Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7772
Peer-review started: February 28, 2021
First decision: April 24, 2021
Revised: May 11, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: September 16, 2021
Processing time: 194 Days and 5.2 Hours
Several techniques of nasogastric tube (NGT) insertion have been described in the literature with different success rates.
To systematically search the literature and conduct a meta-analysis comparing the success rates, insertion time and complications associated with different techni
An electronic search of the PubMed, Scopus, CENTRAL (Cochrane Central Register of Controlled Trials), and Google Scholar databases were performed up to October 31, 2019. We included 17 randomized controlled trials with 2500 participants in the meta-analysis.
As compared to the conventional method, successful insertion of the NGT on first attempt was higher with modified techniques such as the reverse Sellick’s ma
The use of modified techniques of NGT insertion such as the reverse Sellick’s maneuver, neck flexion with lateral neck pressure, frozen NGT, endotracheal tube-guided or video-assisted methods result in a significantly better chance of successful tube insertion at first attempt as compared to the conventional tech
Core Tip: Our study indicates that the use of modified techniques of nasogastric tube (NGT) insertion such as the reverse Sellick’s maneuver, neck flexion with lateral neck pressure, frozen NGT, endotracheal tube-guided or video-assisted methods result in a significantly better chance of successful tube insertion at first attempt as compared to the conventional technique.
- Citation: Ou GW, Li H, Shao B, Huang LM, Chen GM, Li WC. Comparison of different methods of nasogastric tube insertion in anesthetized and intubated patients: A meta-analysis. World J Clin Cases 2021; 9(26): 7772-7785
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7772.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7772
Nasogastric tube (NGT) placement is one of the most commonly performed proce
In most clinical settings, the primary responsibility of placing NGTs is that of trained nurses and resident physicians[8-10]. With the significantly increasing role of nurses, they must be aware and well-trained in various techniques of NGT insertion whilst minimizing complications. There are merits and demerits to the different techniques used for placing NGTs in anesthetized and intubated patients, and di
A comprehensive electronic search of the PubMed, Scopus, CENTRAL (Cochrane Central Register of Controlled Trials), and Google Scholar databases was conducted for English as well as non-English language papers published up to October 31, 2019. For non-English language papers, we used Google translator to extract relevant information. Both free text words and medical subject heading terms were used for the systematic search. Details of the search strategy are provided in the supplementary document (Supplementary Table 1). Our key aim was to identify randomized control
Two authors reviewed citations and selected studies. After removing duplicates, the studies were screened by their titles and abstracts. Thereafter, potentially eligible trials were reviewed by their full text. We resolved any discrepancies related to the inclusion of studies through detailed discussion among the study authors. A hand-search of bibliographic lists of the identified studies and relevant reviews was conducted to identify any additional studies.
We included only RCTs on anesthetized and intubated patients that compared at least two different techniques of NGT insertion. Studies were to report any of the following outcomes of interest: success rate on first insertion, overall success rate of insertion (more than two attempts at insertion labeled as failure), time required for successful intubation, and complications (such as mucosal bleeding, gag reflex, cough, kinking and coiling of the NGT).
We excluded studies conducted on awake and non-intubated patients. Studies not reporting relevant outcomes, non-randomized studies, retrospective studies, case reports and review articles were also excluded.
Two authors independently collected relevant data from the included studies using a data extraction sheet. The data from eligible studies included: authors, year of publication, study site, study design, sample size, study groups, and outcomes. Two authors independently evaluated the study methodologies using the Cochrane assessment tool[11].
RCTs comparing the same techniques were pooled for the meta-analysis. In instances where RCTs compared different techniques and pooling of studies was not feasible, results were presented in a descriptive format. Statistical analyses were carried out using STATA version 13.0. Weighted mean differences (WMD) were used to pool effect size for continuous variables. For ordinal data, the relative risk (RR) ratio was calculated. All estimates were expressed with 95% confidence intervals (CIs). We assessed heterogeneity of effects and quantified them based on the I2 value. I2 values > 50% represented substantial heterogeneity[12]. We applied the random-effects model to cases with substantial heterogeneity[12]. A P value of < 0.05 was considered statistically significant. Publication bias was assessed using Egger’s test and visual inspection of funnel plots.
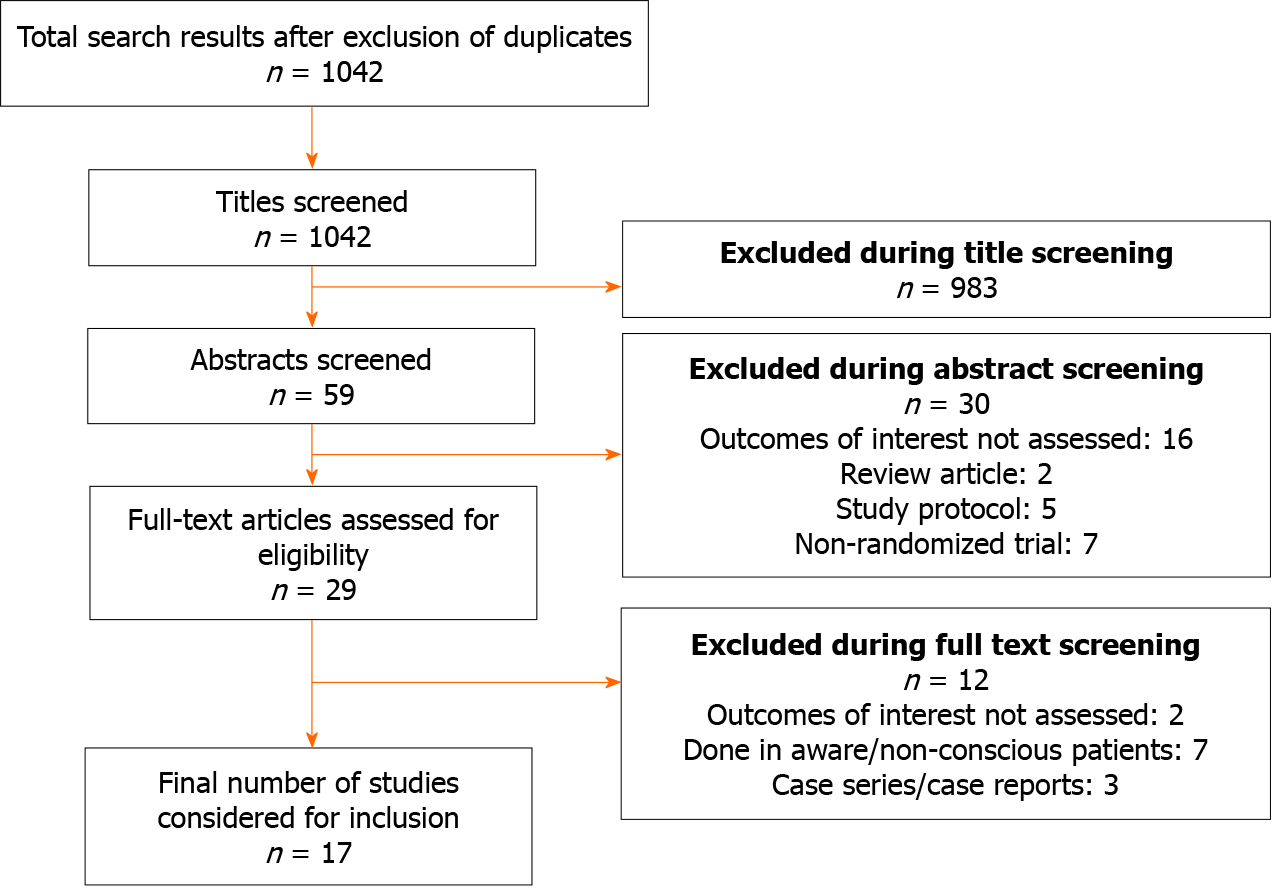
We obtained 1042 unique citations after our search in the PubMed, Scopus, CENTRAL (Cochrane Central Register of Controlled Trials), and Google scholar databases (Figure 1). Of these, 983 papers were excluded after screening the titles, and 30 citations after reading the abstracts. Twenty-nine studies were reviewed by their full texts. Twelve articles did not fulfill the inclusion criteria and were excluded. A total of 17 trials were included in the RCT with a total of 2500 participants[13-29]. The characteristics of the included studies are presented in Table 1. All the included studies were RCTs (6 were conducted in India, 4 in Korea, 2 in Taiwan, 2 in Iran, and 1 in China, Malaysia, and Turkey). The authors’ judgment of risk of bias of the included studies is presented in Supplementary Table 2. All the studies adopted random sequence ge
| Ref. | Country | Sample size | Study participant characteristics | Practitioner inserting NGT with level of expertise | Study groups | Key outcome(s) |
| Zhao et al[13], 2018 | China | 110 | Patients with cerebral hemorrhage or traumatic brain injury | Not specified | Control group (C): Nasogastric tube (NGT) insertion using conventional technique i.e., with head in a neutral position; Intervention group (I): Nasogastric tube insertion in right lateral decubitus position | Success rate on 1st attempt: C = 36/54 (66.7%); I = 50/56 (89.3%). Overall success rate of insertion: C = 47/54 (87.0%); I = 55/56 (98.2%). Intubation time, mean (SD): C = 114.1 (35.6) s; I = 77.9 (33.5) s. Complication rate: (1) Gag reflex: C = 20/54 (37.0%); I = 7/56 (12.5%); (2) Cough: C = 8/54 (14.8%); I = 1/56 (1.8%); (3) Mucosal bleeding: C = 14/54 (25.9%); I = 3/56 (5.4%); and (4) No major adverse events in both groups |
| Mandal et al[14], 2018 | India | 195 | Adult patients undergoing abdominal surgery | Not specified | Group A: Conventional; Group B: Frozen NGT; Group C: Reverse Sellick’s manoeuvre | Success rate on 1st attempt: Group A = 29/65 (44.6%); Group B = 45/65 (69.2%); Group C = 59/63 (93.6%). Overall success rate of insertion: Group A = 45/65 (69.2%); Group B = 55/65 (84.6%); Group C = 60/63 (95.2%). Intubation time, mean (SD): Group A = 42.2 (21.4) s; Group B = 42.1 (13.2) s; Group C = 31.5 (9.5) s. Complication rate: (1) Mucosal bleeding: Group A = 3/65 (4.6%); Group B = 20/65 (30.8%); Group C = 0/63 (0.0%); (2) Coiling: Group A = 12/65 (18.5%); Group B = 16/65 (24.6%); Group C = 5/63 (7.9%); (3) Kinking: Group A = 8/65 (12.3%); Group B = 6/65 (9.2%); Group C = 0/63 (0.0%); and (4) No major adverse events in any of the three groups |
| Chun et al[15], 2009 | Korea | 100 | Patients undergoing elective general anesthesia | Not specified | Patient placed in a neutral position with moderate head elevation; Control (C)-normal silicone NGT; Intervention (I)-frozen NGT | Overall success rate of insertion: C = 29/50 (58.0%); I = 44/50 (88.0%). Intubation time, mean (SD): C = 120 (133) s; I = 83 (43) s. Complication rate: (1) Mucosal bleeding: C = 6/50 (12.0%); I = 3/50 (6.0%); and (2) No major adverse events in any of the groups |
| Siddhartha et al[16], 2017 | India | 120 | Patients undergoing laparoscopic hysterectomy | Not specified | Group C (Control group): Conventional technique with head in a neutral position and NGT through nostril; Group R: Reverse Sellick’s manoeuvre; Group F: Neck flexion with lateral neck pressure | Success rate on 1st attempt: Group C = 15/40 (37.5%); Group F = 16/40 (40.0%); Group R = 31/40 (77.5%). Overall success rate of insertion: Group C = 30/40 (75.0%); Group F = 31/40 (77.5%); Group R = 37/40 (92.5%). Intubation time; mean (SD): Group C = 25.5 (4.5) s; Group F = 20.5 (4.7) s; Group R = 13.1 (2.6) s. Complication rate: (1) Mucosal bleeding: Group C = 12/40 (30.0%); Group F = 12/40 (30.0%); Group R = 10/40 (25.0%); (2) Coiling: Group C = 25/40 (62.5%); Group F = 12/40 (30.0%); Group R = 7/40 (17.5%); and (3) Kinking: Group C = 3/40 (7.5%); Group F = 3/40 (7.5%); Group R = 3/40 (7.5%) |
| Appukutty et al[17], 2009 | India | 200 | Patients receiving GA and tracheal intubation for various surgical procedures | Group of four 3rd year anaesthesia residents; all judged proficient in insertion techniques by the authors | Group C (Control group): Conventional technique with head in a neutral position and NGT through nostril; Group W: Guidewire group; guidewire introduced within a 14-F nasogastric tube; Group S: Slit endotracheal group; Group F- Neck flexion with lateral neck pressure | Success rate on 1st attempt: Group C = 17/50 (34.0%); Group W = 33/50 (66.0%); Group S = 41/50 (82.0%); Group F = 41/50 (82.0%). Overall success rate of insertion: Group C = 36/50 (72.0%); Group W = 46/50 (92.0%); Group S = 46/50 (92.0%); Group F = 47/50 (94.0%). Intubation time, mean (SD): Group C = 56 (36) s; Group W = 42 (29) s; Group S = 98 (43) s; Group F = 31 (19) s. Complication rate: (1) Mucosal bleeding: Group C = 0/50 (0.0%); Group W = 0/50 (0.0%); Group S = 11/50 (22.0%); Group F = 0/50 (0.0%); (2) Coiling: Group C = 1/50 (2.0%); Group W = 1/50 (2.0%); Group S = 0/50 (0.0%); Group F = 0/50 (0.0%); and (3) Kinking: Group C = 10/50 (20.0%); Group W = 4/50 (8.0%); Group S = 0/50 (0.0%); Group F = 4/50 (8.0%) |
| Kwon et al[18], 2014 | Korea | 56 | Intubated patients in the emergency department | By 3 paramedics; 8 h of education and practice on a mannequin for NGT insertion | Control group (C): Conventional technique with head in a neutral position and NGT through nostril; Intervention group (I): Endotracheal tube-assisted insertion through mouth | Success rate on 1st attempt: C = 14/28 (50.0%); I = 28/28 (100.0%). Overall success rate of insertion: C = 18/28 (64.0%); I = 28/28 (100.0%). Intubation time, mean (SD): C = 111.7 (74.5) s; I = 58 (16.9) s. Complication rate: (1) Mucosal bleeding: C = 2/28 (7.0%); I = 5/28 (17.8.0%); and (2) Kinking: C = 5/28 (17.8%); I = 0/28 (0.0%) |
| Illias et al[19], 2013 | Taiwan | 150 | Patients intubated for gastrointestinal surgery | By 2 experienced anesthesiologists | Control group: Conventional technique with head in a neutral position and NGT through nostril; Group F: Neck flexion with lateral neck pressure; Group L: NGT placed after lifting of the larynx | Success rate on 1st attempt: Control = 26/50 (52.0%); Group F = 41/50 (82.0%); Group L = 44/50 (88.0%). Overall success rate of insertion: Control = 30/50 (60.0%); Group F = 44/50 (88.0%); Group L = 46/50 (92.0%). Intubation time, mean (SD): Control = 26.7 (16.0) s; Group F = 29.5 (14.8) s; Group L = 21.3 (8.4) s. Complication rate: (1) Mucosal bleeding: Control = 5/50 (10.0%); Group F = 1/50 (2.0%); Group L=1/50 (2.0%); (2) Kinking: Control = 20/50 (40.0%); Group F = 8/50 (16.0%); Group L = 6/50 (12.0%); (3) Coiling: Control = 19/50 (38.0%); Group F = 2/50 (4.0%); Group L = 0/50 (0.0%); and (4) Bradycardia: Control = 0/50 (0.0%); Group F = 0/50 (0.0%); Group L = 1/50 (2.0%) |
| Kavakli et al[20], 2017 | Turkey | 200 | Patients intubated for gastrointestinal surgery | By 3 anaesthesiologists of similar experience | Control group: Conventional technique with head in a neutral position and NGT through nostril; Group L: head in lateral position; Group ET: Endotracheal tube-assisted NGT placement; Group MG: McGrath video laryngoscope-assisted NGT placement | Success rate on 1st attempt: Control = 27/50 (54.0%); Group L = 39/50 (78.0%); Group ET = 50/50 (100.0%); Group MG = 46/50 (92.0%). Overall success rate of insertion: Control = 33/50 (66.0%); Group L = 44/50 (88.0%); Group ET = 50/50 (100.0%); Group MG = 49/50 (98.0%). Intubation time, mean (SD): Control = 62.5 (15.3) s; Group L = 43.4 (7.8) s; Group ET = 82.3 (7.9) s; Group MG = 42.4 (4.2) s. Complication rate: (1) Mucosal bleeding: Control = 10/50 (20.0%); Group L = 9/50 (18.0%); Group ET = 10/50 (20.0%); Group MG = 1/50 (2.0%); and (2) Coiling: Control = 10/50 (20.0%); Group L = 3/50 (6.0%); Group ET = 0/50 (0.0%); Group MG = 1/50 (2.0%) |
| Wan Ibadullah et al[21], 2016 | Malaysia | 96 | Patients scheduled for surgery under GA requiring tracheal intubation and NGT insertion | Multiple anesthetists proficient in both techniques of insertion | Group A: NGT insertion using GlideScope visualization; Group B: NGT insertion using direct MacIntosh laryngoscope | Success rate on 1st attempt: Group A = 35/47 (74.5%); Group B = 28/48 (58.3%). Overall success rate of insertion: Group A = 46/47 (97.8%); Group B = 46/48 (95.8%). Intubation time, mean (SD): Group A = 17.2 (9.3) s; Group B = 18.9 (13.0) s. Complication rate: (1) Mucosal bleeding: Group A = 4/47 (8.5%); Group B = 4/48 (10.4%); (2) Coiling: Group A = 11/47 (23.4%); Group B = 17/48 (35.4%); and (3) Kinking: Group A = 2/47 (4.3%); Group B = 1/48 (2.1%) |
| Tsai et al[22], 2012 | Taiwan | 103 | Patients scheduled for gastrointestinal or hepatic surgery under GA | Single anesthetist; practice of both techniques for 2 wk with 20 patients per technique | Control (C): Conventional technique with head in a neutral position and NGT through nostril; Intervention (I)- NGT insertion with help of “Rusch” intubation stylet tied together at the tips by a slipknot | Success rate on 1st attempt: C = 27/50 (54.0%); I = 50/53 (94.3%). Overall success rate of insertion: C = 32/50 (64.0%); I = 52/53 (98.1%). Intubation time, mean (SD): Control= 39.5 (19.5) s; I = 40.3 (23.2) s. Complication rate: (1) Mucosal bleeding: Control = 6/50 (12.0%); I = 6/53 (11.3%); and (2) Kinking: C = 9/50 (18.0%); I = 0/53 (0.0%) |
| Kirtania et al[23], 2012 | India | 480 | Patients scheduled for gastrointestinal surgery under GA | 2 independent operators trained by authors before the study; the operators demonstrated the techniques on one patient each before the study | Group 1: NGT placement with esophageal guidewire with manual forward displacement of larynx; Group 2: Neck flexion with lateral neck pressure | Success rate on 1st attempt: Group 1 = 230/240 (99.2%); Group 2 = 136/240 (56.7%). Overall success rate of insertion: Group 1 = 240/240 (100.0%); Group 2 = 205/240 (85.4%). Intubation time, mean (SD): Group 1 = 54.9 (7.4) s; Group 2 = 90.1 (43.6) s. Complication rate: (1) Mucosal bleeding: Group 1 = 10/240 (4.2%); Group 2 = 36/240 (15.0%); (2) Coiling: Group 1 = 2/240 (0.8%); Group 2 = 104/240 (43.3%); and (3) Moderate injury: Group 1 = 1/240 (0.42%); Group 2 = 9/240 (3.8%) |
| Shwetha Odeyar et al[24], 2019 | India | 60 | Patients scheduled for laparoscopic or laparotomy under GA | Single anesthesiologist | Group A: Conventional technique with head in a neutral position and NGT through nostril; Group B: Reverse Sellick’s maneuver | Success rate on 1st attempt: Group A = 6/30 (20.0%); Group B = 14/30 (46.7%). Overall success rate of insertion: Group A = 27/30 (90.0%); Group B = 27/30 (90.0%). Intubation time, mean (SD): Group A = 97 (23.1) s; Group B = 84 (17.3) s. Complication rate: Mucosal bleeding: Group A = 2/30 (6.7%); Group B = 1/30 (3.3%) |
| Ghaemi et al[25], 2013 | Islamic Republic of Iran | 80 | Patients undergoing elective GA and required NGT insertion | Single anesthesiologist | Control (C): Conventional technique with head in a neutral position and NGT through nostril; Intervention (I): NGT insertion same as control except the NGT was equipped with a Nelaton catheter. Nelaton equipped NGT was inserted through nostril as deeply as the Nelaton catheter length. Then the catheter was withdrawn and NGT was inserted further to reach the stomach | Overall success rate of insertion: C = 23/40 (57.5%); I = 36/40 (90.0%). Intubation time, mean (SD): Control = 92 (35) s; Intervention = 80 (43) s. Complication rate: Mucosal bleeding: C = 3/40 (7.5%); I = 5/40 (12.5%) |
| Kim et al[26], 2018 | Korea | 70 | Patients undergoing gastrointestinal surgery under GA | Single anesthesiologist | Control: Conventional (C) technique with head in a neutral position and NGT through nostril;Intervention (I): NGT insertion using GlideScope and Modified Magill forceps | Success rate on 1st attempt: C = 13/35 (37.1%); I = 35/35 (100.0%). Overall success rate of insertion: C = 26/35 (74.3%); I = 35/35 (100.0%). Intubation time, mean (SD): C = 96.7 (57.5) s; I = 71.3 (22.6) s |
| Kim et al[27], 2016 | Korea | 100 | Patients undergoing gastrointestinal surgery under GA | Not Specified | Control: Conventional (C) technique with head in a neutral position and NGT through nostril; Intervention (I): NGT insertion same as the control except that a lubricated tube exchanger was used to facilitate insertion | Success rate on 1st insertion: C = 34/50 (68.0%); I = 46/50 (92.0%). Overall success rate of attempt: C = 46/50 (92.0%); I = 50/50 (100.0%). Intubation time; Mean (SD): C = 75.1 (9.8) s; I = 18.5 (8.2) s. Complication rate: (1) Mucosal bleeding: C = 9/50 (18.0%); I = 1/50 (2.0%); and (2) Kinking: C = 10/50 (20.0%); I = 0/50 (0.0%) |
| Singh et al[28], 2016 | India | 300 | Patients requiring admission to intensive care unit and NGT insertion | 3rd year anesthesia residents judged proficient in insertion techniques | Control group: Manual anterior displacement of cricoid cartilage and NGT insertion; Group W: NGT insertion using guidewire; Group B: Combination of Manual anterior displacement of cricoid cartilage and guidewire | Success rate on 1st attempt: Control = 64/100 (64.0%); Group B = 88/100 (88.0%); Group W = 84/100 (84.0%). Overall success rate of insertion: Control = 82/100 (82.0%); Group B = 97/100 (97.0%); Group W = 90/100 (90.0%). Intubation time, mean (SD): Control = 60.2 (20.9) s; Group B = 39.3 (9.6) s; Group W = 42.9 (10.1) s. Complication rate: (1) Mucosal bleeding: Control = 3/100 (3.0%); Group B=7/100 (7.0%); Group W = 7/100 (7.0%); and (2) Kinking: Control = 7/100 (7.0%); Group B = 1/100 (1.0%); Group W = 2/100 (2.0%) |
| Moharari et al[29], 2010 | Iran | 80 | Patients requiring intraoperative placement of NGT | Single anesthesiologist | Control group (C): Conventional technique with head in a neutral position and NGT through nostril; Intervention (I): NGT inserted and placed using GlideScope visualization | Success rate on 1st attempt: Control = 23/40 (57.5%); I = 34/40 (85.0%). Overall success rate of insertion: Control = 27/40 (67.5%); Intervention = 35/40 (87.5%). Intubation time, mean (SD): Control = 38.6 (29) s; Intervention = 10.9 (9.0) s. Complication rate: Mucosal bleeding: Control = 14/40 (35.0%); Intervention = 8/40 (20.0%) |
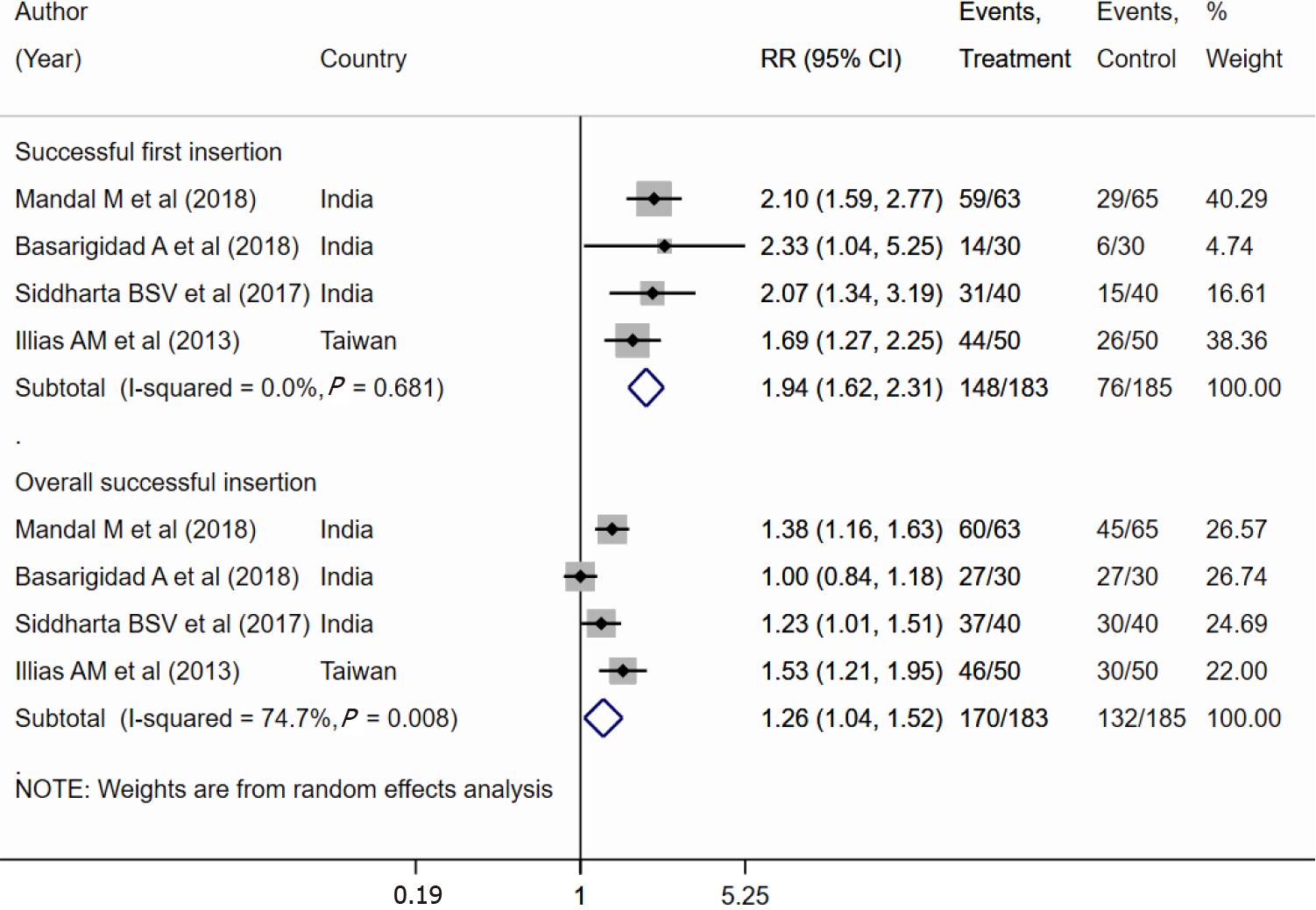
The results of the meta-analysis indicated a nearly 2-fold increased chance of suc
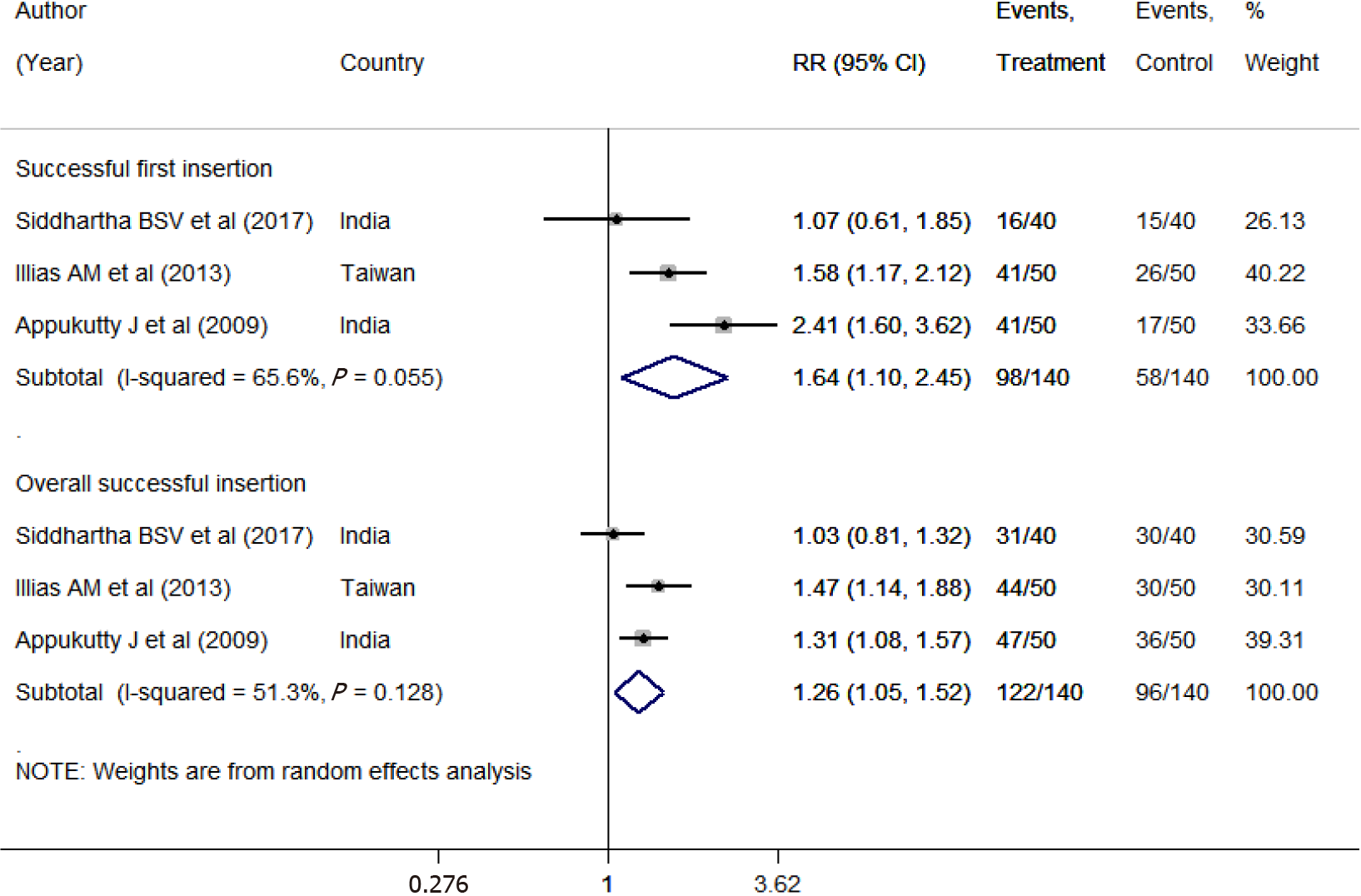
The results of our meta-analysis indicated a 1.64-fold increased chance of successful first insertion using neck flexion with lateral neck pressure (NFLNP) than using the conventional technique (RR 1.64; 95%CI: 1.10-2.45) (Figure 3). Also, with NFLNP, the chance of overall successful insertion was 1.26 times higher than that with the conventional technique (RR 1.26; 95%CI: 1.05-1.52). The pooled mean time involved in placement of the NGT was statistically similar for the two groups [WMD: -7.60; 95%CI: -17.73 to 2.53] (Supplementary Figure 4). NFLNP was associated with a reduced risk of coiling (RR 0.40; 95%CI: 0.24-0.65) and kinking of the NGT (RR 0.45; 95%CI: 0.26-0.79), but no significant effect on the risk of mucosal bleeding was noted (RR 0.86; 95%CI: 0.46-1.63) (Supplementary Figure 5). We found no evidence of publication bias (P = 0.912) (Supplementary Figure 6).
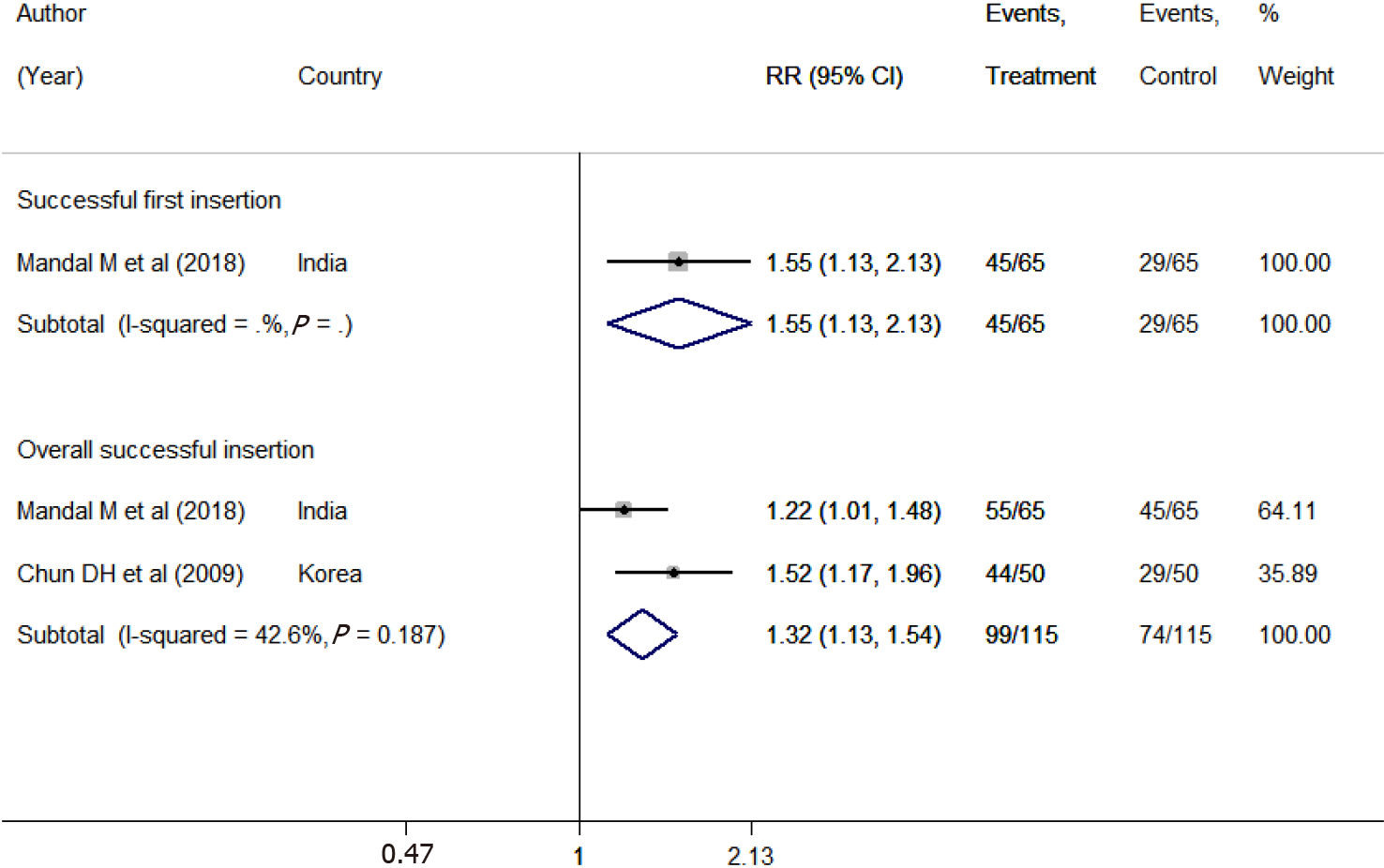
The pooled estimates indicated a 1.55-fold increased chance of successful first insertion using frozen NGTs compared to the use of the conventional technique (RR 1.55; 95%CI: 1.13–2.13) (Figure 4). However, only one study provided this comparison. Moreover, the chance of overall successful insertion was 1.32 times higher with the use of frozen NGTs (RR 1.32; 95%CI: 1.13-1.54). The pooled mean time involved in NGT placement was statistically similar for the two groups [WMD -13.39; 95%CI: -48.10 to 21.33] (Supplementary Figure 7). We found no differences in terms of the risk of complications between the two groups; pooled risk of mucosal bleeding (RR 1.86; 95%CI: 0.14-24.08), or risk of NGT coiling (RR 1.33; 95%CI: 0.69-2.59) and risk of kinking of NGT (RR 0.75; 95%CI: 0.28-2.04) (Supplementary Figure 8). We found no evidence of publication bias (P = 0.317) (Supplementary Figure 9).
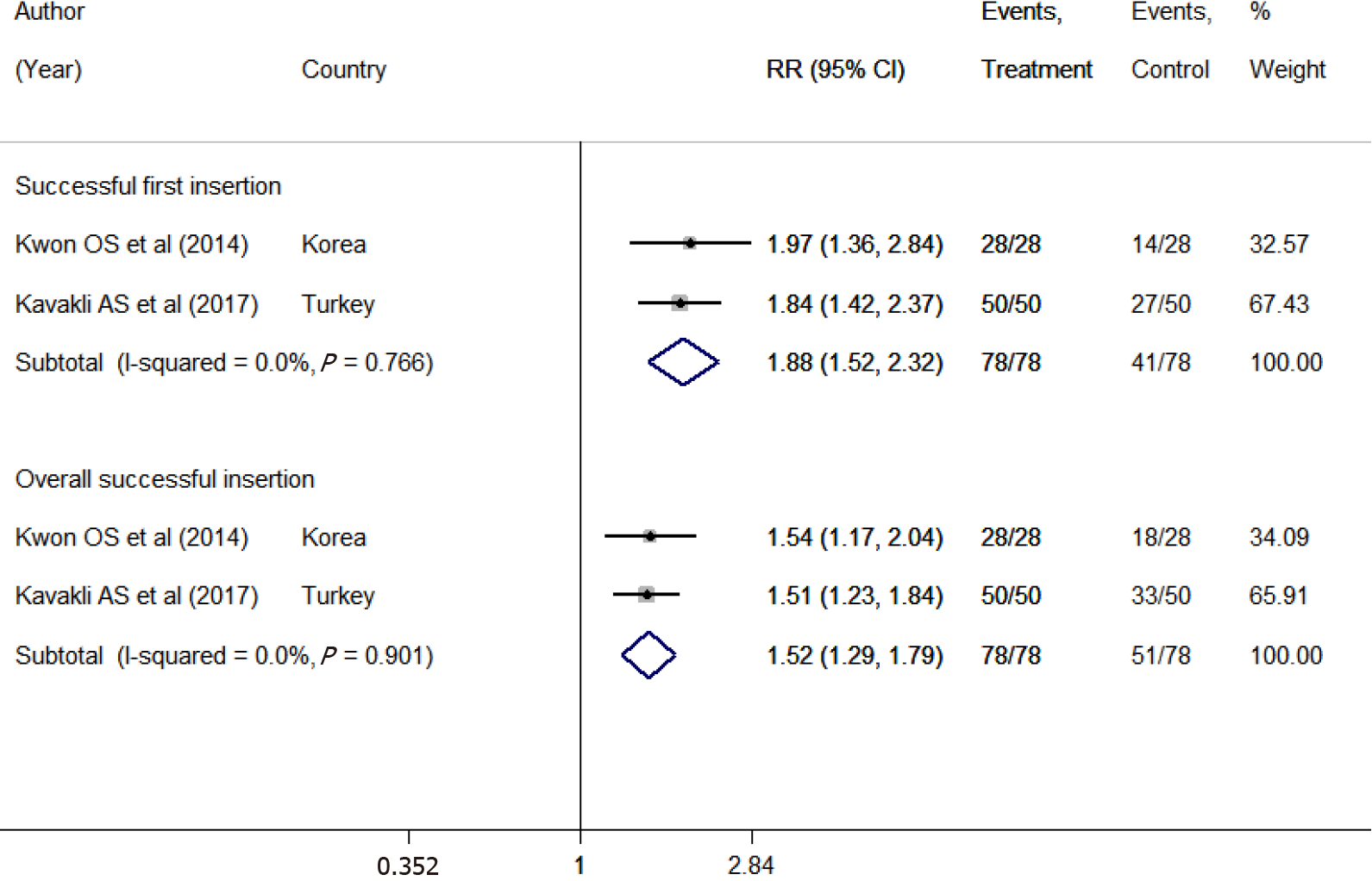
The pooled estimates indicated an approximately 2-fold increased chance of successful first insertion with endotracheal tube-assisted NGT placement than with the conventional technique (RR 1.88; 95%CI: 1.52-2.32) (Figure 5). The chance of overall successful insertion was 1.5 times higher with the endotracheal tube (RR 1.52; 95%CI: 1.29-1.79). The pooled mean time involved in NGT placement was statistically similar for the two groups (WMD: -15.57; 95%CI: -87.55 to 56.41) (Supplementary Figure 10). We found no differences in the risk of mucosal bleeding (RR 1.20; 95%CI: 0.60-2.43) or kinking (RR 0.09; 95%CI: 0.01-1.57) between the two groups. However, the risk of coiling (RR 0.05; 95%CI: 0.00-0.79) of the NGT was close to being significantly different and reflected the decreased risk with the use of an endotracheal tube (Supplementary Figure 11). We found no evidence of publication bias (P = 0.312) (Supplementary Figure 12).
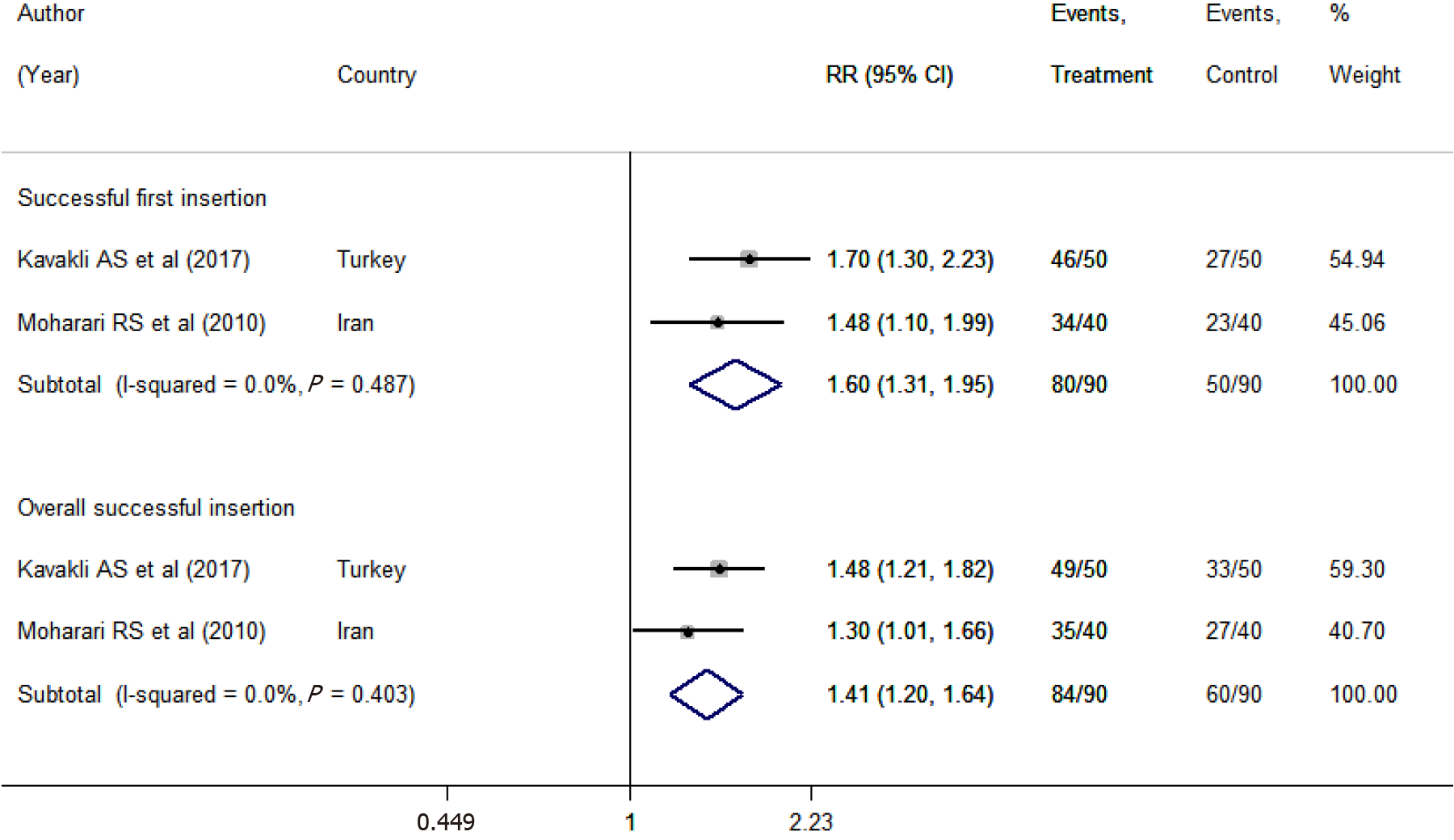
The chances of successful insertion in the first attempt were 1.60 times higher (RR 1.60; 95%CI: 1.31-1.95) with video-assisted placement than with the conventional technique (Figure 6). Similarly, video-assisted placement led to a higher chance of overall successful insertion (RR 1.41; 95%CI: 1.20-1.64). The pooled mean time involved in NGT placement was comparatively less with the video-assisted technique than with the conventional technique (WMD: -22.71; 95%CI: -29.79 to -15.64) (Supplementary Figure 13). We found no differences in the risks of mucosal bleeding (RR 0.30; 95%CI: 0.05-1.74) between the two groups. The risk of coiling (RR 0.10; 95%CI: 0.01-0.75) was decreased with the use of video-assisted NGT placement (Supplementary Figures 14 and 15).
A summary of the meta-analysis for the successful placement of NGT is presented in Table 2. Some studies could not be pooled in the meta-analysis because the insertion techniques tested were not used in other studies. Zhao et al[13] compared the conventional NGT insertion technique with NGT placement in the right lateral decubitus position and found a statistically significant difference in the rates of successful insertion in the first attempt, overall success, insertion time, and complications (gag reflex, cough, and mucosal bleeding) with the right lateral decubitus position. Ghaemi et al[25] compared Nelaton catheter-assisted NGT placement with the conventional technique and showed a higher rate of successful insertion with relatively shorter insertion duration in the Nelaton group. Wan Ibadullah et al[21] documented a higher, although non-significant, success rate of insertion for the GlideScope compared to the Macintosh laryngoscope. Appukutty et al[17] compared a slit endotracheal tube and guidewire with the conventional method and showed similar success rates. Kirtania et al[23] showed that the esophageal guidewire-guided technique with a manual shift of the larynx resulted in correct NGT placement in anesthetized patients and had a low incidence of complications and comparatively shorter insertion times.
| Techniques compared/outcomes | Success on 1st insertion | Overall success of insertion |
| Reverse Sellick’s maneuver vs conventional technique | RR 1.94; 95%CI: 1.62-2.31 | RR 1.26; 95%CI: 1.04-1.52 |
| Neck flexion with lateral neck pressure vs conventional technique | RR 1.64; 95%CI: 1.10-2.45 | RR 1.26; 95%CI: 1.05-1.52 |
| Frozen nasogastric tube vs conventional technique | RR 1.55; 95%CI: 1.13-2.13 | RR 1.32; 95%CI: 1.13-1.54 |
| Endotracheal tube-guided vs conventional technique | RR 1.88; 95%CI: 1.52-2.32 | RR 1.52; 95% CI: 1.29-1.79 |
| Video-assisted vs conventional technique | RR 1.60; 95%CI: 1.31-1.95 | RR 1.41; 95%CI: 1.20-1.64 |
A meta-analysis of available data indicated that modified techniques of NGT insertion (use of reverse Sellick’s maneuver, NFLNP, frozen NGT, endotracheal tube or video-assisted method) results in a significantly improved success on first attempt compared with the conventional technique of NGT placement. Similarly, all modified methods significantly improved the overall success rate of NGT insertion.
Failure of NGT insertion in patients who are unconscious and anesthetized fre
Despite all modified methods achieving better success rates of NGT insertion as compared to the conventional technique, a statistically significant difference in the mean time to tube insertion was found with only two techniques in our study. The mean intubation times were significantly reduced only in the case of the reverse Sellick’s maneuver and with video-assisted placements. It is important to note that, only a few studies were available for meta-analyses for each comparison and results may have been skewed due to the limited data. Also, there was wide variation in the time to insertion of the NGT in the included studies. This may be attributed to the varied sample of the included trials, study settings, methodological differences, operator expertise, etc.
NGT insertion in an anesthetized and intubated patient can also cause trauma leading to patient complications. The incidence of complications increases with multiple attempts of insertion and instrumentation[3]. Therefore, strategies that increase the first attempt success rate and ease of NGT placement could also reduce the complication rate. However, in contrast, the results of our study indicate that none of the modified techniques were able to reduce the risk of mucosal bleeding as compared to the conventional method. This may be attributed to the methodological differences of the included studies such as variation of outcome definition, differences in patient population (use of anticoagulants or presence of bleeding disorders) and the limited data pooled in the meta-analysis. Our results showed that the risk of NGT coiling was significantly reduced with all techniques, except with frozen NGTs. The risk of NGT kinking during placement was reduced only with the NFLNP technique.
We are aware of the limitations of this meta-analysis. Firstly, while the quality of the studies included was good, most of them were conducted on a limited study popu
To conclude, our study indicates that the use of modified techniques of NGT insertion such as the reverse Sellick’s maneuver, NFLNP, frozen NGT, endotracheal tube-guided or video-assisted method result in a significantly better chance of successful tube insertion at first attempt as compared to the conventional technique. All modified techniques also significantly improve the overall chances of successful NGT placement as compared to the conventional method. Insertion times were significantly reduced with the use of the reverse Sellick’s maneuver and with video-assisted placements. None of the modified techniques were able to reduce the incidence of mucosal bleeding as compared to the conventional method. However, strong conclusions cannot be drawn due to the lack of coherent studies and limited data available. Further homogenous large-scale RCTs comparing multiple techniques of NGT insertion are needed to strengthen the evidence on this important subject.
Several techniques of nasogastric tube (NGT) insertion have been described in the literature with different success rates. The best NGT insertion method is still unclear.
No meta-analysis has summarized the evidence with the intent to provide reliable information both in terms of relative advantages of the techniques and their associated complication rates.
To compare the success rates, insertion time, and complications associated with different techniques of NGT insertion in anesthetized and intubated patients.
An electronic search of the PubMed, Scopus, CENTRAL (Cochrane Central Register of Controlled Trials), and Google Scholar databases was performed up to October 31, 2019.
Seventeen randomized controlled trials (RCTs) featuring data on 2500 patients showed that successful insertion of the NGT on the first attempt was higher with modified techniques such as the reverse Sellick’s maneuver, use of a frozen NGT, adopting neck flexion and lateral neck pressure, as well as endotracheal tube-assisted and video-assisted placements. All modified techniques also led to comparatively higher overall insertion success rates.
The use of modified techniques of NGT insertion appears superior to conventional methods. However, limited available data makes drawing a strong conclusion diffi
Further homogenous large-scale RCTs comparing multiple techniques of NGT in
Manuscript source: Unsolicited manuscript
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anandan H S-Editor: Yan JP L-Editor: Webster JR P-Editor: Yuan YY
| 1. | Gottrand F, Sullivan PB. Gastrostomy tube feeding: when to start, what to feed and how to stop. Eur J Clin Nutr. 2010;64 Suppl 1:S17-S21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 2. | Schlein K. Gastric Versus Small Bowel Feeding in Critically Ill Adults. Nutr Clin Pract. 2016;31:514-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 3. | Sanaie S, Mahmoodpoor A, Najafi M. Nasogastric tube insertion in anaesthetized patients: a comprehensive review. Anaesthesiol Intensive Ther. 2017;49:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Lyske J. A rare complication of nasogastric tube insertion. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 5. | Isik A, Firat D, Peker K, Sayar I, Idiz O, Soytürk M. A case report of esophageal perforation: Complication of nasogastric tube placement. Am J Case Rep. 2014;15:168-171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Xu Z, Li W. Aspiration pneumonia caused by inadvertent insertion of gastric tube in an obtunded patient postoperatively. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Hanna AS, Grindle CR, Patel AA, Rosen MR, Evans JJ. Inadvertent insertion of nasogastric tube into the brain stem and spinal cord after endoscopic skull base surgery. Am J Otolaryngol. 2012;33:178-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Cannaby AM, Evans L, Freeman A. Nursing care of patients with nasogastric feeding tubes. Br J Nurs. 2002;11:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 9. | Das S, Patra D, Pradhan P. Critical Care Nurses’ Knowledge and Skill regarding Enteral Nutrition in Critically Ill Patients at a Glance. JONSP. 2014;4. |
| 10. | Ibrahim MH, Qalawa SAA. Assessment of Nurses’ Knowledge and Performance Regarding Feeding Patients with Nasogastric Tube in Ismailia General Hospital. 2016. [cited 10 February 2021]. Available from: https://www.semanticscholar.org/paper/Assessment-of-Nurses%27-Knowledge-and-Performance-in-Ibrahim-Qalawa/baa52b619e4f0ca0947696be22c7def6c7dc7797. |
| 11. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24651] [Article Influence: 1760.8] [Reference Citation Analysis (3)] |
| 12. | Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. [cited 10 February 2021]. Available from www.training.cochrane.org/handbook. |
| 13. | Zhao W, Ge C, Zhang W, Sun Z, Li X. The important role of positioning in nasogastric tube insertion in unconscious patients: A prospective, randomised, double-blind study. J Clin Nurs. 2018;27:e162-e168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Mandal M, Karmakar A, Basu SR. Nasogastric tube insertion in anaesthetised, intubated adult patients: A comparison between three techniques. Indian J Anaesth. 2018;62:609-615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Chun DH, Kim NY, Shin YS, Kim SH. A randomized, clinical trial of frozen versus standard nasogastric tube placement. World J Surg. 2009;33:1789-1792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Siddhartha BSV, Sharma NGA, Kamble S, Shankaranarayana P. Nasogastric Tube Insertion in Anesthetized Intubated Patients Undergoing Laparoscopic Hysterectomies: A Comparative Study of Three Techniques. Anesth Essays Res. 2017;11:550-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Appukutty J, Shroff PP. Nasogastric tube insertion using different techniques in anesthetized patients: a prospective, randomized study. Anesth Analg. 2009;109:832-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Kwon OS, Cho GC, Jo CH, Cho YS. Endotracheal tube-assisted orogastric tube insertion in intubated patients in an ED. Am J Emerg Med. 2015;33:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Illias AM, Hui YL, Lin CC, Chang CJ, Yu HP. A comparison of nasogastric tube insertion techniques without using other instruments in anesthetized and intubated patients. Ann Saudi Med. 2013;33:476-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Kavakli AS, Kavrut Ozturk N, Karaveli A, Onuk AA, Ozyurek L, Inanoglu K. [Comparison of different methods of nasogastric tube insertion in anesthetized and intubated patients]. Rev Bras Anestesiol. 2017;67:578-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 21. | Wan Ibadullah WH, Yahya N, Ghazali SS, Kamaruzaman E, Yong LC, Dan A, Md Zain J. Comparing insertion characteristics on nasogastric tube placement by using GlideScope™ visualization vs. MacIntosh laryngoscope assistance in anaesthetized and intubated patients. Braz J Anesthesiol. 2016;66:363-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Tsai YF, Luo CF, Illias A, Lin CC, Yu HP. Nasogastric tube insertion in anesthetized and intubated patients: a new and reliable method. BMC Gastroenterol. 2012;12:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Kirtania J, Ghose T, Garai D, Ray S. Esophageal guidewire-assisted nasogastric tube insertion in anesthetized and intubated patients: a prospective randomized controlled study. Anesth Analg. 2012;114:343-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Shwetha Odeyar S, Shilpa HL, Ramesh Kumar PB. Preemptive melatonin versus pregabalin for perioperative anxiety and sedation in patients undergoing cataract surgeries: A double blind, prospective randomized clinical trial. MedPulse Int J Anesthesiol. 2019;9:129-132. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Ghaemi M, Mousavinasab N, Jalili S. Nelaton catheter assisted versus standard nasogastric tube insertion: a randomized, clinical trial. EMHJ. 2013;19:1-5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Kim HJ, Park SI, Cho SY, Cho MJ. The GlideScope with modified Magill forceps facilitates nasogastric tube insertion in anesthetized patients: A randomized clinical study. J Int Med Res. 2018;46:3124-3130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Kim HJ, Lee HJ, Cho HJ, Kim HK, Cho AR, Oh N. Nasogastric tube insertion using airway tube exchanger in anesthetized and intubated patients. Korean J Anesthesiol. 2016;69:568-572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Singh LC, More S, Elangovan TA, Bd D, Fatima N. Nasogastric tube insertion revisited: An RCT of three techniques. 2016. [cited 10 February 2021]. Available from: https://www.ijbamr.com/assets/images/issues/pdf/September%202016%20305-309.pdf.pdf. |
| 29. | Moharari RS, Fallah AH, Khajavi MR, Khashayar P, Lakeh MM, Najafi A. The GlideScope facilitates nasogastric tube insertion: a randomized clinical trial. Anesth Analg. 2010;110:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |