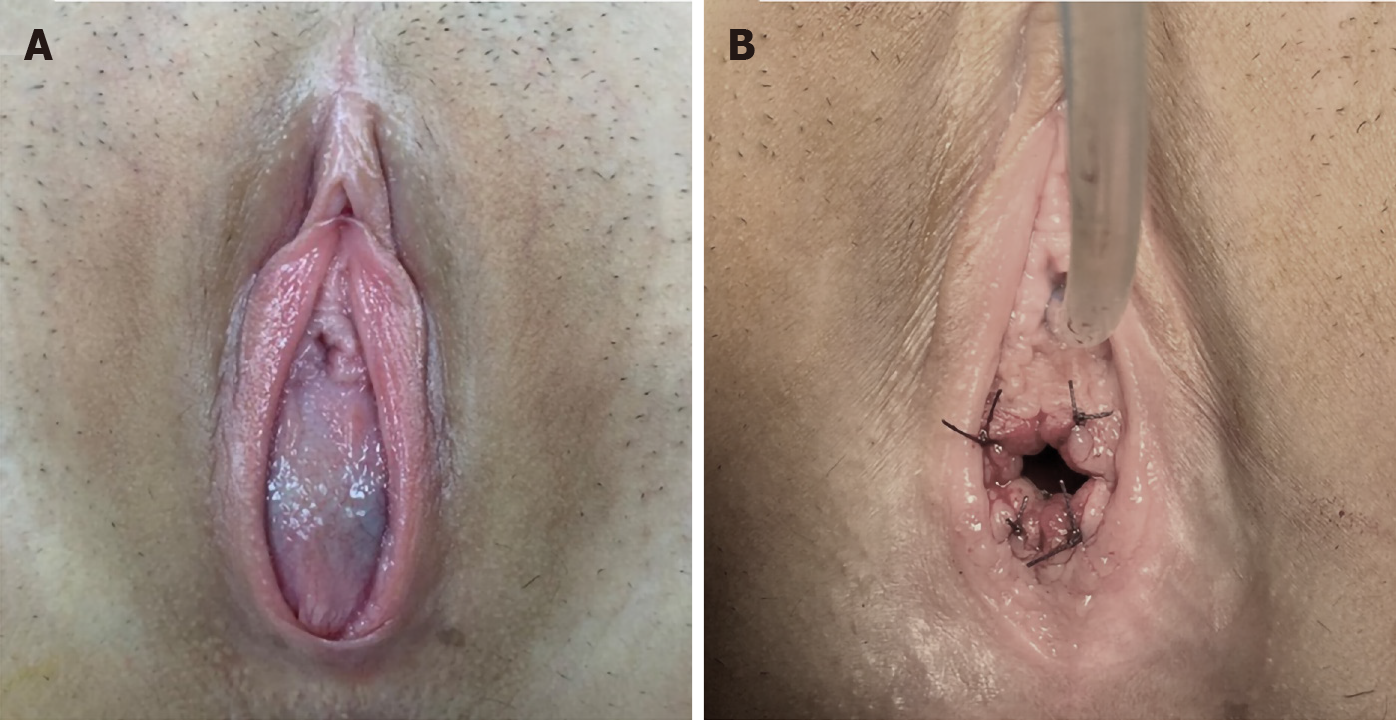
The patient’s blood pressure, heart rate, and body temperature were within the respective normal ranges. On physical examination, Tanner stage III-IV secondary sexual characteristics were observed. The lower abdomen was mildly distended, and a tender pelvic mass was palpable. On pelvic examination, the hymen was found to be imperforated with bulging of the membrane that completely occluded the vaginal canal. No external genital anomalies were noted.
Initial laboratory findings were as follows: Leukocytosis (12150/µL with 80% neutrophils); elevated serum C-reactive protein level (194.4 mg/L; normal range < 3 mg/L); and erythrocyte sedimentation rate was 30 mm/h (normal range < 20 mm/h).
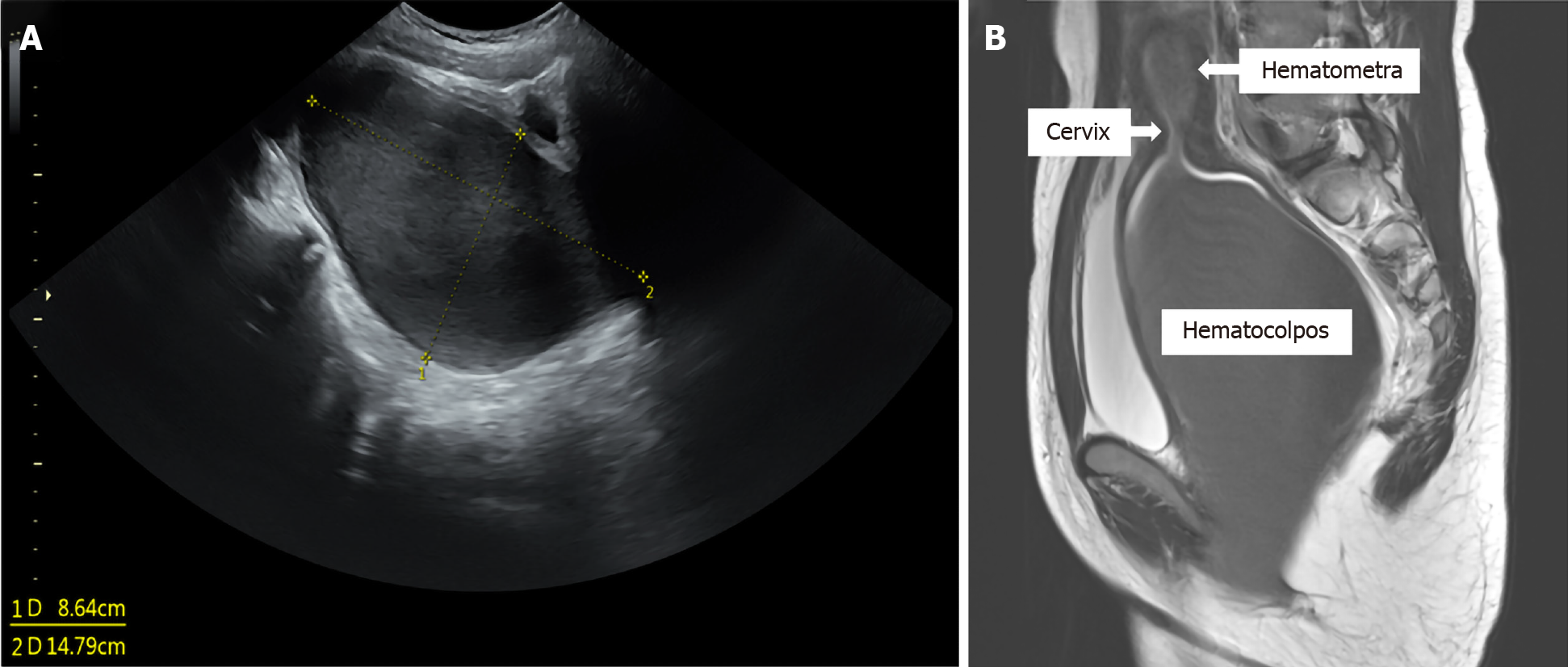
Initial imaging included transabdominal ultrasonography; it revealed a hypoechoic pelvic mass below the bladder, which was suggestive of hematocolpos (Figure 1A). The vaginal cavity was grossly distended with hypoechoic contents. The uterus was not identified on ultrasonography because of the huge hematocolpos. Magnetic resonance imaging (MRI) revealed severe dilatation of the vagina and uterus with high signal intensity on T1-weighted images and low signal intensity on T2-weighted images. These findings suggested hematometra with huge hematocolpos with no other urogenital abnormalities (Figure 1B).
The patient was diagnosed with a huge hematocolpometra with imperforate hymen.
Under general anesthesia, the patient underwent hymenectomy with a cruciate incision on the obstructing membrane. Approximately 800 mL of dark red blood was drained immediately after the incision. After adequate drainage and irrigation, no other abnormalities were found on examination of the vaginal canal. The edges of the incised vaginal mucosa were everted and sutured using 3-0 Vicryl (Ethicon Inc., Somerville, NJ, United States) (Figure 2). Intravenous antibiotics were administered for 3 d after the surgery.
The abdominal pain resolved completely after the surgery, and she had regular menstruation subsequently. The uterus and vagina were normal in appearance on follow-up sonography.
During the later stages of embryonic development, the hymen becomes perforated to connect the uterus with the vaginal canal. A failure of this stage of development results in an imperforate hymen, which is a remnant of mesodermal tissue[4,5]. Imperforate hymen is a rare anomaly of the reproductive tract. Although most cases of imperforate hymen are sporadic, some cases can be due to familial inheritance. A previous report suggested that imperforate hymen can have recessive and dominant inheritance patterns[6]. Most patients with imperforate hymen are asymptomatic until menarche, and early diagnosis is difficult before this period. Abdominal pain is the most common clinical symptom associated with an imperforate hymen. Abdominal pain develops after an asymptomatic period during which the menstrual blood becomes accumulated. The accumulation of blood in the uterus and vagina results in a huge pelvic mass. The frequency of hematocolpos is 0.14% in patients with an imperforate hymen[7]. Primary amenorrhea, cyclical abdominal pain, palpable pelvic mass, and non-specific symptoms, such as abdominal distension, constipation, and urinary retention are observed in adolescent girls with an imperforate hymen. The diagnosis of an imperforate hymen can be easily missed without careful history taking and a thorough physical examination. Early diagnosis and appropriate treatment are important because complications, such as endometriosis, subfertility, infection, hydronephrosis, and renal failure, can occur in rare cases[3,4].
Imperforate hymen can be readily diagnosed on pelvic examination. A bluish bulging hymen is observed at the vaginal introitus in patients with hematocolpos. Ultrasound can help in differentiating pelvic cystic masses. Additionally, MRI may help to identify other diagnoses, such as cervical atresia, vaginal septum, and vaginal agenesis[8]. Generally, an imperforate hymen is not accompanied by other Müllerian abnormalities. The treatment of choice for an imperforate hymen is surgery, such as hymenectomy (cruciate incision or excision of hymen)[3]. After adequate drainage of menstrual blood and irrigation, the incised vaginal mucosa may be sutured to form a hymenal ring. The possible complications of this procedure include reclosure, vaginal adhesion, and vaginal adenosis[5]. The incidence of recurrence can be reduced by everting the edges of the incised vaginal mucosa[9]. The prognosis following surgery is generally excellent, and the fertility rate in patients with an imperforate hymen is within the normal range.
Imperforate hymen is a rare obstructive disease of the female reproductive tract. Surgical treatment provides excellent outcomes. Therefore, early diagnosis of an imperforate hymen is essential for successful treatment. Diagnosis of an imperforate hymen can be easily missed without careful history taking and physical examination, which can lead to delayed treatment. It is important to consider imperforate hymen in adolescent girls with cyclical pelvic pain and primary amenorrhea.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He CY S-Editor: Chang KL L-Editor: A P-Editor: Ma YJ
| 1. | Stelling JR, Gray MR, Davis AJ, Cowan JM, Reindollar RH. Dominant transmission of imperforate hymen. Fertil Steril. 2000;74:1241-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Dane C, Dane B, Erginbas M, Cetin A. Imperforate hymen-a rare cause of abdominal pain: two cases and review of the literature. J Pediatr Adolesc Gynecol. 2007;20:245-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 3. | Eksioglu AS, Maden HA, Cinar G, Tasci Yildiz Y. Imperforate hymen causing bilateral hydroureteronephrosis in an infant with bicornuate uterus. Case Rep Urol. 2012;2012:102683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Abraham C. Imperforate Hymen Causing Hematocolpos and Urinary Retention. J Emerg Med. 2019;57:238-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Lee KH, Hong JS, Jung HJ, Jeong HK, Moon SJ, Park WH, Jeong YM, Song SW, Suk Y, Son MJ, Lim JJ, Shin JI. Imperforate Hymen: A Comprehensive Systematic Review. J Clin Med. 2019;8:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Sakalkale R, Samarakkody U. Familial occurrence of imperforate hymen. J Pediatr Adolesc Gynecol. 2005;18:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Chang JW, Yang LY, Wang HH, Wang JK, Tiu CM. Acute urinary retention as the presentation of imperforate hymen. J Chin Med Assoc. 2007;70:559-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Burgis J. Obstructive Müllerian anomalies: case report, diagnosis, and management. Am J Obstet Gynecol. 2001;185:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 105] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Mou JW, Tang PM, Chan KW, Tam YH, Lee KH. Imperforate hymen: cause of lower abdominal pain in teenage girls. Singapore Med J. 2009;50:e378-e379. [PubMed] |