Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6582
Peer-review started: February 2, 2021
First decision: March 16, 2021
Revised: March 28, 2021
Accepted: April 14, 2021
Article in press: April 14, 2021
Published online: August 16, 2021
Processing time: 183 Days and 20.4 Hours
The coronavirus disease 2019, which is caused by severe acute respiratory syndrome coronavirus 2, was first identified in December 2019 in Wuhan, China, and has since spread rapidly, evolving into a full-blown pandemic. We would like to report our experience after 1 year of this pandemic in the surgical service of a district hospital in Spain. There have been many changes (including new protocols) that our service and the hospital have undergone, to adapt to the new situation. We believe that this experience can be useful for other professionals who have lived and are living a similar situation.
Core Tip: The pandemic caused by the severe acute respiratory syndrome coronavirus 2 virus has created a complex, unexpected and uncertain situation that has gravely affected health systems, in Spain and worldwide, provoking significant stress among healthcare personnel. This article describes the experiences and reactions of the surgery service in a district hospital in southern Spain during the coronavirus disease 2019 pandemic, detailing the changes made to the daily routine in order to cope with this new situation.
- Citation: Pérez Lara FJ, Jimenez Martinez MB, Pozo Muñoz F, Fontalba Navas A, Garcia Cisneros R, Garcia Larrosa MJ, Garcia Delgado I, Callejon Gil MDM. COVID-19 pandemic, as experienced in the surgical service of a district hospital in Spain. World J Clin Cases 2021; 9(23): 6582-6590
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6582.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6582
The pandemic caused by the severe acute respiratory syndrome coronavirus 2 virus has created a complex, unexpected and uncertain situation that has gravely affected health systems, in Spain and worldwide, provoking significant stress among healthcare personnel. In this article, we describe how the crisis has affected the surgery service in a first-level hospital in southern Spain. We believe this information on how the hospital has adapted to cope with the problems described will be of great interest to comparable institutions.
As is well known, the outbreak was first detected in the Chinese city of Wuhan on December 31, 2019[1], when several cases of atypical pneumonia of unknown origin were diagnosed. Researchers concluded on January 7, 2020 that the infection was caused by a novel coronavirus, termed coronavirus disease 2019 (COVID-19). The disease evolved and spread to other countries. On March 11, 2020, the World Health Organization declared the situation to be one of global pandemic.
Although this situation is uncommon in modern times, the world has regularly suffered large-scale outbreaks of infectious disease throughout history, especially as the global population has grown and become increasingly urbanized. Since the first pandemics were documented, studies have shown that a major global pandemic takes place every 100-200 years.
Particularly deadly pandemics that have scourged humanity include the Plague of Justinian[2,3], which first hit Constantinople between 541 and 549 and then spread throughout the Roman Empire, killing millions; the Black Death[4-6], which ravaged Europe in the fourteenth century and caused the population to fall by two thirds; the smallpox outbreak of the eighteenth century[7], which infected and disfigured millions; and the so-called Spanish flu[8,9], after the end of the First World War, which killed 50 million people worldwide.
As we know, “Those who cannot remember the past are condemned to repeat it”. Pandemics recur periodically and should be prepared for. Nevertheless, to a large extent we were caught unawares, and the present crisis has caused immense harm—social, political, economic and, of course, to individual and collective health. In this paper, we address the latter concern, namely the impact of the pandemic on hospitals, and on the surgical service in particular, relaying our own experiences in this regard.
In the following sections, we discuss how the pandemic has affected each of the sectors in our hospital environment.
The crisis has obliged all medical personnel to make a series of changes, including heightened safety measures such as frequent hand washing, the constant disinfection of surfaces, placing hydroalcoholic gel dispensers in all areas of the hospital, not wearing rings, watches or street clothes (hospital gowns only), and using personal protective equipment (PPE) during all contacts with confirmed or suspected COVID-19 patients. The use of masks has been an issue of some controversy, regarding the most appropriate type. In this respect, we have followed the recommendations of the Center for Evidence-Based Medicine at the University of Oxford[10], according to which wherever aerosols may be generated the masks worn should be high-efficiency ones such as types N95, FFP2 or FFP3; otherwise, surgical masks are sufficient.
It is also important to determine the health status of hospital personnel themselves. All staff are periodically tested for COVID-19 contagion, not only for their own sake but also to ensure that no danger is posed to uninfected patients.
During the first, difficult stage of the pandemic (March to June 2020), the members of the surgical service worked in two non-overlapping groups. This policy was adopted in order to avoid the possible simultaneous contagion of the entire service. Furthermore, all staff meetings and committee sessions took place via online connections, using Circuit. This application was chosen to ensure compliance with data protection legislation, although it did require some training and time for the staff to become familiarized with its use.
Despite the precautions taken, the surgical service (ten persons) did experience one episode of contagion. However, it occurred not in the hospital itself, but during a trip to Madrid. This outcome, an infection rate of 10% in the service, is well below the 23% average that has been reported in Spain.
The COVID-19 crisis has also brought about many changes for our patients and their families, who have had to understand this new reality: The need to maintain social distancing, to be scrupulous about hand washing and to wear masks at all times. Moreover, only one visitor per patient is allowed. Patients are also given detailed information about the surgical procedure to be performed and the special circumstances involved, as follows.
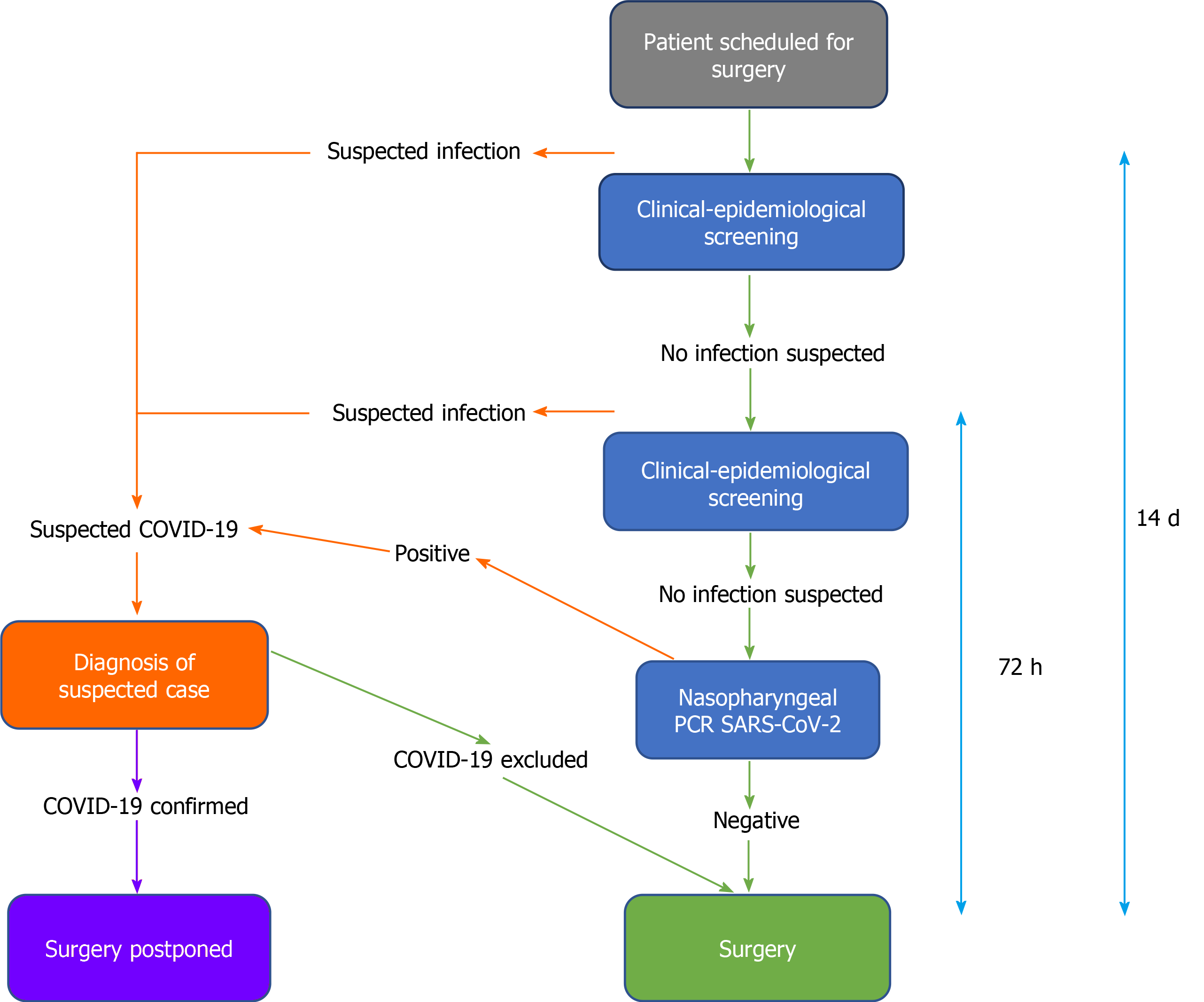
Before the intervention, a COVID-19 screening is performed, in accordance with the method recommended by the Spanish Association of Surgeons (AEC, Spanish initials)[11] (Figure 1). First, a clinical-epidemiological evaluation is conducted 14 d before the intervention. If the results are negative for COVID-19, a further evaluation is conducted 72 h before the intervention. If this, too, is negative, the final step is to perform a polymerase chain reaction (PCR) test. If this is negative, the intervention can proceed.
Apart from the possible presence of COVID-19 infection, it is also necessary to assess whether the intervention is advisable, in view of the added risks of the pandemic situation and, especially, considering the patient's present status. In this respect, we follow the AEC recommendations[12], which in turn are based on the guidelines of the American College of Surgeons. The approach taken is detailed in Table 1, which lists the 18 parameters considered, each of which is scored from 1-5 points. Thus, the total score possible ranges from 18-90 points. The lower the score, the greater the possibility of the intervention being approved. Higher scores indicate greater frailty and hence less aptitude for surgery during the COVID-19 pandemic. This scale has not yet been validated for use in Spain, and so the scores obtained and the surgical decisions thereby recommended are not considered conclusive, but merely indicative.
| 1 | 2 | 3 | 4 | 5 | |
| Effectiveness of conservativetreatment | None/not available | < 40% of that provided by surgery | 40%-60% of that provided by surgery | 60%-95% of that provided by surgery | Fully equivalent to that provided by surgery |
| Impact of a 2-wk delay on disease prognosis | Very severe worsening | Significant worsening | Moderate worsening | Slight worsening | No worsening |
| Impact of a 6-wk delay on disease prognosis | Very severe worsening | Significant worsening | Moderate worsening | Slight worsening | No worsening |
| Surgical time (min) | < 30 | 30-60 | 60-120 | 120-180 | > 180 |
| Average hospital stay | Minor surgery/major ambulatory surgery | < 24 h | 24-48 h | 3 d | > 4 d |
| Likelihood of need for ICU (%) | Unlikely | < 5 | 5-10 | 10-25 | > 25 |
| Blood required (cc) | < 100 | 100-250 | 250-500 | 500-750 | > 750 |
| Members of the surgical team | 1 | 2 | 3 | 4 | > 4 |
| Location of surgery | None of the following | Upper and lower abdomen, by laparoscopy | Lower abdomen, open surgery | Upper abdomen, open surgery | Head and neck, thorax, gastro-oesophageal complex |
| Age | < 20 | 20-40 | 40-50 | 50-65 | > 65 |
| Chronic lung pathology (COPD, asthma, cystic fibrosis) | No | Treatment on demand | Usual treatment | ||
| Obstructive sleep apnea syndrome | No | No treatment | Continuous positive airway pressure | ||
| Cardiovascular disease | No | 1 drug | 2 drugs | 3 drugs | |
| BMI (kg/m2) | < 25 | 25-30 | > 30 | ||
| Diabetes mellitustype 2 | No | No medication | Oral antidiabetic | + Insulin | |
| Immunosuppression | No | Moderate | Severe | ||
| Flu syndrome | No | Yes | |||
| Contact with COVID-19 in the last 15 d | No | Unknown | Yes |
The present crisis has had a major impact on scheduled surgical activity, in various ways. Perioperative mortality is greater among COVID-19 patients, and healthcare personnel are exposed to high risks of contagion during surgical and anesthetic procedures. Moreover, epidemiological conditions may vary and local resources are subject to limitations. Accordingly, the surgical program for oncological patients must be carefully considered. In this respect, the American College of Surgeons[13] recommends that decisions should be taken on a case-by-case basis. As commented above, in our hospital, the corresponding AEC score is determined, and oncological patients are evaluated according to their status and disease prognosis. As an example, during the most critical moments of the pandemic and due to lack of space in the intensive care unit (ICU), for some patients with cancer of the colon there was no alternative but to perform tumor resection without immediate reconstruction (i.e. temporary colostomy).
Another sensitive question is the type of surgery to be employed. At the outset of the pandemic, laparoscopy was said to pose a high risk of contagion, due to the release of contaminant gases. Later, it was observed in open surgery that when an electric scalpel is employed, this can provoke possibly contagious aerosolization in the digestive tract. Therefore, the least dangerous option appears to be constant pressure laparoscopy, with gas extraction through a virus filter[14]. Other measures that have been adopted in response to the COVID-19 crisis include: (1) The installation of an independent circuit for the COVID operating room, (2) Limiting the number of staff in the operating room, (3) Using disposable material whenever possible, (4) Keeping doors and separating screens closed, and (5) Using PPE.
At first, PPE was used with all patients (before virus-detection kits became available). When PCR testing became generalized, the equipment was used only for patients who tested positive.
The first protective equipment used was the traditional version, with an FFP2 mask, adjustable glasses and protective overalls. However, those who have used this equipment will know that it is very difficult to operate in these conditions for more than an hour at a time, since the glasses fog up continuously. Moreover, heat and dehydration are severe problems that also arise. To address these issues, we obtained equipment fitted with an air-recirculation system, composed of a motor with a virus filter. This system recycles the air within a transparent headset, thus protecting the wearer from infection, maintaining a transparent view and preventing the excessive accumulation of heat.
The patients considered most eligible for surgery, according to the current intensity of the pandemic, are assessed using the AEC-recommended scale[11] (Table 2), which sets out five scenarios, depending on the number of COVID-19 patients currently being treated, for ICU use, triage policies in emergency situations, resources available and surgical activity. Between March and June 2019, our hospital reached Scenario 3, during which only emergency interventions or those needed by cancer patients could be performed. At present, we are in Scenario 1 (almost normal) and therefore the surgical service is fully operational, for all types of patients.
| Scenario | I (almost normal) | II (initial alert) | III (moderate alert) | IV (high-level alert) | V (emergency) |
| % of hospital beds occupied by COVID-19 patients | < 5 | 5-25 | 25-50 | 50-75 | > 75 |
| Hospital resources | No impact | No impact, but precautionary reserve of resources | Some impact on resources, with precautionary reserve of beds | Some impact on resources and on healthcare personnel | Significant impact with limited access to beds and ventilatory support |
| Surgical activity | Normal | Emergencies, cancer pathologies and preferential benign pathologies | Emergencies and cancer pathologies for which a 3-mo delay would worsen the prognosis | Only emergencies | Only non-deferrable emergency attention. Status assessment by the hospital’s ethics committee |
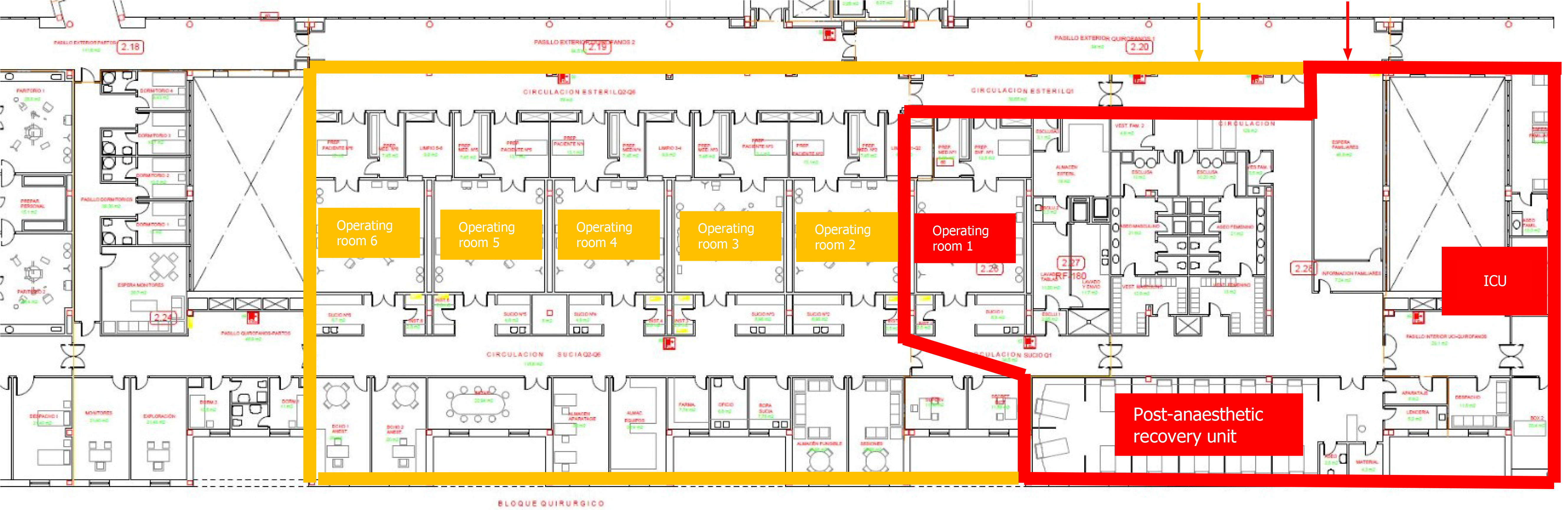
Finally, with regard to scheduled surgical activity, the following handicaps have been encountered. On the one hand, we have fewer operating rooms than before the crisis (since two were reserved for COVID-positive patients in the first stage of the pandemic and one is still reserved for this purpose), although the number of patients remains the same. In consequence, the waiting list has grown. In response, work has begun to create an additional operating room, but until it is available the demand will exceed our capacity.
In addition, as all patients must be given a PCR test before surgery, the result of which is only obtained on the day before the intervention, any patient whose result is positive leaves a gap that cannot be filled. In fact, this is a relatively minor concern, as the situation has only occurred twice during the entire period in question. However, the problem is more acute in the case of patients who for various reasons must be excluded from the schedule during the 4 d immediately prior to the expected date—and this situation arises more frequently. When this happens, it does not leave sufficient time to react and fill the gap (as contacting a new patient, scheduling the PCR test and obtaining the result takes more than 4 d).
A third problem is that the patients whose intervention was scheduled to take place after the initial March-June period tend to present more advanced pathologies, due to the delay in their treatment caused by the lengthening waiting list. In consequence, these interventions are more complex and so fewer patients can be treated per day (for example, in biliary pathology, where previously four gall bladder operations were performed in a surgical shift, now we may only complete two, because the patients often present with advanced cholecystitis, which requires greater attention and operating time). All these problems aggravate the situation, and will take time to resolve. Nevertheless, our first priority is to acknowledge their existence and the need to find a solution.
Regarding urgent surgical activity, in the present circumstances we have had to apply stricter criteria in selecting patients to be treated. Thus, processes that are usually dealt with surgically but which can be addressed via conservative treatment—as is the case of appendicitis, cholecystitis or other types of abdominal infection—are now being treated conservatively, with antibiotics, at least initially, so that the operating room can be reserved for essential interventions.
In addition, in recent months, and especially during the first 4 mo of the pandemic, the types of pathology being treated in the emergency department have varied considerably, with a very significant decrease in patients presenting trauma or inflammatory pathologies. Studies elsewhere have confirmed this pattern. Thus, the Waikato trauma center in New Zealand has reported a 43% reduction in abdominal trauma pathologies[15], while hospitals in the United States have reported significant decreases in inflammatory emergencies and in deaths from cerebrovascular and cardiovascular accidents[16]. In our own hospital, during the first 3 wk of the pandemic we operated on only two patients, when under normal conditions thirty would have been treated. In other words, the activity of the surgical department fell by 93%.
Among other indicative data, during the period March-June 2019, we attended 646 emergency consultations, while in the same period in 2020 there were only 197, a reduction of 70%.
We believe this pattern of reduced surgical activity can be explained as the logical consequence of the pandemic situation, with patients being afraid to come to the emergency room, for fear of infection. However, this reluctance to seek treatment has given rise to a significant increase in morbidity and mortality. For example, in a very short period of time we observed ten cases of appendicitis, three of which developed peritonitis, and two strangulated hernias that were already catastrophic and resulted in the patient’s death, as well as numerous cases of exacerbated inflammatory symptoms.
Finally, we emphasize the importance of making a differential diagnosis of coronavirus infection in patients with acute digestive symptoms. In 10% of cases, this is the initial sign of coronavirus infection. The differential diagnosis is usually performed by clinical analysis, since lymphopenia is present in 80% of such cases, and procalcitonin levels are low in 90% of these patients. Accordingly, these indications are of crucial importance in guiding our treatment approach[17].
At the beginning of the pandemic, normal face-to-face consultations were out of the question, and were replaced by telephone/video communications. These tasks were performed by two teams working independently, from home. The teams included the hospital surgeons, who received appropriate equipment and training. Thus, the necessary consultations were conducted remotely, and all proceedings were recorded in the hospital’s patient-care computer. Patients whose pathology absolutely required a physical evaluation were seen on Fridays, in a consultation with stringent safety measures (distancing, only one person per consultation, application of hand disinfectant, etc.).
This system was applied during the first 4 mo of the crisis, from March to June 2020. Later, physical consultations were gradually reinstated, with all possible safety measures. Moreover, the rate of consultations was increased by 30% to address the accumulated backlog.
One of the most important changes provoked by COVID-19 is that of the hospital infrastructure, which has required major adaptation. In our surgical area, for example, an independent COVID circuit has been created (Figure 2), with an operating room in which the usual positive-pressure ventilation has been inverted to create a slight negative pressure, of approximately two Pascals. Moreover, plasterboard partitions have been installed to isolate this operating room, as well as a postoperative recovery unit and an ICU, from the usual surgical area. To date, this isolation has functioned quite well.
The above changes meant there was one operating room fewer for normal scheduled activity, and so the management team rapidly decided to have a new one installed. It is now completed and ready for use.
Similarly, the Alerts and Emergencies room had suffered from problems of space, making it difficult to maintain two independent circuits (respiratory and non-respiratory). Therefore, the decision was taken to construct a 600 m2 additional facility, specifically for the respiratory circuit. In consequence, the problem is now completely resolved.
No modifications were needed for the area dedicated to consultations, because the waiting room there has an area of 120 m2, which is more than enough to achieve safe distancing between patients.
According to the recommendations of the Center for the Coordination of Health Alerts and Emergencies[18], the capacity of the ICU should be double that previously available, and space should be identified for three times as many beds as before, should the need arise. In our hospital, the ICU originally had seven beds. To address the present situation, the postoperative recovery unit has been re-purposed as an ICU, with 21 beds, thus tripling its capacity.
Broadly speaking, these are the main problems that we have had to face, and the measures adopted in response. However, we believe that in our environment, as in the business world, those with vision perceive not only problems but also great opportunities when a crisis strikes. Therefore, we must identify the fundamental elements of the issue and focus on obtaining a positive outcome. What positive aspects has the crisis produced? In the first place, we have acquired various new skills: Most of us have learned to work with webinars, telematic consultations and virtual sessions. These changes may well become permanent. Furthermore, the patients have learned to prioritize and to seek Alerts and Emergencies attention only for matters that are really urgent. This is a very positive outcome for the present; whether it will persist, only time will tell.
We have also learned to use isolation suits, which may be useful in specific situations in the future. Another important contribution is that the hospital infrastructure has been significantly improved, gaining 600 m2 in the emergency room and an additional operating room in the surgical area. Once the pandemic has ended, these improvements will remain. We hope to overcome the present crisis and to be strengthened by it, so that when this situation is only a memory, we shall remember the lessons learned and successfully address future challenges.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mohammadi M S-Editor: Gao CC L-Editor: Filipodia P-Editor: Li JH
| 1. | Lee A. Wuhan novel coronavirus (COVID-19): why global control is challenging? Public Health. 2020;179:A1-A2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 2. | Horgan J. Justinian’s Plague (541–542 CE). World Hist Encyclop 2014. |
| 3. | Sabbatani S, Manfredi R, Fiorino S. [The Justinian plague (part one)]. Infez Med. 2012;20:125-139. [PubMed] |
| 4. | The Editors of Encyclopaedia Britannica. Black death. Encyclopedia Britannica 2018. |
| 5. | DeWitte SN. Mortality risk and survival in the aftermath of the medieval Black Death. PLoS One. 2014;9:e96513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Benedictow OJ. The Black Death, 1346-1353: The Complete History. Woodbridge, Suffolk: Boydell Press, 2004.. |
| 7. | Henderson DA. The eradication of smallpox--an overview of the past, present, and future. Vaccine. 2011;29 Suppl 4:D7-D9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 8. | Flecknoe D, Charles Wakefield B, Simmons A. Plagues & wars: the 'Spanish Flu' pandemic as a lesson from history. Med Confl Surviv. 2018;34:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Almond D. Is the 1918 influenza pandemic over? Long-term effects of in utero influenza exposure in the post-1940 U.S. population. J Polit Econ 2006; 114: 672-712. |
| 10. | Greenhalgh T, Chan XH. What is the efficacy of standard face masks compared to respirator masks in preventing COVID-type respiratory illnesses in primary care staff? [Internet] [cited 9 January 2021]. Available from: https://www.cebm.net/covid-19/what-is-the-efficacy-of-standard-face-masks-compared-to-respirator-masks-in-preventing-covid-type-respiratory-illnesses-in-primary-care-staff/. |
| 11. | Arnal Velasco D, Morales-Conde S. Recomendaciones para la programación de cirugía en condiciones de seguridad durante el periodo de transición de la pandemia COVID-19 [Internet]. [cited 11 January 2021]. Available from: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/200517-DOCUMENTO_CIRUGIA-FINAL_(2).pdf. |
| 12. | Management recommendations for the return to normality and "de-escalation" in general surgery services in the context of the COVID 19 pandemic [Internet] Spanish Association of Surgeons (AEC) [cited 28 December 2020]. Available from: https://www.aecirujanos.es/files/noticias/152/documentos/Vuelta_a_la_normalidad(1).pdf. |
| 13. | COVID-19: Elective case triage guidelines for surgical care [Internet]. American College of Surgeons; updated 25 March 2020. [cited 11 November 2020]. Available from: https://www.facs.org/covid-19/clinical-guidance/elective-case. |
| 14. | Aranda-Narváez JM, Tallón-Aguilar L, Pareja-Ciuró F, Martín-Martín G, González-Sánchez AJ, Rey-Simó I, Tamayo-Medel G. Atención de la urgencia quirúrgica durante la pandemia COVID-19. Recomendaciones de la Asociación Española de Cirujanos. Cir Esp 2020; 98: 433-441. |
| 15. | Erratum for the Research Article "Recent global decline of CO2 fertilization effects on vegetation photosynthesis" by S. Wang, Y. Zhang, W. Ju, J. M. Chen, P. Ciais, A. Cescatti, J. Sardans, I. A. Janssens, M. Wu, J. A. Berry, E. Campbell, M. Fernández-Martínez, R. Alkama, S. Sitch, P. Friedlingstein, W. K. Smith, W. Yuan, W. He, D. Lombardozzi, M. Kautz, D. Zhu, S. Lienert, E. Kato, B. Poulter, T. G. M. Sanders, I. Krüger, R. Wang, N. Zeng, H. Tian, N. Vuichard, A. K. Jain, A. Wiltshire, V. Haverd, D. S. Goll, J. Peñuelas. Science. 2021;371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 577] [Cited by in RCA: 830] [Article Influence: 166.0] [Reference Citation Analysis (0)] |
| 17. | Soraya GV, Ulhaq ZS. Crucial laboratory parameters in COVID-19 diagnosis and prognosis: An updated meta-analysis. Med Clin (Barc). 2020;155:143-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 18. | COVID-19: health recommendations for the transition strategy [Internet]. Center for the Coordination of Health Alerts and Emergencies [cited 6 June 2020]. Available from: https://www.lavozdegalicia.es/default/2020/04/26/00171587897012028592596/Fichero/recomendaciones_transicion.pdf. |