Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6552
Peer-review started: April 9, 2021
First decision: April 23, 2021
Revised: May 2, 2021
Accepted: May 15, 2021
Article in press: May 15, 2021
Published online: August 6, 2021
Processing time: 109 Days and 13 Hours
Adrenal myelolipoma is a rare, benign, non-functioning mass that occurs in the adrenal gland. It is composed of an admixture of hematopoietic elements and mature adipose tissue, similar to bone marrow. Even at large sizes, adrenal myelolipomas are usually asymptomatic and often incidentally found by ultrasonography or computed tomography (CT) scan. This paper describes an unusual case of adrenal myelolipoma presenting as flank pain.
A 50-year-old male with severe right flank pain underwent a CT scan revealing a huge mass extending into the suprarenal space. The mass showed a fat component with retroperitoneal hemorrhage. The tumor was treated laparoscopically, and pathologic examination revealed features of myelolipoma originating from the adrenal gland.
Adrenal myelolipomas are generally asymptomatic and can be treated conservatively. However, rupture and hemorrhage of the tumor can cause symptoms requiring surgical removal.
Core Tip: Adrenal myelolipomas are rare, benign, non-functioning masses that are generally asymptomatic. They can be managed conservatively, but in symptomatic cases with rupture or hemorrhage, surgical removal may be required. This article presents a rare case of adrenal myelolipoma rupture requiring laparoscopic excision with a review of literature on this subject.
- Citation: Kim DS, Lee JW, Lee SH. Spontaneous rupture of adrenal myelolipoma as a cause of acute flank pain: A case report. World J Clin Cases 2021; 9(22): 6552-6556
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6552.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6552
Adrenal myelolipoma is a rare, benign, non-functioning mass of the adrenal gland. It is composed of an admixture of hematopoietic elements and mature adipose tissue, similar to the elements of the bone marrow[1]. The name myelolipoma was given to the tumor by Oberling[2] in 1929. Myelolipomas can occur at various sites, especially in the retroperitoneum, pelvis, mediastinum, and paravertebral region[3]. To our knowledge, very few cases of adrenal myelolipoma have been reported. Recently, we treated a complicated case of a ruptured huge adrenal myelolipoma. This paper discusses our experience and provides a short review of the literature.
A 50-year-old man visited the department of emergency medicine complaining of severe right flank pain.
He had no recent history of trauma or injuries to his abdomen or right flank. The pain had started a few hours before arriving at the emergency department and it could not be relieved with generic over-the-counter pain killers.
Review of the patient’s past medical history revealed nothing significant. He had no history of receiving any surgeries or medical procedures.
The patient could not remember any remarkable medical history of his parents and siblings.
On physical examination, he had severe tenderness at the right costovertebral angle. There was no discoloration of the skin and no traumatic wounds or lesions were observed. He described having a severe flank pain that he could not accurately localize. The pain had abruptly started a few hours ago and it had not subsided with medication. It was distinct from pain caused by ureteral stones, which would have been acute, colicky, and more responsive to analgesics. The patient’s vital signs were stable, though he was slightly tachycardic.
His hemoglobin level was normal and did not change after the first day. Although the computed tomography (CT) findings were consistent with adrenal myelolipoma, we assessed his hormone levels to rule out other hormonally active tumors, and all results were within normal limits.
CT scan showed a huge mass in the right suprarenal area, with fat components and retroperitoneal hemorrhage (Figure 1). It was approximately 9 cm with homogeneous adipose density that was not enhanced by contrast media. Hematoma formation due to retroperitoneal hemorrhage from the rupture was observed but no active bleeding or dye leakage was seen. Follow-up CT scan was performed one week later, and no definite change was observed compared to the initial scan.
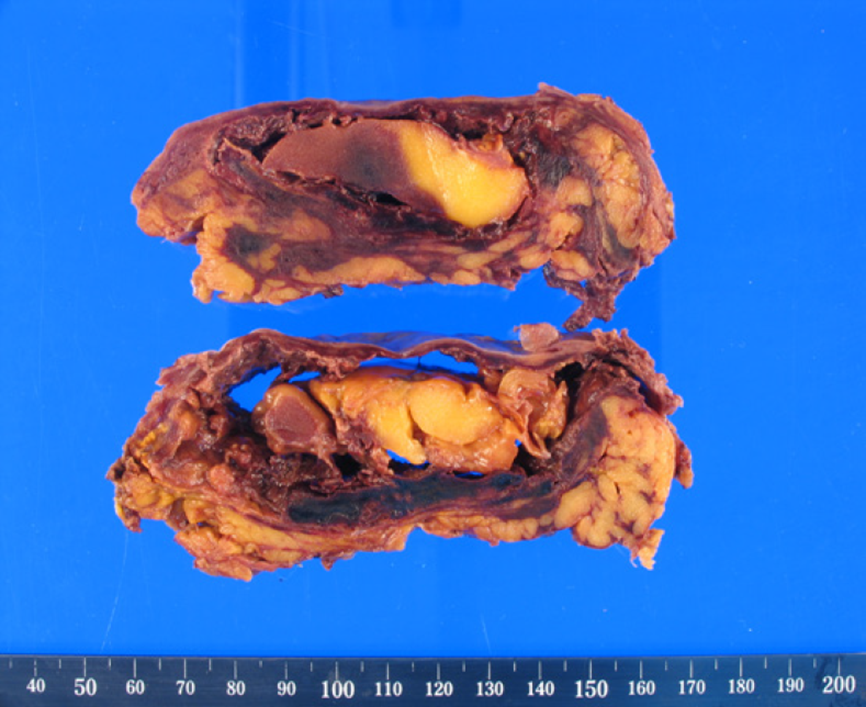
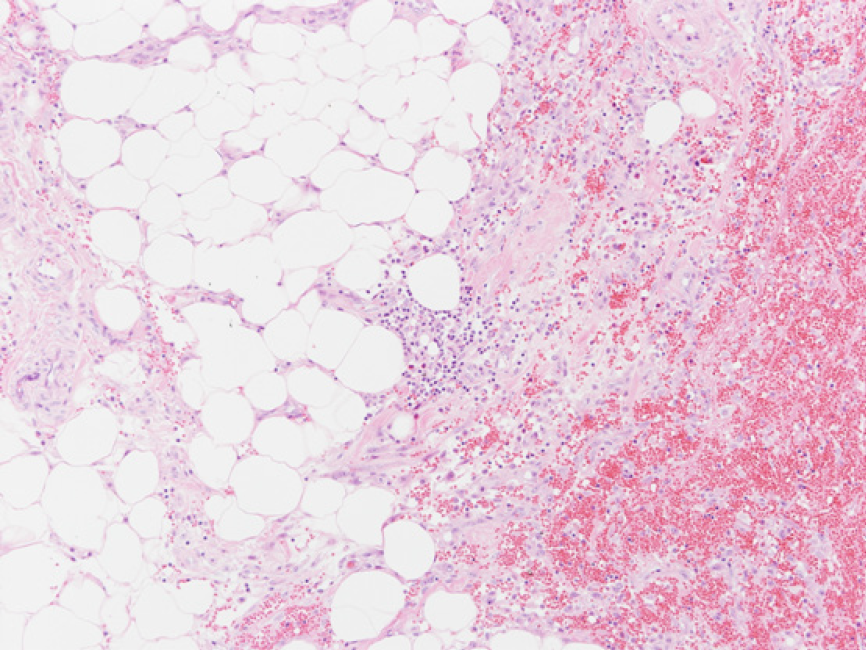
The final diagnosis of the patient was a ruptured right adrenal myelolipoma. Pathologic examination after surgery revealed the typical findings of an adrenal myelolipoma with hematoma (Figures 2 and 3) and confirmed our diagnosis.
After consulting with the patient, laparoscopic surgical excision was performed to remove the ruptured adrenal myelolipoma.
The patient recovered from surgery without complications and no other problems were observed during follow-up.
Knowledge of this tumor type remains suboptimal because of its rarity. There are multiple theories concerning the development and etiology of adrenal myelolipomas, including extramedullary hematopoiesis by autonomous proliferation of bone marrow cells transferred during embryogenesis, development from embryonic rests of primitive mesenchymal stem cells, embolism of bone marrow lodging in the adrenal gland, and adrenocortical cell metaplasia of the reticuloendothelial cells of blood capillaries in response to stimuli such as necrosis, infection, or stress[3].
Adrenal myelolipoma is most often an asymptomatic, benign, and hormonally inactive tumor[4-7]. Some studies have shown gender predilection, but there is no statistically significant difference in the incidence between males and females overall. The disease is usually unilateral, with preference for the right side[4,5]. Almost all detailed cases, except extremely huge tumors, were diagnosed by CT scan. Because of the high adipose character of the tumor, CT features are remarkable. The CT value is usually less than -30 Hounsfield units (HU) and is often as low as -100 HU[8]. On magnetic resonance imaging (MRI), the fatty component of this tumor is hyperintense on non-fat-suppressed T1-weighted images. The use of fat suppression can help confirm the diagnosis by demonstrating a loss of signal intensity within the fatty component. MRI is the most sensitive and specific modality for diagnosing adrenal hemorrhage[8]. Therefore, when adrenal myelolipoma is difficult to confirm with CT scan, MRI can provide useful information. However, tumors with minimal adipose tissue or hemorrhage can be more difficult to characterize. Although not usually required, fine needle aspiration (FNA) biopsy can confirm the diagnosis. Upon air-dried May-Grunwald-Giemsa staining, the FNA material reveals hematopoietic precursors including megakaryocytes, myeloid elements of varying stages of maturation, and fat vacuoles, with adrenal cortical cells in the background[9].
Despite numerous studies on adrenal myelolipomas, there is no universally accepted treatment to manage this tumor. Meyer and Behrend[6] concluded that patients with large, asymptomatic tumors greater than 10 cm should be treated surgically because of the risk of abdominal pain or life-threatening shock caused by spontaneous hemorrhage. Even in cases of small, asymptomatic, incidentally discovered adrenal lesions, some studies have recommended long-term follow-up because interval growth has been reported[10]. However, Han et al[11] insisted that not all tumors should be resected, and that almost none of the tumors grow. They decided to perform surgical resection only in the presence of symptoms, regardless of mass size. Even though each report reached different conclusions, resection of symptomatic adrenal myelolipomas is an acceptable treatment method.
The majority of adrenal myelolipomas is “silent” tumors with no hormonal activity; however, some cases with hormonal abnormality have been noted. Wagnerová et al[7] and Liu et al[12] reported cases of adrenal myelolipomas with hormonal activities. Therefore, patients diagnosed with adrenal myelolipomas on radiologic evaluation and who have other medical problems should be evaluated to detect abnormal hormonal activity.
Adrenal myelolipoma is generally a benign and non-functional tumor. If the tumor is asymptomatic and is characteristic on CT scan, it can be treated conservatively. However, if a patient presents with severe symptoms, the tumor must be removed surgically. Based on our experience, surgical intervention can be easily conducted with a laparoscopic approach, even when the tumor has caused hemorrhage.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Marickar F, Mu PY, Naem A S-Editor: Yan JP L-Editor: A P-Editor: Wang LL
| 1. | Gierke E. Uber Knochenmarksgewebe in der Nebenniere. Beitr Path Anat Supple. 1905;311. [DOI] [Full Text] |
| 2. | Oberling C. Les formations myelo-lipomateuses. Bull Assoc Fr Cancer. 1929;234. |
| 3. | Decmann Á, Perge P, Tóth M, Igaz P. Adrenal myelolipoma: a comprehensive review. Endocrine. 2018;59:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 4. | Bokhari MR, Zulfiqar H, Garla VV. Adrenal Myelolipoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2021. [PubMed] |
| 5. | Hsu SW, Shu K, Lee WC, Cheng YT, Chiang PH. Adrenal myelolipoma: a 10-year single-center experience and literature review. Kaohsiung J Med Sci. 2012;28:377-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Meyer A, Behrend M. Presentation and therapy of myelolipoma. Int J Urol. 2005;12:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Wagnerová H, Lazúrová I, Bober J, Sokol L, Zachar M. Adrenal myelolipoma. 6 cases and a review of the literature. Neoplasma. 2004;51:300-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Guo YK, Yang ZG, Li Y, Deng YP, Ma ES, Min PQ, Zhang XC. Uncommon adrenal masses: CT and MRI features with histopathologic correlation. Eur J Radiol. 2007;62:359-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Osborn M, Smith M, Senbanjo T, Crofton M, Robinson S, Rajan P. Adrenal myelolipoma - clinical, radiological and cytological findings: a case report. Cytopathology. 2002;13:242-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Gershuni VM, Bittner JG 4th, Moley JF, Brunt LM. Adrenal myelolipoma: operative indications and outcomes. J Laparoendosc Adv Surg Tech A. 2014;24:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Han M, Burnett AL, Fishman EK, Marshall FF. The natural history and treatment of adrenal myelolipoma. J Urol. 1997;157:1213-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Liu N, Zhang W, Tan J, Zhou J, Yu X, Ren N, Fang Z, Jiao W, Fan Y, Liu C. Adrenal myelolipoma with hyperandrogenemia and schizophrenia. Cancer Manag Res. 2018;10:177-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |