Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7786
Peer-review started: December 16, 2020
First decision: May 5, 2021
Revised: May 31, 2021
Accepted: August 3, 2021
Article in press: August 3, 2021
Published online: September 16, 2021
Processing time: 262 Days and 22.4 Hours
Increasing attention is being given to burn rehabilitation, and an increasing number of burn patients are undergoing rehabilitation. However, little attention has been given to secondary injuries caused by ill-suited rehabilitation practices. Patients, especially those in undeveloped countries, sustain injuries due to inadequate burn rehabilitation practices and the nonstandard implementation of rehabilitation treatments.
This study reports 5 cases of secondary injuries caused by ill-suited burn rehabilitation practices in our institute, including first web space contracture caused by a single orthosis treatment, finger deformity caused by improper compression therapy with a self-adhering bandage, developmental impairment of the affected limb caused by continuous improper compression therapy, and fracture caused by overly intensive rehabilitation exercise.
More attention should be given to burn rehabilitation to reduce the incidence of secondary injuries caused by ill-suited rehabilitation practices. Burn rehabilitation system should include specialized hospitals (burn rehabilitation centers), com
Core Tip: Functional reconstruction and rehabilitation are dynamically developing processes. Burn rehabilitation treatment should encompass the whole process from the time of the injury to when the patient returns to society, and appropriate rehabilitation measures should be taken at different stages of burn treatment. Rehabilitation therapists should systematically study clinical knowledge related to burns and explore the timing and use of various rehabilitation treatment techniques with clinical treatment to im
- Citation: Zhou L, Zhou YQ, Yang L, Ma SY. Secondary injuries caused by ill-suited rehabilitation treatments: Five case reports. World J Clin Cases 2021; 9(26): 7786-7797
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7786.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7786
With improvements in healthcare, the chances of survival and rehabilitation after burn injury have increased substantially. In the comprehensive treatment of patients, burn rehabilitation, which is gradually being offered to an increasing number of patients, with almost all patients now receiving rehabilitation, is initiated after the completion of burn treatment as well as during the late, middle, and even early stages of burn treatment[1-3]. The current global consensus is that functional exercise and rehabilitation should start early in the burn treatment course, especially in patients with severe burns[4-7]. Preventing postburn deformities is more beneficial than correcting deformities after they occur[8]. Burn rehabilitation is an emerging discipline that has gradually developed in recent years, especially in China, which has the largest population of burn patients, but treatment concepts and operational specifications for burn rehabilitation are not aligned with actual clinical processes, resulting in secon
All 5 patients were male, with ages ranging from 2 years to 31 years; all of the patients were burned by flame. The patients had hypertrophic burn scars and functional impairments.
They underwent different burn rehabilitation techniques and sustained secondary injuries due to these techniques (Tables 1 and 2).
| Sex | Age (yr) | Cause of injury | Total body surface area (%) | Main body parts | Skin grafting | Rehabilitation issues | |
| Case 1 | Male | 31 | Flame | 72 | Hands | Split-thickness skin grafting | Hypertrophic burn scar, flexion deformity, narrowing of the first web space |
| Case 2 | Male | 2 | Flame | 2 | Left hand | Split-thickness skin grafting | Hypertrophic burn scar, left syndactyly |
| Case 3 | Male | 6 | Flame | Unknown | Face | No skin grafting | Hypertrophic burn scar of the jaw |
| Case 4 | Male | 3 | Flame | Unknown | Right lower limb | Mesh grafting | Hypertrophic burn scar |
| Case 5 | Male | 11 | Flame | 71 | Lower limbs | Skin grafting | Flexion contracture of bilateral popliteal fossa caused by scar contracture |
| Main rehabilitation measures | Main problems | New injuries | Remedies | Outcomes | |
| Case 1 (Figure 1) | Compression therapy; Functional orthosis | Orthotic device was not adjusted properly | Significantly reduced first web space angle, thumb abduction and flexion contracture of metacarpophalangeal joint | Added an extension position orthosis that was alternated with a functional orthosis | Appearance and function of the hands were improved significantly |
| Case 2 (Figure 2) | Compression therapy, home rehabilitation, regular follow-up | Wrong wrapping method, excessive compression, not followed regularly | Syndactyly, hyperplasia, and hypertrophy of the distal soft tissue of the fingers on the left hand | Educated the parents about rehabilitation training, demonstrated correct wrapping methods, surgically corrected syndactyly, followed up regularly | The finger webs were evenly spaced, and the soft tissue hypertrophy of the little finger was alleviated |
| Case 3 (Figure 3) | Compression therapy with elastic headgear | Elastic headgear was worn too long, size was not adjusted in time; not followed regularly | Restricted development of alveolar bone; restricted mouth opening and occlusal dysfunction | Provided modified elastic headgear in time and optimized the wearing scheme; followed up every month | Restricted mouth opening was relieved; occlusal function returned to normal, and the facial appearance was significantly improved |
| Case 4 (Figure 4) | Compression therapy | Elastic bandage was applied with too much pressure for a long time | Limb muscle atrophy | Adjusted the compression intensity of the elastic bandage, strengthened functional exercise of the affected limb, performed massage and kerotherapy to promote blood circulation | Deformity of the lower leg was improved slightly |
| Case 5 (Figure 5) | Functional exercise, antiscar treatment | Violent correction of lower limb flexion deformity | Femoral fracture | Immobilized the affected limb with a plaster cast | The fracture gradually healed |
No special circumstances.
All 5 patients have no special personal and family history.
Hypertrophic burn scars and functional impairments.
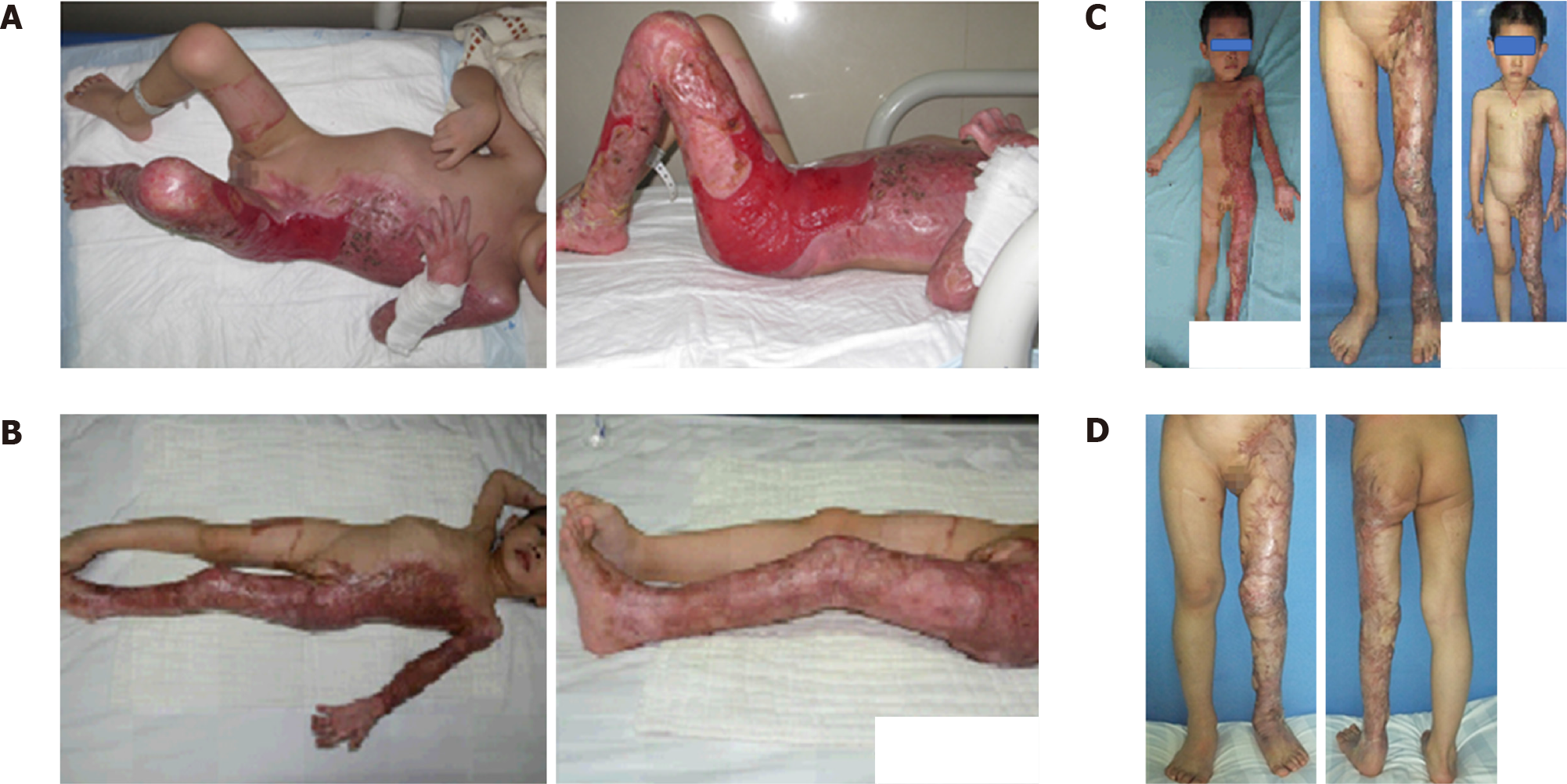
Seventy-two percent total body surface area burned (Figure 1).
Hypertrophic burn scar and syndactyly on the left hand (Figure 2A).
Hypertrophic scars of the jaw after a burn (Figure 3A).
Hypertrophic scar on the right lower limb (Figure 4).
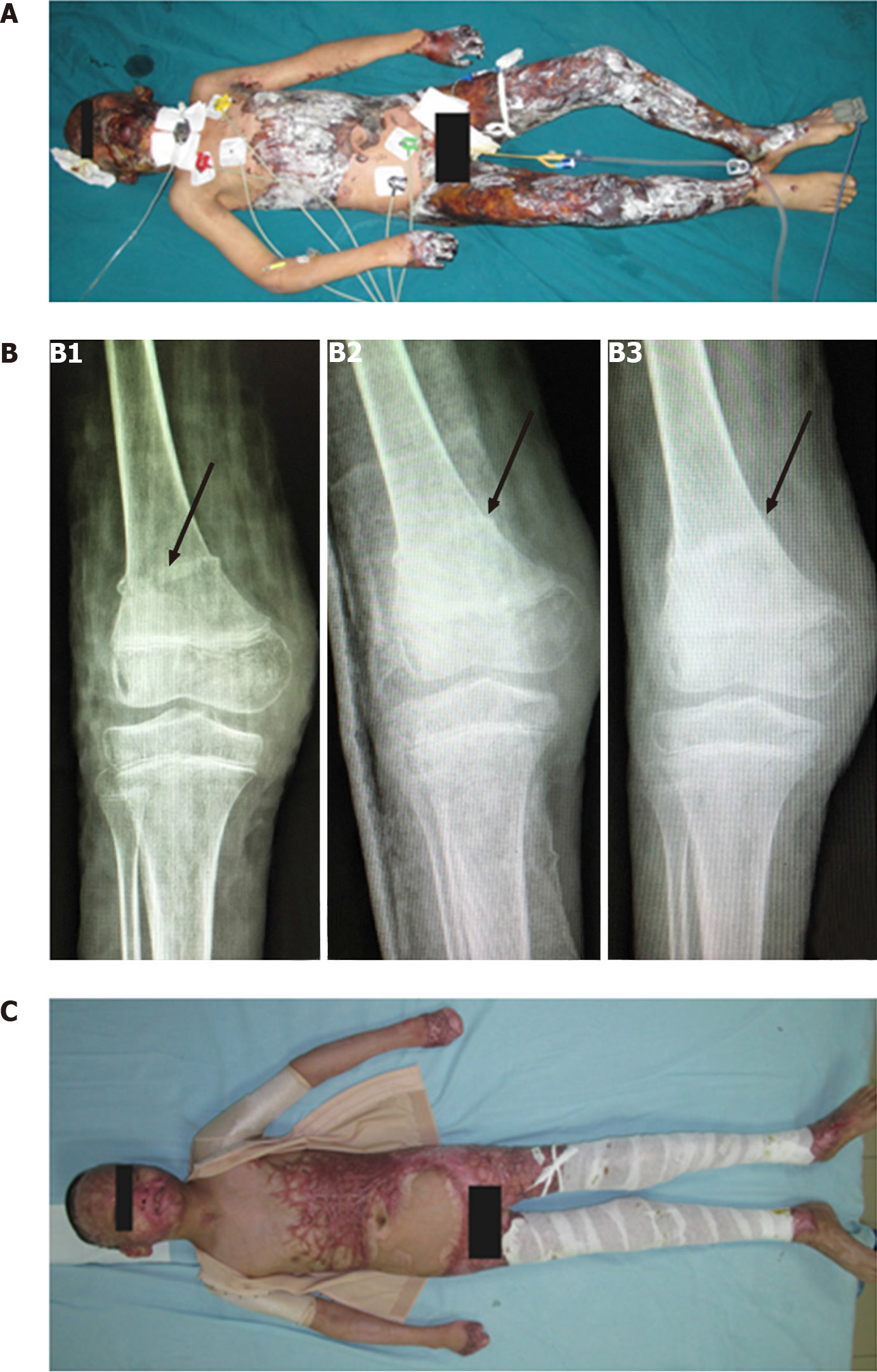
Large-area burn and flexion contracture of the bilateral popliteal fossa caused by scar contracture (Figure 5A).
Split-thickness skin grafting.
Compression therapy with a self-adhering bandage, range-of-motion exercises for the hand joints, home rehabilitation, and regular follow-up (which was not adhered to by the patient’s parents) comprised the rehabilitation regimen.
Compression therapy with elastic headgear performed at home.
An elastic bandage applied with pressure.
Skin grafting, functional exercise, occupational therapy, physical therapy, and antiscar treatment.
Outcome: Although the wound healed, hypertrophic burn scars, flexion deformities, and narrowing of the first web space developed. He received the following rehabilitation regimen: Compression therapy with a self-adhering bandage and bedside range-of-motion exercises and a functional orthosis at night and while at rest (the wrist was placed in the palmar flexion position, the finger webs were spaced with sterile gauze, the metacarpophalangeal joint was maintained in a natural position of 40°-50° of flexion, the interphalangeal joints were fully extended, and the thumb was fixed in opposition to the fingers with abduction (Figure 1A).
Follow-up: Several weeks later, flexion-adduction deformity of both thumbs and flexion contracture of the metacarpophalangeal joint gradually appeared, and the first web space angle and thumb abduction were significantly reduced (Figure 1B). The orthosis was immediately adjusted. An additional orthosis was used to fix the fingers in the extension position, and the thumb was abducted (Figure 1C). The functional orthosis and the extension position orthosis were worn alternately on the subsequent days. Approximately four months later, the appearance and function of the hands improved significantly (Figure 1D).
Outcome: Because of ischemia and hypoxia caused by improper wrapping (using a self-adhering bandage starting from the middle of the fingertip) and too much pressure, excessive cell proliferation, hypertrophy and syndactyly occurred in the distal soft tissue of the fingers of the left hand. Abnormal tissue exceeded the boundary of the nail bed, especially in the little finger. The patient did not regularly attend follow-ups. X-ray examination showed significant hyperplasia of the soft tissue beyond the distal phalanx of the left little and ring fingers, with these fingers being significantly longer than the corresponding fingers of the right hand (Figure 2B).
Follow-up: Syndactyly was surgically corrected, and pads were placed between the fingers to provide compression. The parents received training on the appropriate wrapping method (i.e., wrapping the self-adhering bandage starting from the distal end of the fingernail with proper compression to ensure that the skin of the fingertip was pink after bandaging) and were advised to attend the follow-ups regularly. Several months later, the finger webs were evenly spaced, and soft tissue hypertrophy of the little finger was alleviated (Figure 2C and D).
Outcome: Due to the lack of regular follow-up, the elastic headgear was worn for too long, and the size was not adjusted in a timely manner. The development of alveolar bone was restricted and led to mandibular adduction deformity and occlusal dys
Follow-up: To address these issues, elastic headgear of an appropriate size was immediately provided to increase local compression of the lower jaw and provide circumferential compression of the head. An optimized wearing scheme was provided and relevant precautions were taken to balance pressure treatment and occlusal function training. Regular follow-up every month was planned. Seven years later, the restricted mouth opening was relieved. Moreover, the occlusion was alleviated, and the facial appearance had significantly improved (Figure 3C and D). During rehabilitation, the child underwent a tissue expander flap repair operation because of scalp scar hyperplasia and hair loss.
Outcome: The limb muscle was atrophied because the elastic bandage was applied too tightly for prolonged period of time (Figure 4A and B).
Follow-up: After adjusting the compression intensity of the elastic bandage and strengthening functional exercise of the affected limb, as well as providing massage and kerotherapy to promote blood circulation for 5 years, the deformity of the lower leg was slightly improved (Table 3, Figure 4C and D).
| Body part | Left circumference (the injured side, cm) | Right circumference (cm) |
| Ankle joint | 20 | 19 |
| Thickest part of the calf | 20 | 25 |
| 10 cm below the knee | 21.2 | 21 |
| Thickest part of the thigh | 30 | 33 |
| Leg length | 65.5 | 67 |
Outcome: During rehabilitation provided by his parents, violent correction of the lower limb flexion deformity led to femoral fracture (Figure 5B1 and B2).
Follow-up: The fracture gradually healed after immobilization in a plaster cast for one month (Figure 5B3), and the scar was reduced (Figure 5C).
In the 5 cases reported herein, ill-suited rehabilitation treatment led to secondary injuries, including serious deformities and irreversible developmental disorders. In patient 1, the therapists focused on fixation in the functional position and neglected to apply an orthosis in the extension position; this was due to a lack of therapist ex
It should be emphasized that the burn treatment process is extremely complicated and long. Burn rehabilitation should encompass the whole process from the time of the injury to return to society, and appropriate rehabilitation measures should be implemented at different stages during burn treatment. Rehabilitation therapists should systematically study clinical information related to burns and explore the timing and use of various rehabilitation techniques together with clinical treatments to improve rehabilitation outcomes. Precise instruments and equipment, accurate measurement methods, and objective monitoring indicators are effective in improving the quality of burn rehabilitation. For example, accurate pressure measurement can reduce complications associated with pressure treatments, objective angle measure
Burn rehabilitation involves teamwork. The multidisciplinary team should comprise burn surgeons, rehabilitation physicians, rehabilitation therapists, nurses, family members of the patient and the patient[14]. Personnel specializing in burn rehabilitation, orthopedics, psychology, sports medicine and other relevant disciplines should be recruited through interdisciplinary consultations and multi disciplinary team. The burn department should initiate the establishment of a flexible and interdisciplinary burn rehabilitation team to establish rehabilitation approaches for burn patients and a relatively stable multidisciplinary diagnosis and treatment guidelines. Moreover, the establishment of a national burn rehabilitation society and other academic organizations to further promote the popularization, development, standardization and im
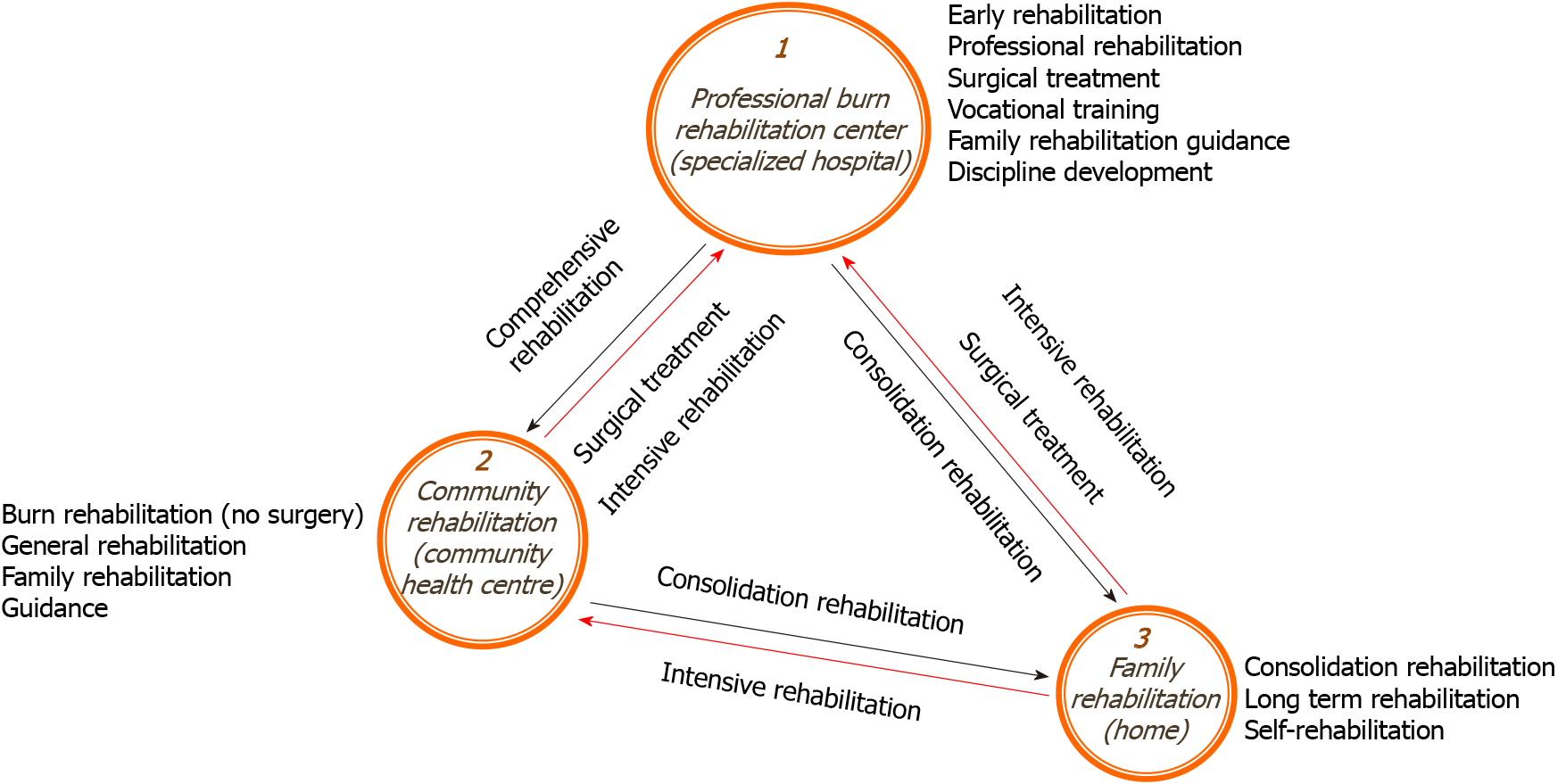
A three-level burn rehabilitation system comprising a specialized hospital (burn rehabilitation center), community hospital, and family rehabilitation clinic will help alleviate and improve the current challenges of burn rehabilitation in China (Figure 6). In this system, well-equipped professional burn rehabilitation centers, as the first and highest level of the system, can also be established as regional burn rehabilitation training bases with the support of the state or social institutions. Their main tasks are the early rehabilitation of burn patients and the administration of important key treatments, excluding surgical treatment. In addition, the development of novel innovations, the formulation and promotion of standards, and training on and the popularization of burn rehabilitation knowledge and skills should be implemented to provide rehabilitation guidance for community health care institutions and families. Community health centers mainly treat patients requiring burn rehabilitation who are transferred from professional burn rehabilitation centers. They provide general or burn-related rehabilitation, including functional exercise, and technical guidance for family members, but they do not perform surgery. As the terminal treatment unit, family rehabilitation clinics are mainly responsible for regular and ongoing general rehabilitation, including functional exercise, which is needed by all burn rehabilitation patients. Studies have shown that family involvement in burn rehabilitation has positive impacts on a patient’s return to society and physical, social, and psychological wellbeing[15]. However, family involvement in rehabilitation requires the participa
Improper burn rehabilitation leads to more serious or even irreversible secondary damage in children with burns than in adults. For example, patient 4 experienced limb dystrophy, and patients 2 and 3 exhibited skeletal and soft tissue developmental malformations. We should pay more attention to burn rehabilitation in children. Under the premise of early rehabilitation, combined with the characteristics of children’s growth and development and specific rehabilitation needs, we should establish meticulous individualized treatment courses, increase the frequency and duration of follow-up, and adjust treatment plans and approaches, such as changing the pressure of clothing or adjusting the parameters of braces, in a timely manner.
In summary, more attention should be given to secondary injuries caused by ill-suited rehabilitation. The three-level burn rehabilitation system, standardized treatment guidelines and recommendation, precision instruments and equipment, accurate measurement methods, objective monitoring indices, good multidisciplinary coope
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Karim HMR, Mance M, Sahu SA S-Editor: Gao CC L-Editor: A P-Editor: Yuan YY
| 1. | Jacobson K, Fletchall S, Dodd H, Starnes C. Current Concepts Burn Rehabilitation, Part I: Care During Hospitalization. Clin Plast Surg. 2017;44:703-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Guo ZR. Current situation and perspective of burn rehabilitation in China. Zhonghua Sunshang Yu Xiufu Zazhi (Dianzi Ban). 2018;13:161-164. [DOI] [Full Text] |
| 3. | Kornhaber R, Rickard G, McLean L, Wiechula R, Lopez V, Cleary M. Burn care and rehabilitation in Australia: health professionals' perspectives. Disabil Rehabil. 2019;41:714-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Gomez M, Tushinski M, Jeschke MG. Impact of Early Inpatient Rehabilitation on Adult Burn Survivors' Functional Outcomes and Resource Utilization. J Burn Care Res. 2017;38:e311-e317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Dodd H, Fletchall S, Starnes C, Jacobson K. Current Concepts Burn Rehabilitation, Part II: Long-Term Recovery. Clin Plast Surg. 2017;44:713-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Jagnoor J, Lukaszyk C, Christou A, Potokar T, Chamania S, Ivers R. Where to from here? BMC Res Notes. 2018;11:224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Chinese Burn Association; Chinese Association of Burn Surgeons, Cen Y, Chai J, Chen H, Chen J, Guo G, Han C, Hu D, Huan J, Huang X, Jia C, Li-Tsang CW, Li J, Li Z, Liu Q, Liu Y, Luo G, Lv G, Niu X, Peng D, Peng Y, Qi H, Qi S, Sheng Z, Tang D, Wang Y, Wu J, Xia Z, Xie W, Yang H, Yi X, Yu L, Zhang G; Chinese Burn Care and Rehabilitation Association. Guidelines for burn rehabilitation in China. Burns Trauma. 2015;3:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Young AW, Dewey WS, King BT. Rehabilitation of Burn Injuries: An Update. Phys Med Rehabil Clin N Am. 2019;30:111-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Wu J, Wang YZ. [A brief history of burn rehabilitation medicine in China]. Zhonghua Shao Shang Za Zhi. 2019;35:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Ao M, Wu J, Chen J. [Investigation of burn rehabilitation development of China in 2014]. Zhonghua Shao Shang Za Zhi. 2017;33:260-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Guo ZR, Li F, Tu HX, Gao GZ, Cui XL, Zhang B, Lu CH, Zhang P. [Initiation, development, and achievements of burn rehabilitation therapy in China]. Zhonghua Shao Shang Za Zhi. 2018;34:835-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Chen J, Li-Tsang CW, Yan H, Liang G, Tan J, Yang S, Wu J. A survey on the current status of burn rehabilitation services in China. Burns. 2013;39:269-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Wu J, Chen J. [Current situation and reflection on rehabilitation after burn injury in China]. Zhonghua Shao Shang Za Zhi. 2013;29:505-508. [PubMed] |
| 14. | Goverman J, Mathews K, Holavanahalli RK, Vardanian A, Herndon DN, Meyer WJ, Kowalske K, Fauerbach J, Gibran NS, Carrougher GJ, Amtmann D, Schneider JC, Ryan CM. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Twenty Years of Contributions to Clinical Service and Research. J Burn Care Res. 2017;38:e240-e253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 15. | Yurdalan SU, Ünlü B, Seyyah M, Şenyıldız B, Çetin YK, Çimen M. Effects of structured home-based exercise program on depression status and quality of life in burn patients. Burns. 2018;44:1287-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |