Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6759
Peer-review started: February 7, 2021
First decision: March 6, 2021
Revised: April 15, 2021
Accepted: July 7, 2021
Article in press: July 7, 2021
Published online: August 16, 2021
Processing time: 183 Days and 23.7 Hours
Acute colonic diverticulitis (ACD) is common in Western countries, with its prevalence increasing throughout the world. As a result of the coronavirus disease 2019 (COVID-19), elective surgery and in-patients’ visits have been cancelled or postponed worldwide.
To systematically explore the impact of the pandemic in the management of ACD.
MEDLINE, Embase, Scopus, MedxRiv, and the Cochrane Library databases were searched to 22 December 2020. Studies which reported on the management of patients with ACD during the COVID-19 pandemic were eligible. For cross sectional studies, outcomes of interest included the number of hospital admission for ACD, as well as key features of disease severity (complicated or not) across two time periods (pre- and during lockdown).
A total of 69 papers were inspected, and 21 were eligible for inclusion. Ten papers were cross sectional studies from seven world countries; six were case reports; three were qualitative studies, and two review articles. A 56% overall decrease in admissions for ACD was observed during lockdown, peaking 67% in the largest series. A 4%-8% decrease in the rate of uncomplicated diverticulitis was also noted during the lockdown phase. An initial non-operative management was recommended for complicated diverticulitis, and encouraged to an out-of-hospital regimen. Despite initial concerns on the use of laparoscopy for Hinchey 3 and 4 patients to avoid aerosolized contamination, societal bodies have progressively mitigated their initial recommendations as actual risks are yet to be ascertained.
During the COVID-19 pandemic, fewer patients presented and were diagnosed with ACD. Such decline may have likely affected the spectrum of uncomplicated disease. Established outpatient management and follow up for selected cases may unburden healthcare resources in time of crisis.
Core Tip: Acute colonic diverticulitis is one of the most common conditions encountered by surgeons in the acute setting. As a result of the pandemic, elective surgery and in-patients’ visits have been cancelled or postponed worldwide. Conservative strategies for surgical diseases, such as acute appendicitis and acute cholecy
- Citation: Gallo G, Ortenzi M, Grossi U, Di Tanna GL, Pata F, Guerrieri M, Sammarco G, Di Saverio S. What paradigm shifts occurred in the management of acute diverticulitis during the COVID-19 pandemic? A scoping review. World J Clin Cases 2021; 9(23): 6759-6767
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6759.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6759
Since its declaration as a pandemic by the World Health Organization in March 2020, coronavirus disease 2019 (COVID-19) has severely affected health systems throughout the globe.
As of 27 January 2021, the number of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections was just over the 100 million mark[1].
In the effort to increase local responses to the ongoing need for hospital beds and facilities for COVID-19 patients, surgical services have been reshaped[2]. Elective surgery and in-patient visits have been cancelled or postponed[3]. Conservative strategies for surgical diseases, such as acute appendicitis and acute cholecystitis, have also been supported[4], as have more frequent indications for stoma formation in urgent colonic resections for the prevention of the life-threatening consequences of anastomotic leaks. Furthermore, perioperative infection from SARS-CoV-2 has proven to be detrimental for the overall survival and complication rates in surgical patients[5].
Acute diverticulitis represents a common cause of surgical admission in emergency settings[6]. Whether the pandemic has had an impact on the rate of admission and treatment for acute diverticulitis has not yet been systematically explored. For these reasons, we conducted a scoping review in order to map the research currently being performed in this area.
A systematic scoping review was performed according to a predefined protocol. The study was reported in line with the PRISMA Extension for Scoping Reviews[7].
A scoping search was undertaken to identify published articles related to the management of patients with acute diverticulitis during the SARS-CoV-2 pandemic.
To be included in the review, papers needed to report on the management of patients with acute diverticulitis during the COVID-19 pandemic. Articles in any language were included. Any study design was eligible. Quantitative, qualitative and mixed-method studies were included in order to consider different methods of measuring treatment burdens. Papers were excluded if they did not fit into the conceptual framework of the study.
To identify potentially relevant documents, the following bibliographic databases were searched from December 1, 2019 to December 22, 2020: MEDLINE, Embase, Scopus, MedxRiv and the Cochrane Library databases. The final search strategy for EMBASE was “(diverticulosis OR 'colon diverticulosis' OR diverticulitis) AND ('coronavirus disease 2019' OR 'severe acute respiratory syndrome coronavirus 2')”.
Two reviewers (Ortenzi M and Grossi U) sequentially evaluated the titles, abstracts and, finally, the full text of all publications; all publications were identified by our searchers for their potential relevance. Any disagreements on study selection and data extraction were resolved by consensus and discussion with other authors (GG and SDS).
A single investigator (Ortenzi M) charted all data from eligible papers using a semi-structured charting pro-forma designed for the purpose of this study. Two other researchers verified the data’s accuracy (Gallo G and Grossi U).
We abstracted data on article (country of origin) and patient characteristics. No assessments of study quality were undertaken. A narrative synthesis of data collected from eligible papers is presented.
In contrast to classic meta-analyses, the outcome was defined as the percentages of an event (without comparison) in pseudo-cohorts of observed patients. Overall proportions can be estimated from the weighted mean of percentages measured in each study. Data were expressed using descriptive statistics, including proportions and averages.
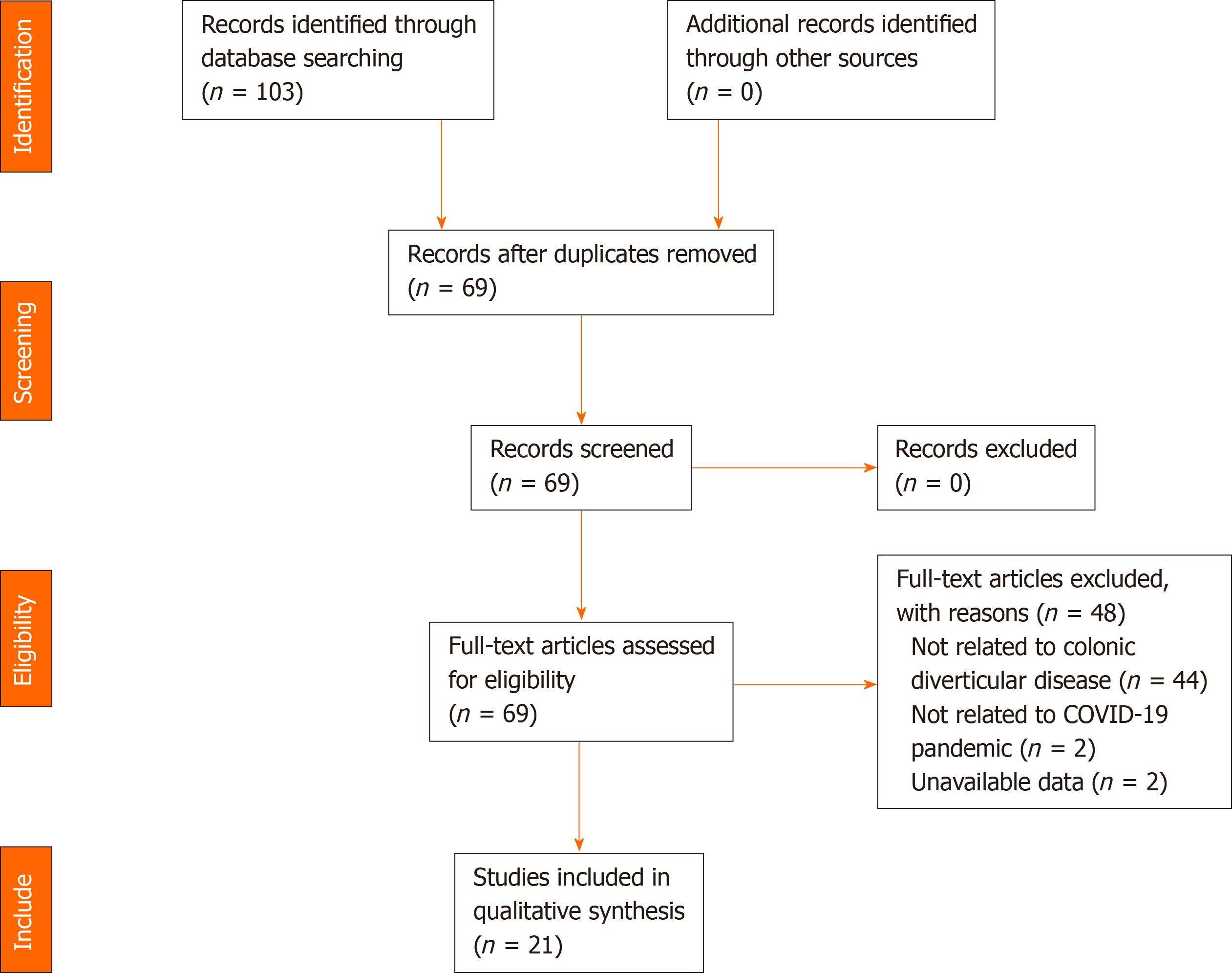
After 34 duplicates were removed, a total of 69 citations were identified from searches of electronic databases and review article references. Based on the title and the abstract, 48 citations were excluded, with 21 full text articles being retrieved and assessed for eligibility. Of these, the following were considered eligible for this review: 10 cross sectional studies[8-17], 6 case reports[18-23], 3 qualitative studies[3,24,25] and 2 review articles[26,27] (Figure 1).
Of the included cross-sectional studies (Table 1), two were multicentric[12,14]. The timing of the outbreak differed in each country at the time of data collection. Indeed, the number of COVID-19 cases ranged from 1 to 3036 per 106 people at the mid lockdown phase of data collection. Overall, admissions for acute diverticulitis decreased by 56%, from 749 in pre-lockdown to 332 during lockdown. A higher percentage reduction (up to 67%) was observed in the largest series[11,12,14,16,17]. A 4%-8% decrease in the rate of uncomplicated diverticulitis (defined as localized diverticular inflammation without any abscess or perforation) was also noted during the lockdown phase in the three studies from United States.[11,16,17]
| Ref. | Country | No. COVID cases per 106 people at mid lockdown period2 | Observation periods during and pre-lockdown (d) | Patients (n) | Percentage reduction | Uncomplicated diverticulitis (%) | ||
| Lockdown | Pre-lockdown | Lockdown | Pre-lockdown | |||||
| Anteby et al[8] | Israel | 1 | 30 | 2 | 11 | -82% | NR | NR |
| Boyle et al[9] | New Zealand | 272 | 33 | 17 | 15 | 0.1% | 11 (65) | 8 (53) |
| Chung et al[10] | United Kingdom | 1383 | 32 | 20 | NR | NA | NR | NR |
| Gibson et al[11] | United States | 2395 | 77 | 56 | 139 | -60% | 40 (71) | 105 (76) |
| Guadalajara et al[12] | Spain1 | 3036 | 49 | NR | NR | -60% | NR | NR |
| O'Brien et al[13] | Canada | 228 | 31 | 15 | 20 | -25% | NR | NR |
| Rausei et al[14] | Italy1 | 409 | 31 | 31 | 94 | -67% | NR | NR |
| Rosa et al[15] | Italy | 1431 | 73 | 6 | 9 | -33% | NR | NR |
| Soriano et al[16] | United States | 621 | 91 | 65 | 122 | -47% | 50 (77) | 99 (81) |
| Zintsmaster et al[17] | United States | 1017 | 49 | 120 | 339 | -65% | 106 (88) | 324 (96) |
There were six case reports among the included papers. Badar et al[18] described the case of an 82-year-old male with colo-colonic fistula as a result of delayed presentation and the onset of conservative treatment of diverticular abscess due to concerns regarding SARS-CoV-2 exposure in hospital.
Costanzi et al[19] presented the case of a 64-year-old male with mild acute respiratory distress syndrome related to COVID-19 pneumonia and perforated diverticulitis of the sigmoid colon. The operation was delayed due to an intensive care unit (ICU) bed shortage, and the patient was monitored and treated with antibiotics until a repeated computed tomography scan after 6 d, which showed an increase in the para-sigmoid collection. An ICU bed eventually became available, and the patient underwent a laparotomic Hartmann procedure.
Fabbri et al[20] described the case of an 80-year-old woman who was admitted with COVID-19 gastrointestinal symptoms and discharged after 2 wk on improved general clinical conditions. Due to a recurrence of gastrointestinal symptoms, the patient was readmitted to hospital and underwent an urgent exploratory laparotomy for a pinpoint perforation of a sigmoid diverticulum.
Lisi et al[21] outlined the state of colorectal emergency surgical activity during the first 2 wk of the second COVID-19 wave in Italy by focusing on the increase in the number of complex cases. Among the 11 difficult cases of emergency colorectal surgery, 4 were Hinchey stage 3 and 4 were diverticulitis.
Montali et al[22] reported the first confirmed case of early postoperative SARS-CoV-2 infection in an 83-year-old male recovering after a Hartmann’s procedure for acute diverticulitis. After an otherwise uneventful postoperative course, the patient developed acute respiratory failure on post-operative day 8, leading to death 36 h later.
Patel et al[23] described the case of a 38-year-old male presenting with acute perforated diverticulitis three days after being discharged from the hospital for respiratory symptoms secondary to COVID-19.
The three qualitative studies published between March and April 2020 contained practice recommendations from the first COVID-19 outbreak[3,24,25]. All highlighted that there was a dearth of evidence related to the management of patients needing surgery for colorectal conditions during the COVID-19 pandemic.
While specifically addressing complicated diverticulitis, an initial conservative approach, with subsequent observation and antibiotic treatment, was recommended[3,24,25]. This may also be encouraged for an out-of-hospital regimen (combined with percutaneous drainage, if necessary)[24]. Meanwhile, in COVID-19 positive patients, open surgery may be preferred to laparoscopic surgery for Hinchey 3 and 4 patients to avoid aerosolized contamination, and Hartmann might be preferred over anastomosis in this particular situation[3].
A systematic review by De Simone et al[26] focused on the impact on the management of emergency and trauma surgery on the acute abdomen. Trained staff, adequate instruments and strict application of the recommendations were deemed crucial to avoid increasing the risk of contamination. In case of a lack of skills or adapted materials for enabling a safe laparoscopic surgical intervention, a laparotomy should be privileged.
As for acute diverticulitis, its management should follow the WSES guidelines[6], with a word of caution regarding the utilization of laparoscopy because of the risk of aerosolization[28], especially if a long operative duration is expected.
A second review by El Boghdady and Ewalds-Kvist[27] specifically addressed the debates raised around the safety of laparoscopic surgery during the pandemic, especially given the potential generation of contaminated aerosols from CO2 leakage and the creation of smoke from the use of energy devices. The authors concluded that, in COVID-19 patients, non-operative treatment and delay of surgery should be considered whenever possible and safe, even with established outpatient management and follow-up for subacute, uncomplicated and/or mild abdominal conditions (e.g., uncomplicated or Hinchey 1a diverticulitis). Follow-up can, for instance, be conducted by telephone if a patient can use antibiotics and is reliable in assessing their response to treatment.
In this scoping review, we identified 21 studies that reported on the management of acute diverticulitis in the COVID-19 era; all studies were published in 2020. Our findings indicate that there is a general lack of high-quality evidence regarding the impact of the COVID-19 pandemic on epidemiology and the management of acute diverticulitis. However, most studies showed a substantial decrease in the number of overall admissions between the pre-lockdown and lockdown phases. Some authors noticed how this trend was at odds with that observed in the pre-pandemic period, as it had been increasing in recent years[11,16].
The first finding could somehow be expected, especially given the need to set preventive measures, such as social distancing, to limit the spread of the virus and the associated widespread fear of infection that prevented patients from seeking medical care, even when necessary[15]. Some of the reasons put forward to explain this trend include changes in lifestyle during confinement, particularly with regard to diet (i.e., low-fat, less convenience food), hygiene (i.e., handwashing and personal hygiene, environmental sanitation), habits (i.e., less stressing activities) and reduced bed availability in hospital[11,14].
Given the recommendation to be more cautious in the indication of surgery, as well as the preference for non-operative management when feasible, one would expect that the incidence of a disease requiring a surgical treatment would have been unchanged, even during a pandemic. However, a significant decrease in the overall number of diverticulitis cases failed to mirror a concomitant reduction in complicated diverticulitis. Indeed, the number of more complicated cases that required surgery and/or hospitalization remained fairly unchanged or slightly reduced in some studies [11,14,17].
The initial warnings about the possible role of nonsteroidal anti-inflammatory drugs and corticosteroids in worsening the severity of COVID-19[29] may have discouraged their use; this may potentially explain the decreased incidence of perforated diverticulitis (for demonstrated cause–effect relationships)[14]. These trends were also confirmed in an Italian survey administered to 150 Italian heads of General Surgery[30].
It has been a year since the first outbreak, yet little is known about the evolution of SARS-CoV-2 infection in patients undergoing surgery. The same could be said in relation to the real impact of the pandemic on surgery for diverticulitis. An intense debate emerged regarding the timing of surgery for abdominal emergencies at different levels, including acute diverticulitis. Studies uniformly advised taking extra precautions when it came to delaying surgery, even in the presence of a free perforation if the condition of a patient was not stable enough.
Secondly, the published recommendations were broadly concordant in favoring a Hartmann procedure over a sigmoidectomy. This is unsurprising given both the high risk of complications (e.g., anastomotic leak and intra-abdominal collections) and the subsequent consumption of healthcare resources that the latter entails. It was also mentioned that patients with an ongoing COVID-19 infection carry a higher risk of post-operative morbidity and mortality[3].
Thirdly, an intense debate about the utilization of the laparoscopic approach was generated. After some first publications aimed to discourage the utilization of laparoscopy, several societies progressively mitigated their initial recommendations and statements[14]. Moreover, after the first wave of COVID-19 infections, these societies no longer took a clear position for or against its use, which sometimes generated more confusion among surgeons regarding whether laparotomy was appropriate or not.
We still lack evidence regarding whether SARS-CoV-2 can be found in smoke/aerosol generated within the peritoneal cavity, though the theoretical risks may be extrapolated from previous pandemics and viral infections[20]. Laparoscopy can be used with precautions because of its benefits compared to open surgery. We concluded that recommended precautions should be respected while performing laparoscopy during the pandemic[3]. On the other hand, surgeons may feel safer performing open surgery. However, the underlying reason for doing so should not be found in the supposed increased risk of virus spread but in the fact that open surgery can be less time-consuming, especially if laparoscopic skills are lacking.
The key strength of this review is its broad inclusion of study designs, which allowed us to construct a representative summary of novel and heterogeneous literature. Limitations included the difficulty in making solid comparisons between studies, as well as the diverticulitis-specific nature of this study. Hence, a number of studies where data on patients with diverticulitis could not be segregated by other abdominal emergencies were excluded.
During the COVID-19 pandemic, there was a reduction in the rate of both complicated and uncomplicated diverticulitis. As a result of a switch towards non-operative treatment and clinical follow-up in selected patients with diverticular disease, the pandemic outbreak may have unburdened healthcare resources in time of crisis.
Acute diverticulitis represents a common cause of surgical admission in emergency settings.
The pandemic has had an impact on the rate of admission and treatment for acute diverticulitis. The aim of this review is to map the research done in this area.
The main objective of this review was to systematically explore the impact of the coronavirus disease 2019 (COVID-19) pandemic on the rate of admission and treatment for acute diverticulitis.
We searched five electronic databases from December 1, 2019 to December 22, 2020, for studies that reported on the management of patients with acute diverticulitis during the COVID-19 pandemic. Quantitative, qualitative and mixed-method studies were included in order to consider different aspects of measuring treatment burden. Overallproportions were estimated from the weighted mean of percentages measured in each study. Data were expressed using descriptive statistics, including proportions and averages.
The review demonstrated an overall decrease in admissions for acute complicated diverticulitis (ACD) during the pandemic peak and consequent lockdown, peaking 67% in the largest series. A reduction in the rate of uncomplicated diverticulitis was observed as well. The pandemic outbreak produced a major shift towards non-operative and out-of-hospital management of ACD.
During the COVID-19 pandemic, there was a reduction in the rate of both complicated and uncomplicated diverticulitis. The pandemic outbreak may have unburdened healthcare resources in time of crisis as a result of a switch towards non-operative treatment and clinical follow-up in selected patients with diverticular disease.
Whether the pandemic has had an impact on the rate of admission and treatment for acute diverticulitis has not yet been systematically explored. Besides offering a general overview of the changes in epidemiology and management of acute diverticulitis that occurred during the pandemic, the review will inform on changes in the management of this disease in the likely forecast that severe acute respiratory syndrome coronavirus 2 will become a chronic problem to deal with.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: European Society of Coloproctology.
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bulian D S-Editor: Liu M L-Editor: A P-Editor: Li JH
| 1. | Coronavirus disease (COVID-19). Weekly Epidemiological Update and Weekly Operational Update. [cited 27 January 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. |
| 2. | Gallo G, Trompetto M. The Effects of COVID-19 on Academic Activities and Surgical Education in Italy. J Invest Surg. 2020;33:687-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Di Saverio S, Pata F, Gallo G, Carrano F, Scorza A, Sileri P, Smart N, Spinelli A, Pellino G. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22:625-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 142] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 4. | COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440-1449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 454] [Cited by in RCA: 667] [Article Influence: 133.4] [Reference Citation Analysis (0)] |
| 5. | COVID Surg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1185] [Cited by in RCA: 1220] [Article Influence: 244.0] [Reference Citation Analysis (0)] |
| 6. | Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R, Ceresoli M, Chiara O, Chiarugi M, Coimbra R, Cortese F, Cui Y, Damaskos D, De' Angelis GL, Delibegovic S, Demetrashvili Z, De Simone B, Di Marzo F, Di Saverio S, Duane TM, Faro MP, Fraga GP, Gkiokas G, Gomes CA, Hardcastle TC, Hecker A, Karamarkovic A, Kashuk J, Khokha V, Kirkpatrick AW, Kok KYY, Inaba K, Isik A, Labricciosa FM, Latifi R, Leppäniemi A, Litvin A, Mazuski JE, Maier RV, Marwah S, McFarlane M, Moore EE, Moore FA, Negoi I, Pagani L, Rasa K, Rubio-Perez I, Sakakushev B, Sato N, Sganga G, Siquini W, Tarasconi A, Tolonen M, Ulrych J, Zachariah SK, Catena F. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 224] [Cited by in RCA: 201] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 7. | Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22118] [Cited by in RCA: 18341] [Article Influence: 2620.1] [Reference Citation Analysis (1)] |
| 8. | Anteby R, Zager Y, Barash Y, Nadler R, Cordoba M, Klang E, Klein Y, Ram E, Gutman M, Horesh N. The Impact of the Coronavirus Disease 2019 Outbreak on the Attendance of Patients with Surgical Complaints at a Tertiary Hospital Emergency Department. J Laparoendosc Adv Surg Tech A. 2020;30:1001-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Boyle LI, Boyle A, Jay S, Marnewick J. COVID-19 lockdown impact on common general surgical acute presentations to a regional centre in New Zealand. N Z Med J. 2020;133:96-105. [PubMed] |
| 10. | Chung WY, Winyard J, Layton GR, Isherwood J, Issa E, Radjendrin A, Sangal S, Dennison AR, Garcea G. Impact of the COVID-19 pandemic on acute adult surgical admissions- a single centre experience. Br J Surg. 2020;107:e370-e371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Gibson AL, Chen BY, Rosen MP, Paez SN, Lo HS. Impact of the COVID-19 pandemic on emergency department CT for suspected diverticulitis. Emerg Radiol. 2020;27:773-780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Guadalajara H, Muñoz de Nova JL, Fernandez Gonzalez S, Yiasemidou M, Recarte Rico M, Juez LD, García Septiem J, Galindo Jara P, García Virosta M, Lobo Martínez E, Martín-Pérez E, García-Olmo D; PIACO Collaboration Group. Patterns of acute surgical inflammatory processes presentation of in the COVID-19 outbreak (PIACO Study): Surgery may be the best treatment option. Br J Surg. 2020;107:e494-e495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 13. | O'Brien CM, Jung K, Dang W, Jang HJ, Kielar AZ. Collateral Damage: The Impact of the COVID-19 Pandemic on Acute Abdominal Emergency Presentations. J Am Coll Radiol. 2020;17:1443-1449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Rausei S, Ferrara F, Zurleni T, Frattini F, Chiara O, Pietrabissa A, Sarro G; for Italian Association of Hospital Surgeons; and Collected Data Contributors. Dramatic decrease of surgical emergencies during COVID-19 outbreak. J Trauma Acute Care Surg. 2020;89:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Rosa F, Covino M, Sabia L, Quero G, Fiorillo C, Cozza V, Sganga G, Gasbarrini A, Franceschi F, Alfieri S. Surgical emergencies during SARS-CoV-2 pandemic lockdown: what happened? Eur Rev Med Pharmacol Sci. 2020;24:11919-11925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 16. | Soriano C, Kaplan JA, Law JK, Williams BL, Blackmore CC, Simianu VV. The Immediate, Hospital-Level Impact of Stay-at-Home Order on Diverticulitis Burden. J Gastrointest Surg. 2021;25:533-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Zintsmaster MP, Myers DT. Patients avoided important care during the early weeks of the coronavirus pandemic: diverticulitis patients were more likely to present with an abscess on CT. Emerg Radiol. 2021;28:279-282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Badar F, Schwartzberg D, Rajapakse R. S1820 Diverticulitis in the Time of COVID-19: Acute Diverticulitis Complicated by Colo-Colonic Fistula. Am J Gastroenterol. 2020;115:S941-S942. [DOI] [Full Text] |
| 19. | Costanzi A, Monteleone M, Confalonieri M, Colletti G, Frattaruolo C, Magni C, Corizia L, Fingerhut A. COVID-19 and acute perforated diverticulitis: management and surgical timing. Minerva Chir. 2020;75:468-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Fabbri N, Righini E, Cardarelli L, Di Marco L, V Feo C. Risks of COVID-19 transmission in blood and serum during surgery A prospective cross-sectional study from a single dedicated COVID-19 center. Ann Ital Chir. 2020;91:235-238. [PubMed] |
| 21. | Lisi G, Campanelli M, Villa M, Grande S, Grande M. Colorectal emergency surgery in a COVID-19 referral hospital during the phase 2 in Italy. Int J Colorectal Dis. 2020;35:2137-2138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Montali F, Palmieri G, Casali L, Pagliai L, Costi R. Rapidly fatal outcome of Covid-19 after successful emergency surgery during pandemic outbreak in Northern Italy. Int J Surg Case Rep. 2020;73:9-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Patel P, Phan E, Pona A, Mao Y. S1625 Acute Perforated Diverticulitis as a Potential Complication of SARS-CoV-2 (COVID-19). Am J Gastroenterol. 2020;115:S834. [PubMed] [DOI] [Full Text] |
| 24. | Aranda-Narváez JM, Tallón-Aguilar L, Pareja-Ciuró F, Martín-Martín G, González-Sánchez AJ, Rey-Simó I, Tamayo-Medel G, Yánez-Benítez C, Costa-Navarro D, Montón-Condón S, Navarro-Soto S, Turégano-Fuentes F, Pérez-Díaz MD, Ceballos-Esparragón J, Jover-Navalón JM, Balibrea JM, Morales-Conde S. [Emergency Surgery and Trauma Care During COVID-19 Pandemic. Recommendations of the Spanish Association of Surgeons]. Cir Esp (Engl Ed). 2020;98:433-441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Gallo G, La Torre M, Pietroletti R, Bianco F, Altomare DF, Pucciarelli S, Gagliardi G, Perinotti R. Italian society of colorectal surgery recommendations for good clinical practice in colorectal surgery during the novel coronavirus pandemic. Tech Coloproctol. 2020;24:501-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 26. | De Simone B, Chouillard E, Di Saverio S, Pagani L, Sartelli M, Biffl WL, Coccolini F, Pieri A, Khan M, Borzellino G, Campanile FC, Ansaloni L, Catena F. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020;102:323-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 162] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 27. | El Boghdady M, Ewalds-Kvist BM. Laparoscopic Surgery and the debate on its safety during COVID-19 pandemic: A systematic review of recommendations. Surgeon. 2021;19:e29-e39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 28. | Bianco F, Incollingo P, Grossi U, Gallo G. Preventing transmission among operating room staff during COVID-19 pandemic: the role of the Aerosol Box and other personal protective equipment. Updates Surg. 2020;72:907-910. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Capuano A, Scavone C, Racagni G, Scaglione F; Italian Society of Pharmacology. NSAIDs in patients with viral infections, including Covid-19: Victims or perpetrators? Pharmacol Res. 2020;157:104849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 30. | Patriti A, Baiocchi GL, Catena F, Marini P, Catarci M; FACS on behalf of the Associazione Chirurghi Ospedalieri Italiani (ACOI). Emergency general surgery in Italy during the COVID-19 outbreak: first survey from the real life. World J Emerg Surg. 2020;15:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |