Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8192
Peer-review started: April 23, 2021
First decision: June 6, 2021
Revised: June 30, 2021
Accepted: August 3, 2021
Article in press: August 3, 2021
Published online: September 26, 2021
Processing time: 146 Days and 0.3 Hours
Abnormal systemic artery to the left lower lobe is a rare congenital abnormality characterized by anomalous communication between the systemic and pulmonary circulation. Owing to its rarity, there is limited clinical experience with respect to the diagnosis and treatment of this disease.
We report a 60-year-old man who presented with a history of hemoptysis for 20 d. Contrast-enhanced computed tomography of the chest confirmed the diagnosis of abnormal systemic artery to the left lower lobe, and surgical treatment was performed. The aberrant artery arising from the descending thoracic aorta was ligated, followed by removal of the left lower lobe. The patient showed good recovery and was discharged 6 d after the surgery. At the 1-year follow-up, the patient had recovered completely, and lung CT showed no abnormal findings.
We present a case of abnormal systemic artery to the left lower lobe that was successfully managed by surgical resection of the aberrant artery and the left lower lobe. This case report adds to the clinical experience of diagnosing and treating this rare entity.
Core Tip: Abnormal systemic artery to the left lower lobe is a rare congenital vascular malformation. Experience in diagnosis and treatment remains limited. Here we pre
- Citation: Zhang YY, Gu XY, Li JL, Liu Z, Lv GY. Surgical treatment of abnormal systemic artery to the left lower lobe: A case report . World J Clin Cases 2021; 9(27): 8192-8198
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8192.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8192
Abnormal systemic artery to the left lower lobe (ASALLL) is a rare congenital anomaly that creates an anomalous communication between the systemic and the pulmonary circulation[1]. It is characterized by aberrant systemic arterial blood flow to the left lower lobe of the lung, which drains into the pulmonary vein[1,2]. Owing to its rarity, only a few reports have described this entity. Hemoptysis is the most common manifestation, while some patients may exhibit no symptoms; in rare cases, patients may develop fever and cough with or without expectoration[2-4]. Surgical resection or therapeutic embolization are the main treatment modalities, while some cases may require vascular reconstruction[2,5,6]. We report a senile patient with ASALLL who was successfully treated by surgical resection. In addition, we summarize the diag
A 60-year-old man was admitted to our hospital in October 2019 with a chief com
The symptoms started 20 d ago with no obvious cause of hemoptysis.
The past history was unremarkable apart from a history of appendicectomy. The patient was otherwise healthy and had no history of hypertension, diabetes mellitus, coronary heart disease or infectious disease.
The patient is a life-long non-smoker. He denied any family history of related diseases.
The general condition of the patient at presentation was good. His vital signs were normal with stable hemodynamic status. Breath sounds were clear, and no pulmonary crackles were detected on auscultation.
The laboratory parameters of the patient were almost normal.
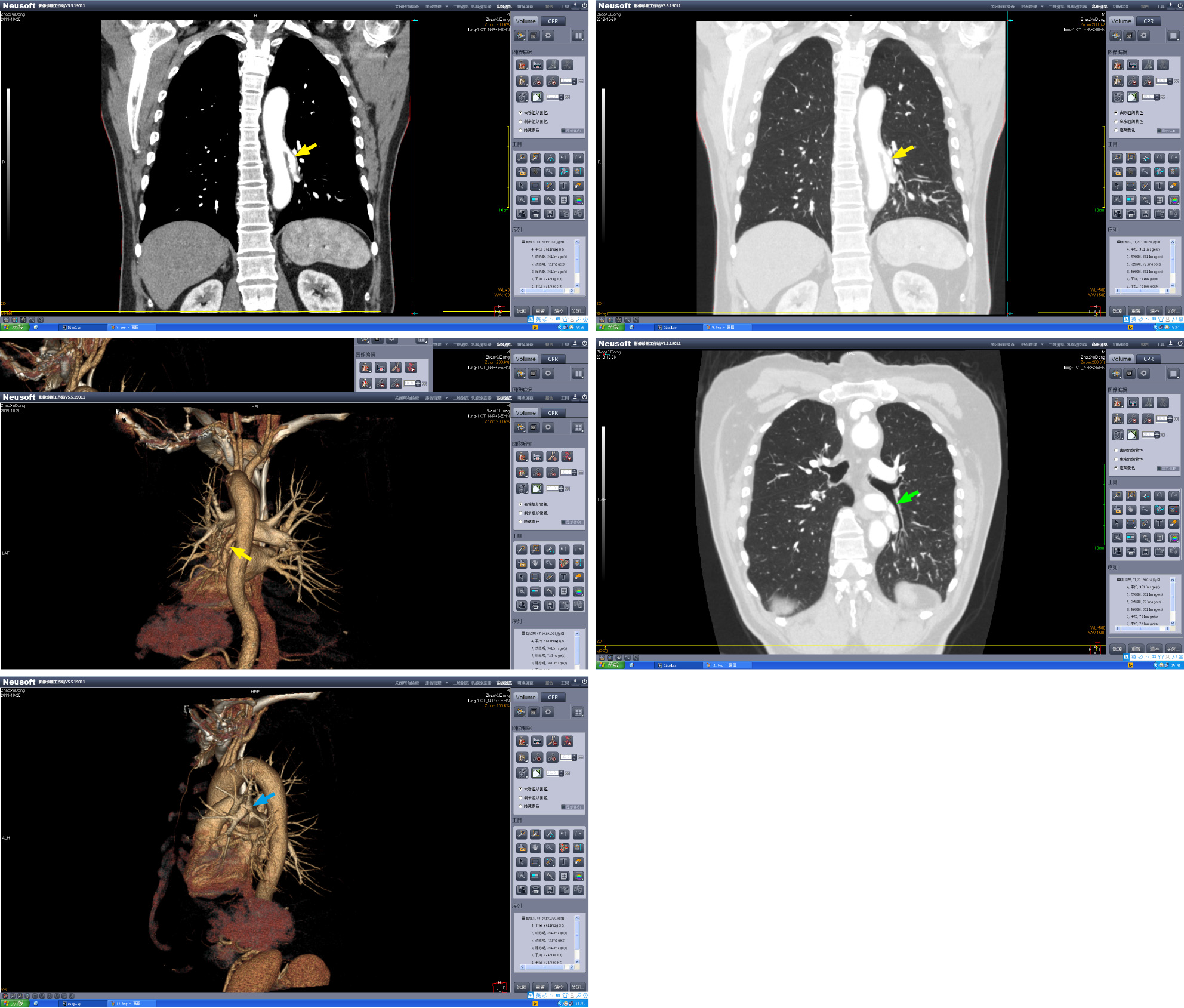
Pulmonary contrast-enhanced computed tomography (CT) with three-dimensional reconstruction performed immediately after admission revealed an aberrant vessel supplying the left lower lung lobe (Figure 1); its origin was traced to the descending thoracic aorta. At the same time, pulmonary artery of the left lower lobe of the lung was absent. There were no abnormalities in the left lower pulmonary vein or in the bronchus of the left lower lobe of the lung.
The potential differential diagnoses in this case were ASALLL and pulmonary sequestration (PS). The corresponding pulmonary artery is usually absent in ASALLL, but the bronchus is usually normally developed. PS is characterized by the absence of normal communication with the bronchial tree, which helps differentiate it from ASALLL. The final diagnosis of the presented case was ASALLL.
Routine preoperative workup did not reveal any other abnormality, and the patient underwent surgical treatment in November 2019. After general anesthesia and intubation with double lumen tube, the thoracic cavity was opened via the fifth intercostal space. An anomalous systemic artery arising from the thoracic aorta and supplying blood to the left lower lobe was identified during surgery; the anomalous artery was ligated by vascular stapler and subsequently sutured. The pulmonary artery supplying the left lower lobe was absent, while the corresponding pulmonary artery and bronchus were normal and were all sundered during the removal of the left lower lobe. The surgery was uneventful, and the thoracic cavity was closed after the placement of a closed drainage tube.
The patient showed good recovery and was discharged after removal of the drainage tube 6 d after the surgery. At the 1-year follow-up, the patient had recovered com
ASALLL is a rare congenital arterial malformation that is relatively more common in the Asian population[7]. Pathologically, an aberrant artery originates from the de
We conducted a literature search in the PubMed database for all papers written in English utilizing the search term: “Abnormal Systemic Artery to the Left Lower Lobe.” A total of 82 previous cases published since 1976 were retrieved. A summary of the 83 cases (including the present case) is presented in Table 1. Among these, 59% of pa
| Yr | Author | n | Age in yr | Symptoms | Treatment | Follow-up | Complication |
| 1976 | Kirks | 2 | 6 mo | Asymptomatic | Lobectomy | - | - |
| 17 mo | Asymptomatic | Lobectomy | |||||
| 1979 | Ishihara | 1 | 5 | Asymptomatic | Lobectomy | - | - |
| 1981 | Yabek | 1 | 6 mo | Tachypnea | Lobectomy | 6 mo | None |
| 1992 | Tao | 1 | 38 | Dyspnea | Lobectomy | - | - |
| 1993 | Kurosaki | 3 | 59 | Hemoptysis | - | - | - |
| 54 | Asymptomatic | Lobectomy | |||||
| 46 | Asymptomatic | Segmentectomy | |||||
| 1996 | Hirai | 2 | 29 | Hemoptysis | Lobectomy | 6 mo | None |
| 30 | Asymptomatic | Anastomosis | |||||
| 1999 | Yamanka | 2 | 46 | Cough | Lobectomy | - | - |
| 68 | Dyspnea, hemoptysis | Segmentectomy | |||||
| 2000 | Ko | 3 | 39 | Hemoptysis | Lobectomy | 9 mo | None |
| 58 | Asymptomatic | None | 6 mo | None | |||
| 47 | Pain, hemoptysis | None | 2 yr | Chest pain | |||
| 2001 | Ashizawa | 5 | 29 | Asymptomatic | Surgery (5) | - | - |
| Asymptomatic | |||||||
| Asymptomatic | |||||||
| Dyspnea | |||||||
| Hemoptysis | |||||||
| 2002 | Kim | 11 | 49 | Asymptomatic (11) | None (11) | - | - |
| 2003 | Iizasa | 4 | 50 | Asymptomatic | Segmentectomy | - | - |
| 17 | Hemoptysis | Segmentectomy | |||||
| 43 | Hemoptysis | Segmentectomy | |||||
| 20 | Asymptomatic | Lobectomy | |||||
| 2004 | Haraguchi | 1 | 29 | Hemoptysis | Lobectomy | - | - |
| 2006 | Saida | 1 | 41 | Hemoptysis | Embolization | 6 yr | Chest pain for 1 mo |
| 2008 | Albertini | 1 | 21 | Dyspnea, hemoptysis | Lobectomy | - | - |
| 2008 | Wu | 1 | 24 | Hemoptysis | None | 2.5 yr | Hemoptysis |
| 2009 | Wong | 1 | 10 mo | Tachypnea | Lobectomy | - | - |
| 2009 | Lim | 1 | 26 | Hemoptysis, chest pain | Embolization | 6 mo | None |
| 2011 | Jiang | 4 | 33 | Hemoptysis | Embolization | 2 wk | 2 patients with chest pain for 2 wk |
| 28 | Hemoptysis | Embolization | |||||
| 24 | Hemoptysis | Embolization | |||||
| 19 | Hemoptysis | Embolization | |||||
| 2011 | Abe | 1 | 24 | Hemoptysis | Embolization | 1 yr | None |
| 2011 | Canyigit | 1 | 53 | Chest pain | Embolization | 10 mo | Chest pain for 1 wk |
| 2012 | Anil | 1 | 23 | Hemoptysis | Embolization | 6 mo | Chest discomfort for 2 d |
| 2013 | Higuchi | 1 | 58 | Asymptomatic | Segmentectomy | - | - |
| 2013 | Sugihara | 1 | 67 | Fatigue | Embolization | 9 mo | None |
| 2015 | Kawaguchi | 1 | 25 | Hemoptysis | Ligation | 4 yr | None |
| 2015 | Qin | 16 | 23 | Hemoptysis (16), Cough (4), Sputum (2) | - | - | - |
| 2016 | Jiang | 91 | 32.7 | Hemoptysis (9) | Embolization (9) | 42.1 mo | 4 patients with chest pain for weeks |
| 2017 | Miller | 1 | 2 mo | Tachypnea | Anastomosis | 6 wk | None |
| 2018 | Thakur | 1 | 18 | Hemoptysis | Ligation | 6 wk | None |
| 2018 | Kim | 1 | 7 mo | Asymptomatic | Anastomosis | 3 yr | None |
| 2020 | Utsumi | 1 | 42 | Asymptomatic | Lobectomy | 6 mo | None |
| 2020 | Hu | 1 | 53 | Hemoptysis | Medical treatment | - | - |
| 2021 | Ema | 1 | 39 | Asymptomatic | Segmentectomy | 2 mo | None |
| 2021 | Current case | 1 | 60 | Hemoptysis | Lobectomy | 1 yr | None |
The blood pressure in the systematic circulation is considerably higher than that in the pulmonary circulation; therefore, perfusion of pulmonary tissue by the systematic circulation can result in alveolar bleeding, leading to hemoptysis[9]. As hemoptysis can also occur in PS[10], the differentiation between ASALLL and PS relies on further investigations. Contrast-enhanced chest CT with three-dimensional reconstruction is the main modality for diagnosis of ASALLL, as it can easily delineate the aberrant artery supplying the left lower lobe[1]. However, differentiation of ASALL from PS based on CT findings can be challenging, as both conditions exhibit similar arterial malformation. In a study, the diameter of the abnormal artery of ASALLL was significantly greater than that of PS (11.88 ± 1.13 mm vs 5.96 ± 0.98 mm), which can facilitate differentiation between the two conditions on CT[11]. Moreover, patients with ASALLL commonly exhibit ground-glass opacity on CT, which is attributable to alveolar bleeding; in contrast, the typical manifestation of PS on CT scan is solid or solid-cystic mass, which is attributable to coinfection[11].
Persistent communication between the systematic circulation and the pulmonary circulation in the pulmonary tissue results in a series of consequences such as alveolar hemorrhage, increase in cardiac load and impaired oxygenation. The therapeutic goal for this disease is to correct the left-to-right shunt, which can be achieved by pul
ASALLL is a rare congenital vascular malformation with limited knowledge about its diagnosis and treatment. Our experience in the management of ASALLL highlights the importance of contrast-enhanced computed tomography in the diagnosis of this disease. Specifically, ASALLL needs to be differentiated from PS as these two con
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Naseer M S-Editor: Zhang H L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Ashizawa K, Ishida Y, Matsunaga N, Otsuji H, Sakamoto I, Hayashi K. Anomalous systemic arterial supply to normal basal segments of left lower lobe: characteristic imaging findings. J Comput Assist Tomogr. 2001;25:764-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Miller JR, Lancaster TS, Abarbanell AM, Manning PB, Eghtesady P. Anomalous Systemic Artery to the Left Lower Lobe: Literature Review and a New Surgical Technique. World J Pediatr Congenit Heart Surg. 2018;9:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Yamanaka A, Hirai T, Fujimoto T, Hase M, Noguchi M, Konishi F. Anomalous systemic arterial supply to normal basal segments of the left lower lobe. Ann Thorac Surg. 1999;68:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 89] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Yan M, Khan A, Cheng G. The abnormal systemic artery to the left lower lobe (ASALLL): a report of two cases. Radiol Case Rep. 2020;15:1960-1964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Saida T, Ninomiya H, Hojo F, Nakayama M, Yamauchi T, Saida Y. Systemic arterial supply to the normal basal segments of the left lower lobe treated by coil embolization, with long-term follow-up. Radiat Med. 2006;24:365-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Lim HH, Huh JK, Kim JH, No HS, Choe du H, Kim CH, Lee JC. Therapeutic embolization of systemic arterial supply to normal basal segments of the left lower lobe of the lung. Respirology. 2009;14:606-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Wu KA, Wu CP, Perng WC. Ethnicity relation to anomalous systemic arterial supply to normal basal segments of the left lower lobe. Clin Imaging. 2008;32:477-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Alizadeh E, Suliman H. Intralobular pulmonary sequestration. JBR-BTR. 2013;96:208-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Mautone M, Naidoo P. A case of systemic arterial supply to the right lower lobe of the lung: imaging findings and review of the literature. J Radiol Case Rep. 2014;8:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Ellis J, Brahmbhatt S, Desmond D, Ching B, Hostler J. Coil embolization of intralobar pulmonary sequestration - an alternative to surgery: a case report. J Med Case Rep. 2018;12:375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Qin J, Wang XL, Bai MJ, Huang SH, Chen XZ, Shan H. Comparison of anomalous systemic artery to left lower lobe and pulmonary sequestration in left lower lobe by computed tomography. Acta Radiol. 2015;56:1100-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kim DW, Jeong IS, Kim JH, Kim YH, Cho HJ. Operation for an anomalous systemic arterial supply to the left lower lobe using an anastomosis procedure in an infant. J Thorac Dis. 2018;10:E301-E303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Abe T, Mori K, Shiigai M, Okura N, Okamoto Y, Saida T, Sakai M, Minami M. Systemic arterial supply to the normal basal segments of the left lower lobe of the lung--treatment by coil embolization--and a literature review. Cardiovasc Intervent Radiol. 2011;34 Suppl 2:S117-S121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Jiang S, Yu D, Jie B. Transarterial Embolization of Anomalous Systemic Arterial Supply to Normal Basal Segments of the Lung. Cardiovasc Intervent Radiol. 2016;39:1256-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Jaspers R, Barendregt W, Limonard G, Visser F. Necessary resection of the left lower lobe due to systemic arterial supply. J Thorac Cardiovasc Surg. 2007;133:1384-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Iizasa T, Haga Y, Hiroshima K, Fujisawa T. Systemic arterial supply to the left basal segment without the pulmonary artery: four consecutive cases. Eur J Cardiothorac Surg. 2003;23:847-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |