Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7110
Peer-review started: December 21, 2020
First decision: May 5, 2021
Revised: May 25, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: August 26, 2021
Processing time: 245 Days and 22.6 Hours
Extramedullary plasmacytoma (EMP), a variant form of myeloma, is a rare solid plasma cell tumor that originates from the bone marrow hematopoietic tissue and accounts for about 3% of all plasma cell tumors. EMP can affect various tissues and organs, about 90% of which is found in the head and neck. However, EMP in the reproductive organs is rare, and is difficult to be distinguished from other primary or metastatic genital tumors according to clinical symptoms and imaging findings.
Herein, we report a case with coexistence of EMP and squamous cell carcinoma in the cervix. The first histopathological report of neoplasms on the surface of the cervix and vagina showed an EMP. Both ultrasound and pelvic enhanced magnetic resonance imaging (MRI) indicated that there was a tumor in the cervix. Thus, another cervical biopsy and pathological examination were performed, which indicated EMP combined with squamous cell carcinoma. Then, the patient underwent extensive total hysterectomy (type C1) + systemic lymph node dissection and received 25 external pelvic irradiations with a dose of 50 Gy following surgery. During 2-year follow-up, no recurrence was reported.
In conclusion, EMP involving the reproductive system is relatively rare. In this case, MRI, B-ultrasound, and cervical canal scraping were used to further determine the diagnosis of EMP combined with squamous cell carcinoma. The patient had improved prognosis after appropriate treatments.
Core Tip: Extramedullary plasmacytoma (EMP) is a plasma cell tumor that occurs outside the bone marrow. EMP in the reproductive organs is rare, and is difficult to distinguish from other primary or metastatic genital tumors or is easily missed. Herein, we describe a case with coexistence of EMP and squamous cell carcinoma in the cervix. Magnetic resonance imaging (MRI), B-ultrasound, and cervical canal scraping were used to further determine the diagnosis of EMP combined with squamous cell carcinoma. The patient had improved prognosis after appropriate treatments. This report suggests that screening with vaginal ultrasound and enhanced MRI can help to avoid misdiagnosis.
- Citation: Zhang QY, Li TC, Lin J, He LL, Liu XY. Coexistence of cervical extramedullary plasmacytoma and squamous cell carcinoma: A case report. World J Clin Cases 2021; 9(24): 7110-7116
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7110.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7110
Extramedullary plasmacytoma (EMP) is a plasma cell tumor that occurs outside the bone marrow. It is a solid plasma cell tumor that originates from the bone marrow hematopoietic tissue and accounts for about 3% of plasma cell tumors. It is clinically rare. Approximately 90% of EMP occurs in the head and neck, but EMP in the reproductive organs is rare. EMP combined with cervical squamous cell carcinoma has not been reported. EMP combined with cervical squamous cell carcinoma is difficult to be distinguished from metastatic genital tumors and thus is easy to misdiagnose. Herein, we describe a case with coexistence of EMP and squamous cell carcinoma in the cervix.
A 77-year-old female, gravida 3, para 3, was admitted with vaginal bleeding over a 7 d period.
The vaginal bleeding lasted for more than 1 wk.
No special personal and family history.
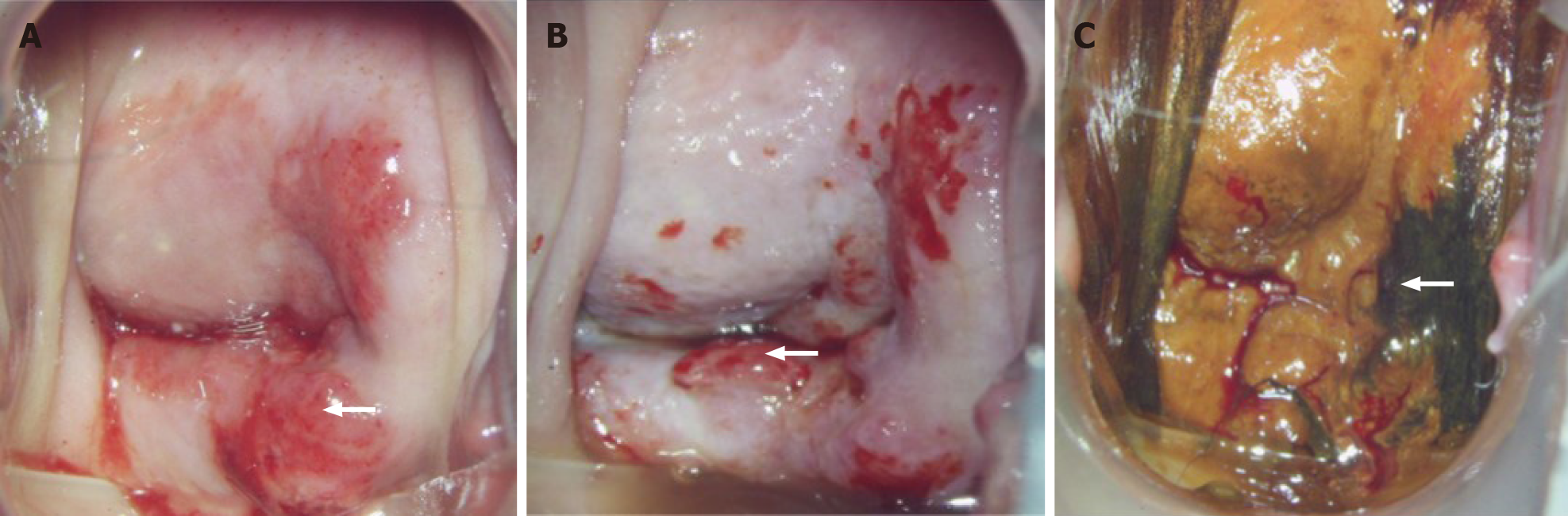
Gynecological examination showed granular protrusions with red color and hard texture on 2/3 of the surface of the cervix and vaginal wall, and cervix atrophy. The cervical lesions under colposcopy are shown in Figure 1A. The lesions on the cervical surface and vaginal wall were positive for visual inspection with acetic acid (Figure 1B) and negative for cervical iodine staining (Figure 1C).
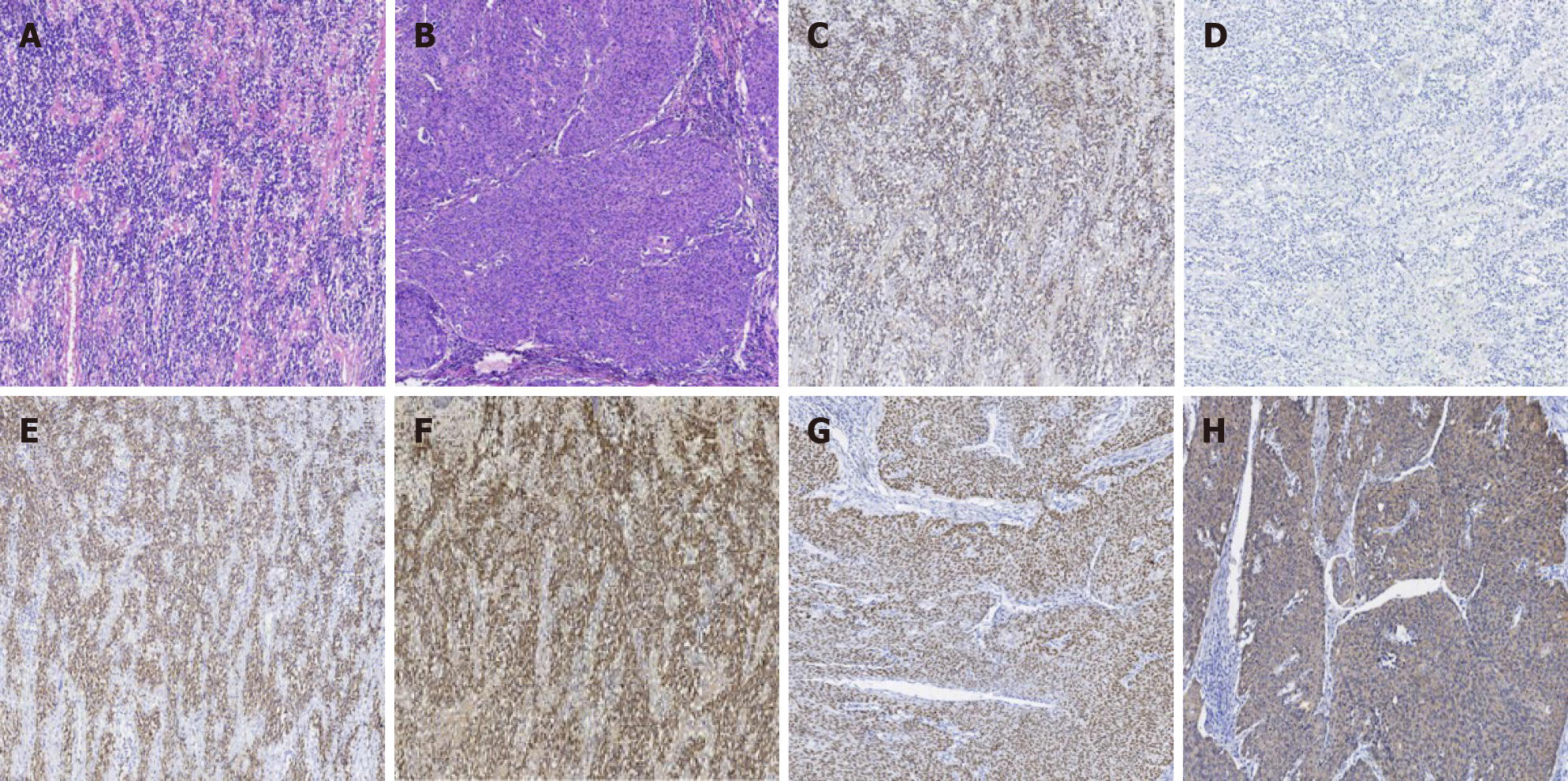
Hematoxylin-eosin (HE) staining of EMP showed that the tumor cells were diffusely distributed and pathological spindle division and Russell body were observed (Figure 2A). HE staining of cervical squamous cell carcinoma showed hyperplasia of epithelioid cell nests, infiltrating growth pathological fission, and intercellular Bridges (Figure 2B). Immunohistochemistry staining results: Kappa diffusely positive (Figure 2C), Lambda diffusely negative (Figure 2D), CD38 diffusely positive (Figure 2E), CD138 diffusely positive (Figure 2F), p40 diffusely positive (Figure 2G), and, CK5/6 diffusely positive (Figure 2H).
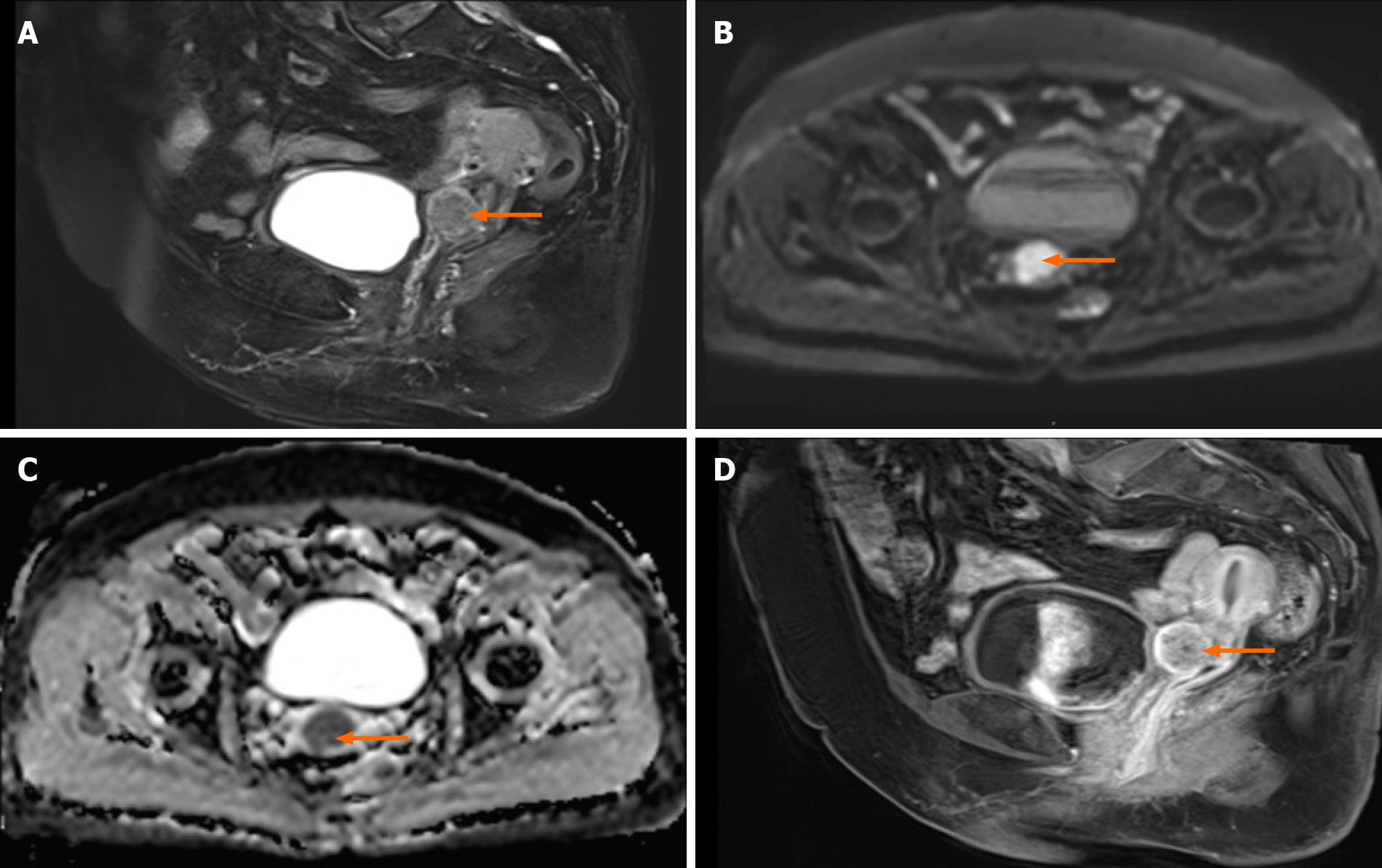
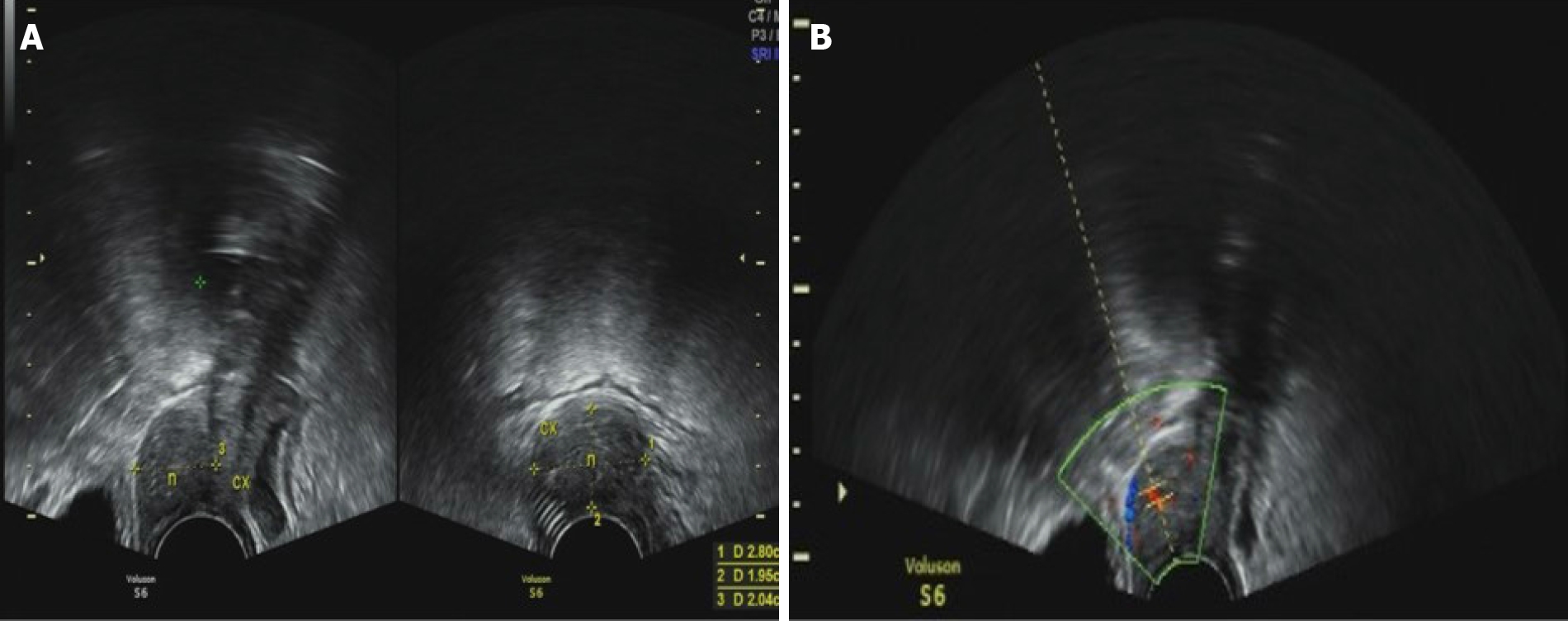
Pelvic enhanced magnetic resonance imaging (MRI) showed a 3 cm diameter quasi-circular high T2WI signals in the anterior lip of the cervix and the anterior wall of the cervix, with limited diffusion and an apparent diffusion coefficient (ADC) value of 0.838 × 10-3 mm2/s, with a markedly enhanced edges during enhanced phrase (Figure 3A-D). Vaginal ultrasound showed obviously thickened anterior cervix, and a 3 cm diameter solid hypoechoic nodule with a poorly defined boundary and a dotted blood flow signal (Figure 4A and B).
Finally, the diagnosis of EMP combined with squamous cell carcinoma was made.
The patient underwent extensive total hysterectomy (type C1) + systemic lymph node dissection and received external pelvic irradiations with a dose of 50 Gy at 2 wk after surgery. The radiotherapy was completed within 8 wk.
The patient recovered well after the operation and radiotherapy. After radiotherapy, the patient was followed-up every 3 mo. Gynecological examinations, including pelvic and abdominal ultrasound, squamous cell carcinoma antigen detection, and vaginal stump exfoliated cytology, were performed each time. Whole abdomen CT was performed at a 6 mo interval. During 2-year follow-up, no recurrence was found. The patient is under constant follow-up.
Plasma cell tumors result from abnormal proliferation of the plasma cell system. The most common plasma cell tumors are intramedullary lesions, namely multiple myeloma and solitary myeloma, followed by extramedullary manifestations, namely EMP, which accounts for about 3% of systemic plasma cell tumors[1]. EMP can affect various tissues and organs, and about 90% occurs in the head and neck, such as the nasal cavity, sinuses, tonsil fossa, and oral cavity. It can also occur in the upper and lower respiratory tract, gastrointestinal tract, central nervous system, conjunctiva, thyroid, breast, mediastinum, broad ligament, bladder, testis, lymph nodes and other organs[1-4]. Until now, there was no report focusing on coexistence of EMP and cervical squamous cell carcinoma in the genitals. EMP is more common in males, and can occur at any age, most often between 50-years-old and 70-years-old[5]. The diagnostic criteria of EMP include: (1) Pathologically confirmed primary plasma cell tumor outside the bone marrow; (2) Normal bone marrow; (3) No multiple myeloma related clinical manifestations and relevant laboratory test positive indicators; and (4) No M protein or a small amount of M protein detected[6,7]. The pathology of this case showed primary EMP in genital tract, with a normal bone marrow. Moreover, the whole body bone scan excluded multiple myeloma, and no M protein was detected. Therefore, the diagnosis of EMP in this case was clear. The etiology of EMP is not yet fully understood, but it has been found that chronic irritation caused by inhalation of certain irritants or viral diseases may be related to development of EMP[8]. In this case, EMP may be related to the HPV virus infection, which is also the cause of cervical squamous cell carcinoma. However, this hypothesis is needed to be confirmed by more cases of EMP.
The nature of EMP is currently controversial. Some scholars believed that EMP was a benign tumor but has a tendency to become malignant, and some showed that EMP was a borderline tumor can develop into multiple myeloma[9]. However, most scholars currently believe that EMP should be regarded as malignant due to local infiltration and tendency of metastasis[3]. The primary site of EMP metastasis is regional lymph nodes, accounting for about 30%[10]. Sasitharan[11] divided EMP into three stages: Stage I, the tumor was confined to the extramedullary primary tumor; Stage II, the tumor had regional lymph node metastasis; Stage III, there were multiple metastases. The EMP in this case was limited to the reproductive tract, and no lymphatic and multiple metastases were found. Thus, the staging should be stage I.
The incidence of EMP is low. In this case, cervical lesions were found by ultrasound and MRI. The early imaging findings of EMP had a low specificity, which should be furtherly confirmed by biopsy. Vaginal ultrasound diagnosis of cervical cancer is not only simple, fast, non-invasive and economical, but also can fully reflect the blood flow of cervical tumor and the distribution of blood vessels in the tumor[12]. In this case, the vaginal B-ultrasonography found a local cervical lesion with blood flow signal. Therefore, the vaginal B-ultrasonography has a certain value on the early cervical cancer screening. MRI characterized by multi-level, multi-directional, multi-sequence imaging, with strong tissue resolution can be used for imaging staging of cervical cancer[13]. In this case, the MRI of the cervix showed a 3 cm diameter quasi-circular high T2WI signals in the anterior lip of the cervix and the anterior wall of the cervix, with limited diffusion and an ADC value of 0.838 × 10-3 mm2/s, with a markedly enhanced edges during enhanced phrase. In DWI, the ADC is usually used to describe the diffusion speed of water molecules in the tissue. In this case, ADC was reduced and DWI showed high signal. The T2WI sagittal scan showed slightly high signal, which was consistent with the MRI manifestations of cervical cancer.
The results of immunohistochemical examination are an important basis for the diagnosis of EMP. EMP immunohistochemistry: LCA(+), CD79α(+), CD38(+), CD138(+), κ(+) and λ(+)[14]. The immunohistochemistry results of this case was basically consistent with the that of EMP [except λ(-)]. The expression of κ or λ light chain is an important indicator for evaluating monoclonal plasma cells[15]. In this case, the plasma cell κ light chain was positive and λ light chain was negative, which supports the diagnosis of monoclonal plasma cells.
According to FIGO 2018 cervical cancer staging, the lesion in this case was stage IB2 cervical cancer and the treatment should be type C extensive total hysterectomy combing with radiotherapy or chemotherapy. The main treatments of EMP are surgery and/or radiotherapy. According to Sasitharan's statistics, the local recurrence rate of EMP after surgery alone is 39%, the local recurrence rate after radiotherapy alone is 31%, and the local recurrence rate after surgery plus radiotherapy is 22%[11]. Therefore, surgery plus radiotherapy has the best effect. Early detection, complete resection as much as possible and adjuvant radiotherapy are curial for prompting prognosis of EMP. In this case, type C extensive hysterectomy plus radiotherapy was performed. There was no recurrence until last following-up.
In conclusion, EMP of the genital tract is rare and its etiology is not clear. In this case, the rare EMP was combined with cervical cancer, a common cancer, the diagnosis of which is easily missed. When rare cases are identified, further examinations are needed to rule out common diseases. The screening with vaginal ultrasound and enhanced MRI can help to avoid missed diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Morilla I S-Editor: Gao CC L-Editor: Filipodia P-Editor: Liu JH
| 1. | Liu T. Diagnostic pathology of Liu Tonghua. Beijing: People's Medical Publishing House, 2019. |
| 2. | Kitamura F, Doi K, Ishiodori H, Ohchi T, Baba H. Primary extramedullary plasmacytoma of the sigmoid colon with perforation: a case report. Surg Case Rep. 2018;4:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Jizzini MN, Shah M, Yeung SJ. Extramedullary Plasmacytoma Involving the Trachea: A Case Report and Literature Review. J Emerg Med. 2019;57:e65-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Csomor J, Bunganič B, Dvořáková D, Hříbek P, Kmochová K, Campr V, Tučková I, Šálek C, Urbánek P, Zavoral M. Extramedullary Plasmacytoma of the Pancreas Complicated with Left-Sided Portal Hypertension-a Case Report and Literature Review. J Gastrointest Cancer. 2019;50:962-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Yamaguchi O, Kaira K, Nakamura Y, Kagamu H. Unexpected response of extramedullary plasmacytoma in patients with lung cancer who received nivolumab. Ann Hematol. 2019;98:2851-2852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Caers J, Paiva B, Zamagni E, Leleu X, Bladé J, Kristinsson SY, Touzeau C, Abildgaard N, Terpos E, Heusschen R, Ocio E, Delforge M, Sezer O, Beksac M, Ludwig H, Merlini G, Moreau P, Zweegman S, Engelhardt M, Rosiñol L. Diagnosis, treatment, and response assessment in solitary plasmacytoma: updated recommendations from a European Expert Panel. J Hematol Oncol. 2018;11:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 185] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 7. | Zhong YP, Chen SL, Li X, Hu Y, Zhang JJ, An N. [Multiple myeloma complicated with spinal infiltration]. Zhongguo Shiyan Xueye Xue Zazhi. 2010;18:466-468. [PubMed] |
| 8. | Tsang RW, Campbell BA, Goda JS, Kelsey CR, Kirova YM, Parikh RR, Ng AK, Ricardi U, Suh CO, Mauch PM, Specht L, Yahalom J. Radiation Therapy for Solitary Plasmacytoma and Multiple Myeloma: Guidelines From the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2018;101:794-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 131] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 9. | Wang J, Li J, Zhang F, Zhang P. Retroperitoneal extramedullary plasmacytoma: A case report and review of the literature. Medicine (Baltimore). 2018;97:e13281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Katayama Y, Kaneko M, Tamano M. Extramedullary Plasmacytoma of the Stomach. Clin Gastroenterol Hepatol. 2020;18:e91-e92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Ge S, Tan Z, Xie D, Yi Y. [Clinical analysis on extramedullary plasmacytoma in the upper airway]. Linchung Er Bi Yan Hou Tou Jing Waike Zazhi. 2013;27:227-230. [PubMed] |
| 12. | Hu X, Peng C, Wang P, Cai J. Extramedullary Plasmacytoma of Nasal Cavity: A Case Report and Literature Review. Ear Nose Throat J. 2020;145561320960005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Goldberg Y, Siegler Y, Segev Y, Mandel R, Siegler E, Auslander R, Lavie O. The added benefit of transvaginal sonography in the clinical staging of cervical carcinoma. Acta Obstet Gynecol Scand. 2020;99:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Bae JM, Kim CK, Park JJ, Park BK. Can diffusion-weighted magnetic resonance imaging predict tumor recurrence of uterine cervical cancer after concurrent chemoradiotherapy? Abdom Radiol (NY). 2016;41:1604-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Ge X, Chen P, Zhang X, Zhang H, Zhang Y, Fan Y, Wang Q, Fu J, Li B. [Extramedullary plasmacytoma presented with multiple pulmonary plasmacytoma as first manifestation: a case report and literature review]. Zhonghua Xueye Xue Zazhi. 2015;36:956-959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |