Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7729
Peer-review started: May 7, 2021
First decision: June 6, 2021
Revised: June 16, 2021
Accepted: July 20, 2021
Article in press: July 20, 2021
Published online: September 16, 2021
Processing time: 125 Days and 20.7 Hours
At present, silicone oil has been widely used in vitrectomy to deal with complex fundus diseases. Usually, cataract extraction is combined with vitrectomy. However, reducing the complications of silicone oil tamponade and facilitating the secondary implantation of intraocular lens (IOL) are still an urgent problem.
To evaluate the clinical effect of vitrectomy combined with peripheral capsule preservation (PCP) in eyes with silicone oil tamponade.
This single-center retrospective analysis included 70 patients (73 eyes) who underwent vitrectomy and silicone oil tamponade combined with cataract surgery (stage I) between January 2015 and July 2019. All patients underwent selective reoperation for silicone oil extraction and IOL implantation (stage II) more than 3 mo after stage I. These patients were divided into three groups according to the different lens capsule preservation methods: 28 patients (31 eyes) in a whole capsule preserved (WCP) group, 17 (17 eyes) in a capsule absent (CA) group, and 25 (25 eyes) in a peripheral capsule preserved (PCP) group. Intraocular pressure (IOP), best-corrected visual acuity, surgery time, and other complications were recorded at each time point (1 d, 1 wk, and 1 mo after stages I and II).
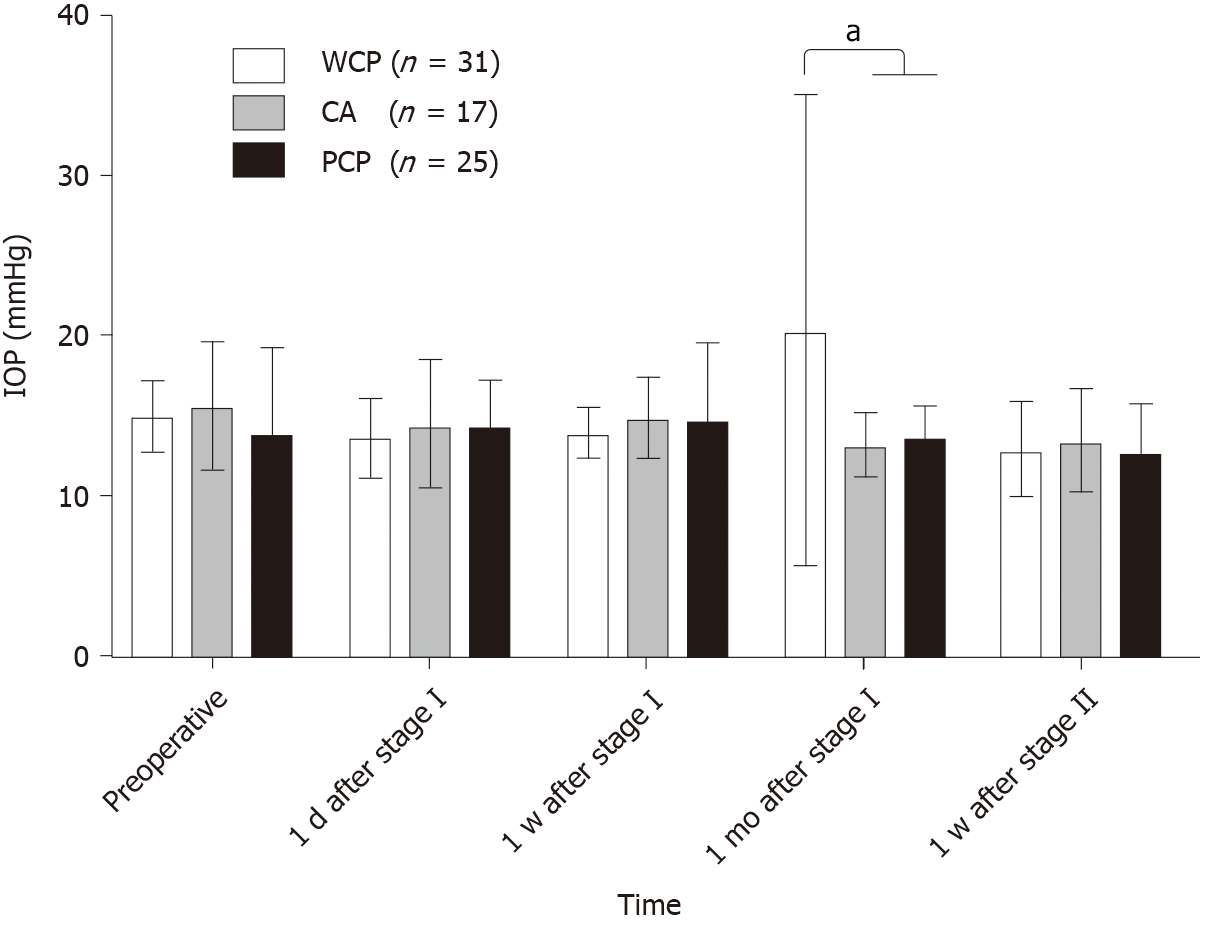
The IOP values were 14.9 ± 8.2 mmHg in the WCP group, 20.3 ± 13.0 mmHg in the CA group, and 14.2 ± 9.7 mmHg in the PCP group (P < 0.05) at 1 mo after stage I operation. Five eyes had IOP higher than 30 mmHg, and one eye in the WCP group appeared to have silicone oil entering the anterior chamber. There was no significant difference in IOP among the three groups at any other time point (P > 0.05). With IOL implantation, visual acuity improved significantly compared to stage I. The incidence rate of posterior capsule opacity was higher in the WCP group than in the other groups (P < 0.001). In the CA group, IOL deviation due to suture relaxation occurred in one case. There was no significant difference in the surgery time among the three groups in stage I (P = 0.618). In stage II, the surgery time of the PCP group and WCP group was significantly shorter than that of the AC group (P = 0.031).
Preservation of the peripheral capsule in vitrectomy combined with lens removal is a better option. This method has significant advantages in reducing intraoperative and postoperative complications.
Core Tip: This study retrospectively analyzed and compared the clinical effects of vitrectomy combined with cataract extraction in silicone oil-filled eyes under three different capsule retention conditions, including whole capsule preserved, capsule absent, and peripheral capsule preserved. We would like to promote a new surgical method to preserve the peripheral capsule membrane, effectively preventing silicone oil from entering the anterior chamber and reducing the operation time and complications associated with intraocular lens implantation.
- Citation: Jiang B, Dong S, Sun MH, Zhang ZY, Sun DW. Clinical effect of peripheral capsule preservation in eyes with silicone oil tamponade. World J Clin Cases 2021; 9(26): 7729-7737
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7729.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7729
Since the development of vitrectomy in 1962, many fundus diseases have been treated using this procedure. Silicone oil is widely used in vitrectomy for complex fundus diseases[1], and its effectiveness has been confirmed. However, long-term silicone oil tamponade will cause complications, including increased secondary intraocular pressure, complicated cataract formation, and corneal degeneration, especially when silicone oil enters the anterior chamber[2]. Vitrectomy is often combined with cataract extraction because of the influence of lens opacity on the observation of the fundus, or because of the presence of lens problems before vitrectomy; the capsule can be preserved intact or none. It is difficult to remove silicone oil when it enters the anterior chamber of an eye with a lens or an intact lens capsule. For aphakic eyes, Ando used peripheral iridectomy at 6 o’clock to solve the problem of silicone oil entering the anterior chamber[3]. However, in the second stage of silicone oil extraction and intraocular lens (IOL) implantation, IOL implantation becomes a challenge due to the loss of capsular support in aphakic eyes. At present, the most widely used method is to suspend the IOL from the sclera and fix the lens in place with sutures. However, this operation is complicated and may cause complications such as inflammatory reactions, intraocular pressure (IOP) fluctuation, IOL deviation,and dislocation.
Therefore, a new surgical method is needed to preserve the peripheral capsule membrane, effectively preventing silicone oil from entering the anterior chamber and reducing the operation time and complications associated with IOL implantation. This study retrospectively analyzed and compared the clinical effects of vitrectomy combined with cataract extraction in vitrectomized, silicone oil-filled eyes in three different capsule retention states.
The ophthalmology clinic at the Second Affiliated Hospital of Harbin Medical University, Harbin, China has carried out this single-center retrospective consecutive case series between January 2015 and July 2019. The study protocol was in accordance with the Declaration of Helsinki and was approved by the hospital’s Institutional Review Board.
The inclusion criteria were as follows: Patients were at least 18 years old; vitrectomy and silicone oil tamponade were performed for ocular trauma, endophthalmitis, rhegmatogenous retinal detachment with grade C proliferative vitreoretinopathy (PVR), stage VI proliferative diabetic retinopathy (PDR), or lens dislocation; regular postoperative follow-up was performed; 3-6 mo after stage I, the silicone oil was removed, and an IOL was implanted. Before stage II surgery, best-corrected visual acuity has improved by at least 5 letters.
The exclusion criteria were as follows: Patients with severe systemic disease; previous history of glaucoma, uveitis, age-related macular degeneration, or other ocular diseases affecting the prognosis of vision; and incomplete clinical data.
All patients underwent standard 23G three-port pars plana vitrectomy (Constellation, Alcon, United States), intraoperative combined cataract extraction (phacoemulsification, ultrasonic crushing, or lens resection), and silicone oil (Oxane 5700, Bausch+Lomb, United States) tamponade in stage I surgery.
In stage I surgery, the patients were divided into three groups according to the different degrees of capsule preservation.
Capsule absent (CA) group: The lens capsule could not be preserved, and Ando’s incision was performed. Patients had one of the following conditions: Lens capsule rupture, lens dislocation falling into the vitreous cavity, or severe endophthalmitis with exudative pupil block.
Peripheral capsule preserved (PCP) group: Eyes underwent cataract extraction, and the capsule was polished. Then, the central capsule was cut to a diameter of approximately 5 mm, combined with Ando’s incision. Eyes met one of following conditions: Cataracts with central calcification; lens opacity with dislocation of no more than one quadrant; rupture of the suspensory ligament at no more than 3 clock positions; penetrating injury of the iris and central area of the lens capsule; air bubbles or triamcinolone acetonide (TA) entering the anterior chamber when gas-fluid exchange occurred during surgery.
Whole capsule preserved (WCP) group: Patients with severe ocular fundus disease complicated with simple cataracts can preserve the anterior capsule or posterior capsule.
Within 3 to 6 mo after stage I surgery, silicone oil removal and IOL implantation could be performed if the patients met the following conditions: Retinal reattachment; no retinal proliferative membrane formation; best-corrected visual acuity improved by more than 5 Letters; elevated intraocular pressure caused by silicone oil emulsification or other reasons; average corneal endothelial cells no less than 1000/mm2.
In the stage II surgery, the silicone oil was extracted through 23G pars plana vitrectomy (Constellation, Alcon, United States). The peripheral sclera was pressed to check whether there was residual silicone oil. In serious emulsification of silicone oil, a gas-fluid exchange is used to remove silicone oil drops completely.
The specific steps of IOL implantation were as follows. In the CA group, parallel to the corneal limbus, a sclera flap with a thickness of 1/2 and a size of approximately 4 mm*3 mm was produced at the temporal and nasal horizontal position. A polystyrene (Alcon pair/Pak) long needle was inserted into the side of the scleral lamina to pass the preset suspension line from the opposite side, the preset suture was then passed through the two loop holes of the IOL and knot, the suture outside the scleral flap was tightened, and the IOL was adjusted to normal position. In the PCP and WCP groups, a corneal tunnel was made at the limbus, and then the iris and capsule were separated with a viscoelastic agent, after which the IOL was implanted into the ciliary sulcus.
The same surgeon performed all surgeries.
The patient’s basic information, including gender, age, chief complaint, current medical history, past history, course of disease, operation mode, and operation time, was reviewed. An international visual acuity chart was used to measure best-corrected visual acuity (BCVA), and BCVA was recorded. BCVA was converted into logMAR visual acuity for statistical analysis. A slit lamp was used to examine the anterior segment, indirect ophthalmoscopy to examine the ocular fundus, and intraocular pressure (Full Auto Tonometer TX-F; Canon, Japan) was measured. Additionally, ocular A/B ultrasound (MD-2300S, Tianjin of Medical Science and technology) and ultrasound biomicroscopy (UBM) were performed (UBM300, Tianjin of Medical Science and Technology). Color fundus photography (TRC-50 ex Japan Topcon), optical biological measurement (IOL Master 500, Carl Zeiss, Germany), and optical coherence tomography (OCT) (Heidelberg, Germany) were performed as well.
The IOP values of the three groups were compared at 1 d, 1 wk, and 1 mo after vitrectomy and 1 wk after IOL implantation. BCVA was measured 1 mo before and after vitrectomy and 1 mo after silicone oil removal combined with IOL implantation. Other complications were corneal edema, silicone oil entering the anterior chamber, anterior chamber reaction, endophthalmitis, retinal detachment, posterior capsule opacification, and IOL deviation. All patients were followed for at least 6 mo.
Statistical analyses were performed using Stata SE 13.1 (serial number 401306302851). Summary statistics were computed for continuous (mean and standard error) and categorical (counts and percentages) variables. Analysis of variance (ANOVA) was performed to evaluate differences in visual acuity, IOP, and surgery time. The Tamhani test was adopted for stage II surgery time among the three groups as the post hoc test. Pearson chi-square test was performed to evaluate BCVA among the three groups after IOL implantation. Values of P < 0.05 were considered statistically significant. Graphs were created using Prism 8 software (GraphPad Software, San Diego, CA, United States) and Excel (Microsoft Corp., Seattle, WA, United States).
Of 218 eyes in 190 patients who underwent vitrectomy and silicone oil tamponade combined with cataract surgery (stage I), 73 eyes in 70 patients underwent selective reoperation of silicone oil extraction and IOL implantation. The mean age of the patients in this study was 52.3 ± 14.7 years (38 males, 54.3%; 32 females, 45.7%). The average follow-up time was 211 ± 108 d (range, 151-272 d).
Of the 73 eyes with primary ocular diseases, 29 had PDR, and 32 had retinal detachment (RD), including 5 eyes with giant retinal tears, 4 with high myopia, and 5 with recurrent RD. Nine eyes had severe ocular trauma, including 8 with iris and/or lens penetrating injury (Table 1).
| WCP (n = 31) | CA (n = 17) | PCP (n = 25) | |
| PDR | 19 | 4 | 6 |
| Rhegmatogenous RD (PVR C) | 8 | 2 | 8 |
| Giant retinal detachment | 2 | 1 | 2 |
| Recurrent RD | 1 | 2 | 2 |
| RD of high myopia | 1 | 0 | 3 |
| Ocular trauma | 0 | 5 | 4 |
| Endophthalmitis | 0 | 3 | 0 |
Out of 73 eyes, 31 had the whole anterior or posterior capsule preserved through phacoemulsification or phacofragmentation (WCP group), 17 underwent lens resection without capsule preservation (CA group), and 25 underwent vitrectomy with central capsule removal and peripheral capsule preservation (PCP group).
Figure 1 shows the IOP values of the three groups at different time points after the operation (1 d, 1 wk, and 1 mo after vitrectomy and 1 wk after IOL implantation). There was a significant difference in IOP among the WCP, CA and PCP groups at 1 mo after the operation (P = 0.006). IOP of the WCP group was significantly different from that of the CA group and the PCP group (P = 0.012, 0.041), but there was no significant difference between the CA and PCP groups (P = 1.000). There was no significant difference among the three groups at other time points.
In this study, five patients in the WCP group had elevated IOP; in one eye, it was caused by silicone oil entering the anterior chamber during the follow-up within 1 mo after stage I surgery. After emergency treatment of partial aqueous humor drainage and silicone oil aspiration by anterior chamber puncture, we were forced to perform stage II surgery to remove the intraocular silicone oil. In the CA group, four patients had elevated IOP due to Ando’s incision atresia (fiber exudation, hemorrhage, etc.). We performed anterior chamber puncture to reopen Ando’s incision and kept the patients prone to maintain aqueous circulation and promote the return of the silicone oil to the posterior chamber, and in this manner, IOP was restored to the normal range.
There were no statistically significant differences in the incidence of corneal edema or anterior chamber/intraocular reaction among the three groups (P = 0.82, P = 1.00, and P = 0.23, respectively).
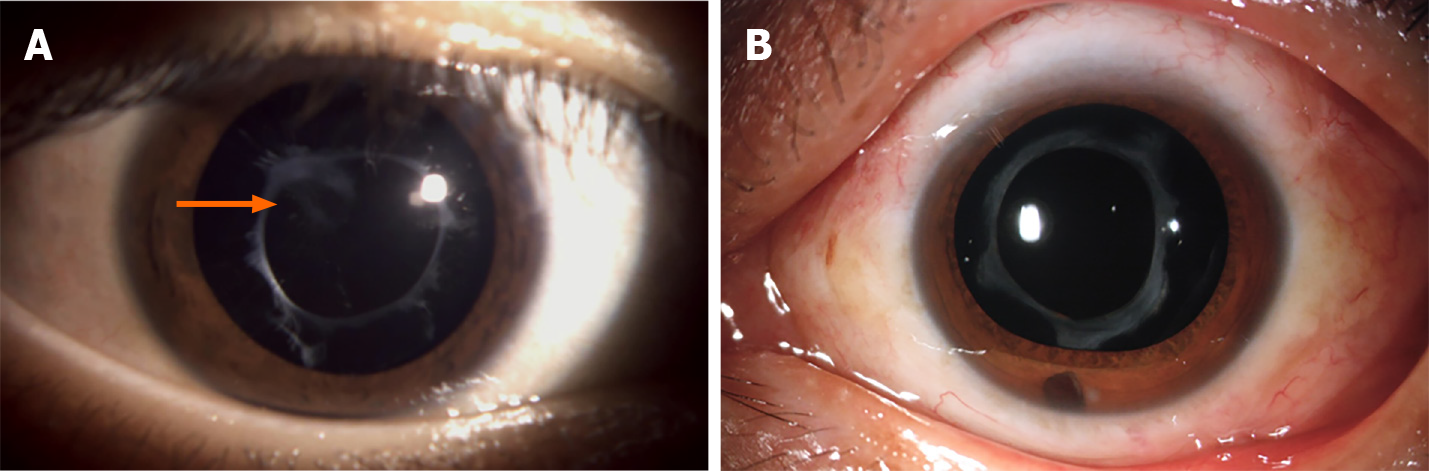
There was no statistically significant difference among the three groups in visual acuity preoperatively, 1 mo after surgery in stage I, or 1 mo after surgery in stage II (F = 1.39, 0.32, and 0.16; P = 0.26, 0.73, and 0.85, respectively) (Tables 2 and 3). However, the incidence of posterior capsular opacity in the PWC group was significantly higher than that in the other two groups (P < 0.001) (Figure 2).
| Group | Number of eyes | Preoperative | 1 mo after stage I | 1 mo after stage II |
| WCP | 31 | 1.04 ± 0.38 | 1.39 ± 0.52 | 0.93 ± 0.28 |
| CA | 17 | 1.14 ± 0.53 | 1.29 ± 0.55 | 0.94 ± 0.45 |
| PCP | 25 | 1.26 ± 0.58 | 1.41 ± 0.42 | 0.99 ± 0.45 |
| F | 1.39 | 0.32 | 0.16 | |
| P value | 0.26 | 0.73 | 0.85 |
| WCP | CA | PCP | P value | |
| BCVA improved | 29 (93.55) | 16 (94.12) | 24 (96) | 0.92 |
| BCVA deteriorated | 2 (0.06) | 1 (5.88) | 1 (4) | - |
There was no significant difference in the surgery time among the three groups in stage I (P = 0.618). In stage II, the surgery time of the PCP group and WCP group was significantly shorter than that of the AC group (P = 0.031)(Tables 4 and 5).
| Group | Stage I | Stage II | ||
| mean ± SD | P value | mean ± SD | P value | |
| WCP | 72.74 ± 26.90 | 0.618 | 5.58 ± 1.19 | 0.031a |
| CA | 78.91 ± 16.05 | 15.38 ± 2.04 | ||
| PCP | 78.16 ± 26.39 | 5.74 ± 1.32 | ||
| Group | P value | 95%CI |
| WCP vs PCP | 0.954 | -0.95-0.626 |
| WCP vs CA | < 0.01 | -10.68-(-8.92) |
| PCP vs CA | < 0.01 | -10.56-(-8.72) |
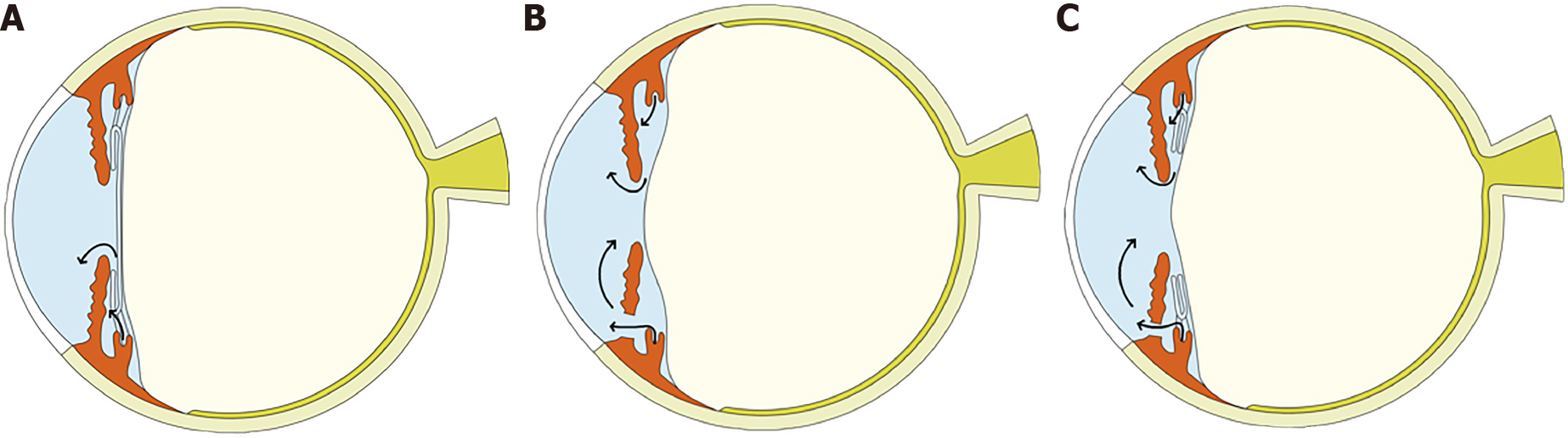
In a vitrectomy, the lens sometimes cannot be preserved for various reasons. When ocular fundus disease is stable, the patient will face IOL implantation again[4]. In a vitrectomy, a preserved lens capsule can reduce the difficulty of subsequent IOL implantation and maintain the IOL in the center of the pupil. Compared with the safe and conventional operation method, there were many advantages such as minor incision and less damage to ocular tissue[5]. However, for patients with loose lens ligaments, silicone oil can enter the anterior chamber after vitrectomy, and the incidence is 3.6% to 29.5%[6,7], which causes extremely high intraocular pressure that drugs cannot control. At this time, anterior chamber puncture is needed to remove silicone oil to relieve the angle block, but reducing the quantity of silicone oil in the vitreous cavity is not conducive to the recovery of ocular fundus diseases (Figure 3A). This study observed silicone oil entering the anterior chamber in five eyes with an axial length greater than 26 mm. It is speculated that the reason may be the relaxation of the lens suspensory ligament due to axial growth, especially the superior nasal or temporal lens suspensory ligament. In one case, silicone oil had to be removed due to repeated entry into the anterior chamber. In the second stage IOL implantation, the postoperative inflammatory reaction of the WCP group was mild, intraocular pressure was stable, and the IOL was successfully implanted into the ciliary sulcus. Still, there was capsular opacity. Therefore, Nd:YAG laser posterior capsulotomy was needed to further improve visual acuity.
For eyes in which it is impossible to preserve the complete capsule, we usually remove the entire lens. Due to the pathway between the vitreous cavity and anterior chamber, silicone oil can easily enter the anterior chamber, but Ando’s incision can allow the aqueous humor to enter the anterior chamber and effectively keep the silicone oil inside the vitreous cavity[8,9] (Figure 3B). Even if silicone oil enters the anterior chamber, the aqueous humor can enter the anterior chamber through the prone position and push the silicone oil back to the vitreous cavity. In this study, four eyes had exudation that caused iris Ando’s incision closure, resulting in increased IOP. After anterior chamber puncture or Nd:YAG laser treatment to reopen Ando’s incision, the IOP returned to the normal range without extracting silicone oil from the anterior chamber, avoiding the loss of silicone oil filling, which is conducive to the recovery of fundus diseases. For patients without capsular support, posterior chamber ciliary sulcus suture fixation is often used during IOL implantation, which places the IOL closer to the physiological position of the lens. Compared with anterior chamber IOL, it has less interference on corneal endothelial cells, angle, and iris. Therefore, the incidence of pupillary block and uveitis glaucoma anterior chamber syndrome is lower[10]. However, IOL fixation increases the operation steps and operation time, and even in some patients with conjunctival and scleral scarring, it undoubtedly increases the operation difficulty. In addition, the fixation of each loop requires two knotting operations, namely, knot tying at the intraocular loop and knot tying under the 10-0 suture of the scleral flap, which increases the risk of suture-related long-term complications, such as loosening, rupture, or erosion of the sutures[11]. In this study, one patient in the CA group had one loose knot, which caused deviation of the IOL.
In addition to the above two capsular preservation methods, we observed PCP (Figure 3C). In this study, the intraocular pressure was normal in the PCP group after stage I surgery, and no silicone oil entered the anterior chamber. In stage II IOL implantation, the IOL is implanted into the ciliary sulcus through the corneal limbal puncture, which can reduce the number of operation steps and the difficulties of suturing the IOL and thus avert the above complications[12]. Compared with eyes with a full capsular membrane, the effect of peripheral capsule opacity on central vision is reduced, which is conducive to the observation of fundus and retinal laser photocoagulation after vitrectomy.
In this study, the incidence of band-shaped degeneration of the cornea was very low. Corneal band-shaped degeneration is due to the long-term contact between silicone oil and corneal endothelium, which affects the metabolism of corneal endothelial cells. Although silicone oil enters the anterior chamber in the two groups, silicone oil retreats after timely treatment to avoid the occurrence of corneal degeneration[13,14].
Above all, preservation of the peripheral capsule in vitrectomy combined with lens removal is a better option. This method has significant advantages in reducing intraoperative and postoperative complications.
PCP in vitrectomy surgery can reduce the incidence of silicone oil entering the anterior chamber, thus avoiding elevated intraocular pressure and corneal degeneration. In stage II IOL implantation, the support of the peripheral capsule can be used properly to implant the IOL into the ciliary sulcus, thus avoiding the complexity and complications of IOL suspension. In addition, it avoids the trouble of posterior capsular membrane preservation and the necessity of an Nd:YAG laser in posterior capsular opacity. Therefore, in treating severe fundus vitrectomy combined with lens removal, preserving the peripheral capsule is a better method.
In order to better treat complex fundus diseases, cataract extraction is widely combined with vitrectomy due to the influence of lens opacity on fundus observation or lens problems before vitrectomy.
Long-term silicone oil tamponade will cause some complications, especially when silicone oil enters the anterior chamber. It is difficult to remove silicone oil when the anterior chamber of an eye has lens or intact lens capsule. However, in the second stage of silicone oil extraction and intraocular lens (IOL) implantation, IOL implantation becomes a challenge due to the loss of capsular support in aphakic eyes.
This study aimed to evaluate the clinical effect of vitrectomy combined with peripheral capsule preservation (PCP) in eyes with silicone oil tamponade.
This single-center retrospective study analyzed the patients who underwent vitrectomy and silicone oil tamponade combined with cataract surgery (stage I). All patients underwent selective reoperation for silicone oil extraction and IOL implantation (stage II) more than 3 mo after stage I. These patients were divided into three groups according to the different lens capsule preservation methods used: Whole capsule preserved (WCP) group, capsule absent (CA) group, and peripheral capsule preserved (PCP) group. The main indicator was intraocular pressure (IOP) at each time point.
There was no significant difference in IOP among the three groups at any other time point, but five eyes had IOP higher than 30 mmHg, and one eye in the WCP group appeared to have silicone oil entering the anterior chamber. With IOL implantation, the surgery time of the PCP and WCP groups was significantly shorter than that of the AC group, and the incidence rate of posterior capsule opacity was higher in the WCP group than in any other groups. In the CA group, IOL deviation due to suture relaxation occurred in one case.
Peripheral capsule preserved in vitrectomy combined with lens removal for treatment of severe fundus diseases is an effective method, which can prevent silicone oil from entering the anterior chamber, maintain normal intraocular pressure, facilitate secondary IOL implantation, and reduce intraoperative and postoperative complications.
In vitrectomy combined with cataract surgery, different capsular preserved status plays different roles in the occurrence of postoperative complications and secondary surgery. Preserving the peripheral capsular can reduce the incidence of postoperative complications and the difficulty of IOL implantation.
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bor'i A S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Guo X
| 1. | Deuchler S, Ackermann H, Singh P, Kohnen T, Wagner C, Koch F. Key Factors to Improve the Outcome of Retinal Reattachment Surgery in Proliferative Vitreoretinopathy and Proliferative Diabetic Retinopathy. J Ophthalmol. 2017;2017:2323897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Feng X, Li C, Zheng Q, Qian XG, Shao W, Li Y, Li W, Yin L, Wang Y, Gao Q. Risk of silicone oil as vitreous tamponade in pars plana vitrectomy: A Systematic Review and Meta-Analysis. Retina. 2017;37:1989-2000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Laganowski HC, Leaver PK. Silicone oil in the aphakic eye: the influence of a six o'clock peripheral iridectomy. Eye (Lond). 1989;3 ( Pt 3):338-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Treumer F, Bunse A, Rudolf M, Roider J. Pars plana vitrectomy, phacoemulsification and intraocular lens implantation. Comparison of clinical complications in a combined vs two-step surgical approach. Graefes Arch Clin Exp Ophthalmol. 2006;244:808-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 88] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Alió JL, Toffaha BT, Peña-Garcia P, Sádaba LM, Barraquer RI. Phakic intraocular lens explantation: causes in 240 cases. J Refract Surg. 2015;31:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | Sugiura T, Kaji Y, Tanaka Y. Anatomy of the ciliary sulcus and the optimum site of needle passage for intraocular lens suture fixation in the living eye. J Cataract Refract Surg. 2018;44:1247-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol. 2005;50:429-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 241] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 8. | Bausili Portabella MM, Nadal J, Alvarez de Toledo J, Fideliz de la Paz M, Barraquer RI. Long-term outcome of scleral-sutured posterior chamber intraocular lens: a case series. Br J Ophthalmol. 2020;104:712-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Riazi M, Moghimi S, Najmi Z, Ghaffari R. Secondary Artisan-Verysise intraocular lens implantation for aphakic correction in post-traumatic vitrectomized eye. Eye (Lond). 2008;22:1419-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Czajka MP, Frajdenberg A, Stopa M, Pabin T, Johansson B, Jakobsson G. Sutureless intrascleral fixation using different three-piece posterior chamber intraocular lenses: a literature review of surgical techniques in cases of insufficient capsular support and a retrospective multicentre study. Acta Ophthalmol. 2020;98:224-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Kokame GT, Yanagihara RT, Shantha JG, Kaneko KN. Long-term Outcome of Pars Plana Vitrectomy and Sutured Scleral-Fixated Posterior Chamber Intraocular Lens Implantation or Repositioning. Am J Ophthalmol. 2018;189:10-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Obeng FK, Vig VK, Singh P, Singh R, Dhawan B, Sahajpal N. Posterior Chamber Scleral Fixation of Intraocular Lenses in Post-Vitrectomised Aphakic Eyes. J Clin Diagn Res. 2017;11:NC09-NC13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Jabbour E, Azar G, Antoun J, Kourie HR, Abdelmassih Y, Jalkh A. Incidence and Risk Factors of Ocular Hypertension following Pars Plana Vitrectomy and Silicone Oil Injection. Ophthalmologica. 2018;240:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Moisseiev E, Ohana O, Gershovitch L, Barak A. Visual prognosis and complications following silicone oil removal. Eur J Ophthalmol. 2013;23:236-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |