Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8702
Peer-review started: June 10, 2021
First decision: July 5, 2021
Revised: July 13, 2021
Accepted: August 6, 2021
Article in press: August 6, 2021
Published online: October 16, 2021
Processing time: 127 Days and 0.5 Hours
Although rectal prolapse is not a life-threatening condition, it can cause defecation disorders, anal incontinence, sensory abnormalities, and other problems that can seriously affect quality of life.
To study the efficacy of the modified Gant procedure for elderly women with internal rectal prolapse.
Sixty-three elderly female patients with internal rectal prolapse underwent the modified Gant procedure. The preoperative and postoperative anal symptoms, Patient Assessment of Constipation Quality of Life (PAC-QOL), Wexner incontinence score, incontinence quality of life score, and complications (massive hemorrhage, infection, anorectal stenosis, and anorectal fistula) were compared.
The improvement rates of postoperative symptoms were defecation disorders (84.5%), anal distention (69.6%), defecation sensation (81.4%), frequent defecation (88.7%), and anal incontinence (42.9%) (P < 0.05). All dimensions and total scores of the PAC-QOL after the procedure were lower than those before the operation (P < 0.05). The postoperative anal incontinence score and Wexner score were significantly lower than those before the procedure (P < 0.05). The quality of life and total scores of postoperative anal incontinence were significantly higher than those before the procedure (P < 0.05). There were no serious complications and no deaths.
The modified Gant procedure has significant advantages in the treatment of elderly women with internal rectal prolapse.
Core Tip: Intrarectal prolapse in elderly patients, who have low tolerance for surgery, is often complicated by medical diseases. In this study, we explored a new kind of operation with a reliable curative effect, few postoperative complications and tolerance by elderly women with intrarectal prolapse.
- Citation: Xu PP, Su YH, Zhang Y, Lu T. Modified Gant procedure for treatment of internal rectal prolapse in elderly women. World J Clin Cases 2021; 9(29): 8702-8709
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8702.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8702
Intrarectal prolapse (IRP) is defined as the intraluminal intussusception of a part of, or the whole rectal wall, in which no external lesions can be observed on the flat surface of the anus[1]. IRP commonly tends to affect older women. Some patients need surgical treatment when conservative treatment does not improve the condition. However, serious complications such as anastomotic fistula, rectal stricture, and pelvic infection may occur despite the many surgical options for IRP. IRP in elderly patients, who have low tolerance for surgery, is often complicated by medical diseases[2]. This study investigated a new type of procedure with a reliable curative effect, few postoperative complications, and tolerance in elderly women with IRP.
From September 2018 to April 2020, 63 elderly female patients with IRP were selected according to the previously published diagnostic criteria[3]. The patients were aged 60 to 82 years, with an average age of 67.19 ± 5.57 years, and six patients presented with serious medical diseases (Table 1). Inclusion criteria: (1) patients who met the diagnostic criteria of IRP with clinical symptoms; (2) patients aged ≥ 60 years; and (3) patients who had multidisciplinary treatment (gastroenterology, urology and gynecology) and were cured by long-term conservative treatment. The exclusion criteria were: (1) patients with perianal diseases such as perianal abscess, anal fissure, anal fistula, and perianal condyloma acuminatum; (2) patients with gynecological diseases, urinary diseases or colorectal tumors; (3) patients with mental illness; and (4) judgment of the efficacy or safety of the procedure was affected by incomplete data.
| Characteristics | n |
| Age (yr) | |
| 60–69 | 36 |
| 70–79 | 25 |
| ≥ 80 | 2 |
| Preoperative complication of serious disease | |
| Coronary atherosclerotic heart disease | 2 |
| Chronic obstructive pulmonary disease | 1 |
| Liver cirrhosis | 1 |
| Diabetes | 2 |
| Oxford Rectal Prolapse Grade (ORPG) | |
| ORPG-1 (High rectal) | 1 |
| ORPG-2 (Low rectal) | 6 |
| ORPG-3 (High anal) | 25 |
| ORPG-4 (Low anal) | 31 |
A detailed medical history was taken, comprehensive physical examination and investigations (routine examination, urine, stool, blood biochemistry, five items of liver disease, electrogram, and electric colonoscopy) were made, and all the patients were treated. They were also examined by defecography and graded according to the Oxford Rectal Prolapse Grade (ORPG). A detailed explanation of the procedure was provided to all the patients, who were reassured in order to enhance compliance with the treatment. Written informed consent was obtained from each of the patients.
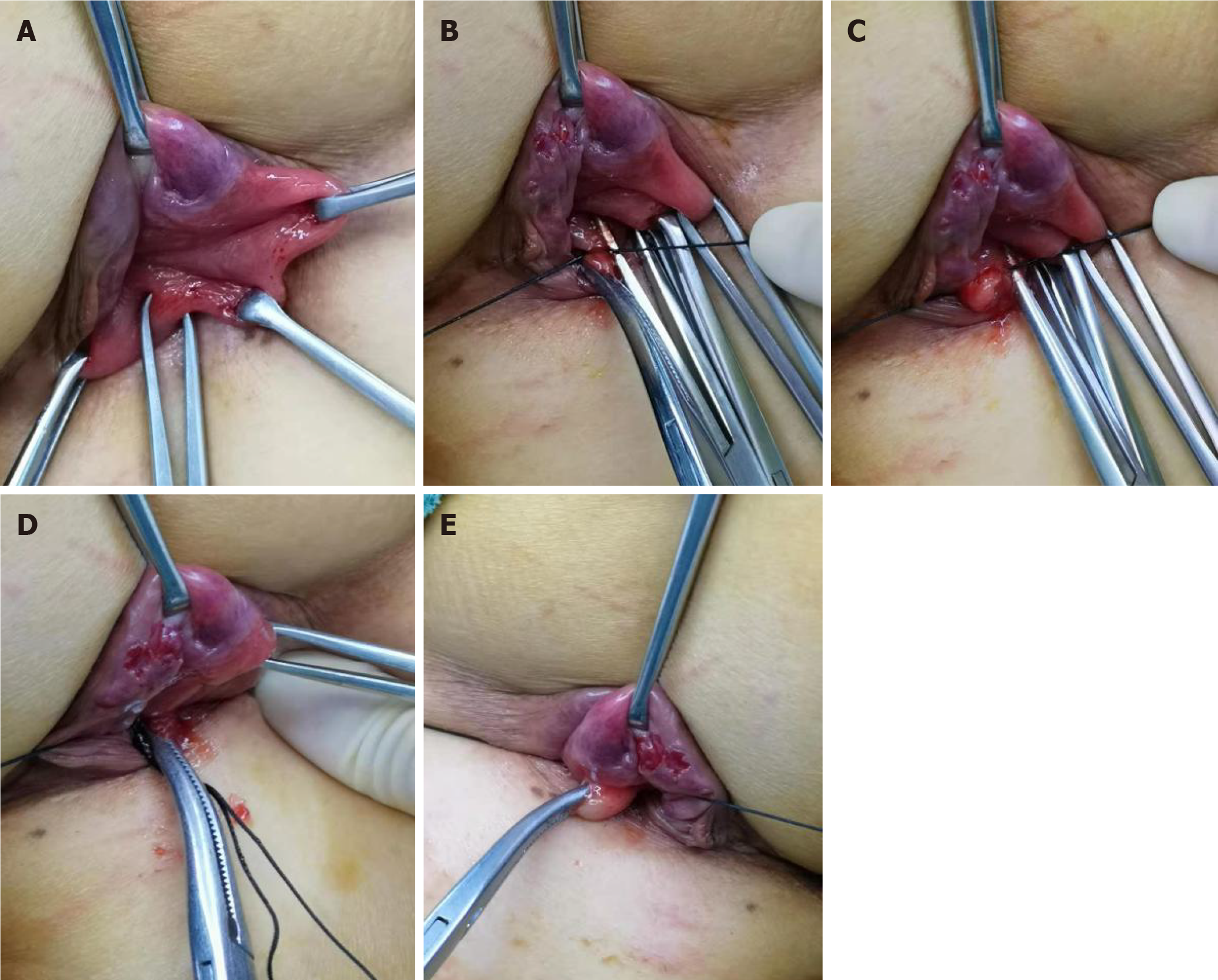
Patients were placed in the right lateral position and the operation site was exposed. Routine disinfection and anorectal iodophor cotton ball disinfection were performed. Digital rectal examination was conducted to rule out rectal space-occupying lesions and anal fistulae, and an anal retractor was used to keep the anal canal open for exploration. Guided by a finger, an Alice tissue forceps was used to clamp the loose rectal mucosa from the anal margin to the proximal end of the rectum and to pull it outward along the same point. The loose and prolapsed rectal mucosa was pulled out to the maximum extent, with a total length of ~6 cm. Using the Alice tissue forceps, the rectal mucosa was longitudinally clamped at the uppermost end of the intestinal mucosa and ligated with No. 10 mu silk line to form a mucosal ball. By repeating these steps, several mucosal balls were formed on the mucous membrane, 1 cm from the tooth line, and approximately three mucosal balls were flattened with the same forceps. There were 3–5 mucosal balls from the top of the rectum at the same point. We ensured that two fingers could be inserted into the rectal cavity, even with the mucosal balls, and that there was tension between the flat mucous balls during the ligation process (Figure 1).
The preoperative and postoperative anal symptoms, the Patient Assessment of Constipation Quality of Life (PAC-QOL), the Wexner anal incontinence score, the anal incontinence quality score, and the postoperative complications (massive hemorrhage, infection, anorectal stricture, anorectal fistula) were recorded.
SPSS 20.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analyses. The measurement data were expressed as mean ± SD and compared by single factor analysis of variance, while the numerical data was expressed as the number of cases (constituent ratio) and compared by χ2 or Fisher’s exact test (α = 0.05).
The improvement rates of postoperative symptoms were as follows: defecation disorders, 84.5%; anal distention, 69.6%; defecation sensation, 81.4%; frequent defecation, 88.7%; and anal incontinence, 42.9% (P < 0.05) (Table 2).
| Symptoms | Proportion | Improvement rate (%) | χ2 | P | |
| Before procedure (n = 63) | After procedure (n = 63) | ||||
| Defecation disorder | 58 (92.1) | 9 (14.3) | 84.5 | 76.531 | 0.000 |
| Anal distension | 56 (88.9) | 17 (27.0) | 69.6 | 49.537 | 0.000 |
| Inexhaustible sense of defecation | 59 (93.7) | 11 (17.5) | 81.4 | 74.057 | 0.000 |
| Frequent defecation | 53 (84.1) | 6 (9.5) | 88.7 | 61.050 | 0.000 |
| Anal incontinence | 35 (55.6) | 20 (31.7) | 42.9 | 7.260 | 0.007 |
All dimensions and total scores of PAC-QOL after the procedure were lower than those before the procedure (P < 0.05). The postoperative anal incontinence score and Wexner score were significantly lower than those before the procedure (P < 0.05). The quality of life and total score of postoperative anal incontinence were significantly higher than those before the procedure (P < 0.05) (Table 3).
| Before procedure (n = 63) | After procedure (n = 63) | t | P | |
| PAC-QOL score | ||||
| Physiology (4 items) | 8.41 ± 2.18 | 5.48 ± 1.41 | 8.966 | 0.000 |
| Social psychology (8 items) | 18.79 ± 4.05 | 12.16 ± 3.23 | 10.157 | 0.000 |
| Worry (11 items) | 20.58 ± 5.59 | 15.49 ± 4.35 | 5.672 | 0.000 |
| Satisfaction (5 items) | 16.87 ± 4.39 | 11.52 ± 3.24 | 7.788 | 0.000 |
| Total score | 64.63 ± 14.05 | 44.65 ± 10.60 | 9.012 | 0.000 |
| Wexner score of anal incontinence | 8.54 ± 3.19 | 5.70 ± 3.33 | 3.129 | 0.003 |
| Quality of life score of anal incontinence | ||||
| Lifestyle (10 items) | 26.83 ± 7.23 | 31.25 ± 8.81 | -2.013 | 0.049 |
| Coping/behavior (9 items) | 20.06 ± 6.06 | 25.05 ± 5.52 | -3.032 | 0.004 |
| Depression/self-perception (7 items) | 14.91 ± 5.79 | 18.10 ± 4.24 | -2.149 | 0.036 |
| Awkward (3 items) | 5.46 ± 1.82 | 6.85 ± 1.76 | -2.764 | 0.008 |
| Total score | 67.26 ± 13.56 | 81.25 ± 13.95 | -3.644 | 0.001 |
IRP is a condition that affects the pelvic floor, and its pathogenesis remains unclear[4]. In the clinical setting, rectal prolapse syndrome is the main manifestation and includes defecation disorder, auxiliary defecation, repeated trips to the restroom, and a feeling that the anus is falling out. Due to the low sensitivity and specificity of the clinical manifestations and limited understanding of IRP in the past, the diagnosis mainly depended on a detailed medical history[5]. In the past 20 years, IRP has been further diagnosed with the development of imaging techniques such as defecography and rectal ultrasound, and especially dynamic pelvic floor magnetic resonance[6]. The ORPG is an internationally recognized grading system for IRP based on imaging findings. According to the degree of prolapse, IRP can be divided into five grades: 1 and 2 indicate rectal intussusception; 3 and 4 indicate rectoanal intussusception; and 5 indicates external rectal prolapse. There is a correlation between the severity of prolapse and age[7]. The degree of prolapse increases and has more obvious clinical symptoms with increasing age. Female sex and multiparity are also risk factors for IRP[8].
Surgical treatment can be considered for patients with IRP in whom conservative treatments have been ineffective. In addition, many procedures to treat IRP are performed during surgery for external rectal prolapse, including laparoscopic ventral rectal repair and fixation (LVMR)[9], transanal surgeries such as Delorme’s procedure, and transanal rectal anastomosis (STARR). One study showed that the improvement rates for constipation and fecal incontinence treated by LVMR for IRP were 65%–92% (39%–43%) and 73%–97% (39%–40%), respectively. The incidence of complications is low, ranging from 0% to 23% (44%). Most complications are mild, but there are also serious complications (vaginal erosion with prosthesis exposure, infection, intestinal obstruction, rectal perforation, and hernia)[10,11]. The improvement rate of clinical constipation after Delorme’s procedure is 76%, but the risk of incomplete defecation and fecal incontinence increases (24%)[12,13]. STARR is often recommended for the treatment of obstructive constipation, with an efficacy rate of 80%[14,15]. However, because of the decrease in rectal volume and changes in sensitivity, there is an increased risk of fecal incontinence as well as serious complications such as nail line rupture, abnormal pelvic cellulitis, and rectovaginal fistula[16]. The present study showed that the improvement rates for constipation and anal incontinence after the modified Gant procedure for elderly female patients with IRP were 84.5% and 42.9%, respectively, and there were no serious complications. Compared to the above-mentioned surgical methods for IRP, there was no significant difference in the improvement rate of constipation; there was a certain advantage in the convenience of correcting anal incontinence; and there were no serious complications caused by other surgical methods.
Although anorectal measurement is an objective means of examination, it cannot precisely evaluate the severity of anal incontinence and/or defecation disorders in patients with IRP. For patients with IRP with anal incontinence or defecation disorders, the subjective constipation/anal incontinence quality of life questionnaire can precisely reflect the severity of the complaints and help surgeons formulate treatment strategies and evaluate treatment outcomes for clinical and research objectives. Therefore, the present study used the PAC-QOL scale[17], the Wexner anal incontinence score scale[18], and the anal incontinence quality score to evaluate the clinical efficacy of the procedure[19]. The results showed that the modified Gant procedure could significantly improve constipation, anal incontinence, and the quality of life of patients with IRP.
The modified Gant procedure used in this study for treatment of IRP can shorten the rectal mucosa and fix it to the muscular layer by ligating the scar. In addition, the procedure is limited to the loose rectal mucosa, as the surrounding tissue is damaged. It can relieve defecation disorders and anal incontinence caused by rectal intussusception and reduce the stimulation to the rectal defecation receptor by the prolapsed tissue[20]. As a result, the modified Gant procedure can improve clinical symptoms such as anal distension and incomplete defecation and quality of life, postoperative pain, and serious complications caused by other procedures. This procedure does not require general anesthesia, and as a palliative procedure, it is particularly suitable for elderly patients with internal diseases and low surgical tolerance. During the procedure, attention to the following points is required: The prolapsed tissue must be pulled out gently to avoid mucosal tear. In addition, the index finger should be extended into the rectum under guidance to ensure that the pulled rectal mucosa is located on the same longitudinal axis. Moreover, a digital rectal examination should be performed before ligating the mucosa, to ensure that the rectal cavity at the point of ligation is greater than two fingers wide to avoid rectal stricture.
The long-term effect of this procedure needs to be observed and measured as the short follow-up time of the study was a limitation. The treatment of IRP requires a multidisciplinary management. In future studies, we will investigate whether comprehensive postoperative treatment, such as pelvic floor muscle training, traditional Chinese medicine, and psychological intervention, would benefit patients with rectal prolapse.
The modified Gant procedure has significant advantages in the treatment of elderly women with IRP, a reliable curative effect, few postoperative complications, and is easily tolerated.
Intrarectal prolapse (IRP) is defined as the intraluminal intussusception of part of, or the whole rectal wall, in which no external lesions can be observed on the flat surface of the anus.
IRP tends to commonly affect older women. Some patients need surgical treatment when conservative treatment does not improve the condition.
To explore a new type of procedure with a reliable curative effect, few postoperative complications, and easy tolerance by elderly women with IRP.
Sixty-three elderly female patients with IRP underwent the modified Gant procedure.
The quality of life and total score of postoperative anal incontinence were significantly higher than those before the procedure.
The modified Gant procedure has significant advantages in the treatment of elderly women with IRP. It has reliable curative effect, few postoperative complications, and is easily tolerated by elderly patients.
In future studies, the authors will investigate whether comprehensive postoperative treatment, such as pelvic floor muscle training, traditional Chinese medicine, and psychological intervention, would be of benefit to patients with IRP.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Brochard C S-Editor: Wang JL L-Editor: Kerr C P-Editor: Wang LYT
| 1. | Cariou de Vergie L, Venara A, Duchalais E, Frampas E, Lehur PA. Internal rectal prolapse: Definition, assessment and management in 2016. J Visc Surg. 2017;154:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Iida Y, Honda K, Saitou H, Munemoto Y, Tanaka H. Modified Gant-Miwa-Thiersch procedure (mucosal plication with anal encircling) for rectal prolapse. Colorectal Dis. 2019;21:588-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | van der Schans EM, Paulides TJC, Wijffels NA, Consten ECJ. Management of patients with rectal prolapse: the 2017 Dutch guidelines. Tech Coloproctol. 2018;22:589-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Collinson R, Cunningham C, D'Costa H, Lindsey I. Rectal intussusception and unexplained faecal incontinence: findings of a proctographic study. Colorectal Dis. 2009;11:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 84] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Wijffels NA, Jones OM, Cunningham C, Bemelman WA, Lindsey I. What are the symptoms of internal rectal prolapse? Colorectal Dis. 2013;15:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Faucheron JL, Barot S, Collomb D, Hohn N, Anglade D, Dubreuil A. Dynamic cystocolpoproctography is superior to functional pelvic MRI in the diagnosis of posterior pelvic floor disorders: results of a prospective study. Colorectal Dis. 2014;16:O240-O247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Wijffels NA, Collinson R, Cunningham C, Lindsey I. What is the natural history of internal rectal prolapse? Colorectal Dis. 2010;12:822-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Joshi HM, Woods AK, Smyth E, Gosselink MP, Cunningham C, Lindsey I, Urban J, Jones OM, Vollrath F. Histological and mechanical differences in the skin of patients with rectal prolapse. Int J Colorectal Dis. 2015;30:1117-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | D'Hoore A, Cadoni R, Penninckx F. Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg. 2004;91:1500-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 317] [Article Influence: 15.1] [Reference Citation Analysis (1)] |
| 10. | Portier G, Kirzin S, Cabarrot P, Queralto M, Lazorthes F. The effect of abdominal ventral rectopexy on faecal incontinence and constipation in patients with internal intra-anal rectal intussusception. Colorectal Dis. 2011;13:914-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Franceschilli L, Varvaras D, Capuano I, Ciangola CI, Giorgi F, Boehm G, Gaspari AL, Sileri P. Laparoscopic ventral rectopexy using biologic mesh for the treatment of obstructed defaecation syndrome and/or faecal incontinence in patients with internal rectal prolapse: a critical appraisal of the first 100 cases. Tech Coloproctol. 2015;19:209-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Liberman H, Hughes C, Dippolito A. Evaluation and outcome of the delorme procedure in the treatment of rectal outlet obstruction. Dis Colon Rectum. 2000;43:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Pescatori M, Zbar AP. Tailored surgery for internal and external rectal prolapse: functional results of 268 patients operated upon by a single surgeon over a 21-year period*. Colorectal Dis. 2009;11:410-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ribaric G, D'Hoore A, Schiffhorst G, Hempel E; TRANSTAR Registry Study Group. STARR with CONTOUR® TRANSTAR™ device for obstructed defecation syndrome: one-year real-world outcomes of the European TRANSTAR registry. Int J Colorectal Dis. 2014;29:611-622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Ren XH, Yaseen SM, Cao YL, Liu WC, Shrestha S, Ding Z, Wu YH, Zheng KY, Qian Q, Jiang CQ. A transanal procedure using TST STARR Plus for the treatment of Obstructed Defecation Syndrome: 'A mid-term study'. Int J Surg. 2016;32:58-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Kim M, Meurette G, Ragu R, Lehur PA. Current surgical treatment of obstructed defecation among selected European opinion leaders in pelvic floor surgery. Tech Coloproctol. 2016;20:395-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Mokhtare M, Ghafoori SM, Soltani-Kermanshahi M, Boghratian AH, Agah S, Sheikhvatan M. Reliability and validity of the Persian version of patient assessment of constipation- quality of life (PAC-QOL) questionnaire. Gastroenterol Hepatol Bed Bench. 2017;10:289-294. [PubMed] |
| 18. | Fonseca AM, Meinberg MF, Lucas DV, Monteiro MV, Figueiredo EM, Fonseca L, Filho AL. Cultural adaptation and validation of the Wexner scale in patients with anal incontinence in a Brazilian population. Int Urogynecol J. 2016;27:959-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Tejedor P, Bodega-Quiroga I, Plaza J, Ortega López M, Gutierrez C, García Olmo D, Pastor C. Quality of life and 3D-EUS assessment for anal incontinence after childbirth. Rev Esp Enferm Dig. 2019;111:453-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Tranchart H, Valverde A, Goasguen N, Gravié JF, Mosnier H. Conservative treatment of intrarectal mesh migration after ventral laparoscopic rectopexy for rectal prolapse. Int J Colorectal Dis. 2013;28:1563-1566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |