Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7433
Peer-review started: February 5, 2021
First decision: March 7, 2021
Revised: March 17, 2021
Accepted: August 13, 2021
Article in press: August 13, 2021
Published online: September 6, 2021
Processing time: 206 Days and 11.6 Hours
The uncertainties about coronavirus disease 2019 (COVID-19), the change in routine, lifestyles and the reduction of physical contact can cause stress, anxiety, emotional overload, poor sleep and even physical health complications.
To evaluate the scientific publications available on the relationship between COVID-19 and anxiety experienced in the general population, during the period of social isolation, adopted by governmental organizations and public health policymakers as a measure to contain the spread of cases.
A literature search was performed systematically exploring the PubMed and Medline databases using the following terms classified as MeSH descriptors: (“anxiety” AND “pandemic” AND “COVID-19”). For the search, in the Biblioteca Virtual em Saúde – BVS, Science.gov, Web of Science and National Library plat
After applying the inclusion criteria, seven (n = 7) original scientific articles were selected. The collated evidence demonstrated increased levels of symptoms of anxiety and depression during the period of social isolation. The population between 21 to 40 years was most affected. The risk of severe depression was twice as high at the epicenter of the pandemic. Sleep quality was significantly impaired. Questions about politics, religion, and consumption of products from China were found to generate fear and anticipate probable changes in the pattern of post-pandemic consumption. Social isolation exacerbated feelings of extreme hope
We conclude that there is a potential relationship between social isolation during the COVID-19 pandemic and symptoms of anxiety. It is important to note that the direct and indirect costs of not identifying the detrimental effects of this phenomenon and neglecting strategies for intervention could lead to a significant psychological burden on society in several aspects after social isolation.
Core Tip: There is a potential relationship between social isolation during the coronavirus disease 2019 pandemic and symptoms of anxiety. The population between the age of 21 to 40 years is notably most affected. The risk of severe depression is noted to be twice as high at the epicenter of the pandemic. Sleep quality was signi
- Citation: Santos ERRD, Silva de Paula JL, Tardieux FM, Costa-e-Silva VN, Lal A, Leite AFB. Association between COVID-19 and anxiety during social isolation: A systematic review. World J Clin Cases 2021; 9(25): 7433-7444
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7433.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7433
In December 2019 a group of patients was hospitalized due to viral pneumonia caused by a microbial agent, hitherto unidentified. The patients were epidemiologically linked to the Huanan seafood market in Wuhan, Hubei Province, China. Shortly afterward, a new coronavirus that infects humans, which probably originates from bats, was identified as the etiologic agent that caused the hospitalizations. Until then, among the various types of coronavirus, majority caused only mild clinical symptoms, except for severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus. However, the new typing identified in Wuhan also proved to be dangerous[1,2].
The spread of the coronavirus was a decisive contributor to unleashing an unprecedented worldwide public health crisis. Transmission of this virus occurs through droplets and aerosols that disperse through the air when someone contagious sneezes, coughs, or speaks[3]. Another form of transmission can also occur through contact and fomites on which the virus can lodge for hours, or days[4,5].
In this context, coronavirus disease 2019 (COVID-19) manifests clinically from mild to severe and varies substantially according to the age and sexual characteristics of the patients. One of the most frequent manifestations in mild and moderate cases is predominantly olfactory dysfunction. Severe cases present with a higher risk for older men with comorbid underlying hypertension, cardiovascular, malignant and chronic renal diseases with signs of dyspnea and nausea[6,7].
The uncertainties about COVID-19, the change in routine, lifestyles and the reduction of physical contact can cause stress, anxiety, emotional overload, poor sleep and even physical health complications. A report released by the Centers for Disease Control and Prevention released a report in August 2020 highlighting the considerable rise in adverse mental health conditions. The most affected groups identified were younger adults, ethnic minority groups, essential workers, and adult caregivers. The coronavirus pandemic brought panic and fear in various aspects of individual lives. Therefore, in addition to the need for attention to the physical and biological aspects related to this disease, it is relevant to carry out an analysis of the aspects related to the mental and emotional health of people who are following the guidelines of global health authorities, to maintain social isolation as a strategy to reduce contagion by the coronavirus[5].
In case of exposure to frightening situations, a cascade of events involving hormones and neurotransmitters such as serotonin, dopamine, norepinephrine is activated in humans, which prepare the individual to react, which represents positive anxiety, which helps to maintain the species in nature[8,9]. With extended periods of social isolation, vulnerable groups of people start to manifest, the signs of pathological anxiety, which in addition to activating the state of constant alertness, enhances the feeling of fear and despair to cope with unexpected circumstances and future uncertainties. This condition presents itself as generalized discomfort in homeostasis, as it alters cardiorespiratory systems (tachycardia, shortness of breath), digestion bringing changes in appetite and usually accompanied by sleep disorders[10].
This constellation of disorders associated with the limbic system, the brain unit specialized in dealing with emotions when it comes to anxiety is still little explored in situations such as the COVID-19 pandemic. Sensations of fear, pathological anxiety generated by the process of social isolation, quarantine and restrictions adopted by most health authorities in nations affected by the coronavirus are important at the same time they have an impact on the economy, fall in income generation and rising unemployment[8,10].
This systematic review aimed to evaluate the scientific publications available on the relationship between COVID-19 and the anxiety experienced by individuals in the general population, during the period of social isolation.
It is a qualitative systematic review to identify original articles about the relationship between COVID-19 and the anxiety experienced by the general population over the age of 18 years, in the period of social isolation.
The search and selection of studies were carried out in the Pubmed and Medline databases using the following terms classified as keywords of the MeSH: (“anxiety” AND “pandemic” AND “COVID-19”). For the search, in the Biblioteca Virtual em Saúde - BVS, Science.gov, Web of Science and National Library platforms, the following keywords were used: (“anxiety” AND “coronavirus” AND “social isolation”). The keywords were combined using the boolean operator AND, with a reference period established for the bibliographic survey from 2019 to 2020, and data extraction were from March 1 to April 30, 2020. An active search was also carried out on the references of the selected articles.
Inclusion criteria: The following items were observed: Original research articles that discussed the association of "anxiety", "social isolation", "coronavirus", detected in the title and/or abstract structure; studies carried out with the general population over the age of 18 years, and manuscripts must be published in English.
Exclusion criteria were: Studies that did not present a degree for the measurement (scales) of anxiety symptoms related to COVID-19 were excluded. Besides that, articles structured in the modalities: systematic review; narrative review; speeches; editorials; conference abstracts were excluded. Duplicate articles, reviews performed exclusively with gray literature, studies on COVID-19 and anxiety with specific groups of the population at greatest risk, such as health professionals, adolescents, children, pregnant women, and people with comorbidities (diabetes, systemic arterial hypertension, oncological disease, mental disorder, neurological or renal pathology) were also excluded.
Initially, the titles and abstracts of the articles found in the search were manually reviewed, to identify the studies that met the eligibility criteria. Then the full texts were evaluated including reference lists to identify other relevant articles. Both procedures were performed by two independent reviewers, with blinding. Subsequently, the divergences were compared and actions were taken to adjust them in a consensual way.
After the application of the descriptors, combined with each other, in an integrated search in the fields, information about data of interest was extracted in predefined forms, with the inclusion of fields for the annotation of health outcome variables, data sources of outcomes, year of publication of studies, the period of occurrence of the assessed outcomes, locations investigated and origin. From the data of each study were selected: author/date, objective, method, result, and conclusion.
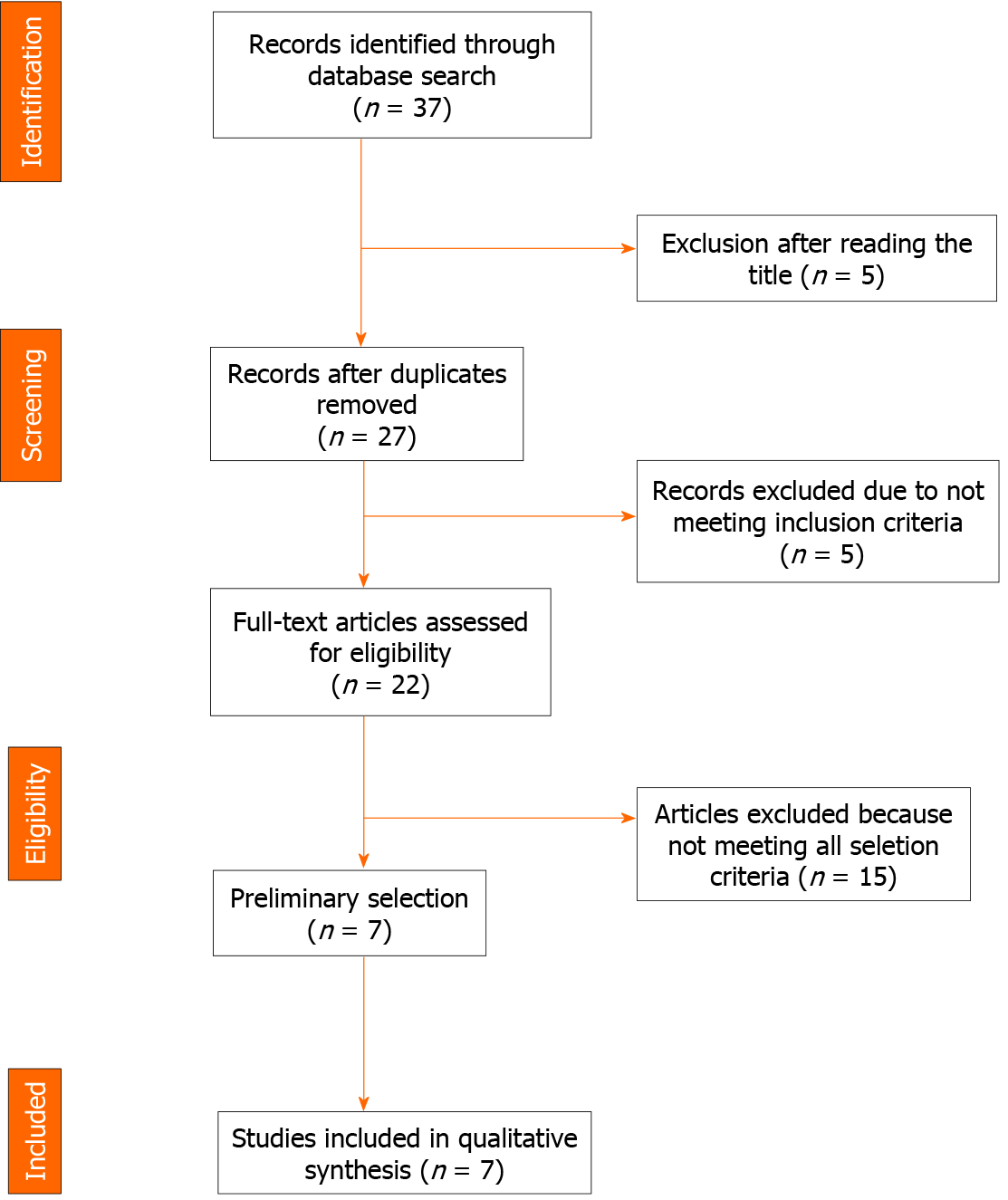
The PRISMA tool (Preferred Reporting Items for Systematic Reviews and Meta-analyzes) was used as a guide in the selection of review articles[11,12].
The scientific articles examined in this systematic review study were evaluated concerning the methodological adequacy used in the sample selection, collection, and data analysis from the scores of the quality assessment instrument Checklist Downs & Black, adjusted for observational studies, with a scale ranging from 0 to 15 points[13].
Following items were examined in each study: Definition of objectives and outcome measures; definition of inclusion and exclusion criteria, as well as the period and place of the study; sampling procedures (population, attrition, bias, standard deviation, confidence interval); description of methods for measuring outcomes; and adequate statistical analysis (calculation of power and control of confounding factors).
The main results of the selected studies were grouped into thematic categories and discussed based on a narrative synthesis. To define the thematic categories, the content analysis technique was adopted, the tool used to assess the quality of the studies was the condensation matrix of meanings, which helped in the systematization of the items assessed as to the components of methodological quality. The extracted data were based on the results evaluated in each cross-sectional study.
Of the total of 37 articles that were found in the databases the breakdown was as follows: (n = 2) case reports; (n = 1) lecture; (n = 2) editorials; (n = 15) review articles; and (n = 12) original articles.
The evaluation performed by pairs of reviewers during the initial screening strategy removed (n = 20) articles that did not meet the selection criteria. Manuscripts were also removed in the modalities of literature reviews, editorials, and case reports (n = 10), resulting in (n = 7) studies submitted to full reading and analysis (Figure 1). There was 100% interobserver agreement.
The origin of the studies evaluated in this review is highlighted in four countries: The United State of American, China, Iran, and Turkey.
When evaluating the objectives of the studies described in this systematic review, all declared that they sought to fill the gaps in the literature with regards to mental health in the case of the COVID-19 epidemic, in the general population. These studies also attempt to address the lack of application tools to measure the impact of social isolation for those who suffer with disorders like anxiety, stress, and depression.
Regarding methods, all studies used a cross-sectional design, using psychometric scales[14] applied via the internet from social networks, self-reported already tested for anxiety in other studies, such as the Beck Anxiety Inventory (BAI), used in two of the studies examined in this sample[15-19].
The most common scales used were: Personal Social Capital Scale 16, Likert Scale, Self-Rating Anxiety Scale (SAS) and Stanford Acute Stress Reaction Scale[20]; The Pittsburgh Sleep Quality Index questionnaire[17,20]; Self Reporting Questionnaire[17]; The Depression Anxiety Stress Scales (DASS)[19]; BAI; and Beck Depression Inventory-II[18]. In addition to these, the Alcohol Use Disorders Identification Test[18]; The Warwick Edin Scale[18]; Work and Social Adjustment Scale[16]; Coronavirus-related anxiety assessment scale - Coronavirus Anxiety Scale (CAS), made specifically for the measurement of anxiety signs related to COVID-19[16]. The Self-Assessment Anxiety Scale (SAS) was also used; Self-Assessment Depression Scale[15]; Hospital Anxiety and Depression Scale; and Health and Anxiety Inventory[14,20]; and DASS[19].
The studies used the scales in populations with varied sample numbers, the smallest with 170 respondents and the largest with 10754. In all the studies, more than one scale was used, in addition to the fields for declaring the respondents' demographic data. An instrument of process technological innovation was identified, from the creation of CAS as the first published psychometric scale, related to COVID-19, validated in a large sample[16].
The main sociodemographic variables most used were sex, age, education, place of residence, history of smoking, previous history of mental disorder, cohabitation with people over 60 years old. The number of household members; use of health services and; comorbidities of chronic disease were the other commonly studied variables.
The relative variables collected on the psychometric scales, applied via the internet from social networks, measured the symptoms of self-reported anxiety, compatible with important symptoms such as fear, stress, and generalized anxiety disorder (GAD).
When the results of the studies were evaluated, the scales measured symptoms of self-reported anxiety, compatible with important symptoms of panic attacks and GAD, such as dizziness, nausea, and abdominal discomfort[21,22].
Findings with statistical significance signaled the following risk factors that lead to increased likelihood to develop anxiety symptoms, such as place of residence in an urban area, subjects with a history of emotional instability or previous mental disorders, constant exposure to news, (or other media outlets that focused on deaths), morbidities of chronic illness, death of relatives or close friends due to COVID-19. There was evidence that the levels of anxiety and depression were detected on a larger scale during the isolation period[14,20].
A study demonstrated significant evidence that young people aged 21 to 40 were in a more vulnerable position in terms of mental health conditions and alcohol use (6 times higher risk for men)[19]. The risk of severe depression was twice as high in Hubei when compared to the population of other provinces in China (the epicenter of the pandemic)[17].
In most studies, quality of sleep was mentioned as a very impaired element and when associated with the profession, the effect was most pronounced for the personnel involved in the healthcare and business sectors. Issues related to international politics, religion, consumption of products from China, were also mentioned as the object of much fear and a probable change in the consumption pattern for the future. Extreme hopelessness and suicidal ideation were also reported in the worst moments of loneliness experienced during social isolation[8,9,17].
There was a linear correlation for severity in anxiety symptoms related to exposure to news about the coronavirus. News of the death of a relative or close person also contributed to exacerbating the symptoms. Overburdened hospitals and the fear of the collapse of the health care system were also cited as being of great relevance for increasing levels of anxiety in the confined population[21].
A narrative summary of these studies is presented in Table 1. The peculiarities of the content of each original study are highlighted. All studies also stated that there was no conflict of interest.
| Ref. | Location, year | Sample | Objective | Psychosometric Scales | Statistical analysis | Key results | Conclusion |
| Özdin and Bayrak Özdin[14], 2020 | Turkey, 2020 | 343 | To assess levels of depression, health anxiety in Turkish society during the COVID-19 pandemic and examine the factors that affect them. | Hospital Anxiety and Depression Scale; Health and Anxiety Inventor. | Logistic regression and multiple linear regression. | Risk factors for depression and anxiety, living in urban areas. Risk factor for depression, female, residing in urban areas and previous psychiatric illness. | The groups most affected psychologically by the pandemic are women, individuals with previous and current psychiatric illnesses, who living in urban areas, and those with a comorbid chronic disease |
| Lei et al[15], 2020 | China, 2020 | 1.593 | To evaluate and compare the prevalence and associated factors of anxiety and depression among the public affected and unaffected by quarantine during the COVID-19 outbreak | SAS; Self-assessment depression scale. | χ2 test and U Mann-Whitney test, and ANOVA | The most affected group, prone to have poor health and worrying about getting infected | The prevalence of anxiety and depression in the affected group is higher than the unaffected group, during the COVID-19 outbreak, with factors associated with serious material damage and low self-perceived health status |
| Lee[16], 2020 | United States, 2020 | 775 | To develop and evaluate the properties of a mental health screening scale that health professionals and researchers can readily use to identify likely cases of dysfunctional anxiety associated with coronavirus | Work and Social Adjustment Scale, adapted; CAS. | It was used to examine the construct validity and diagnostic viability of the coronavirus anxiety symptoms using a series of correlations and receiver operating characteristic analyses | The anxiety measured by CAS regarding Coronavirus was strong and positively correlated with functional incapacity, confrontation with alcohol or drugs, negative religious confrontation, extreme hopelessness, and passive suicidal ideation | The results support the CAS scale as an accurate diagnostic tool for mental health screening with strong classification characteristics, efficient and valid for research and clinical practice, and the first created to assess anxiety directly related to COVID-19 |
| Yuan et al[17], 2020 | China, 2020 | 939 | To compare the emotional state, somatic responses, quality of sleep and behavior of people in Hubei province with non-endemic provinces in China for two weeks in February 2020 | Stress Response Questionnaires; PSQI. | χ2 tests and ANOVA | Sleep disorders have increased significantly in people aged 18 to 24. COVID-19 anxiety was positively correlated with all somatic symptom signatures and the full scale score. The subscales of somatic symptoms were all highly and positively correlated, and the correlations with GAD were higher than for the COVID-19 anxiety score | There are levels of anxiety that affect quality of life during epidemics, including periods of population quarantine or self-isolation |
| Ahmed et al[18], 2020 | China, 2020 | 1.074 | To approach in literature Gap in psychological morbidity induced by the current COVID-19 epidemic also systematically reviews the prevalence of Political problems due to the prolonged confinement of itizens | Beck's Anxiety Inventory; Beck Depression Inventory II; Alcohol Use Disorders Identification Test; Warwick Edin-Scale | Descriptive statistics and | There were significant differences in depression and alcohol abuse among respondents from different localities.Young people aged 21-40 are more vulnerable in terms of mental health and alcohol use, with the risk being six times higher among men | It has been exposed that simple infection does not cause psychological problems, but a social behaviour due to infection/illness. The prevalence of anxiety, depression and alcohol use due to isolation and widespread economic damage has made many people psychologically problematic |
| Moghanibashi-Mansourieh[19], 2020 | Iran, 2020 | 10.754 | To assess the level of anxiety of the general Iranian population during the outbreak of COVID-19 | Depression Anxiety Stress Scales | They were analyzed by descriptive statistics (frequency distribution, mean and standard deviation) and inferential statistics (χ2 tests, independent t-test and analysis of variance) | The level and severity of anxiety symptoms were significantly higher among people living in an area of high prevalence of COVID-19; higher among women in the age group 21 to 40; at a higher level of education; and among people who had at least one family member, relative or friend with the disease | The more people followed the news about the coronavirus, the more the level and severity of anxiety symptoms increased. Especially when a relative or close person died |
| Xiao et al[20], 2020 | China, 2020 | 170 | To Investigate the effects of social capital on sleep quality and the mechanisms involved in people who were isolated at home for 14 days in January 2020 during the COVID-19 epidemic in central China | Anxiety Scale Self-Rating Questionnaire; SASR; PSQI; Likert Scale | Path analysis, or multiple regression analysis, using Pearson correlation analysis (r) and structural equation modeling with a bootstrap number set as 5000 to test | Pearson's correlation analysis showed that the Personal Social Capital Scale 16 score for social capital was positively associated with the SAS score for anxiety, the SASR score for stress and the PSQI score for sleep quality. The SAS anxiety score for study participants was positively associated with the SASR stress score and the PSQI score for sleep quality | During a period of individual self-isolation in the COVID-19 virus epidemic, increased social capital improved sleep quality, reducing anxiety and stress |
This systematic review identified from the studies selected in the sample the presence of a significant correlation between COVID-19 and anxiety in the period of social isolation. The most significant findings confirmed: the predominancy of anxiety generated during the period of social isolation in the younger age group (20-40 years), the important role of the internet in the pandemic, and government action on strategic measures for mental health was insufficient.
The results from this systematic review corroborate the findings of identifying the risk factors for the development of anxiety and depression as a result of social isolation related to COVID-19 in various dimensions (gender, age, lifestyle, economy, place of residence, psychological, cognitive, behavioral and emotional aspects). It was observed that women of younger age, single, widows, divorced, who live alone, slept little and felt loneliness, were associated with a higher risk of problems in the components of anxiety and/or depression[14,23]. There was a perception that loneliness has different effects between genders, when compared, lonely women are more prone to developing anxiety whereas men were noted to be more prone to depression[24].
The physical distancing or social isolation, although protect against the spread of the disease resulted in loneliness especially for vulnerable groups, generating anxiety and distress, which are the most common mental health complaints. Other adverse outcomes include psychiatric suffering, rise in suicidal ideation, and higher concerns among women about the impact of the pandemic[25,26].
The prevalence of mental disorders during periods of the epidemic, especially anxiety, reduces individuals' resilience against virus infection and can cause irreparable economic, social, cultural, and psychological problems for people in the future (immune system under shock)[22]. The COVID-19 pandemic has a significant influence on mental health. In this perspective, close monitoring of the vulnerable group and early recognition and treatment is a priority according to a study that analyzed psychological health during this global pandemic crisis[25-27]. Another study supports the findings of our review, we show that female gender, higher education, and younger age are associated with a higher risk of experiencing anxiety (P < 0.05). Women, young people, with low physical activity, and singles were associated with higher depression levels (P < 0.05)[24].
The results showed that the people who closely follow the news on the COVID-19 experienced greater symptoms of anxiety. Although necessary to keep the general public updated with the progress of the pandemic, it is also of prime importance to provide outlets for moral support and emotional wellbeing for the general public. This is markedly unexplored at the moment and provides a good point of a potential intervention[19,23,27].
Another study reports that less frequent check-in on current affairs was associated with 19% lower risk of worsening the symptoms of anxiety[24]. The experience of isolated and quarantined people is stressful and makes face-to-face and other communication impossible. The wide range of information about the COVID-19 epidemic through digital media, often with false content, was associated with increased concern and anxiety for people in social isolation[28].
From the point of view of public health administrators and policymakers, it is necessary to concentrate efforts to plan and execute interventions on the negative effects of social isolation, particularly anxiety, sadness, loneliness, as well as symptoms of post-traumatic stress, which can effectively meet the needs of individuals[26,29-31].
Most of the studies at the time of inception of this idea before data collection were narrative reviews, editorial with opinions, case reports, which reveal a low and medium quality of studies due to little methodological rigor and high risk of bias. In this systematic review, all the studies included were of the cross-sectional type, which revealed the first attempts of original works. Some of the studies still had some methodological problems, such as the sample selection (questionnaires available to the population over 18 years old, with access to popular social media in respective countries of origin). The responses were self-reported, so this is considered a limitation[14-20].
All studies were cross-sectional and sought to adapt the method to an atypical pandemic situation, in which personal contact was not possible. Among the strengths of the methodology of the studies, the large number of individuals surveyed in most of the studies stands out, some of them with national representativeness. The novelty of creating a scale to measure the specific anxiety symptoms for COVID-19 in some of the studies should be highlighted.
Sample selection revealed an important risk of bias in the studies. In the study carried out in China more than 50% of the participants were from Wuhan, the epicenter of COVID-19[18].
Internet is a great source of health information and has the potential to influence its users. On the other hand, with the evolving literature, we have witnessed that the information found on the internet may not have the desired scientific rigor and many published scientific articles have been retracted due to fundamental scientific flaws. This implies great concern for scientific societies, governments, and users.
Our systematic review identifies certain areas where a strategic approach can make a difference in the psychological health of people at risk. There is an opportunity to develop and implement a gender-sensitive psychosocial protocol to reduce anxiety. In the times of pandemics, special support is needed to help people with mental disorders and prevent the deterioration of symptoms[27].
By identifying the populations and their sociodemographic variables (gender, housing, marital status, education) and comorbidities at greater risk for mental health in this pandemic (previous psychiatric illnesses), we found that it is necessary to recognize the repercussion degree and magnitude of this pandemic in people's lives, which significantly alters the psychodynamics of each one and social interactions.
The total lack of scientific knowledge about the behavior of COVID-19 in its preventive, epidemiological, clinical, and therapeutic aspects has generated fear in people regarding health care, being aggravated by the necessary social isolation, a positive measure to reduce contagion, but not for the mental health of the most vulnerable groups. Added to this, the economic uncertainty aroused a feeling of powerlessness to reverse the situation, further aggravating the levels of anxiety.
The psychological routine care services do not absorb the demand generated by a pandemic, requiring an investment by the state, and educational and research institutions, in actions that have the potential to act beneficially on the adverse effects, including late effects, of social isolation in people's lives, such as psychological support that strengthens self-confidence and trust in disease control measures (preventive, therapeutic, educational, and recreational). Besides, promote solidarity and economic support networks, for the less favored social classes, to minimize the effects of the pandemic on the economic health of the population.
We conclude that there is a potential relationship between social isolation during the COVID-19 pandemic and symptoms of anxiety. It is important to note that the direct and indirect costs of not identifying the detrimental effects of this phenomenon and neglecting strategies for intervention could lead to a significant psychological burden on society in several aspects after social isolation. This study represents a first approximation on this important theme, which needs to be revisited from future studies, considering longer reference periods.
The uncertainties about coronavirus disease 2019 (COVID-19), the change in routine, lifestyles and the reduction of physical contact can cause stress, anxiety, emotional overload, poor sleep and even physical health complications.
We are more than 1 year into the pandemic and more and more literature is evolving around the psychosocial effects of social isolation during this period. We were motivated to do a deep literature review of the scientific literature available and provide pragmatic insight to the problem.
Our objective was to evaluate the scientific publications available on the relationship between COVID-19 and anxiety experienced in the general population, during the period of social isolation, adopted by governmental organizations and public health policymakers as a measure to contain the spread of cases.
A literature search was performed systematically exploring the Pubmed and Medline databases using the following terms classified as MeSH descriptors: (“anxiety” AND “pandemic” AND “COVID-19”). For the search, in the Biblioteca Virtual em Saúde – BVS, Science.gov, Web of Science and National Library platforms, the following keywords were used: ("anxiety" AND "coronavirus" AND "social isolation"). Thirty-seven peer-reviewed articles were found. PRISMA and the Downs & Black checklist were used for qualitative evaluation.
The collated evidence demonstrated increased levels of symptoms of anxiety and depression during the period of social isolation. The population between the ages of 21 to 40 years was most affected. The risk of severe depression was twice as high at the epicenter of the pandemic. Sleep quality was significantly impaired. Questions about politics, religion, and consumption of products from China were found to generate fear and anticipate probable changes in the pattern of post-pandemic consumption. Social isolation exacerbated feelings of extreme hopelessness, sadness, loneliness and suicidal ideation.
We conclude that there is a potential relationship between social isolation during the COVID-19 pandemic and symptoms of anxiety. It is important to note that the direct and indirect costs of not identifying the detrimental effects of this phenomenon and neglecting strategies for intervention could lead to a significant psychological burden on society in several aspects after social isolation. This study represents a first approximation on this important theme, which needs to be revisited from future studies, considering longer reference periods.
Direction of the future research: We aim to maintain this as a live systematic review and provide timely updates on the evolving literature concerning to this very relevant issue.
We thank da Silva Dantas CG and Barbosa BER for their support with data collection.
Manuscript source: Invited manuscript
Specialty type: Public, environmental and occupational health
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Cardenas Suri H, He YF, Setiawati Y, Tumminello G S-Editor: Wu YXJ L-Editor: A P-Editor: Ma YJ
| 1. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17628] [Article Influence: 3525.6] [Reference Citation Analysis (0)] |
| 2. | Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8473] [Cited by in RCA: 7594] [Article Influence: 1518.8] [Reference Citation Analysis (0)] |
| 3. | Sahu KK, Mishra AK, Lal A. COVID-2019: update on epidemiology, disease spread and management. Monaldi Arch Chest Dis. 2020;90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 4. | Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2034] [Cited by in RCA: 1975] [Article Influence: 395.0] [Reference Citation Analysis (0)] |
| 5. | CDC COVID-19 Response Team. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 878] [Cited by in RCA: 1052] [Article Influence: 210.4] [Reference Citation Analysis (0)] |
| 6. | Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P, Mat Q, Huet K, Plzak J, Horoi M, Hans S, Rosaria Barillari M, Cammaroto G, Fakhry N, Martiny D, Ayad T, Jouffe L, Hopkins C, Saussez S; COVID-19 Task Force of YO-IFOS. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288:335-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 597] [Cited by in RCA: 530] [Article Influence: 106.0] [Reference Citation Analysis (0)] |
| 7. | Popov GT, Baymakova M, Vaseva V, Kundurzhiev T, Mutafchiyski V. Clinical Characteristics of Hospitalized Patients with COVID-19 in Sofia, Bulgaria. Vector Borne Zoonotic Dis. 2020;20:910-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Leichsenring F, Leweke F. Social Anxiety Disorder. N Engl J Med. 2017;376:2255-2264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 9. | Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020;383:510-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2488] [Cited by in RCA: 2407] [Article Influence: 481.4] [Reference Citation Analysis (0)] |
| 10. | Flink IL, Boersma K, Linton SJ. Pain catastrophizing as repetitive negative thinking: a development of the conceptualization. Cogn Behav Ther. 2013;42:215-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 11. | Galvão TF, Pansani TdSA, Harrad D. Principais itens para relatar Revisões sistemáticas e Meta-análises: A recomendação PRISMA. Epidemiologia e Serviços de Saúde. 2015;24:335-342. [RCA] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 189] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47102] [Article Influence: 2943.9] [Reference Citation Analysis (0)] |
| 13. | Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5177] [Cited by in RCA: 5929] [Article Influence: 219.6] [Reference Citation Analysis (0)] |
| 14. | Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66:504-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 854] [Cited by in RCA: 707] [Article Influence: 141.4] [Reference Citation Analysis (0)] |
| 15. | Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by vs People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Med Sci Monit. 2020;26:e924609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 463] [Cited by in RCA: 419] [Article Influence: 83.8] [Reference Citation Analysis (0)] |
| 16. | Lee SA. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44:393-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 850] [Cited by in RCA: 796] [Article Influence: 159.2] [Reference Citation Analysis (0)] |
| 17. | Yuan S, Liao Z, Huang H, Jiang B, Zhang X, Wang Y, Zhao M. Comparison of the Indicators of Psychological Stress in the Population of Hubei Province and Non-Endemic Provinces in China During Two Weeks During the Coronavirus Disease 2019 (COVID-19) Outbreak in February 2020. Med Sci Monit. 2020;26:e923767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 18. | Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J Psychiatr. 2020;51:102092. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 680] [Cited by in RCA: 666] [Article Influence: 133.2] [Reference Citation Analysis (0)] |
| 19. | Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. 2020;51:102076. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 397] [Cited by in RCA: 386] [Article Influence: 77.2] [Reference Citation Analysis (0)] |
| 20. | Xiao H, Zhang Y, Kong D, Li S, Yang N. Social Capital and Sleep Quality in Individuals Who Self-Isolated for 14 Days During the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 441] [Cited by in RCA: 494] [Article Influence: 98.8] [Reference Citation Analysis (0)] |
| 21. | Kerstner T, Witthöft M, Mier D, Diener C, Rist F, Bailer J. A diary-based modification of symptom attributions in pathological health anxiety: effects on symptom report and cognitive biases. J Consult Clin Psychol. 2015;83:578-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J Psychiatr. 2020;51:102111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 139] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 23. | Robb CE, de Jager CA, Ahmadi-Abhari S, Giannakopoulou P, Udeh-Momoh C, McKeand J, Price G, Car J, Majeed A, Ward H, Middleton L. Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Front Psychiatry. 2020;11:591120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 261] [Cited by in RCA: 224] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 24. | Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 655] [Cited by in RCA: 625] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 25. | Somi SA, Dutta P, Tamanna KN, Hussain H, Hasan R, Ghose M, Tanni NU, Parhin A, Moosa SA, Sakibuzzaman M. COVID-19: Embracing Mental Health Upshot from the Coronavirus Pandemic Crisis. J Psychiatr Psychiatric Disord. 2020;4:328-342. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Han RH, Schmidt MN, Waits WM, Bell AKC, Miller TL. Planning for Mental Health Needs During COVID-19. Curr Psychiatry Rep. 2020;22:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | Quittkat HL, Düsing R, Holtmann FJ, Buhlmann U, Svaldi J, Vocks S. Perceived Impact of Covid-19 Across Different Mental Disorders: A Study on Disorder-Specific Symptoms, Psychosocial Stress and Behavior. Front Psychol. 2020;11:586246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 28. | Hernández-García I, Giménez-Júlvez T. Assessment of Health Information About COVID-19 Prevention on the Internet: Infodemiological Study. JMIR Public Health Surveill. 2020;6:e18717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 29. | Z. Cross-country differences in anxiety and behavioral response to the Covid-19 pandemic. Eur Soc. 2020;1-31. [DOI] [Full Text] |
| 30. | Lal A, Sanaullah A, M Saleem MK, Ahmed N, Maqsood A. Psychological Distress among Adults in Home Confinement in the Midst of COVID-19 Outbreak. Eur J Dent. 2020;14:S27-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |