Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6824
Peer-review started: January 31, 2021
First decision: March 11, 2021
Revised: March 31, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: August 16, 2021
Processing time: 186 Days and 1.7 Hours
Nocardiosis is an uncommon infection that usually occurs in immunocompromised patients, and the pulmonary system is the most common site. We report an uncommon case of nocardiosis with diffuse involvement of the pleura, which presented as multiple localized nodular or hillock lesions on computed tomography (CT) with local chest wall infiltration.
A 54-year-old woman was referred to our hospital due to cough and fever for 20 d. She had a history of nephrotic syndrome for 7 mo and was given prednisone (60 mg/d) 6 mo previously. The hormone was then gradually reduced to the current dose of 25 mg/d. Chest CT showed many nodular or hillock lesions in the right pleura, mediastinum, and interlobar fissure areas. On the lower layer, one lesion infiltrated the chest wall. She was treated with piperacillin sodium and sulbactam sodium, but the therapeutic effect was not good. In this regard, ultrasound-guided local infiltration anesthesia was further conducted for perihepatic hydrops drainage to improve diagnostic accuracy. Puncture fluid culture isolated Nocardia species, confirming the diagnosis of nocardiosis. Subtype Nocardia farcinica was identified by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Antibiotic treatment was switched to trimethoprim/sulfamethoxazole and imipenem. After 8 d of treatment, the patient was discharged from the hospital with improved condition, and she has been recurrence-free for 2 years.
This report illustrates that nocardiosis should be suspected when clinicians encounter patients who are immunocompromised and have diffuse involvement of the pleura.
Core Tip: Nocardiosis is an uncommon subacute or chronic suppurative infection that usually occurs in immunocompromised patients. The pathological manifestations of nocardiosis are usually granulomas or abscesses. This case of nocardiosis exhibited diffuse involvement of the pleura and presented as multiple localized nodular or hillock shadows in the pleura, mediastinum, and interlobar fissure areas on computed tomography, which differs from simple pleural effusion or general bacterial infection.
- Citation: Wang P, Yi ML, Zhang CZ. Nocardiosis with diffuse involvement of the pleura: A case report. World J Clin Cases 2021; 9(23): 6824-6831
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6824.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6824
Nocardia species, which belong to Actinomycetes, are ubiquitous in the environment, especially in soil and water[1,2]. Nocardiosis usually occurs in the pulmonary system most commonly through direct inhalation of Nocardia[1,3]. An accurate diagnosis of nocardiosis is essential for determining the appropriate treatment, but it is often misdiagnosed as other infections or malignancy. Only a few studies have described the computed tomography (CT) findings of pulmonary nocardiosis; the most common CT finding is pulmonary manifestations[4-6]. This report describes an uncommon case of nocardiosis with diffuse involvement of the pleura.
A 54-year-old woman was referred to our hospital due to cough and fever.
The patient developed cough and fever 20 d ago after catching a cold. The cough was paroxysmal with white sticky sputum. Her body temperature ranged from 38°C to 39°C.
She had a history of nephrotic syndrome for 7 mo and was given prednisone (60 mg/d) 6 mo previously. The hormone was then gradually reduced to the current dose of 25 mg/d. The patient was a farmer, but she did not work after she became sick. She had no special contact history, such as going into the greenhouse, dust exposure, or pet breeding.
The patient denied any family history.
On admission, her temperature was 38.3°C, respiratory rate was 23 breaths/min, heart rate was 114 bpm, and blood pressure was 90/69 mmHg. Breath sounds in both lungs were rough, and moist rales were heard.
Laboratory data revealed the following values: white blood cell count, 12.58 × 109/L; hemoglobin, 102 g/L; platelets, 118 × 109/L; C-reactive protein, 240 mg/L; and procalcitonin, 2.93 ng/mL.
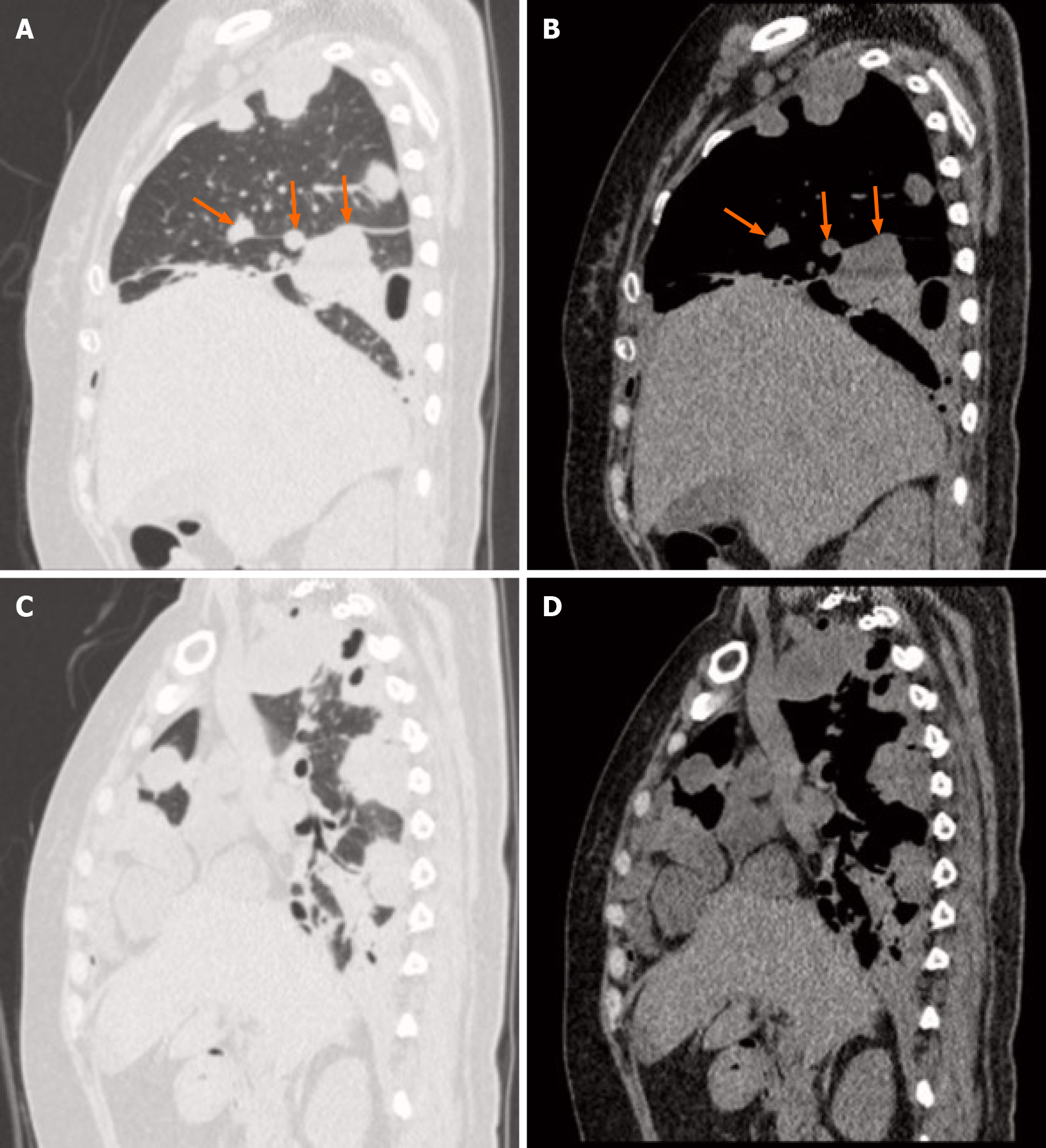
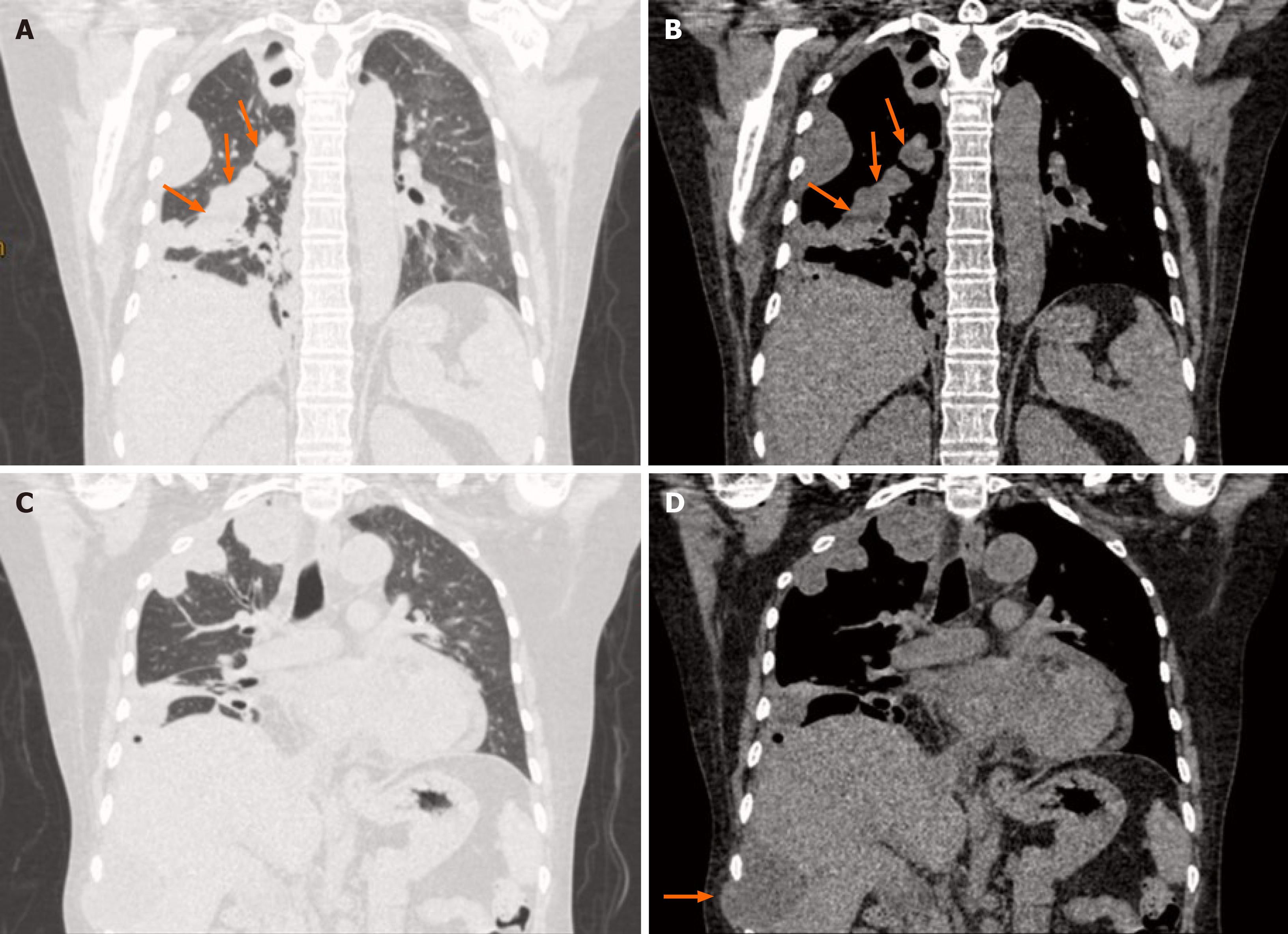
Chest CT showed many nodular or hillock lesions in the right pleura, mediastinum, and interlobar fissure areas (Figures 1-3). Most of the lesions showed low density, and some showed soft-tissue density at the peripheral areas with low density in the center and had cavitary appearance. The edge of the lesion was clear, and the right lung was compressed with volume reduction and partial atelectasis. On the lower layer, one lesion infiltrated the chest wall, and the adjacent liver was compressed (Figure 3D). Right pleural effusion and pericardial effusion were also observed.
She was treated with piperacillin sodium and sulbactam sodium, but her temperature still fluctuated. Her inflammatory markers were still elevated, and follow-up chest CT scan showed no improvement. In this regard, ultrasound-guided local infiltration anesthesia was further conducted for perihepatic hydrops drainage to improve diagnostic accuracy.
The puncture fluid was thick pus. Gram staining of the puncture fluid depicted Gram-positive bacteria with branching filaments (Figure 4A), and the bacteria were positive for weak acid-fast staining (Figure 4B). The tentative diagnosis of nocardiosis was made. Puncture fluid culture isolated Nocardia species, confirming the diagnosis of nocardiosis. Subtype Nocardia farcinica was identified by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry.
The final diagnosis of the presented case was nocardiosis.
Antibiotic treatment was switched to trimethoprim/sulfamethoxazole and imipenem.
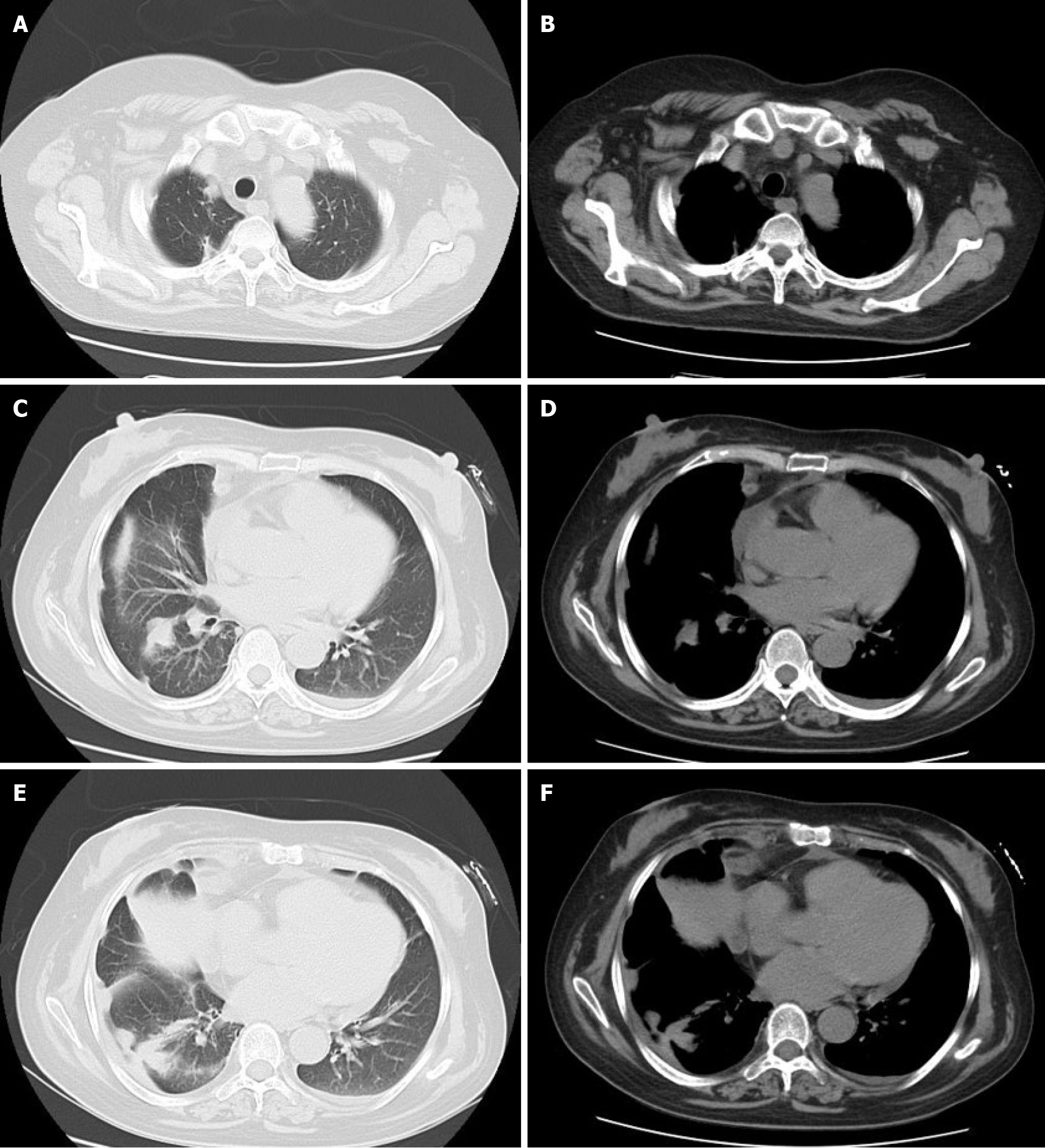
After 8 d of treatment, the patient was discharged from the hospital with improved condition. After 1 mo of treatment, the CT scans showed that the lesions were obviously improved in terms of absorption (Figure 5). The patient has been recurrence-free for 2 years.
Nocardia species, which belong to Actinomycetes, are ubiquitous in the environment, especially in soil and water[1,2]. Nocardiosis is an uncommon infection that usually occurs in immunocompromised patients, such as those with organ transplantation, corticosteroid or cytotoxic agent treatment, HIV infection, and malignancies[1,3]. Infection can occur in many organs, and the pulmonary system is the most common site. The infection can be disseminated further by blood and progress into systemic infection, resulting in poor prognosis, especially if the central nervous system is involved[5,7]. As such, monitoring the patient’s immunity status, especially cellular immunity during corticosteroid use for the present case, is very important.
An accurate diagnosis of nocardiosis is essential for determining appropriate treatment, but it is often misdiagnosed as other infections or malignancy. The definitive diagnosis of nocardiosis is usually based on isolation of microorganisms from clinical samples; however, microorganisms are often difficult to isolate by conventional culture methods. The growth of microorganisms is very slow and may be overlooked by overgrowth of other rapidly growing aerobic bacteria in mixed flora. As such, microbiological samples should be incubated longer to allow Nocardia to grow given that they have a prolonged incubation period of 2 wk to 3 wk[8,9].
Nocardiosis commonly presents as subacute or chronic suppurative disease. The pathological manifestations of nocardiosis are usually granulomas or abscesses[10]. The most common CT findings of pulmonary nocardiosis include multiple nodules, cavitation, consolidation, and masses (or mass-like consolidation) as well as pleural effusion[4-6]. The reported case is special given that the patient had slight pulmonary infiltration but mainly involving the pleura. We hypothesized that the patient’s appearance was due to the spread of the pathogen along pleural or interlobar effusion (pus). Multiple localized nodular or hillock shadows developed in the pleura, mediastinum, and interlobar fissure areas because the lesions usually manifest as granulomas or abscesses, which is different to simple pleural effusion or general bacterial infection. The CT findings in this case need to be differentiated from tuberculous pleurisy and malignancy.
This report illustrates that nocardiosis should be suspected when clinicians encounter patients who are immunocompromised and have diffuse involvement of the pleura on CT. More severe manifestations of nocardiosis should be suspected when prolonged administration of corticosteroids is present.
Manuscript source: Unsolicited manuscript
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Naem AA S-Editor: Yan JP L-Editor: Webster JR P-Editor: Liu JH
| 1. | Restrepo A, Clark NM; Infectious Diseases Community of Practice of the American Society of Transplantation. Nocardia infections in solid organ transplantation: Guidelines from the Infectious Diseases Community of Practice of the American Society of Transplantation. Clin Transplant. 2019;33:e13509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 2. | Haussaire D, Fournier PE, Djiguiba K, Moal V, Legris T, Purgus R, Bismuth J, Elharrar X, Reynaud-Gaubert M, Vacher-Coponat H. Nocardiosis in the south of France over a 10-years period, 2004-2014. Int J Infect Dis. 2017;57:13-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Hui CH, Au VW, Rowland K, Slavotinek JP, Gordon DL. Pulmonary nocardiosis re-visited: experience of 35 patients at diagnosis. Respir Med. 2003;97:709-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Tsujimoto N, Saraya T, Kikuchi K, Takata S, Kurihara Y, Hiraoka S, Makino H, Yonetani S, Araki K, Ishii H, Takizawa H, Goto H. High-resolution CT findings of patients with pulmonary nocardiosis. J Thorac Dis. 2012;4:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 5. | Blackmon KN, Ravenel JG, Gomez JM, Ciolino J, Wray DW. Pulmonary nocardiosis: computed tomography features at diagnosis. J Thorac Imaging. 2011;26:224-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Yoon HK, Im JG, Ahn JM, Han MC. Pulmonary nocardiosis: CT findings. J Comput Assist Tomogr. 1995;19:52-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Rafiei N, Peri AM, Righi E, Harris P, Paterson DL. Central nervous system nocardiosis in Queensland: A report of 20 cases and review of the literature. Medicine (Baltimore). 2016;95:e5255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | McNeil MM, Brown JM. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin Microbiol Rev. 1994;7:357-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 429] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 9. | Bittar F, Rolain JM. Detection and accurate identification of new or emerging bacteria in cystic fibrosis patients. Clin Microbiol Infect. 2010;16:809-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev. 1994;7:213-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 548] [Cited by in RCA: 552] [Article Influence: 17.8] [Reference Citation Analysis (0)] |