Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7944
Peer-review started: May 12, 2021
First decision: June 15, 2021
Revised: July 1, 2021
Accepted: July 19, 2021
Article in press: July 19, 2021
Published online: September 16, 2021
Processing time: 121 Days and 6.4 Hours
Reports on peripherally inserted central catheter (PICC) placement in neonates with persistent left superior vena cava (PLSVC) are rare. The majority of PLSVC patients have no clinical symptoms or hemodynamic changes, which are usually detected during cardiac catheterization, cardiac pacemaker implantation, or PICC placement. However, in neonates with PLSVC, PICC placement can be cha
This article introduces the concept of the “TIMB” bundle. After PICC implantation, we found PLSVC in all eight patients. The key points of care regarding PICC placement in neonates with PLSVC included “TIMB”, where “T” indicates a reasonable choice of the catheterization time, “I” refers to a retrospective analysis of imaging data before catheterization, “M” refers to correct measurement of the body surface length, and “B” indicates that the tip of the PICC is placed in the middle and lower 1/3 of the left superior vena cava under the guidance of B-ultrasound.
“TIMB” is a bundle for PICC placement in neonates, especially for those with PLSVC. Using this new approach can improve the first-attempt success rate of PICC placement, reveal cardiovascular abnormalities in advance, allow the selection of different measurement methods reasonably according to the puncture site, and finally, improve the accuracy of catheter positioning through the use of B-ultrasound guidance.
Core Tip: We report rare cases of persistent left superior vena cava in neonates in whom peripherally inserted central catheter placement was difficult. We faced unprecedented difficulties and challenges during the process of catheterization; several conventional methods were used. Finally, we successfully established a new approach of tube placement, that is, “TIMB”, where “T” indicates time, “I” refers to imaging data, “M” refers to measurement, and “B” indicates B-ultrasound.
- Citation: Chen Q, Hu YL, Li YX, Huang X. Peripherally inserted central catheter placement in neonates with persistent left superior vena cava: Report of eight cases. World J Clin Cases 2021; 9(26): 7944-7953
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7944.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7944
Persistent left superior vena cava (PLSVC) is a common systemic venous malformation identified in 10% of people with congenital heart defects[1]. PLSVC is caused by the failure of the proximal part of the left anterior main vein[2]. The majority of PLSVC patients have no clinical symptoms or hemodynamic changes, which are usually detected during cardiac catheterization, cardiac pacemaker implantation, or peripherally inserted central catheter (PICC) placement[3]. In the neonatal intensive care unit (NICU), the indications for PICC placement in neonates generally include the following[4]: (1) Very low birth weight; (2) Infusion of enteral nutrient solution for ≥ 5 d; (3) Intravenous infusion of hypertonic solution (> 600 mOsm/L); and (4) Intra
PLSVC is divided into four types. In patients with type I PLSVC, which accounts for approximately 90% of all PLSVC cases, when the tip is in the correct position, the catheter can continue to be used because these patients have no other cardiovascular abnormalities[5]. Because PICC liquid exosmosis is inversely proportional to the diameter of the vessel[6], the PLSVC diameter can be judged by B-ultrasound. If the left superior vena cava lumen is obviously larger than the right superior vena cava lumen or the difference between the two is not significant, the PICC can continue to be used. If the left superior vena cava lumen is obviously smaller than the right superior vena cava lumen, the PICC should be removed as soon as possible[7]. Types II, III, and IV PLSVC accounts for approximately 10% of all patients[5], and right-to-left shunting of venous blood into the left atrium can easily lead to an embolism. Moreover, air on the left side of the heart, even as little as 0.5 mL, and direct entry into the systemic circulation can also cause a fatal embolism[8]. It is difficult to clear tiny air bubbles in the infusion line during clinical transfusion; to ensure the safety of these patients, the PICC should be removed immediately and reinserted from the right side or lower limb[8]. Solitary PLSVC accounts for approximately 0.1% of all PLSVC cases and is accompanied by the absence of the right superior vena cava[9]. A PICC can be used when the size of the left superior vena cava lumen is suitable and the position of the end of the catheter is normal[7].
Here, we report rare cases of PLSVC in neonates at NICUs in Chengdu, Sichuan Province, China, in whom PICC placement was difficult. In these cases, we faced unprecedented difficulties and challenges during the process of catheterization that were successfully overcome following application of a new approach. Therefore, we introduce the concept of the “TIMB” bundle, which has seldom been mentioned in previous studies and might be used for PICC placement in neonates with PLSVC.
We describe the clinical data and method of central catheter insertion in eight newborns with PLSVC who underwent PICC placement between January 2017 and June 2020.
A total of 2287 patients underwent PICC placement at the Neonatal Department of West China Second University Hospital of Sichuan University between January 2017 and June 2020. Eight patients (0.35%) required a new approach for PICC placement as they were diagnosed with PLSVC. The general data of these eight patients are shown in Table 1.
| Male: female (patients) | Gestational age (W) | Birth weight (g) | Age at PICC placement | Number of PICC procedures | ||||||||
| < 28 | 28-31+6 | 32-36+6 | > 37 | < 1 000 | 1000-1499 | 1500-2499 | ≥ 2500 | ≤ 24 h | > 24 h | For the first time | For the second time | |
| 5:5 | 1 | 3 | 3 | 1 | 2 | 3 | 2 | 1 | 5 | 3 | 7 | 1 |
PLSVC was not diagnosed in seven patients (except for patient 5) before the first catheterization, and PLSVC was first detected by chest X-ray after catheterization and then confirmed by B-ultrasound. Among the eight patients, two (patients 2 and 6) had congenital malformations of the digestive tract and were treated surgically, and three (patients 3, 4, and 5) had a congenital heart defect. B-ultrasound showed that seven patients had no right-to-left shunt, and one (patient 8) had a right-to-left shunt (Table 2).
| Serial number | Date of admission | Gestational age (W) | Birth weight (g) | Primary diagnosis | Age at PICC placement | Number of PICC procedures | Weight (g) | Puncture site | Placement length (cm) | First tip positioning | Adjustment situation | Reposition | Days of PICC indwelling (d) |
| Patient 1 | May 22, 2017 | 32 | 1310 | Preterm, very low birth weight | 20 h | 1 | 1310 | Left basilic vein | 13.5 | T9 | Pull out 2.7 cm | T5-6 | 8 |
| Patient 2 | July 13, 2017 | 40+2 | 2650 | Postoperative esophageal atresia | 10 d | 1 | 2970 | Left axillary vein | 10 | T7-8 | Pull out 0.5 cm | T6 | 15 |
| Patient 3 | March 18, 2018 | 29+3 | 1200 | Preterm, very low birth weight, patent ductus arteriosus | 1 d | 1 | 1200 | Left basilic vein | 12.5 | T8 | Pull out 0.8 cm | T5-6 | 18 |
| Patient 4 | November 9, 2018 | 34+1 | 975 | Preterm, very low birth weight, atrial septal defect | 1 d | 1 | 975 | Left basilic vein | 12 | T5-6 | — | — | 39 |
| Patient 5 | December 3, 2018 | 27+2 | 880 | Preterm, very low birth weight, patent ductus arteriosus, tricuspid regurgitation (moderate) | 32 d | 2 | 1425 | Left median vein | 11 | T6 | — | — | 10 |
| Patient 6 | December 26, 2018 | 36+4 | 2250 | Postoperative esophageal atresia, preterm, low birth weight | 3 d | 1 | 2640 | Left superficial temporal vein | 12.5 | T6 | — | — | 6 |
| Patient 7 | February 3, 2019 | 30+6 | 1220 | Preterm, very low birth weight | 1 d | 1 | 1220 | Left basilic vein | 12.5 | T9 | Pull out 2.5 cm | T5 | 6 |
| Patient 8 | February 3, 2019 | 30+2 | 1500 | Preterm, low birth weight | 5 h | 1 | 1503 | Left axillary vein | 8 | T8 | The lumen of the left superior vena cava was obviously smaller than that of the right superior vena cava, so the PICC was removed on the same day. The patient was scheduled for catherization through a lower extremity vein, but the family abandoned treatment 12 h after admission | ||
A member of the PICC team (composed of registered nurses who have professional PICC knowledge, have passed skills training, have passed the assessment for qualification for PICC insertion, and have at least 5 years of clinical work experience[10]) placed a 1.9-Fr PICC (1.9 Fr, single lumen, Vascu-PICC, Medcomp, Inc., Harleysville, PA, United States). In all patients, PICC placement was performed in accordance with the standard procedures described in the 2016 Infusion Therapy Standards of Practice[6].
All patients were located with a bedside chest X-ray machine (Philips, PRACTIX 33 plus) after a successful puncture, and the positioning criteria were based on Practice of Neonatology, 5th Edition[5], as follows: (1) Chest X-ray positioning: The baby was placed in the supine position with the head in the center and the upper limbs on both sides of the body; (2) upper limb/head venous catheterization: The tip of the PICC was located at 1/3 of the inferior segment of the superior vena cava (at approximately the level of 4th-6th thoracic vertebrae); and (3) lower limb venous catheterization: The tip of the PICC was located in the inferior vena cava (at approximately the level of 9th-11th thoracic vertebrae or 4th-5th lumbar vertebrae).
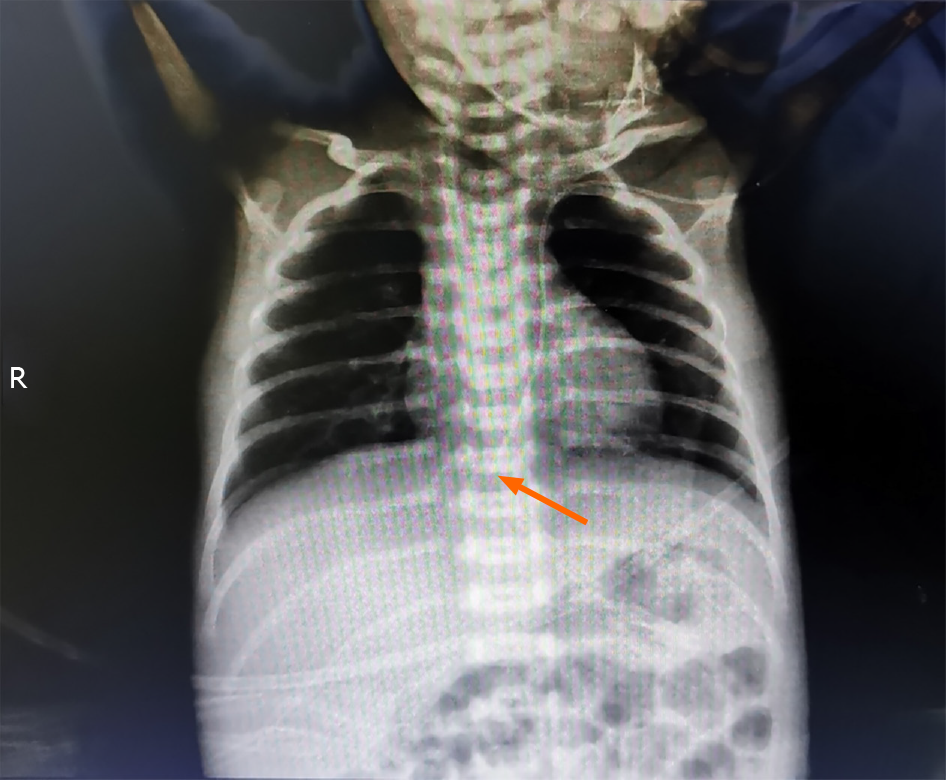
In all eight patients, chest X-rays showed that the catheter descended along the left side of the vertebral column after PICC insertion (Figure 1). It should be considered that the catheter may enter the left thoracic blood vessel (such as the branch of the left internal mammary artery) through other ways[1]. Therefore, a small amount of blood was collected at the PICC for blood analysis, and all results were normal. Blood analysis indicated venous blood in all cases.
On the day of PICC insertion, chest X-ray showed that the PICC was located in the left thoracic cavity in all patients (Figure 1), which was different from that in normal patients (Figure 2). Chest X-ray showed that the tip was positioned at the level of the 9th thoracic vertebra in two patients (patients 1 and 7), the 8th thoracic vertebra in two (patients 3 and 8), the 7th-8th thoracic vertebrae in one (patient 2), and the 5th-6th thoracic vertebrae in another three (patients 4, 5, and 6) (Table 2).
The diagnoses of all patients except for the PLSVC are shown in Table 2.
We summarize our treatment for these cases as the “TIMB” bundle.
The position of the PICC tip was determined by bedside B-ultrasound after chest X-ray localization. Except for three patients (patients 4, 5, and 6) in whom the catheter tip was in a proper position, the catheter tip position in the remaining four patients (patients 1, 2, 3, and 7) was retreated to the middle and lower parts of the left superior vena cava under the guidance of B-ultrasound. In one patient (patient 8), B-ultrasound showed type II PLSVC, with right-to-left shunting, and the lumen of the left superior vena cava was significantly smaller than that of the right superior vena cava. Therefore, the PICC was removed on the same day as advised by the doctor, and recatheterization through a lower extremity vein was planned, but 12 h after admission, the patient’s parents asked that the baby be discharged.
No PICC-related complications, such as arrhythmia or cardiac tamponade, were found in seven patients who were scheduled for catheter removal after 6 to 39 d of indwelling. The details of PICC placement in this group are shown in Table 2.
On January 15, 2019, patient 4 was treated by interventional surgery in the cardiovascular department due to atrial septal defect, and the patient recovered well after the operation. On April 23, 2019, patient 5 was hospitalized in the respiratory department due to mycoplasma pneumonia and was discharged on May 7. Several other patients did not require readmission, and to date, all children have continued to grow well.
Time: On the day of birth, most neonates are still adapting to the external environment, accompanied by varying degrees of edema[5], and in this study, the neonates with PLSVC were not diagnosed before catheterization; if the PICC is placed early after birth, the first-attempt success rate will be reduced. Therefore, a reasonable time for PICC placement should be selected at least 24 h after birth, except for under special circumstances, such as rescue.
Imaging data: The comprehensive evaluation of imaging data before PICC placement plays a vital role in the determination of the puncture site. If a prenatal examination is regularly performed, fetal cardiovascular abnormalities can be discovered in a timely manner, and prenatal ultrasound plays a vital role in the diagnosis of PLSVC. Thus, a retrospective analysis of imaging data should be performed before catheterization.
Measurement: The body surface length should be correctly measured. For some neonates in a critical condition who need hypertonic and irritant drugs within 24 h after birth, central venous access must be established as soon as possible, and it is recommended to select the veins of both lower limbs[4], the right upper extremity, or right head and neck if possible. The body surface length was measured in the same manner as in normal infants, that is, from the prepuncture point along the vein to the right sternoclavicular joint and down to the 1/2 intercostal space. In patients who were diagnosed with PLSVC by B-ultrasound before PICC placement, when a left-side puncture was required due to vascular conditions, the body surface length was measured from the left puncture point along the vein to the left sternoclavicular joint plus 0.5 cm.
B-ultrasound: The tip of the PICC was placed in the middle and lower 1/3 of the left superior vena cava under the guidance of B-ultrasound. Through exploration of the PICC placement approach in patients with PLSVC, we suggest that PICC placement be performed under the guidance of B-ultrasound if a B-ultrasound or chest X-ray examination is not performed before PICC placement.
The catheter tip in four patients (patients 1, 2, 3, and 7) was withdrawn to be positioned in the middle and lower parts of the left superior vena cava under the guidance of B-ultrasound. The PICC was withdrawn outward under the guidance of B-ultrasound 2.7 cm in patient 1, 0.5 cm in patient 2, 0.8 cm in patient 3, and 2.5 cm in patient 7. The catheter tip was properly positioned in the remaining three patients (patients 4, 5, and 6).
When PICC placement is performed in patients with PLSVC, because the internal environment of premature infants is not stable, the blood vessel wall is thin, and the permeability is strong[5], if the catheter tip fails to reach the superior vena cava during catheterization, catheter exudation may occur. Moreover, on the day of birth, most neonates are still adapting to the external environment, accompanied by varying degrees of edema, and in this study, the neonates with PLSVC were not diagnosed before catheterization; if the PICC is placed early after birth, the first-attempt success rate will be reduced. Therefore, appropriate timing of catheterization is particularly important. On the other hand, because some examinations have not been completed, it will directly affect the overall assessment of PICC placement, thus increasing the risk of catheterization. Finally, we have summarized a great deal of experience with PICC placement failure on the first day after birth. Therefore, it is suggested that the best time for PICC placement should be 24 h after birth. In our study, five patients were in urgent need of hyperosmotic and irritant drugs within 24 h after birth due to their critical condition. After a full evaluation by the PICC team, the patients underwent catheter placement within 24 h after birth. Because PLSVC is not an absolute contraindication for PICC placement, B-ultrasound is not performed routinely before catheterization. After catheterization, the PICC tip was positioned deeper in four patients (patients 1, 2, 3, and 7). Two patients (patients 6 and 2) were stable and did not require hyperosmotic and irritant drugs within 24 h after birth. Although B-ultrasound screening was not routinely performed, the difficulty of catheterization was reduced because the PICC was placed on the 3rd day and 10th day after birth. The position of the catheter tip was deeper in one patient (patient 2) and at a suitable position in another patient (patient 6). One patient (patient 5) underwent a second catheterization procedure 32 d after birth. This patient was diagnosed with PLSVC using B-ultrasound before catheterization, which confirmed that the tip of the catheter was placed in the correct position.
A comprehensive evaluation of imaging data before PICC placement plays a vital role in the judgment of the puncture site. If a prenatal examination is regularly performed, fetal cardiovascular abnormalities can be discovered in a timely manner. Prenatal ultrasound plays a vital role in the diagnosis of PLSVC[3]. Moreover, some patients may undergo echocardiography and/or chest X-ray within 24 h after birth. If abnormal anatomical structures of the heart vessels are found, such as PLSVC, dextrocardia, and single atrium, PICC placement can be accurately planned, including the selection of the puncture site, and measurement of the body surface length, direction of the catheter, and tip location. B-ultrasound and/or chest X-ray should be performed before PICC placement to avoid the adverse effects caused by PLSVC.
Because catheter heterotopia in the left superior vena cava often occurs when a catheter is inserted through the left limb[11], left upper extremity and left head and neck vein catheterization should be avoided in newborns with confirmed PLSVC. In our study, patient 5 was diagnosed with PLSVC by B-ultrasound before the second catheterization and was treated for 32 d in another hospital. Considering that there was no suitable vessel on the right side or in either lower limb for catheterization, the left median cubital vein was chosen. For similar cases, catheterization should be performed from the left upper limb and left head or neck, considering that the catheter will descend down the left side of the vertebral column (left superior vena cava) and that the path of the vessel is shorter than the right superior vena cava across the spine and down the right side. In these patients, the descending path of the catheter is shorter than the descending route of the right superior vena cava on the right side across the vertebral column[11]. Therefore, the body surface length was measured from the left puncture point along the vein to the left sternoclavicular joint plus 0.5 cm. Chest X-ray and B-ultrasound showed that the tip of the catheter was in the correct position, at the level of the 6th thoracic vertebra and lower 1/3 of the left superior vena cava, respectively.
For some neonates in a critical condition, the use of hypertonic and irritant drugs is urgently needed within 24 h after birth, and central venous access must be established as soon as possible; however, there were no diagnoses of PLSVC at this time in this study. Thus, it is recommended to choose lower limb veins[4]. The surface length was measured in the same manner as under normal conditions. In our study, in all eight patients, the mother had not received regular prenatal examinations at our hospital and presented to our hospital for emergency obstetric delivery due to a high-risk pregnancy. Among these neonates, five with PLSVC did not undergo bedside B-ultrasound and chest X-ray within 24 h after birth; additionally, all of the neonates had edema of varying degrees in the whole body and limbs, and the vessels were not well exposed. After failing to puncture veins in both lower limbs, the right basilic vein, and the right axillary vein, the PICC team chose to place the catheter from the left upper limb. The surface length was measured as in normal newborns, and all PICCs were located along the left side of the vertebral column. Among the patients, the PICC tip was too deep in four newborns. Finally, PLSVC was confirmed by bedside B-ultrasound. Therefore, PICC placement should be performed under the guidance of B-ultrasound if a B-ultrasound or chest X-ray examination is not performed before PICC puncture. We have changed our practice based on the conclusions that we made from this study. Now, when we encounter neonates who urgently require PICC placement, the PICC team usually evaluates the blood vessel first, and if placement may be difficult or if a B-ultrasound or chest X-ray examination is not performed before PICC placement, we will perform the procedure under B-ultrasound guidance.
Chest X-ray after catheterization showed that the catheter was located in the left side of the thoracic cavity, which was different from the location in normal patients. Factors of malposition should be excluded first. The PICC team usually considers that the catheter can accidentally enter the left thoracic vessel through a branch of the left internal mammary artery and takes care during insertion[1]. A small amount of blood can be collected from the PICC for analysis. PLSVC should be considered when catheter suction and saline injection are normal after the possibility of accidental entry into the artery is excluded, and the catheter location should be confirmed by B-ultrasound or chest X-ray. In patient 2, chest X-ray showed the PICC descending along the left side of the vertebral column, because the catheter was inserted through the left axillary vein, and the axillary artery was superficial. Based on previous experience, the PICC team first evaluated the extent of the possibility of entering the artery by mistake. A small amount of blood was collected for bedside blood analysis, and the results showed the following: PaO2 38.9 mmHg, PaCO2 56.3 mmHg, and SaO2 75%; the baby was quiet, with rosy skin; and SPO2 93%, which suggested venous blood. The location of the PICC in patients with PLSVC was further confirmed using B-ultrasound.
In the other seven patients, chest X-ray showed the PICC descending along the left side of the vertebral column; therefore, after comprehensive analysis of the selection of blood vessels before catheterization, the color of the blood during catheterization, the situation of inserted catheter, and the result of normal saline injection, the possibility of PLSVC was first considered. Finally, PLSVC was confirmed by bedside B-ultrasound.
In our study, seven patients had type I PLSVC, and the right superior vena cava existed at the same time. B-ultrasound showed little difference on both sides of the lumen; therefore, removal of the catheter was not considered. A right-to-left shunt was found on B-ultrasound in one patient (patient 8) with type II PLSVC, and the lumen of the left superior vena cava was obviously smaller than that of the right superior vena cava; thus, the PICC was removed on the same day. In this case, the parents decided to abandon treatment and requested that the PICC not be reinserted.
During the indwelling of a PICC, excessive crying, strenuous activity, or irritation should be avoided to reduce the risk of catheter displacement caused by newborns' physical activities[12]. In seven patients, during indwelling of the PICC, the crying babies were soothed by using pacifiers, touching, and holding. For neonates in whom catheterization proceeded through the left basilic vein and left axillary vein, the left upper limb was restrained and placed on the side of the body to avoid catheter shift caused by excessive movement of the limb. Each baby's heart rate, heart rhythm, and SpO2 were closely monitored by continuous electrocardiogram monitoring and timely detection of arrhythmia, cardiac tamponade, and other complications. The arm circumference was measured daily to observe whether the limb was swollen. Proper flushing and a sealing tube were adopted to avoid drawing back blood, and the minimum infusion pump speed was more than 3 mL/h. Transfusion of blood products from the PICC was avoided to prevent the occurrence of PICC-related thrombosis. In this study, no PICC-related complications, such as arrhythmia, cardiac tamponade, or serious complications, were found in seven patients.
In clinical practice, some neonates require removal and reinsertion of the current PICC catheter due to an ectopic placement, pleural effusion, catheter-related bloodstream infection, or repeated changes in the condition, among other reasons. After the first catheterization, the case data should be recorded in a special case database, which can provide a reference for the second or additional catheterizations. In this study, the records of all patients who underwent PICC placement were stored in a computer, and a separate form was used for the newborn who was diagnosed with PLSVC. The records of the eight patients in this study included the following information: (1) General information: Name, sex, registration number, date of birth, gestational age, birth weight, etc.; (2) Imaging data: Cardiac ultrasound, chest X-ray, type of PLSVC, etc.; and (3) Data related to the first catheterization: Age at PICC placement, weight at the time of catheterization, puncture site, length of catheterization, exposed catheter length, catheter tip position, whether the catheter was adjusted after catheterization, days of PICC indwelling, PICC-related complications, etc. PLSVC was indicated on the discharge certificate, and the parents were informed during discharge to provide a reference for follow-up treatment.
Details of the TIMB method compared with the traditional approach and the challenges of the new approach are shown in Table 3.
| Traditional approach | TIMB methods | |
| Timing of PICC placement | On the day of birth | At least 24 h after birth, except for under special circumstances, such as rescue |
| Review of imaging data before catheterization | N/A | Retrospective analysis of imaging data should be performed before catheterization |
| Selection of the puncture site | The first choice is the basilic vein of the upper limbs, both left and right | The first choice is a lower limb vein; left upper limb and left scalp veins should be avoided in patients with PLSVC |
| Body surface measurement method | From the prepuncture point along the vein to the right sternoclavicular joint and down to the 1/2 intercostal space | In patients who were diagnosed with PLSVC by B-ultrasound before PICC placement, when a left-side puncture was required due to vascular conditions, the body surface length was measured from the left puncture point along the vein to the left sternoclavicular joint plus 0.5 cm. If we chose to insert the PICC from a lower limb or right limb, the body surface length was measured in the same manner as in the traditional approach |
| Whether under B-ultrasound guidance | No | Yes |
| Summary and challenges | Using this traditional approach will reduce the first-attempt success rate of PICC placement and limit the ability to discover cardiovascular abnormalities in a timely manner. The use of one measurement method could lead to the PICC tip position being too deep or too shallow. In addition, not using B-ultrasound guidance could also cause the PICC tip position to be too deep or too shallow | Using this new approach can improve the first-attempt success rate of PICC placement, reveal cardiovascular abnormalities in advance, allow the selection of different measurement methods reasonably according to the puncture site, and finally, improve the accuracy of catheter positioning through the use of B-ultrasound guidance. The new method, summarized after application in 8 neonates, still has certain limitations, and a large sample is needed for further research |
PICC placement has a long history, but neonates with PLSVC are rare clinically. How to identify complications early and take effective measures to prevent the occurrence of serious complications deserves the attention of all medical staff. Therefore, we introduce the concept of the “TIMB” bundle, which has seldom been mentioned in previous studies. In our research, the “TIMB” bundle, defined as follows, was useful for PICC placement in neonates with PLSVC: T (Time): Initially, PICC placement should be delayed until at least 24 h after birth in elective clinical settings; I (Imaging data): The imaging data of the infants should be retrospectively analyzed before catheterization; M (Measurement): Left upper extremity and left head and neck vein catheterization should be avoided in patients with PLSVC, and the body surface length should be measured correctly when left-side puncture is selected; and B (B-ultrasound): The tip of the PICC is placed in the middle and lower 1/3 of the left superior vena cava under the guidance of B-ultrasound to ensure the safe use of a PICC in neonates with PLSVC.
After catheterization, the influence of different PLSVC types on PICC use should be correctly judged in all patients. The vital signs and clinical manifestations of the patients should be carefully observed during catheter use, and PICC-related complications should be identified in a timely manner and adequately addressed. Finally, a special case file should be established to ensure safe PICC use in neonates with PLSVC.
Although this case report has some limitations, such as selection bias, it provides useful advice on how to perform PICC placement in neonates with PLSVC.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cimen SG, Islam SMRU S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Li X
| 1. | Fares WH, Birchard KR, Yankaskas JR. Persistent Left Superior Vena Cava Identified During Central Line Placement: A Case Report. Respir Med CME. 2011;4:141-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Jie LL. Pathological anatomy and ultrasound diagnosis of fetal heart. People's Medical Publishing House, 2010. |
| 3. | Esmer AÇ, Yüksel A, Calı H, Ozsürmeli M, Omeroğlu RE, Kalelioğlu I, Has R. Prenatal diagnosis of persistent left superior vena cava and its clinical significance. Balkan Med J. 2014;31:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Evidence-Based Medicine Group; Neonatologist Society; Chinese Medical Doctor Association. . [Operation and management guidelines for peripherally inserted central catheter in neonates (2021)]. Zhongguo Dang Dai Er Ke Za Zhi. 2021;23:201-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 5. | Shao XM, Ye HM, Qiu XS. Practice of Neonatology, 5th ed. People's Medical Publishing House, 2019. |
| 6. | Gorski LA. The 2016 Infusion Therapy Standards of Practice. Home Healthc Now. 2017;35:10-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 181] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 7. | Wang M, Wang YL, Han YF. Nursing Care of 4 Cases of Persistent Left Superior Vena Cava Patients with PICC Ectopic Position. Zhonghua Huli Zazhi. 2011;46:1018-1019. [DOI] [Full Text] |
| 8. | Joshi D, Ridley N, Imam A. The value of a chest radiograph for diagnosing a misplaced PICC line in the persistent left-sided superior vena cava. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Li XY, Yuan Y, Zhang P. Clinical study of isolated persistent left superior vena cava malformation. Shoudu Yi Ke Daxue Xuebao. 2013;34:308-314. [DOI] [Full Text] |
| 10. | National Health Commission of the People’s Republic of China. Nursing technical operation specification for intravenous therapy, 2013. [cited 1 May 2014]. Available from: www.nhc.gov.cn/wjw/pjl/201412/806fe9a7171e4cf584c0d40ed093dfa7.shtml. |
| 11. | Shyamkumar NK, Brown R. Double superior vena cava with a persistent left superior vena cava: an incidental finding during peripherally inserted central catheter placement. Australas Radiol. 2007;51 Suppl:B257-B259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Luo FX, Chen SH, Cheng XY, Fan XY, Wang Q, Yin YJ. A correlation analysis of PICC tip position and weight gaining in very low birth weight infants. Zhonghua Huli Zazhi. 2017;52:949-953. [DOI] [Full Text] |