Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6804
Peer-review started: January 15, 2021
First decision: February 28, 2021
Revised: March 14, 2021
Accepted: May 15, 2021
Article in press: May 15, 2021
Published online: August 16, 2021
Processing time: 202 Days and 1.5 Hours
Peutz-Jeghers syndrome (PJS) is a genetic disorder characterized by the develop
A 16-year-old teenage male PJS patient presented with a history of colicky abdominal pain, vomiting, blood in stools, loss of appetite, and weight loss. On abdominal examination, a vague mass was palpable over the right upper quadrant. Contrast-enhanced computed tomography (CT) of the abdomen was performed and an intussusception involving the jejunum and rectosigmoid junction was observed. The patient subsequently underwent a laparotomy and intussusception involving the jejunum and another over the ileum was noted intra-operatively. Bowel resection and an endoscopic polypectomy were performed, followed by a primary anastomosis. The patient was discharged well and reviewed again one month later, and was noted to be well.
PJS patients have a high risk of intussusception and can be diagnosed accurately by endoscopic surveillance or radiologically with abdominal CT or magnetic resonance imaging. The mainstay of treatment is surgical intervention followed by endoscopic surveillance with periodic polypectomy.
Core Tip: Peutz-Jeghers syndrome (PJS) is a genetic disorder characterized by the development of gastrointestinal hamartomatous polyps and mucocutaneous melanin pigmentation. Patients with PJS are at risk of complications such as intussusception. Intussusception is a condition where one segment of the intestine invaginates into another, causing intestinal obstruction. We report a PJS patient who was diagnosed with double intussusception in a single setting.
- Citation: Chiew J, Sambanthan ST, Mahendran HA. Double intussusception in a teenage child with Peutz-Jeghers syndrome: A case report. World J Clin Cases 2021; 9(23): 6804-6809
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6804.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6804
Peutz-Jeghers syndrome (PJS) is an autosomal dominant genetic disorder characterized by the development of gastrointestinal hamartomatous polyps and mucocutaneous melanin pigmentation. Patients with PJS are at risk of intussusception, which is a condition where one segment of the intestine invaginates into another, causing in
A 16-year-old Malay male presented to the Emergency Department of our hospital complaining of worsening abdominal pain.
The patient presented with a history of colicky abdominal pain for 1 year and was associated with a history of vomiting, blood in stools, loss of appetite, and loss of weight.
The patient had previously been diagnosed with PJS but had defaulted on subsequent follow-ups.
No significant family history or surgical history was noted.
His vital signs were unremarkable, and on abdominal examination, a vague mass was palpable over the right upper quadrant.
Blood analyses were unremarkable.
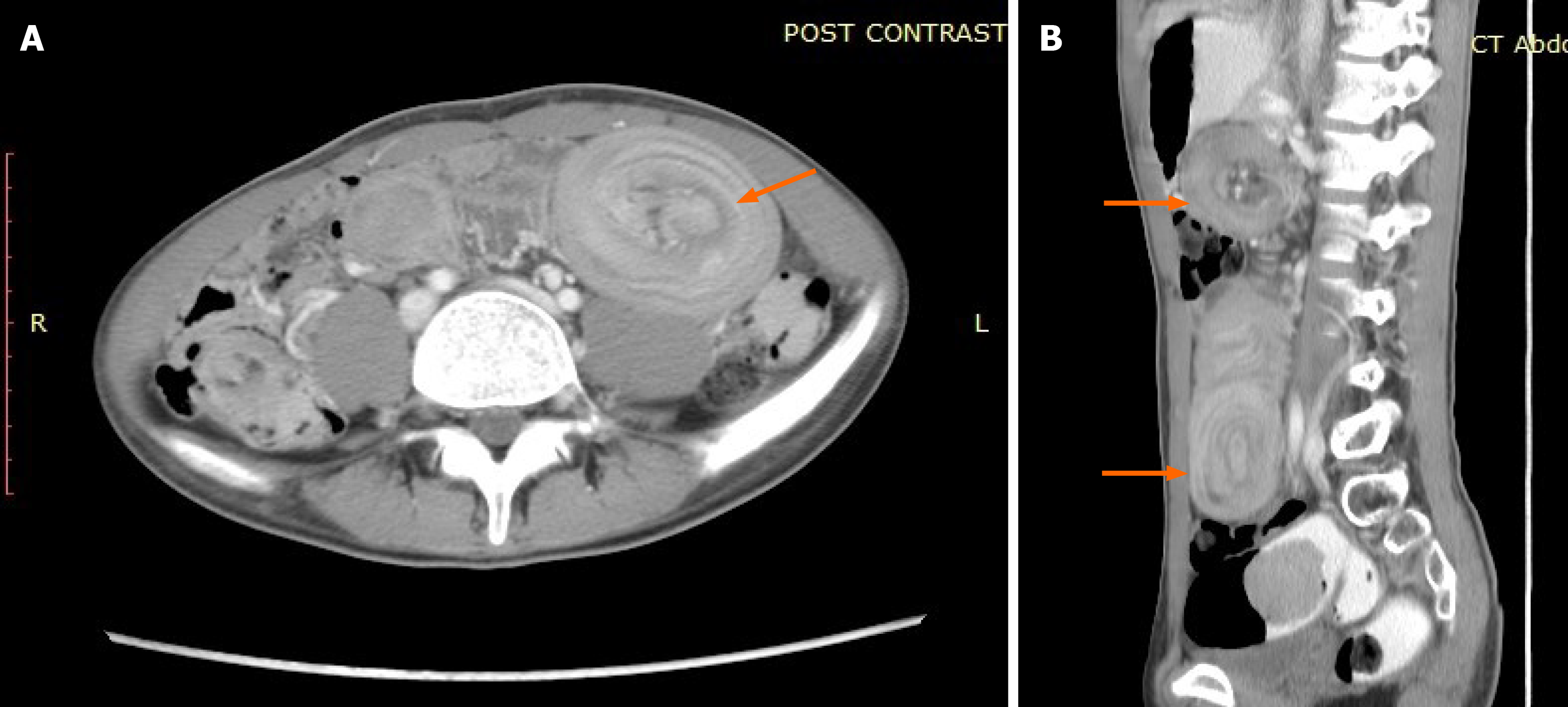
Contrast-enhanced computed tomography (CT) of the abdomen revealed a long segment intussusception in the small bowel extending from the left upper abdomen to the right lower abdomen involving the jejunum and another intussusception involving the rectosigmoid junction (Figure 1A and B).
Intussusception secondary to PJS.
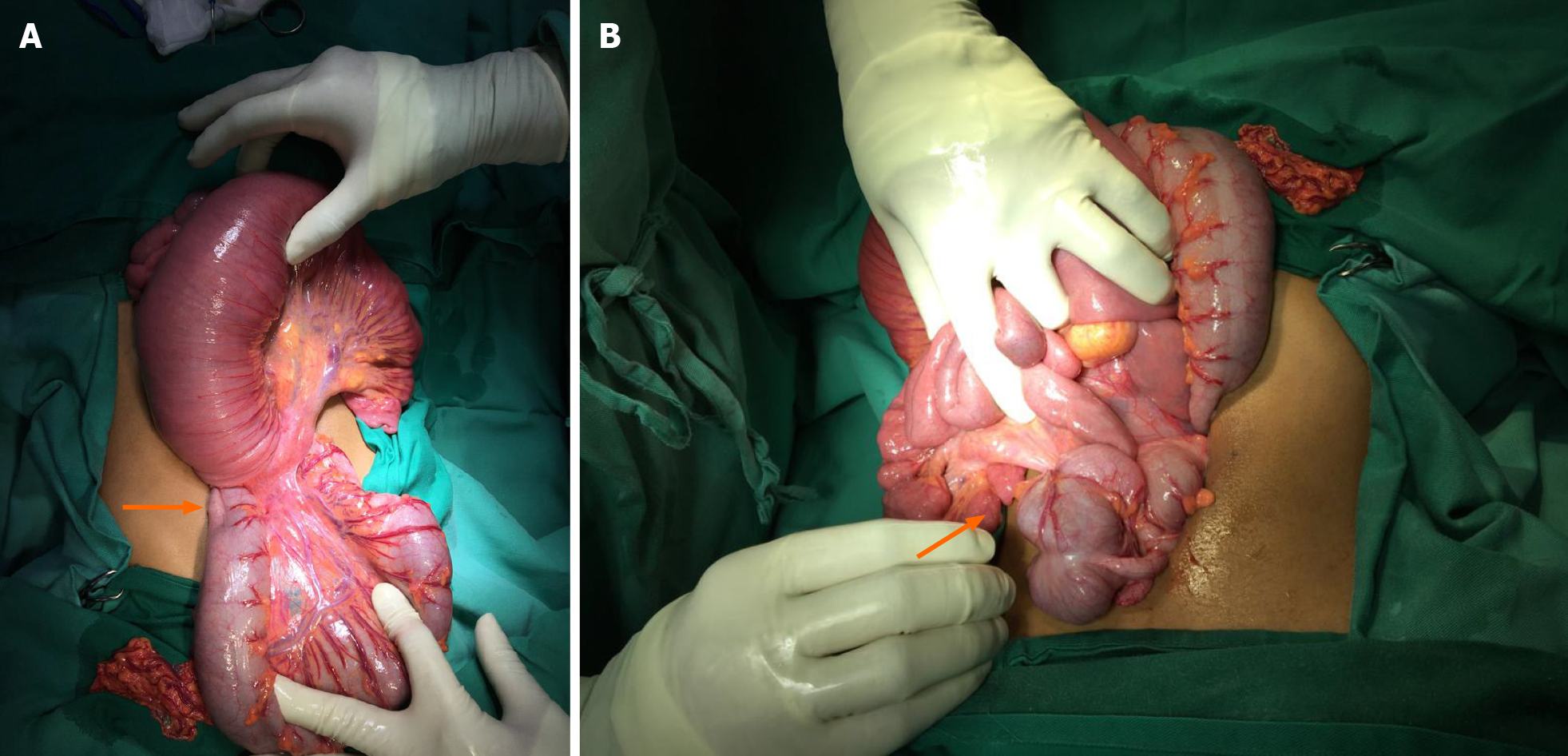
The patient underwent laparotomy. Intra-operatively, there were 2 intussusceptions over the jejunum (Figure 2A) and ileum (Figure 2B) with around 140 cm of bowel length between the 2 intussusceptions. We were able to reduce both intussusceptions; however, we noted multiple large polyps of varying sizes in the area (largest 3-4 cm); hence, it was decided to resect both areas of bowel. Prior to the primary anastomosis of the resected bowels, a gastroscope was inserted through the proximal jejunum, and any visible gastric and duodenal polyps were resected.
The postoperative course was uneventful, and the patient was discharged well. Upon review one-month post-discharge, the patient was noted to be well.
PJS was first described in literature published in 1895 by Dr. Connor, a British physician who reported identical twin sister's with oral pigmentation. One sister died due to intestinal obstruction age 20 years while the other died due to breast cancer aged 59 years[1].
Intussusception was also described as a complication in the year 1942 by Peutz, a German physician. The report described the typical features of a patient with PJS suffering from intussusception, including facial and perioral hyperpigmentation, intermittent abdominal pain, and rectal bleeding. Further analysis of the syndrome led the said physician to conclude that the disease was an autosomal dominant condition[2].
Later, in 1998, it was discovered that the cause of PJS was a mutation in the STK11 gene, also known as the LKB1 gene[3]. STK11/LKB1 genetic mutation is found in around 30% to 70% of PJS patients and in around 70% of patients with a positive family history[4].
The diagnosis of PJS can be made with the presence of hamartomatous polyps in patients with the addition of 2 of the following clinical criteria: labial melanin deposits, positive family history of the syndrome, and small bowel polyposis[5].
The classical triad for intussusception of abdominal pain, mass, and bloody stool was present in our patient. Patients with PJS generally have hundreds of polyposis and are mainly distributed in the small intestine, followed by the large intestine and stomach. Usually, the intestinal polyps are pedunculated, while the polyps in the stomach are broad-based and hamartomatous histologically[6].
These patients are at risk of malignant neoplasm transformation. In 1983, Tovar et al[7] described that 7.14% of children with PJS subsequently developed malignancy, with gonadal tumors being the most common.
Baeza-Herrera et al[2] in 2005, reported that 1.4% of children with PJS also had intussusception. The relationship between PJS and intussusception is a known and predictable outcome as intestinal polyps can increase the risk of the intestine introducing within itself[2].
Nowadays, conventional barium studies have been replaced with more advanced cross-sectional techniques such as ultrasonography, CT, and magnetic resonance imaging (MRI). Ultrasonography will typically show a “doughnut” or a “target” sign picture; however, in this patient, ultrasound was not performed. An abdominal CT scan is the most useful imaging modality as it is helpful in revealing the underlying lesion[8]. Although barium enema can also help in diagnosing intestinal intussusception, a multicenter study by Barussaud et al[9] reported that CT associated or not with barium enema may be the most accurate modality for diagnosis of intussusception in adults. However, the overall diagnostic approach still depends on the patient's clinical presentation.
Definitive surgical intervention is recommended in PJS patients complicated by intestinal obstruction, evidence of malignancy, or considerable gastrointestinal hemorrhage[10-12]. In our case, the patient was complicated by intestinal obstruction caused by intussusceptions due to intestinal polyps.
In a large majority of children with PJS, the existing number of polyps is usually large, causing them to have a recurrent crisis of intussusception that disappears as fast as it appear. It may be due to the large number of polyps present in a short segment of the intestine which causes the intussusception to reoccur, and the child may need multiple surgeries[2].
With the advent of emerging endoscopic techniques, combined endoscopic and surgical interventions have been performed successfully in the reduction of an ileoileal intussusception followed by a double-balloon endoscopic (DBE) resection of the polyp[13,14].
The usage of DBE avoids the need for urgent laparotomy in which the patient can limit the risk of the development of short bowel syndrome. However, this can be limited by the lack of resources in some centers.
In the event of signs suggesting bowel ischemia or peritonitis, an emergency laparotomy is still the preferred choice. In patients with bowel ischemia or an irreversible correction, en bloc removal of the affected intestine followed by a primary anastomosis is recommended. Once the derivation is planned, enterostomies and intra-operative endoscopy must be utilized to extract the highest number of polyps as possible as the disease will produce recurrent intussusceptions[2].
In our case, we were able to perform endoscopic polypectomy for the large polyps preventing future reoccurrence of intussusception and intraoperatively, the patient did not require major resection except for the intussusception segment. However, we were unable to address the polyps in the entire small bowel as it may cause short bowel syndrome if resected.
PJS is an autosomal dominant condition characterized by hamartomatous polyps primarily in the small intestine and mucocutaneous pigmentation. PJS patients have a high risk of intussusception, especially in the younger age group.
Hence, patients with PJS are strongly recommended to have regular follow-up examinations and periodic polypectomy of the entire small bowel to prevent complications[15].
Wireless capsule endoscopy is an emerging and popular diagnostic method and has been found to have a higher diagnostic yield of polyps found as compared to a CT or MRI study[16]. CT and MRI with oral contrast are other options for screening, in which MRI is more advantageous when compared to CT as it prevents young people from being exposed to high doses of radiation and has a higher accuracy rate.
Treatment is mainly surgical intervention followed by endoscopic or radiological surveillance with periodic polypectomy. Patients with PJS should have regular follow-up throughout their lives as they are at risk of malignant transformation.
We would like to thank the Director-General of Health Malaysia for his permission to publish this article. We would also like to express our gratitude to the Surgical Department of Hospital Sultanah Aminah Johor Bahru, and those who have extended their help in contributing to this manuscript.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Malaysian Medical Council, No. 68395.
Specialty type: Surgery
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Di Nardo G S-Editor: Wang JL L-Editor: Webster JR P-Editor: Ma YJ
| 2. | Baeza-Herrera C, García-Cabello LM, Nájera-Garduño HM, Sánchez-Fernández LA, Mora-Hernández F, Ortiz-Zúñiga AI. Surgical aspects of intussusception secondary to Peutz-Jeghers syndrome. Cir Cir. 2005;73:91-95. [PubMed] |
| 3. | Hemminki A, Markie D, Tomlinson I, Avizienyte E, Roth S, Loukola A, Bignell G, Warren W, Aminoff M, Höglund P, Järvinen H, Kristo P, Pelin K, Ridanpää M, Salovaara R, Toro T, Bodmer W, Olschwang S, Olsen AS, Stratton MR, de la Chapelle A, Aaltonen LA. A serine/threonine kinase gene defective in Peutz-Jeghers syndrome. Nature. 1998;391:184-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1136] [Cited by in RCA: 1083] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 4. | Jenne DE, Reimann H, Nezu J, Friedel W, Loff S, Jeschke R, Müller O, Back W, Zimmer M. Peutz-Jeghers syndrome is caused by mutations in a novel serine threonine kinase. Nat Genet. 1998;18:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 802] [Cited by in RCA: 765] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 5. | Giardiello FM, Trimbath JD. Peutz-Jeghers syndrome and management recommendations. Clin Gastroenterol Hepatol. 2006;4:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 257] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 6. | McGarrity TJ, Kulin HE, Zaino RJ. Peutz-Jeghers syndrome. Am J Gastroenterol. 2000;95:596-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 154] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Tovar JA, Eizaguirre I, Albert A, Jimenez J. Peutz-Jeghers syndrome in children: report of two cases and review of the literature. J Pediatr Surg. 1983;18:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 47] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Wang H, Luo T, Liu WQ, Huang Y, Wu XT, Wang XJ. Clinical presentations and surgical approach of acute intussusception caused by Peutz-Jeghers syndrome in adults. J Gastrointest Surg. 2011;15:2218-2225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, Lehur PA, Hamy A, Leborgne J, le Neel JC, Mirallie E. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis. 2006;21:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 164] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 10. | Fraser JD, Briggs SE, St Peter SD, De Petris G, Heppell J. Intussusception in the adult: an unsuspected case of Peutz-Jeghers syndrome with review of the literature. Fam Cancer. 2009;8:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Gonzalez AM, Clapp B. Laparoscopic management of small bowel intussusception in a 16-year-old with Peutz-Jeghers syndrome. JSLS. 2008;12:332-334. [PubMed] |
| 12. | Akimaru K, Katoh S, Ishiguro S, Miyake K, Shimanuki K, Tajiri T. Resection of over 290 polyps during emergency surgery for four intussusceptions with Peutz-Jeghers syndrome: Report of a case. Surg Today. 2006;36:997-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Miura Y, Yamamoto H, Sunada K, Yano T, Arashiro M, Miyata T, Sugano K. Reduction of ileoileal intussusception by using double-balloon endoscopy in Peutz-Jeghers syndrome (with video). Gastrointest Endosc. 2010;72:658-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Sakamoto H, Yamamoto H, Hayashi Y, Yano T, Miyata T, Nishimura N, Shinhata H, Sato H, Sunada K, Sugano K. Nonsurgical management of small-bowel polyps in Peutz-Jeghers syndrome with extensive polypectomy by using double-balloon endoscopy. Gastrointest Endosc. 2011;74:328-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Oncel M, Remzi FH, Church JM, Connor JT, Fazio VW. Benefits of 'clean sweep' in Peutz-Jeghers patients. Colorectal Dis. 2004;6:332-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Kopacova M, Tacheci I, Rejchrt S, Bures J. Peutz-Jeghers syndrome: diagnostic and therapeutic approach. World J Gastroenterol. 2009;15:5397-5408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 135] [Cited by in RCA: 126] [Article Influence: 7.9] [Reference Citation Analysis (1)] |