Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8260
Peer-review started: May 20, 2021
First decision: June 15, 2021
Revised: June 23, 2021
Accepted: August 5, 2021
Article in press: August 5, 2021
Published online: September 26, 2021
Processing time: 119 Days and 0.2 Hours
Fat embolism syndrome (FES) is a rare complication caused by the presence of fat particles in the microcirculation, which usually occurs within 12-72 h after trauma. At present, there have been few cases of fat embolism presenting within 3 h after trauma. Here, we report a case of femoral fracture complicated with an acute fat embolism caused by a car accident.
A 29-year-old woman with pain, swelling and limited movement of her left lower limb after a car accident was taken by ambulance to our hospital. X-ray examination showed fracture of the middle and lower part of the left femur and fracture of the base of the left fifth metatarsal bone. She was hospitalized and admitted to the orthopedic ward. After the attending doctor performed tibial tubercle bone traction, the patient became confused, followed by respiratory distress. Finally, she was transferred to the intensive care unit. After nearly a month of treatment in the intensive care unit, the patient's cognitive function gradually recovered over 6 mo.
For patients with early traumatic fractures, young emergency physicians and orthopedics should be aware of the possibility of FES.
Core Tip: Early fat embolism syndrome (FES) is a rare complication of traumatic orthopedics. For patients with sudden hypoxemia and atypical neurological symptoms, young orthopedic surgeons on duty and emergency department physicians should take these symptoms seriously and be highly suspicious of FES. These patients should be immediately transferred to the intensive care unit for life-supportive treatment.
- Citation: Yang J, Cui ZN, Dong JN, Lin WB, Jin JT, Tang XJ, Guo XB, Cui SB, Sun M, Ji CC. Early acute fat embolism syndrome caused by femoral fracture: A case report. World J Clin Cases 2021; 9(27): 8260-8267
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8260.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8260
Fat embolism syndrome (FES) is a rare disease characterized by respiratory distress, cerebral neurological symptoms and rash, is a serious threat to human life and health. Due to the lack of verifiable diagnostic criteria, the actual incidence of FES varies in different reports[1-3]. The most frequently used criteria are Gurd’s[4] and Gurd and Wilson’s[5], which require patients to meet at least one major criterion and at least four minor criteria for a diagnosis of FES. Here, we report a rare case of acute fat embolism that presented within 3 h after femoral fracture. The patient has recovered and has a good prognosis.
The chief complaints were severe pain in the left thigh and swelling with limited movement. The patient did not experience headache, dizziness, chest tightness or other discomfort.
A 29-year-old woman went to the emergency department of our hospital because of a car accident and was admitted to the orthopedic ward with a fracture of the middle and lower femur of the left lower limb.
The patient had no previous medical history.
The patient had no history of surgery, no bad habits such as smoking or drinking, and no history of food or drug allergies.
The patient had a body temperature of 36.5 ℃, pulse of 108 beats/min, respiratory rate of 20 breaths/min, blood pressure of 97/57 mmHg, and blood oxygen saturation of 100%. She had a clear mind and was in good spirits, her pupils were equal in size and sensitive to light, and she had a Glasgow Coma Scale (GCS) score of 15 points. No obvious abnormality was found on head and chest physical examination, and the results of the physical examination was consistent with femoral fracture. After admission, laboratory examinations (Table 1) were performed, fluids and pain relief were provided, and the patient was prepared for left tibial tubercle bone traction treatment.
| Variable | Reference range | 1.5 h after trauma | 3 h after trauma | 5 h after trauma |
| RBC, 1012/L | 3.8-5.1 | 3.86 | 3.73 | 2.54 |
| WBC, 109/L | 3.5-9.5 | 18.35 | 23.79 | 9.55 |
| HG level, g/L | 115-150 | 84.00 | 92.00 | 61.20 |
| HCT level, % | 35-45 | 28.70 | 29.70 | 19.82 |
| PLC, 109/L | 125-350 | 340.00 | 243.00 | 92.40 |
| ALT level, U/L | 7-40 | 19.10 | 21.30 | 18.70 |
| AST level, U/L | 13-35 | 26.20 | 29.30 | 45.00 |
| Total protein level, g/L | 65-85 | 66.30 | 49.20 | 41.30 |
| Albumin level, g/L | 40-55 | 41.60 | 29.10 | 26.50 |
| Arterial blood gas level | ||||
| Partial pressure of CO2, mmHg | 35-45 | 30.50 | 24.90 | |
| Partial pressure of O2, mmHg | 80-100 | 80.50 | 160.30 |
On admission, routine examination indexes were basically normal (1.5 h after trauma) and there were no obvious signs of fat embolism. Within a few hours, abnormal red blood cell counts, white blood cell counts, hemoglobin levels, and albumin levels and other indicators of progressive changes were observed (Table 1).
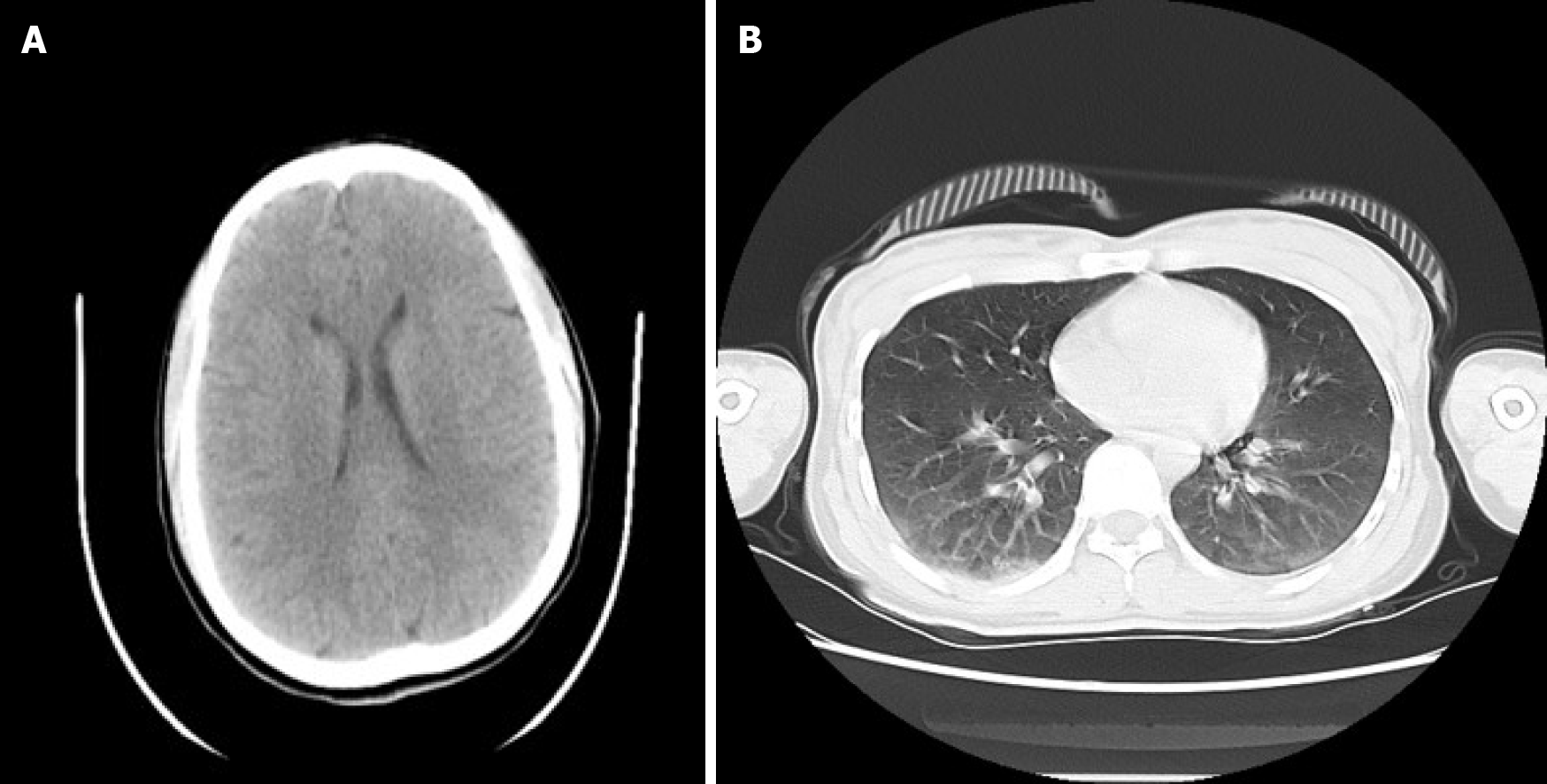
After X-ray examination, the patient was diagnosed with a fracture of the middle and lower part of the left femur and a fracture of the base of the left fifth metatarsal bone (Figure 1). After disturbance of consciousness, the results of computed tomography (CT) showed that there was no obvious abnormality in the skull but contusion of both lungs (Figure 2). After her condition was relatively stable, we performed ORIF on the femur (Figure 3).
Traumatic shock (compensatory period); fracture of the middle and lower part of the left femur; fracture of the base of the left fifth metatarsal bone.
Unfortunately, within 30 min of the patient being hospitalized, that is approximately two and a half hours after the injury, the patient’s consciousness gradually changed from awake to confused and poor. At that time, aggravation of shock, brain trauma and thoracic and abdominal organ injury had not been excluded. Urgent examination of the head, chest and abdomen by spiral CT (Figure 2B), and a plain scan of the head suggested no abnormality; however there were multiple contusions in both lungs and a reexamination was recommended.
At this time, the patient’s consciousness was still clouded, and she had to be asked to open her eyes. Her GCS score was 9. Continuous monitoring of vital signs, oxygen intake, and blood transfusions were performed, and fluids were provided to maintain water and electrolyte balance. Emergency blood gas analysis (Table 1) showed a partial pressure of carbon dioxide of 30.50 mmHg, partial pressure of oxygen of 80.50 mmHg, and oxygenation of 95.3%. Then, the patient experienced an increase in heart rate to 110-138 beats/min, an increase in respiratory rate to 25-36 beats/min, and a progressive decrease in blood oxygen saturation by 95%-78%, and the patient was found to be in a deep coma with a GCS score of 5. Endotracheal intubation and ventilator assistance was performed, and the patient was transferred to the intensive care department at midnight for further treatment. The therapy of patients in the intensive care unit was as follows: Central monitoring; endotracheal intubation; ventilator assistance; close observation of mental state and pupillary changes; early hormone treatment; supplementation with albumin, plasma, and concentrated red blood cells; maintenance of water and electricity balance; and other supportive treatment.
The patient remained in a coma, and her breathing was assisted by a ventilator. On the 3rd d after the injury, a typical bleeding point of a fat embolism appeared under the skin of her chest. On the 15th d, her vital signs were relatively stable, and the patient underwent definitive internal fixation of the fracture, taking into account the risk of fat embolism induced by intramedullary fixation. We chose open reduction and internal fixation (Figure 3). On the 27th d after the injury, the consciousness of the patient changed from coma to clouded. She gradually improved and then woke up on the 29th d after the injury. She was transferred to the rehabilitation department to continue functional limb exercise. Half a year after the injury, the brain and nervous system had no sequelae, her GCS score was 15, and her limb activity was basically normal. One year after the injury, the patient was followed up by telephone, and there were no complaints of discomfort.
FES refers to a clinical syndrome of systemic changes resulting from microcirculation embolism caused by free fat particles with a diameter of 10-40 μm entering the blood circulation through a ruptured vein after severe trauma[6]. The most common scenario is that the free fat particles in the bone marrow cavity after fracture are squeezed into the blood circulation and block the microcirculation of the brain, lung and other organs. It has been proven that orthopedic operations might induce FES during intramedullary fixation of long bone fractures. Repeated reaming, forced injection of an intramedullary needle and filling of bone cement during the operation may lead to FES. It has also been reported that fat embolism can occur during and after joint replacement[7]. The latest literature research shows that FES is most common in young men in the third decade of life following multiple leg fractures. FES may be more common after burst fracture[8]. However, our patient was a young woman with femoral fracture.
The pathophysiological mechanism of FES has not been fully elucidated. At present, it is generally believed that its pathogenesis mainly includes physical and mechanical mechanisms and biochemical mechanisms. In the case presented, both theories are applicable, as outlined below. Mechanical theory proposes that fat cells in the bone marrow gain access to venous sinusoids after trauma. These fat cells have potent proinflammatory and prothrombotic potential. They trigger rapid aggregation of platelets and accelerate fibrin generation as they travel through the venous system, eventually lodging in the pulmonary arterial circulation. Pulmonary capillary obstruction leads to interstitial hemorrhage and edema, alveolar collapse, and reactive hypoxemic vasoconstriction. Massive fat emboli may also lead to macrovascular obstruction and shock[9]. Fat cells may also enter the arterial circulation via a patent foramen ovale or directly through the pulmonary capillary bed, causing the characteristic neurological and dermatologic findings of FES[10].
Biochemical theory holds that the clinical manifestation of FES can be attributed to inflammatory reactions. Bone marrow fat is broken down by tissue lipase, resulting in high levels of triglycerides and toxic free fatty acids. Its toxic damage to pulmonary vascular endothelial cells can lead to angiogenesis, cytotoxic edema and bleeding. Damaged pulmonary vascular endothelial cells trigger a cascade of proinflammatory cytokines, leading to acute lung injury or acute respiratory distress syndrome[11]. This theory explains the delay from the occurrence of traumatic factors to the onset of clinical symptoms of a few hours to a few days. However, the timing of onset of our patient’s symptoms fits better with biochemical theory.
What was extraordinary and challenging in our case? First, our case is extremely rare, and the patient showed rapid progression within 3 h after the injury. Most FES cases occur between 12 and 72 h postinjury[12], and only a few cases have occurred within 12 h after injury[4]. According to the latest global report, the shortest amount of time between the occurrence of trauma and the development of a fat embolism is 55 minutes[13] (Table 2). Second, the presentation of FES is commonly nonspecific, making the diagnosis difficult. The most frequently used diagnostic criteria are Gurd’s and Wilson’s[5] (Table 3). However, our patient presented with acute respiratory failure without radiographic changes. There was no abnormality on CT scans of the brain. On the 3rd d after the injury, a typical bleeding point of a fat embolism appeared under the skin of her chest. In other words, none of the three main criteria seems to fully meet the diagnosis of FES. According to the statistics, the cause of death of many patients with explosive fat embolism can only be confirmed by autopsy. That is, fat particles are found in the blood vessels of the lung and brain tissue, which provides direct evidence for the diagnosis of FES[14]. Third, because it is difficult to diagnose, clinicians are particularly likely to mistakenly believe that craniocerebral injury or trauma and hemorrhagic shock cause symptoms and delay appropriate treatment. After the accident, we also had to rule out these shocks for our patient.
| Ref. | Age/gender | Latent period | Trauma | Outcome |
| Tsuru and Adachi[13] | 83/F | 55 min | Left distal femur fracture | Comatose and eventually died |
| Chen et al[17] | 31/M | 1 h | Right femoral and tibia fracture | Comatose and eventually died |
| Scarpino et al[18] | 17/M | 2 h | Right open femur and tibia fracture | Brain death on hospital day 2 |
| Our case | 29/F | 2.5 h | The middle and left femur fracture | After 29 d in a coma, she became conscious. Returned to work at 6 mo after trauma |
| You et al[19] | 54/M | 2 h 53 min | Multiple fracture (rib, clavicle, femur) and pulmonary contusion and pneumothorax | Brain death on hospital day 5 |
| Dillerud[20] | 25/M | 3 h | Right femur and left tibiofibular fracture | Minimal memory impairment |
| Millen et al[21] | 17/F | 4 h | Multiple fracture (rib, clavicle, femur, tibia, fibular, pubic rami, sacral ala) | After 2 mo in a coma, she was alert, oriented, following with progressively improving cognition |
| Xu et al[22] | 63/W | 4 h | Right tibia and fibula fractures | One month later, the patient was discharged from the hospital without any residual neurological deficit |
| Yang et al[23] | 46/W | 5 h | Left femur fracture | Patient consciousness was restored but language disorders were left |
| Cronin et al[24] | 26/M | 6 h | Right open tibiofibular shaft fracture | Returned to work at 3 mo after trauma |
| Paredes et al[4] | 54/M | 10 h | Multiple fractures: Femoral shaft, radius, patella, metatarsal | A residual mild cognitive impairment |
| Gurd’s criteria |
| Major criteria |
| Petechial rash |
| Respiratory symptoms with radiographic changes |
| Central nervous system signs unrelated to trauma or other condition |
| Minor criteria |
| Tachycardia |
| Pyrexia |
| Retinal changes (fat or petechiae) |
| Renal abnormalities (oliguria, anuria, or lipiduria) |
| Acute thrombocytopenia |
| Acute decrease in hemoglobin |
| High erythrocyte sedimentation rate |
| Fat globules in sputum |
In addition, it is important to consider that FES is not necessarily accompanied by organic changes in the brain tissue; CT scans of the brain may be normal, but brain magnetic resonance imaging is more sensitive in detecting FES[15]. During the CT examination, the patient showed abnormal vital signs, and emergency treatment was needed at this time. Thus, there was no time for a cerebral MRI.
There are currently no disease-specific treatments for FES. Supportive intensive care unit–level care is standard. Most patients are severely hypovolemic and require fluid resuscitation[10]. FES is then described as having a self-limiting course with management consisting predominantly of fracture fixation and supportive care[16]. After one month of symptomatic and supportive treatment, our patient finally achieved a satisfactory outcome.
Explosive fat embolism is rare and can be fatal; therefore, for patients with trauma and long shaft fractures of the extremities, if there are inexplicable brain symptoms in the early stage (after excluding brain trauma), young frontline doctors on duty in emergency and orthopedics departments should strongly suspect the possibility of explosive FES and transfer the patient from the general ward to the intensive care unit as soon as possible to facilitate rescue and supportive care.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Baguma M, Strainiene S S-Editor: Wang LL L-Editor: A P-Editor: Liu JH
| 1. | Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56:145-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 230] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Milroy CM, Parai JL. Fat Embolism, Fat Embolism Syndrome and the Autopsy. Acad Forensic Pathol. 2019;9:136-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Stein PD, Yaekoub AY, Matta F, Kleerekoper M. Fat embolism syndrome. Am J Med Sci. 2008;336:472-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Huang CK, Huang CY, Li CL, Yang JM, Wu CH, Chen CH, Wu PT. Isolated and early-onset cerebral fat embolism syndrome in a multiply injured patient: a rare case. BMC Musculoskelet Disord. 2019;20:377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Gurd AR, Wilson RI. The fat embolism syndrome. J Bone Joint Surg Br. 1974;56B:408-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 245] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Glover P, Worthley LI. Fat embolism. Crit Care Resusc. 1999;1:276-284. [PubMed] |
| 7. | Rosser K, Wilton S, Farrington WJ. Fat Embolism Syndrome: The Ambiguity of Diagnosis in the Postarthroplasty Patient: A Case Report. JBJS Case Connect. 2020;10:e1900594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Vetrugno L, Bignami E, Deana C, Bassi F, Vargas M, Orsaria M, Bagatto D, Intermite C, Meroi F, Saglietti F, Sartori M, Orso D, Robiony M, Bove T. Cerebral fat embolism after traumatic bone fractures: a structured literature review and analysis of published case reports. Scand J Trauma Resusc Emerg Med. 2021;29:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Husebye EE, Lyberg T, Røise O. Bone marrow fat in the circulation: clinical entities and pathophysiological mechanisms. Injury. 2006;37 Suppl 4:S8-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Kosova E, Bergmark B, Piazza G. Fat embolism syndrome. Circulation. 2015;131:317-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Paredes JC, Syquia JF, Chang AM, Zamuco JT. Fat embolism syndrome after shoulder hemiarthroplasty. J Shoulder Elbow Surg. 2011;20:e1-e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Meyer N, Pennington WT, Dewitt D, Schmeling GJ. Isolated cerebral fat emboli syndrome in multiply injured patients: a review of three cases and the literature. J Trauma. 2007;63:1395-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Tsuru S, Adachi H. Extremely Acute-Onset Cerebral Fat Embolism. Int J Gen Med. 2020;13:833-837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Zhou L, Mu J, Dong HM, Zhang J. [Forensic analysis of death caused by fat embolism: A study of 20 autopsy cases]. Fa Yi Xue Za Zhi. 2013;29:431-433. [PubMed] |
| 15. | Rothberg DL, Makarewich CA. Fat Embolism and Fat Embolism Syndrome. J Am Acad Orthop Surg. 2019;27:e346-e355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (1)] |
| 16. | Kwiatt ME, Seamon MJ. Fat embolism syndrome. Int J Crit Illn Inj Sci. 2013;3:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | Chen PC, Hsu CW, Liao WI, Chen YL, Ho CH, Tsai SH. Hyperacute cerebral fat embolism in a patient with femoral shaft fracture. Am J Emerg Med. 2013;31:1420.e1-1420.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Scarpino M, Lanzo G, Lolli F, Grippo A. From the diagnosis to the therapeutic management: cerebral fat embolism, a clinical challenge. Int J Gen Med. 2019;12:39-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | You JS, Kim SW, Lee HS, Chung SP. Use of diffusion-weighted MRI in the emergency department for unconscious trauma patients with negative brain CT. Emerg Med J. 2010;27:131-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Dillerud E. Abdominoplasty combined with suction lipoplasty: a study of complications, revisions, and risk factors in 487 cases. Ann Plast Surg. 1990;25:333-8; discussion 339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 113] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 21. | Millen JA, Watson C, Cain JM, Hagan J, Richards WT, Taylor D, Ang D, Clark JM. An Early Case of Fat Embolism Syndrome Occurring Following Polytrauma. Am Surg. 2021;87:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 22. | Xu XL, Xu P, Zheng RQ, Lin H, Chen QH. A Case of Cerebral Fat Embolism. Chin Med J (Engl). 2016;129:1761-1762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Yang L, Wu J, Wang B. Fat embolism syndrome with cerebral fat embolism through a patent foramen ovale: A case report. Medicine (Baltimore). 2020;99:e20569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Cronin KJ, Hayes CB, Moghadamian ES. Early-Onset Fat Embolism Syndrome: A Case Report. JBJS Case Connect. 2018;8:e44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |