Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6705
Peer-review started: January 7, 2021
First decision: February 12, 2021
Revised: February 21, 2021
Accepted: April 20, 2021
Article in press: April 20, 2021
Published online: August 16, 2021
Processing time: 210 Days and 6.3 Hours
Patients with ankylosing spondylitis (AS) combined with severe cervical fusion deformity have difficult airways. Awake fiberoptic intubation is the standard treatment for such patients. Alleviating anxiety and discomfort during intubation while maintaining airway patency and adequate ventilation is a major challenge for anesthesiologists. Bronchial blockers (BBs) have significant advantages over double-lumen tubes in these patients requiring one-lung ventilation.
To evaluate effective drugs and their optimal dosage for awake fiberoptic nasotracheal intubation in patients with AS and to assess the pulmonary isolation effect of one-lung ventilation with a BB.
We studied 12 AS patients (11 men and one woman) with lung or esophageal cancer who underwent thoracotomy with a BB. Preoperative airway evaluation found that all patients had a difficult airway. All patients received an intramuscular injection of penehyclidine hydrochloride (0.01 mg/kg) before anesthesia. In the operating room, dexmedetomidine(0.5 μg/kg) was infused intravenously for 10 min, with 2% lidocaine for airway surface anesthesia, and a 3% ephedrine cotton swab was used to contract the nasal mucosa vessels. Before tracheal intubation, fentanyl (1 μg/kg) and midazolam (0.02 mg/kg) were administered intravenously. Awake fiberoptic nasotracheal intubation was performed in the semi-reclining position. Intravenous anesthesia was administered immediately after successful intubation, and a BB was inserted laterally. The pre-intubation preparation time, intubation time, facial grimace score, airway responsiveness score during the fiberoptic introduction, time of end tracheal catheter entry into the nostril, and lung collapse and surgical field score were measured. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were recorded while entering the operation room (T1), before intubation (T2), immediately after intubation (T3), 2 min after intubation (T4), and 10 min after intubation (T5). After surgery, all patients were followed for adverse reactions such as epistaxis, sore throat, hoarseness, and dysphagia.
All patients had a history of AS (20.4 ± 9.6 years). They had a Willson's score of 5 or above, grade III or IV Mallampati tests, an inter-incisor distance of 2.9 ± 0.3 cm, and a thyromental (T-M) distance of 4.8 ± 0.7 cm. The average pre-intubation preparation time was 20.4 ± 3.4 min, intubation time was 2.6 ± 0.4 min, facial grimace score was 1.7 ± 0.7, airway responsiveness score was 1.1 ± 0.7, and pulmonary collapse and surgical exposure score was 1.2 ± 0.4. The SBP, DBP, and HR at T5 were significantly lower than those at T1-T4 (P < 0.05). While the values at T1 were not significantly different from those at T2-T4 (P > 0.05), they were significantly different from those at T5 (P < 0.05). Seven patients had minor epistaxis during endotracheal intubation, two were followed 24 h after surgery with a mild sore throat, and two had hoarseness without dysphagia.
Patients with AS combined with severe cervical and thoracic kyphosis should be intubated using fiberoptic bronchoscopy under conscious sedation and topical anesthesia. Proper doses of penehyclidine hydrochloride, dexmedetomidine, fentanyl, and midazolam, combined with 2% lidocaine, administered prior to intubation, can provide satisfactory conditions for tracheal intubation while maintaining the comfort and safety of patients. BBs are safe and effective for one-lung ventilation in such patients during thoracotomy.
Core Tip: To summarize the drugs and their optimal doses for awake fiberoptic nasotracheal intubation in patients with ankylosing spondylitis (AS), and to evaluate the pulmonary isolation effect of one-lung ventilation with bronchial blocker, 12 AS patients complicated with lung or esophageal cancer underwent thoracotomy with a bronchial blocker. The final conclusion is that AS patients with severe cervical and thoracic kyphosis should be intubated by fiberoptic bronchoscopy under conscious sedation and topical anesthesia. Bronchial blocker is safe and effective for one-lung ventilation in such patients during thoracotomy.
- Citation: Yang SZ, Huang SS, Yi WB, Lv WW, Li L, Qi F. Awake fiberoptic intubation and use of bronchial blockers in ankylosing spondylitis patients. World J Clin Cases 2021; 9(23): 6705-6716
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6705.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6705
Ankylosing spondylitis (AS) is a type of autoimmune spondyloarthropathy characterized by chronic progressive exacerbation, with severe complications, such as hip fusion, spinal deformity, and spinal fracture, often occurring in the advanced stage. Severe kyphosis of the cervical spine and thoracic vertebrae often leads to cardiovascular and respiratory complications[1]. Patients at a later stage often require surgery to improve the inability to walk and quality of life, or if they have other diseases requiring surgical interventions. However, severe kyphosis can lead to difficulties in ventilation and intubation, posing a great challenge for anesthesiologists in perioperative management, especially that of the airway.
For adequate surgical site exposure and optimal visual field, thoracic surgery requires pulmonary isolation and one-lung ventilation. One-lung ventilation can be achieved using a double-lumen tube (DLT) or bronchial blocker (BB). Traditionally, a DLT is more commonly used, although the hardness and thick diameter of the pipe increase the risk of tracheal and bronchial damage[2]. However, DLT is being replaced in an increasing number of thoracic surgeries by BB, which has the advantage of allowing a simple, rapid, and less traumatic procedure with no need to change the tube, and can be used for all kinds of airways, especially in difficult ones[3].
Patients with severe kyphosis often have reduced cervical vertebra and atlantooccipital joint movement, difficulty opening the mouth, and cervical and thoracic vertebrae in fixed flexion positions, making tracheal intubation difficult. During airway management, the excessive extension may lead to cervical spine injury and fracture. Therefore, awake fiberoptic intubation is the safest option in these cases. For AS patients undergoing thoracic surgery, there have been few reports on one-lung ventilation with a BB after awake fiberoptic nasotracheal intubation. This study retrospectively analyzed the clinical data on 12 AS patients with spinal deformities who underwent awake fiberoptic nasotracheal intubation and one-lung ventilation with a BB. We have also summarized the airway management methods used for these patients.
Twelve patients with AS complicated with lung or esophageal cancer who underwent thoracic surgery under lung isolation with a BB at the Qilu Hospital of the Shandong University from January 2015 to August 2020 were included.
The inclusion criteria were: (1) Diagnosis of lung or esophageal cancer requiring surgical treatment; (2) Clear diagnosis of AS based on the American Society of Rheumatology as New York standard, which was revised in 1984[4]; and (3) Provided a signed agreement for the method of intubation and anesthesia. Patients (1) Excluded from other lung isolation methods or intubation failure; (2) With a history of drug abuse and mental illness; and (3) With masses inside the nasal cavity (e.g., polyps) and deviated nasal septum were excluded from the study.
The mean age of the 12 patients (11 men and one woman) was 57 (range, 41-68) years. They weighed 45-81 kg and had a body mass index (BMI) of 16.6-28.0. All the patients had a kyphotic deformity of the cervical and thoracic vertebrae and restricted mouth opening. They had physical status II or III as per the American Society of Anesthesiologists, with grade III or IV Mallampati airway, and Willson comprehensive score ≥ 5 points[5], but no cardiovascular or neuropsychiatric diseases.
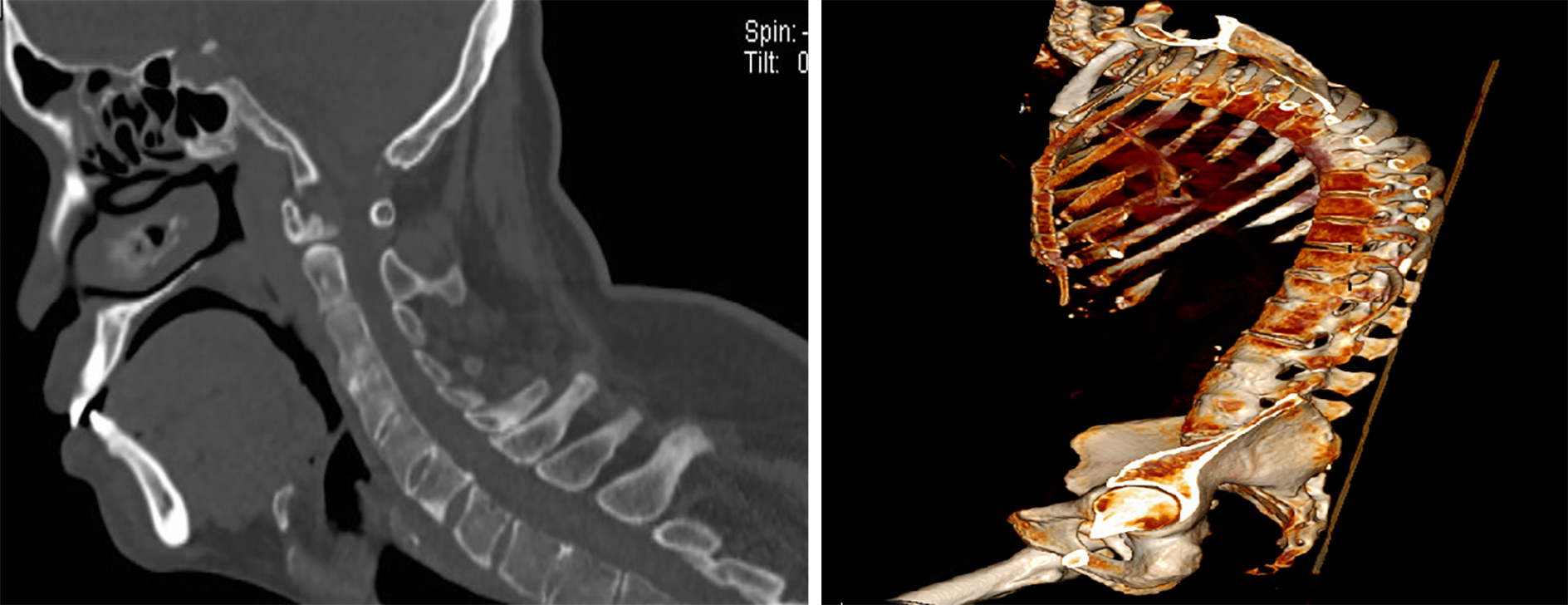
Preoperative airway evaluation and anesthesia were performed in all patients by the same anesthesiologist. The preoperative airway evaluation included the Mallampati test and measurement of the inter-incisor distance, thyromental distance, neck mobility, and Willson score (Figures 1 and 2). Following the airway assessment, 12 cases with difficult airways were identified according to the practice guidelines for the management of difficult airways established by the American Society of Anesthesiologists[6] and the Chinese Society of Anesthesiology. Fiberoptic nasotracheal intubation was performed under conscious sedation and topical anesthesia. All the patients fasted for 8 h and did not drink anything for 4 h before surgery. Before anesthesia, the patients received an intramuscular injection of 0.01 mg/kg penehyclidine hydrochloride. Peripheral venous access was established after entering the operation room, and blood pressure (BP), heart rate (HR), ECG, and oxygen saturation of blood were monitored. Oxygen was administered at 6 L/min via the mask, and a radial artery cannula was placed to monitor arterial BP, with an intravenous infusion of dexmedetomidine (0.5 μg/kg) for 10 min. Before surgery, nasal polyps and nasal septal deviations were excluded. The nasal cavity was selected to be patchier, and the nasal mucosal vessels were contracted using a 3% ephedrine hydrochloride cotton swab. A single-lumen endotracheal tube (ETT) 7.0-7.5 mm in diameter was selected, and the front surface was lubricated with sterile lidocaine cream. Due to the severe cervical and thoracic kyphosis, patients were intubated in the high semi-recumbent position with head and neck pads (Figures 3 and 4). Intravenous fentanyl (1 μg/kg) and midazolam (0.02 mg/kg) were administered before endotracheal intubation, requiring a Ramsay sedation score of 2-4 to avoid excessive sedation (Table 1).
| Drug | Usage and dosage |
| Penehyclidine hydrochloride injection | 0.01 mg/kg, intramuscular injection 30 min before anesthesia |
| Dexmedetomidine | Intravenous infusion of 0.5 μg/kg for 10 min |
| Ephedrine hydrochloride | 3%, nasal drops |
| 2% lidocaine | 3 mL for topical anesthesia of nasal mucosa and nasopharynx; 2 mL for thyrocricocentesis |
| Compound lidocaine cream | Lubrication on forepart of endotracheal tube and local anesthesia |
| Fentanyl | 1 μg/kg, analgesia, sedation, and inhibition of airway reflex |
| Midazolam | 0.02 mg/kg, sedation and anticonvulsant |
A fiberoptic bronchoscope (FOB) with a tip diameter of 3.1 mm was selected and operated by an anesthesiologist proficient in FOB intubation. The FOB was pushed slowly through the nasal cavity until the forepart reached the mid-trachea. The ETT was gently pushed along the trunk until its front end reached 3-4 cm from the carina. After successful intubation, the FOB was quickly removed.
During the operation, the patient's reactions were monitored. If the patients had no obvious symptoms such as nausea, cough, or painful facial grimace, the disappearance of vocal cord activity was observed under the FOB to indicate effective airway surface anesthesia. When the FOB and ETT entered the nostril, the facial grimace was scored, and airway responsiveness was scored when entering the trachea[7]. After successful tracheal intubation, intravenous induction was immediately performed. The patient was placed laterally with a Tappa 9FR BB within the ETT and FOB down for bronchial obstruction. After adjusting the insertion depth, the upper edge of the blocker cuff was placed below the bronchus carina. Pulmonary collapse and surgical exposure were evaluated and recorded intraoperatively, according to the method of Campos[8].
Perioperative clinical data, collected from the electronic medical records, included age, sex, BMI, history of AS, imaging findings, preoperative airway assessment, intubation time, patient reaction during intubation (facial grimace score, airway responsiveness, and comfort), pulmonary collapse and surgical exposure, and postoperative epistaxis, sore throat, hoarseness, dysphagia, and other adverse reactions.
Statistical analyses were performed using SPSS 24.0 (SPSS Inc., Chicago, IL, USA). The data are expressed as the mean ± SD, using ANOVA and paired t-test. Statistical significance was set at P < 0.05.
Table 2 summarizes the clinical data for the 12 patients. The patients had an average history of AS for 20.4 ± 9.6 years. They had a Willson's score of 5 or above, grade III or IV Mallampati tests, an inter-incisor distance of 2.9 ± 0.3 cm, and a thyromental (T-M) distance of 4.8 ± 0.7 cm (Table 3). All intubations were successful. The pre-intubation preparation time was 20.4 ± 3.4 min (including radial artery catheterization, sedation, nasopharyngeal topical anesthesia, nasal preparation, and thyrocricocentesis), and the intubation time was 2.6 ± 0.4 min (from the time of the entry of the FOB in the nose to the front end of the tracheal tube to the point 3-4 cm from the carina). The average facial grimace score was 1.7 ± 0.7, the airway responsiveness score was 1.1 ± 0.7 (Table 4), and the pulmonary collapse and surgical exposure score was 1.2 ± 0.4. T5 was the time point 10 min after intubation (after rapid intravenous drug induction). As shown in Table 5, systolic BP (SBP), diastolic BP (DBP), and HR at T5 were significantly lower than those at T1-T4 (P < 0.05). The values at T1 were not significantly different from those at T2-T4 (P > 0.05) but were significantly different from those atT5 (P < 0.05). Seven patients had minor epistaxis during endotracheal intubation, two had a mild sore throat and were followed for 24 h after surgery, and two had hoarseness without dysphagia (Table 6).
| Case | Gender | Age (yr) | Height (cm) | Weight (kg) | ASA physical status | Time since AS diagnosis (yr) |
| 1 | Male | 63 | 177 | 70 | III | 15 |
| 2 | Male | 59 | 165 | 72 | III | 20 |
| 3 | Male | 52 | 171 | 68 | III | 13 |
| 4 | Male | 41 | 170 | 48 | III | 9 |
| 5 | Male | 56 | 162 | 51 | III | 16 |
| 6 | Male | 68 | 166 | 61 | III | 22 |
| 7 | Male | 63 | 168 | 59 | III | 40 |
| 8 | Male | 61 | 155 | 45 | III | 30 |
| 9 | Male | 54 | 173 | 60 | III | 24 |
| 10 | Male | 60 | 165 | 55 | III | 18 |
| 11 | Female | 59 | 155 | 47 | III | 31 |
| 12 | Male | 43 | 170 | 81 | III | 7 |
| Case | Willson's score | Mallampati classification | Thyromental distance (cm) | Interincisor gap (cm) | Neck mobility (º) |
| 1 | 6 | III | 5.5 | 3.5 | < 90 |
| 2 | 5 | III | 4.5 | 3 | < 90 |
| 3 | 4 | III | 5.8 | 3.2 | < 90 |
| 4 | 5 | III | 6 | 3 | < 90 |
| 5 | 5 | III | 4.3 | 3 | < 90 |
| 6 | 6 | III | 3.8 | 2.5 | < 90 |
| 7 | 5 | IV | 4 | 2.4 | < 90 |
| 8 | 5 | IV | 5 | 3 | < 90 |
| 9 | 5 | III | 4.8 | 2.7 | < 90 |
| 10 | 5 | III | 4.5 | 2.5 | < 90 |
| 11 | 6 | IV | 4.2 | 2.6 | < 90 |
| 12 | 5 | III | 4.8 | 2.8 | < 90 |
| Case | Preparation time before intubation | Intubation time (min) | Scores of facial grimaces | Airway reactivity score |
| 1 | 25 | 3.3 | 2 | 2 |
| 2 | 18 | 2.5 | 1 | 1 |
| 3 | 22 | 3 | 2 | 1 |
| 4 | 27 | 2.7 | 1 | 0 |
| 5 | 15 | 3.1 | 1 | 1 |
| 6 | 19 | 2.6 | 2 | 1 |
| 7 | 20 | 2.2 | 1 | 1 |
| 8 | 23 | 1.9 | 2 | 2 |
| 9 | 18 | 2.1 | 2 | 1 |
| 10 | 21 | 2.6 | 1 | 0 |
| 11 | 20 | 2.8 | 3 | 2 |
| 12 | 17 | 2 | 2 | 1 |
| SBP/mmHg | DBP/mmHg | HR/min | |
| Number of cases | 12 | 12 | 12 |
| T1 | 136 ± 18 | 79 ± 12 | 87 ± 12 |
| T2 | 125 ± 13 | 77 ± 7 | 78 ± 13 |
| T3 | 136 ± 16 | 83 ± 8 | 92 ± 10 |
| T4 | 124 ± 10 | 76 ± 6 | 78 ± 9 |
| T5 | 108 ± 11 | 70 ± 7 | 67 ± 8 |
| Case | Pulmonary collapse and surgical exposure | Epistaxis | Sore throat | Hoarseness | Dysphagia |
| 1 | 1 | 1 | 0 | 0 | 0 |
| 2 | 1 | 0 | 0 | 0 | 0 |
| 3 | 1 | 0 | 0 | 0 | 0 |
| 4 | 1 | 1 | 0 | 0 | 0 |
| 5 | 2 | 1 | 0 | 0 | 0 |
| 6 | 1 | 0 | 0 | 0 | 0 |
| 7 | 2 | 0 | 0 | 0 | 0 |
| 8 | 1 | 1 | 1 | 0 | 0 |
| 9 | 1 | 0 | 0 | 1 | 0 |
| 10 | 1 | 1 | 0 | 0 | 0 |
| 11 | 1 | 1 | 1 | 1 | 0 |
| 12 | 1 | 1 | 0 | 0 | 0 |
AS is a common inflammatory rheumatic disease. The first symptoms occur before the age of 30 in 80% of patients and after the age of 45 in less than 5% of patients[9]. Patients with the disease lasting more than 20 years, especially men, often have spinal structure and function damage and even loss of mobility[10]. When the cervical vertebra is overextended due to tracheal intubation or pressure ventilation, the spine is prone to fracture, leading to cervical spinal cord injury[11]. Therefore, to keep the head and neck neutral, awake fiberoptic intubation is the safest option for these patients.
When nasotracheal intubation is performed, the nasal cavity should be pretreated before intubation. To this end, a cotton swab soaked in a mixture of 2% lidocaine and 3% ephedrine or 0.25% phenylephrine may be placed in the patient's nasal cavity[12]. Topical anesthesia of the larynx and lower airway must be administered through thyrocricocentesis, which provides better airway anesthesia and shortens the awake intubation time, but increases the risk of airway injury[13]. For patients with cervical fusion and fixation, thyrocricocentesis becomes complicated, and in these cases, atomization inhalation of lidocaine can be used for surface anesthesia of the lower airway.
Good airway suction and dryness are required for awake fiberoptic intubation. To achieve this, anticholinergic drugs may be administered before anesthesia, and secretions should be fully absorbed during intubation. Reducing oral secretions facilitates the absorption of local anesthetics during topical airway anesthesia. In addition, excessive secretion blocks the operator's vision and affects fiber optic intubation[14]. It is suggested that penehyclidine hydrochloride (0.01 mg/kg) be injected intramuscularly 30 min before the operation to inhibit salivary gland and airway gland secretions.
Patients with a difficult airway may undergo awake tracheal intubation (ATI). Rational drug sedation can reduce anxiety and discomfort in patients and increase their tolerance to the intubation process[15]. The most commonly used sedation solution is a combination of fentanyl (2 µg/kg) and midazolam (0.02 mg/kg), titrated according to the patient's needs[16]. Midazolam is used for sedation and prevention of seizures in cases of local anesthetic poisoning. Fentanyl inhibits airway reflexes, especially the cough response[14]. The cough reflex is an important factor affecting safe and smooth ATI and is an important indicator of the quality of awake fiberoptic intubation[17]. Sufentanil is difficult to titrate without excessive sedation and res
Compared with fentanyl, dexmedetomidine provides better intubation conditions, lower hemodynamic response, and higher patient tolerance and satisfaction[19,20]. Dexmedetomidine in the dose range of 0.2 to 0.7 µg/kg/h did not inhibit respiration and maintained SpO2 within the normal range[21]. We usually infuse a 0.5 µg/kg loading dose for 10 min for ATI, combined with fentanyl (1 µg/kg) and midazolam (0.02). This combination provides the appropriate sedation and comfort and is well tolerated.
The degree of sedation is measured using the Ramsay sedation classification or modified OAA/S score. Kundra et al[7] monitored the facial grimace and airway reactivity scores during ATI, which provided a better evaluation of patient sedation, comfort level, and intubation conditions compared to the Ramsay sedation grade and improved OAA/S score. During ATI, we often use a modified scale to evaluate patient response.
BB has great advantages in patients who need nasotracheal intubation or have abnormal airways requiring one-lung ventilation. It can be quickly inserted through the established single-lumen ETT during the operation, unlike the DLT, which is difficult to use in such cases. Moreover, in difficult airways, BB allows the placement of a single-lumen ETT using various techniques incompatible with DLT[22,23].
The 9.0 Fr Tappa BB is recommended for use in adults with a single-lumen ETT with an inner diameter of 8.0 or 8.5 mm. An ETT with an inner diameter of 7.0 mm and a vasoconstrictor can reduce epistaxis during nasal intubation. We found that epistaxis during nasotracheal intubation can be reduced by rotating the ETT less than 90° counterclockwise, so that the tip of the tube is located on the outer side of the nasal cavity. This may be related to the distribution and location of blood vessels in the nasal cavity.
In conclusion, accurate preoperative identification and evaluation are critical for DA. For AS patients with cervical and thoracic kyphosis deformities and difficulty opening their mouth, who need one-lung ventilation, awake fiberoptic nasotracheal intubation is the best option. Lidocaine (2%) combined with ephedrine (3%) is recommended for nasal cavity treatment. Penehyclidine hydrochloride injection before anesthesia can effectively reduce oral secretions during intubation. Intravenous infusion of dexmedetomidine, fentanyl, and midazolam before intubation can improve the intubation conditions and patient tolerance. Once the airway is established, a separate BB can be used for effective one-lung ventilation (Figure 5).
AS patients with severe cervical and thoracic kyphosis should be intubated by fiberoptic bronchoscopy under conscious sedation and topical anesthesia. Before intubation, proper dosage of penehyclidine hydrochloride, dexmedetomidine, fentanyl, and midazolam, combined with 2% lidocaine, can provide satisfactory tracheal intubation conditions while maintaining the comfort and safety of patients. Bronchial blocker is safe and effective for one-lung ventilation in such patients during thoracotomy.
Severe kyphosis is common in late stage of ankylosing spondylitis (AS), and tracheal intubation, especially one-lung ventilation, is particularly difficult. Such patients are rare, and have a predictable difficult airway. Awake fiberoptic intubation is the safest choice. Compared with double lumen bronchial catheter, the use of bronchial blocker for one-lung ventilation is particularly suitable for such patients. It is a great challenge for anesthesiologists to choose sedative drugs and methods to complete awake fiberoptic intubation while ensuring oxygenation.
Twelve cases of AS with spinal deformity were analyzed retrospectively to summarize the drug selection, appropriate dose, and patient tolerance of awake fiberoptic intubation, so as to provide guidance for clinical predictable awake fiberoptic intubation and one-lung ventilation in difficult airway.
To summarize the drug selection, appropriate dose, and patient tolerance of awake fiberoptic intubation.
The electronic case records were used to collect the general information of patients. Preoperative airway assessment of difficult airway (including Wilson's score, Mallampati classification, thermomental distance, interval gap, neck mobility, etc.) was performed. Appropriate doses of penehyclidine hydrochloride, dexmedetomidine, fentanyl and midazolam were given before intubation, and the nasal cavity was treated with a lidocaine and ephedrine cotton swab. The preparation time before tracheal intubation, intubation time, facial expression score, airway responsiveness score when fiberoptic bronchoscope was introduced, and airway responsiveness score when tracheal intubation entered the nostril were recorded. Lung collapse and surgical field score was recorded. Blood pressure and heart rate were recorded at different time points. The patients were followed for nasal bleeding, sore throat, hoarseness, dysphagia, etc.
Among the 12 patients, 11 were male and 1 was female; the history of AS was 20.4 ± 9.6 years, the Willson's scores were 5 or above, Mallampati tests were grade III or IV, the inter-incisor distance was 2.9 ± 0.3 cm, and the thyromental distance was 4.8 ± 0.7 cm. The preparation time before intubation was 20.4 ± 3.4 min, and the intubation time was 2.6 ± 0.4 min. The facial grimace score was 1.7 ± 0.7, the airway responsiveness score was 1.1 ± 0.7, and pulmonary collapse and surgical exposure score were 1.2 ± 0.4. The SBP, DBP, and HR at T5 were significantly lower than those at T1-T4 (P < 0.05). While the values at T1 were not significantly different from those at T2-T4 (P > 0.05), they were significantly different from those at T5 (P< 0.05). Seven patients had minor epistaxis during endotracheal intubation, two were followed 24 h after surgery with mild sore throat, and two had hoarseness without dysphagia.
Ankylose spondylitis patients with severe cervical and thoracic kyphosis should be intubated by fiberoptic bronchoscopy under conscious sedation and topical anesthesia. Before intubation, proper dosage of penehyclidine hydrochloride, dexmedetomidine, fentanyl, and midazolam, combined with 2% lidocaine, can provide satisfactory tracheal intubation conditions while maintaining the comfort and safety of patients. Bronchial blocker is safe and effective for one-lung ventilation in such patients during thoracotomy.
The Tampa bronchial blocker used in adults can pass through the endotracheal tube with the minimum inner diameter of 7.0, which leads to a larger inner diameter of the endotracheal tube selected for nasal intubation and higher incidence of epistaxis. The comfort of individual patients during intubation is slightly poor, so it is necessary to further explore the individualized use of sedative drugs. How to choose a more reasonable ventilation mode for patients with special difficult airway needs to be further explored.
Manuscript source: Unsolicited manuscript
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen ZH S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Li X
| 1. | Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, Haroon N, Borenstein D, Wang R, Biehl A, Fang MA, Louie G, Majithia V, Ng B, Bigham R, Pianin M, Shah AA, Sullivan N, Turgunbaev M, Oristaglio J, Turner A, Maksymowych WP, Caplan L. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019;71:1599-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 425] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 2. | Moritz A, Irouschek A, Birkholz T, Prottengeier J, Sirbu H, Schmidt J. The EZ-blocker for one-lung ventilation in patients undergoing thoracic surgery: clinical applications and experience in 100 cases in a routine clinical setting. J Cardiothorac Surg. 2018;13:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Müller SH, Defosse JM, Gerbershagen MU, Loop T. [Difficult Airway Management in Thoracic Anaesthesia]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2018;53:187-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27:361-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3782] [Cited by in RCA: 4116] [Article Influence: 100.4] [Reference Citation Analysis (1)] |
| 5. | Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 474] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 6. | Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, Benumof JL, Berry FA, Bode RH, Cheney FW, Guidry OF, Ovassapian A; American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1327] [Cited by in RCA: 1202] [Article Influence: 100.2] [Reference Citation Analysis (0)] |
| 7. | Kundra P, Kutralam S, Ravishankar M. Local anaesthesia for awake fibreoptic nasotracheal intubation. Acta Anaesthesiol Scand. 2000;44:511-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Campos JH, Kernstine KH. A comparison of a left-sided Broncho-Cath with the torque control blocker univent and the wire-guided blocker. Anesth Analg. 2003;96:283-289, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Feldtkeller E, Khan MA, van der Heijde D, van der Linden S, Braun J. Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis. Rheumatol Int. 2003;23:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 595] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 10. | Leone A, Marino M, Dell'Atti C, Zecchi V, Magarelli N, Colosimo C. Spinal fractures in patients with ankylosing spondylitis. Rheumatol Int. 2016;36:1335-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Rustagi T, Drazin D, Oner C, York J, Schroeder GD, Vaccaro AR, Oskouian RJ, Chapman JR. Fractures in Spinal Ankylosing Disorders: A Narrative Review of Disease and Injury Types, Treatment Techniques, and Outcomes. J Orthop Trauma. 2017;31 Suppl 4:S57-S74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 12. | Song J. A comparison of the effects of epinephrine and xylometazoline in decreasing nasal bleeding during nasotracheal intubation. J Dent Anesth Pain Med. 2017;17:281-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Malcharek MJ, Bartz M, Rogos B, Günther L, Sablotzki A, Gille J, Schneider G. Comparison of Enk Fibreoptic Atomizer with translaryngeal injection for topical anaesthesia for awake fibreoptic intubation in patients at risk of secondary cervical injury: A randomised controlled trial. Eur J Anaesthesiol. 2015;32:615-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Simmons ST, Schleich AR. Airway regional anesthesia for awake fiberoptic intubation. Reg Anesth Pain Med. 2002;27:180-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Johnston KD, Rai MR. Conscious sedation for awake fibreoptic intubation: a review of the literature. Can J Anaesth. 2013;60:584-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 16. | Yousuf A, Ahad B, Mir AH, Mir AW, Wani JG, Hussain SQ. Evaluation of Effectiveness of Dexmedetomidine and Fentanyl-midazolam Combination on Sedation and Safety during Awake Fiberoptic Intubation: A Randomized Comparative Study. Anesth Essays Res. 2017;11:998-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Vasu BK, Rajan S, Paul J, Kumar L. Efficacy of atomised local anaesthetic vs transtracheal topical anaesthesia for awake fibreoptic intubation. Indian J Anaesth. 2017;61:661-666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Puchner W, Egger P, Pühringer F, Löckinger A, Obwegeser J, Gombotz H. Evaluation of remifentanil as single drug for awake fiberoptic intubation. Acta Anaesthesiol Scand. 2002;46:350-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Chu KS, Wang FY, Hsu HT, Lu IC, Wang HM, Tsai CJ. The effectiveness of dexmedetomidine infusion for sedating oral cancer patients undergoing awake fibreoptic nasal intubation. Eur J Anaesthesiol. 2010;27:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Gnaneswaran HH, Jain G, Agarwal A, Chug A, Singla D. Optimal level of bispectral index for conscious sedation in awake fiberoptic nasotracheal intubation. J Oral Biol Craniofac Res. 2020;10:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Hogue CW Jr, Talke P, Stein PK, Richardson C, Domitrovich PP, Sessler DI. Autonomic nervous system responses during sedative infusions of dexmedetomidine. Anesthesiology. 2002;97:592-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Collins SR, Titus BJ, Campos JH, Blank RS. Lung Isolation in the Patient With a Difficult Airway. Anesth Analg. 2018;126:1968-1978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Granell M, Parra MJ, Jiménez MJ, Gallart L, Villalonga A, Valencia O, Unzueta MC, Planas A, Calvo JM. Review of difficult airway management in thoracic surgery. Rev Esp Anestesiol Reanim (Engl Ed). 2018;65:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |