Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6950
Peer-review started: May 9, 2021
First decision: June 5, 2021
Revised: June 6, 2021
Accepted: June 22, 2021
Article in press: June 22, 2021
Published online: August 16, 2021
Processing time: 88 Days and 8.1 Hours
Heterotopic pregnancy (HP) refers to the coexistence of ectopic pregnancy and intrauterine pregnancy. Salpingectomy is proposed as a pretreatment before in vitro fertilization and embryo transfer (IVF-ET) to reduce the risk of HP. HP after IVF-ET occurs in women who had already underwent bilateral salpingectomy, even though it is extremely rare.
A case of a 29-year-old woman with recurrent interstitial HP after IVF-ET following salpingectomy is presented. The main symptom was a sudden and worsening pelvic pain. Physical examinations revealed signs of peritoneal bleeding and irritation with stable vital signs. Transvaginal ultrasound showed a live intrauterine pregnancy and another live embryo with cardiac activity in the left cornu extending beyond the lateral edge of the uterus. Her hemoglobin concentration was 8.0 g/dL, and serum human chorionic gonadotropin value was 171116.9 mIU/mL. With the diagnosis of ruptured HP with internal bleeding, an emergency laparoscopic resection of left cornu was performed. The interstitial pregnancy was removed with caution to protect the intrauterine pregnancy. After the surgical treatment, the intrauterine pregnancy continued with no complications. A healthy baby was delivered by caesarean section at 39 wk. Outcomes of another three cases are further summarized.
Post-salpingectomy HP is a rare but challenging condition. Surgical treatment is preferred in the case with a viable intrauterine pregnancy.
Core Tip: Our paper presented a rare case of a 29-year-old woman with recurrent interstitial heterotopic pregnancy (HP) after in vitro fertilization-embryo transfer following bilateral salpingectomy. We also summarized the outcomes of another three similar cases successfully treated in our department. Furthermore, we reviewed characteristics and outcomes of other reported post-salpingectomy HP cases. Interstitial HP after bilateral salpingectomy is extremely rare and has a high risk of rupture and hemorrhage.
- Citation: Wang Q, Pan XL, Qi XR. Post-salpingectomy interstitial heterotopic pregnancy after in vitro fertilization and embryo transfer: A case report. World J Clin Cases 2021; 9(23): 6950-6955
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6950.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6950
Heterotopic pregnancy (HP) refers to the coexistence of ectopic pregnancy (EP) and intrauterine pregnancy and has a very low incidence ,occurring 1 in 30000 spontaneous pregnancies[1]. Due to the widespread use of assisted reproductive techniques, HP after in vitro fertilization and embryo transfer (IVF-ET) has been frequently reported[2]. Salpingectomy has been proposed as a pretreatment before IVF-ET to reduce the risk of HP. Theoretically, the whole visible part of the fallopian tube is removed by salpingectomy, which could prevent EP after IVF-ET. However, HP after IVF-ET even occurs in women who had already underwent bilateral salpingectomy.
Post-salpingectomy HP is an extremely rare but challenging condition, since the ectopic pregnancy must be removed whilst preserving the normal intrauterine pregnancy. Since the interstitial portion is rich in blood supply, it makes the post-salpingectomy interstitial HP an extremely dangerous complication with risks of sudden rupture and severe hemorrhage. Thus, for patients after tubal sterilization, the possibility of HP should not be neglected even with the presence of live intrauterine pregnancies. Previously reported post-salpingectomy HP cases have been reviewed[1-9]. Four of these cases were diagnosed as interstitial HPs (with three ruptured cases), only one of which reported a live birth of the intrauterine pregnancy after treatment. The other three cases experienced abortions.
Here, we report a case of recurrent and ruptured interstitial HP after IVF-ET following bilateral salpingectomy. We further summarize the outcomes and delivery modes of another three similar cases who were treated successfully in our department in the past 5 years.
A 29-year-old woman presented to our department complaining of worsening pain in the lower left abdominal quadrant. Her last menstrual cycle was 7 wk and 1 d previous.
The pain had started a day before her admission and had been worsened in the last 4 h. An IVF cycle was performed with two frozen embryos transferred 5 wk ago. There were no additional symptoms.
The patient had an obstetric history of gravida 4, para 0-0-3-0. Two years after her first spontaneous abortion, she twice underwent diagnostic hysteroscopy combined with laparoscopy for secondary infertility. Then, she had a history of HP with failing intrauterine pregnancy after ovulation induction treatment. Laparoscopic bilateral salpingectomy and dilation and curettage were performed. After sterilization, she experienced two unsuccessful IVF cycles.
There is no personal and family history.
The patient’s temperature was 36.5 °C, heart rate was 95 bpm, respiratory rate was 20 breaths per min, blood pressure was 102/67 mmHg, and oxygen saturation was 98%. The general appearance was acute distress. The gynecologic examination revealed bulky uterus and tenderness in the left adnexal area, which showed signs of peritoneal bleeding and irritation but with stable vital signs.
Blood analysis revealed an erythropenia (2.58 × 1012/L) and a hemoglobin concentration of 8.0 g/dL with normal leukocyte count and platelet count. Prothrombin and partial thromboplastin times were normal. Serum human chorionic gonadotropin value was 171116.9 mIU/mL. The blood biochemistries and urine analysis were normal.
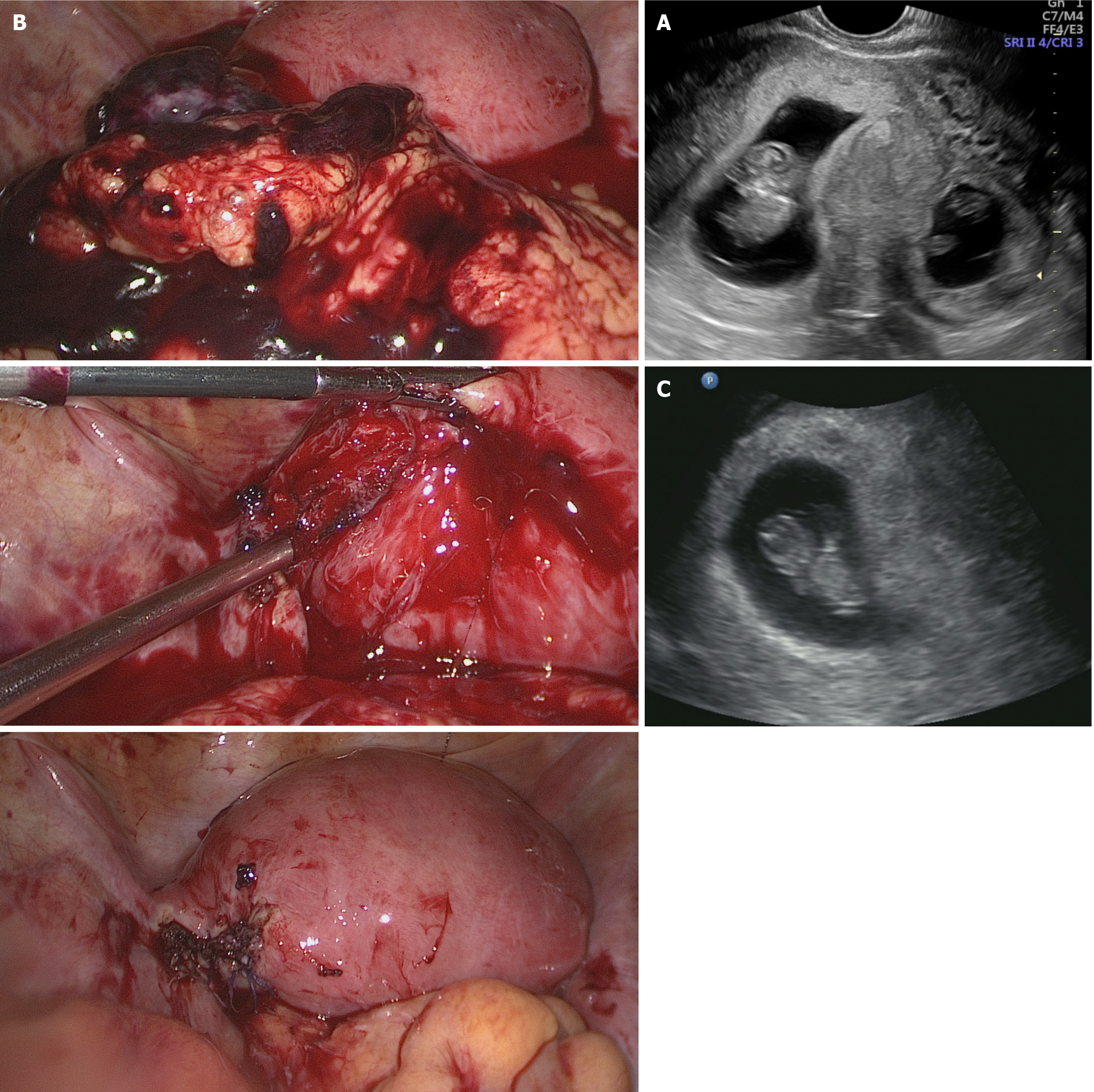
Transvaginal ultrasound showed a live intrauterine pregnancy and another live embryo with cardiac activity in the left cornu extending beyond the lateral edge of the uterus. In addition, free fluid was noted in the cul-de-sac as well as in the abdomen.
The final diagnosis of the presented case is ruptured HP with internal bleeding after IVF-ET.
An emergency laparoscopy was performed after discussion with the patient. After suction of blood clots and hemoperitoneum (about 700 mL), a ruptured interstitial pregnancy within the left salpingectomy site (lateral to the insertion of the left round ligament and not connected with uterine cavity) was confirmed (Figure 1). We performed a left cornual resection to remove the interstitial pregnancy, with caution to protect the intrauterine pregnancy.
The pathological report confirmed the presence of trophoblastic tissue in interstitial and intramural portion. The patient’s post-operative course was uneventful. The synchronous intrauterine pregnancy continued with no complications and with appropriate growth of the fetus. A healthy baby was delivered by caesarean section at 39 wk, weighing 3110 g.
We further retrospectively studied cases of post-IVF interstitial HP following bilateral salpingectomy in our department over the past 5 years. The characteristics and outcomes of these 4 cases are listed in Table 1. All of them were treated by laparoscopic excision of the intramural and cornual segment and had very good outcomes for the intrauterine pregnancies.
| No. | Age, yr | Year | Gravida/Para | EP | History of sterilization | GA | Transferred embryos | Main symptom | Ultrasound manifestation | Ectopic site | Bleeding volume | Outcome of intrauterine pregnancy |
| 1 | 29 | 2019 | G4/P0030 | 1 | Bilateral salpingectomy for HP in 2018 | 50 d | 2 frozen embryos | Abdominal pain | IVE + ECM + PF | Left IP (ruptured) | 700 mL | Full-term CS (selective) |
| 2 | 32 | 2019 | G4/P0030 | 2 | Left salpingectomy for EP in 2013 and right salpingectomy for EP in 2015 | 66 d | 2 fresh embryos | Abdominal pain | IVE + EVE | Left IP | 300 mL | Premature CS at 34 wk (fetal distress) |
| 3 | 36 | 2018 | G4/P1021 | 1 | Right salpingectomy and left tubal ligation for EP in 2015 | 38 d | 2 frozen embryos | Abdominal pain | IVE + ECM + PF | Right IP (ruptured) | 1000 mL | Full-term CS (breech position) |
| 4 | 30 | 2016 | G5/P0040 | 3 | Left salpingectomy for EP in 2007 and right salpingectomy for EP in 2014 | 49 d | 2 fresh embryos | None | IVE + EVE | Left IP | 50 mL | Full-term CS (selective) |
As described above, salpingectomy or tube ligation is used to eliminate the risk of HP and improve outcomes of IVF-ET. The mechanism of HP following bilateral salpingectomy is unclear. The remaining interstitial portion of fallopian tube and the formation of a cornual sinus after laparoscopic salpingectomy might be the causative risk factors. Thus, it is important to perform an appropriate laparoscopic sterilization by minimizing tubal residue. Some studies further suggested cornual suture at the time of salpingectomy to help reduce these risks[10].
HP can be treated by expectancy, medical or surgical treatment. If the intrauterine pregnancy is viable, surgical excision of the ectopic pregnancy is a better option. The intrauterine gestations in HP were more likely to end in spontaneous or induced abortion compared with the outcomes of normal intrauterine pregnancies. The rate of live birth after treatment was even lower. Thus, patients could be treated immediately and appropriately to increase the survival rate of the intrauterine pregnancy. In the case of a non-viable intrauterine pregnancy, conservative treatment should be considered if the patient is in stable condition without rupture. The treatment should be personalized.
Previously reported post-salpingectomy interstitial HP cases revealed a high rate of abortion. In the past 5 years, 4 cases of post-sterilization interstitial HP after IVF-ET were successfully treated by laparoscopic resection of the ectopic tissue and ipsilateral cornu in our department. Each of them had an ongoing healthy gestation culminating in a caesarean section with a live birth.
Post-salpingectomy interstitial HP should be considered as a separate diagnosis after IVF-ET. Timely diagnosis and immediate treatment are essential to achieve better clinical outcomes. In our experience, laparoscopy is the minimally invasive way to remove the ectopic tissue and preserve the viable intrauterine pregnancy with a very high success rate. Caesarean section is the preferred method of delivery considering the risk of metrorrhexis.
The authors would like to thank Institutional Review Board of Ethics Committee of West China Second Hospital for approving this case report for publication.
Manuscript source: Unsolicited manuscript
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Velikova TV S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Kasum M, Grizelj V, Simunic V. Combined interstitial and intrauterine pregnancies after in-vitro fertilization and embryo transfer. Hum Reprod. 1998;13:1547-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Dumesic DA, Damario MA, Session DR. Interstitial heterotopic pregnancy in a woman conceiving by in vitro fertilization after bilateral salpingectomy. Mayo Clin Proc. 2001;76:90-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Cormio G, Santamato S, Putignano G, Bettocchi S, Pascazio F. Concomitant abdominal and intrauterine pregnancy after in vitro fertilization in a woman with bilateral salpingectomy. A case report. J Reprod Med. 2003;48:747-749. [PubMed] |
| 4. | Chang Y, Lee JN, Yang CH, Hsu SC, Tsai EM. An unexpected quadruplet heterotopic pregnancy after bilateral salpingectomy and replacement of three embryos. Fertil Steril. 2003;80:218-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Ben-Ami I, Panski M, Ushakov F, Vaknin Z, Herman A, Raziel A. Recurrent heterotopic pregnancy after bilateral salpingectomy in an IVF patient: case report. J Assist Reprod Genet. 2006;23:333-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Zhaoxia L, Honglang Q, Danqing C. Ruptured heterotopic pregnancy after assisted reproduction in a patient who underwent bilateral salpingectomy. J Obstet Gynaecol. 2013;33:209-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Shavit T, Paz-Shalom E, Lachman E, Fainaru O, Ellenbogen A. Unusual case of recurrent heterotopic pregnancy after bilateral salpingectomy and literature review. Reprod Biomed Online. 2013;26:59-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Oral S, Akpak YK, Karaca N, Babacan A, Savan K. Cornual heterotopic pregnancy after bilateral salpingectomy and uterine septum resection resulting in term delivery of a healthy infant. Case Rep Obstet Gynecol. 2014;2014:157030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Seshadri S, Shirley P, Jaiganesh T, Uchil D, Jolaoso A. In vitro fertilisation and embryo transfer for bilateral salpingectomies results in a ruptured ovarian ectopic pregnancy due to a tubal stump fistula: a case report and review of the literature. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Chen J, Huang D, Shi L, Zhang L, Sun D, Lin X, Zhang S. Cornual Suture at the Time of Laparoscopic Salpingectomy Reduces the Incidence of Interstitial Pregnancy after In Vitro Fertilization. J Minim Invasive Gynecol. 2018;25:1080-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |