Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6515
Peer-review started: April 1, 2021
First decision: April 28, 2021
Revised: April 30, 2021
Accepted: May 7, 2021
Article in press: May 7, 2021
Published online: August 6, 2021
Processing time: 117 Days and 11.8 Hours
In critical care medicine, mesenteric ischemia (MI) is a life-threatening disease that can be present in both critically ill patients and those undergoing major surgery. For the first time, we report a case of concealed MI with a long course after knee arthroplasty.
A male patient underwent left total knee arthroplasty for gouty arthritis and developed a persistent fever and persistently high levels of serum infection markers after surgery. He was considered to have a periprosthetic site infection and treated with antibiotics and colchicine, periprosthetic debridement was performed, and the spacer was replaced, but no improvement was seen. At 54 d after arthroplasty, the patient developed gastrointestinal symptoms of nausea and vomiting, abdominal distention, and subsequently, cloudiness of consciousness, and hypotensive shock. Finally, the patient was diagnosed with ascending colonic mesentery ischemia with necrosis after laparotomy, which improved after right hemicolectomy.
Concealed MI without gastrointestinal symptoms after major surgery is rare and easily misdiagnosed. Orthopedic surgeons need to be aware of this complication.
Core Tip: We describe for the first time a case of concealed mesenteric ischemia (MI), a type of MI that lacks gastrointestinal signs and symptoms with fever as the only early symptom, which makes early diagnosis extremely difficult. MI often has a poor prognosis, and orthopedic surgeons must be aware of MI as a possible complication after total knee arthroplasty so that early diagnosis and intervention can be made for such concealed MI.
- Citation: Zhang SY, He BJ, Xu HH, Xiao MM, Zhang JJ, Tong PJ, Mao Q. Concealed mesenteric ischemia after total knee arthroplasty: A case report. World J Clin Cases 2021; 9(22): 6515-6521
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6515.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6515
Mesenteric ischemia (MI) is not uncommon in clinical practice and can be considered either acute or chronic[1]. Chronic MI, characterized by repeated transient blood flow disturbances in the intestine, is often associated with atherosclerotic disease[2]. Acute MI is usually caused by arterial or venous thromboembolism blocking the blood supply and needs to be considered when signs such as severe abdominal pain, nausea, and vomiting with elevated levels of inflammatory markers occur after major surgery[3]. Acute MI progresses rapidly and is associated with a mortality rate of 50% to 70%[4]. We report a case of concealed MI after total knee replacement with a course different from those of acute and chronic MI; fever was the only early symptom, making early diagnosis and intervention extremely difficult.
A 56-year-old male patient presented to our orthopedic outpatient clinic with swelling and pain in both knees with limited range of motion for more than 6 mo.
Six months ago, the patient presented with swelling and pain in both knees, especially in the left knee. The pain worsened over the past 6 mo, he was unable to stand and walk, and his activities were limited.
The patient had a history of gout for more than 10 years and hypertension for more than 20 years. The patient underwent heart valve replacement 9 years ago and took oral warfarin 1.875 mg once daily after surgery (coagulation was never monitored during treatment with the drug). He had a history of gastrointestinal bleeding. He denied having other major medical illnesses, such as diabetes, coronary heart disease, and kidney disease, and a history of infectious diseases, such as hepatitis and tuberculosis.
The patient had swelling and deformities in both knees, pressure pain around both knees, an elevated skin temperature, limited range of motion in both knees, and multiple swollen gout stones visible on both hands and both feet.
The patient’s blood uric acid level was 503 μmol/L. The international normalized ratio was 5.75.
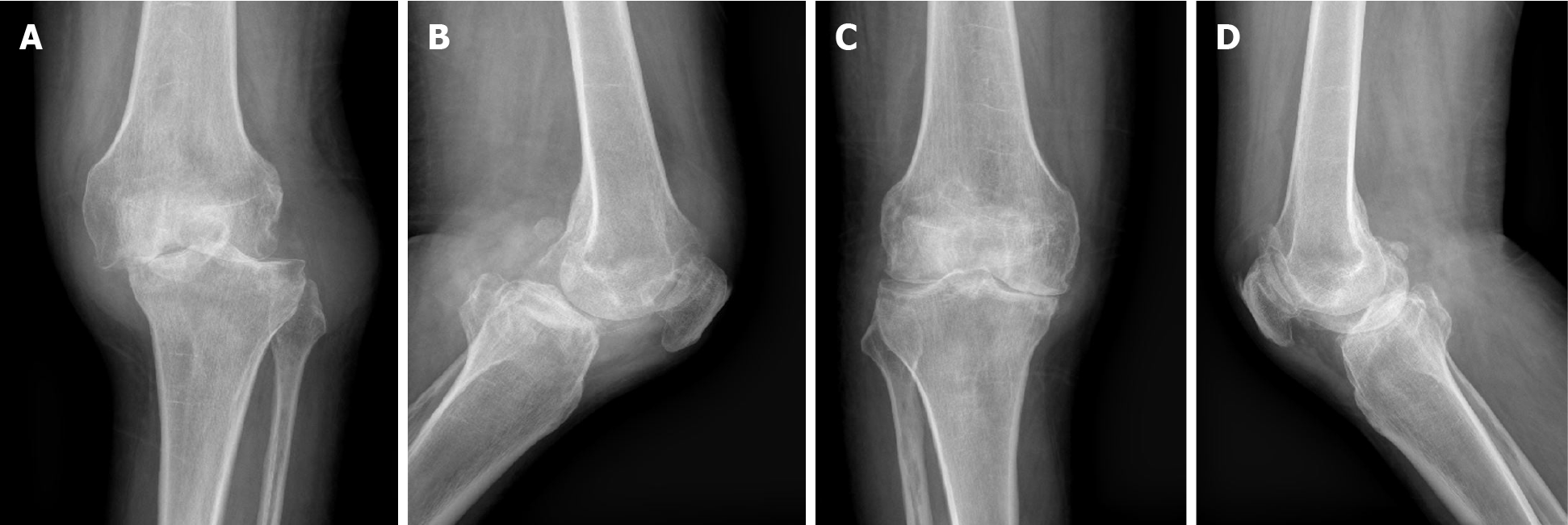
The patient’s X-ray examination showed gouty arthritis in both knees (Figure 1).
After multidisciplinary consultation, the patient underwent left-sided total knee arthroplasty because of relatively severe symptoms to regulate coagulation and renal insufficiency. Postoperative coagulation indicators showed that fibrinogen was 4.81 g/L, activated partial thromboplastin time was 43.7 s, and D-dimer was 4.7 mg/L FEU. The postoperative radiographs (Figure 2) showed good prosthesis alignment and good force lines in the lower extremities, and antibiotics anti-infection and low-molecular-weight heparin anticoagulation treatment were given postoperatively.
On the third day after surgery, the patient developed recurrent hyperthermia with a maximum temperature of 38.6 °C. The dressing on the surgical incision was dry and clean, there was no obvious bleeding or oozing from the incision, and the levels of blood flow and sensation in the left lower limb were normal. The procalcitonin, white blood cell (WBC), and C-reactive protein levels were consistently elevated, and the patient was considered to have a surgical site infection. He received anti-infection treatment for 48 d, during which the antibiotics were escalated several times and the patient was given anti-inflammatory treatment and pain relief, but there was still recurrent fever and elevated levels of inflammatory indexes.
The patient was considered to have a periprosthetic infection based on the recurrent elevated temperature and inflammatory indicator levels. We then performed a necrosectomy of the left knee joint, replaced the spacer, and performed vacuum sealing drainage. Intraoperatively, a large amount of white discharge and uric acid crystals were found in the knee joint, but no necrotic tissue or pus was observed. Three days later, the patient had a sudden onset of chest tightness and shortness of breath, nausea, and vomiting, with a temperature of 39 °C. Then the patient began to expe
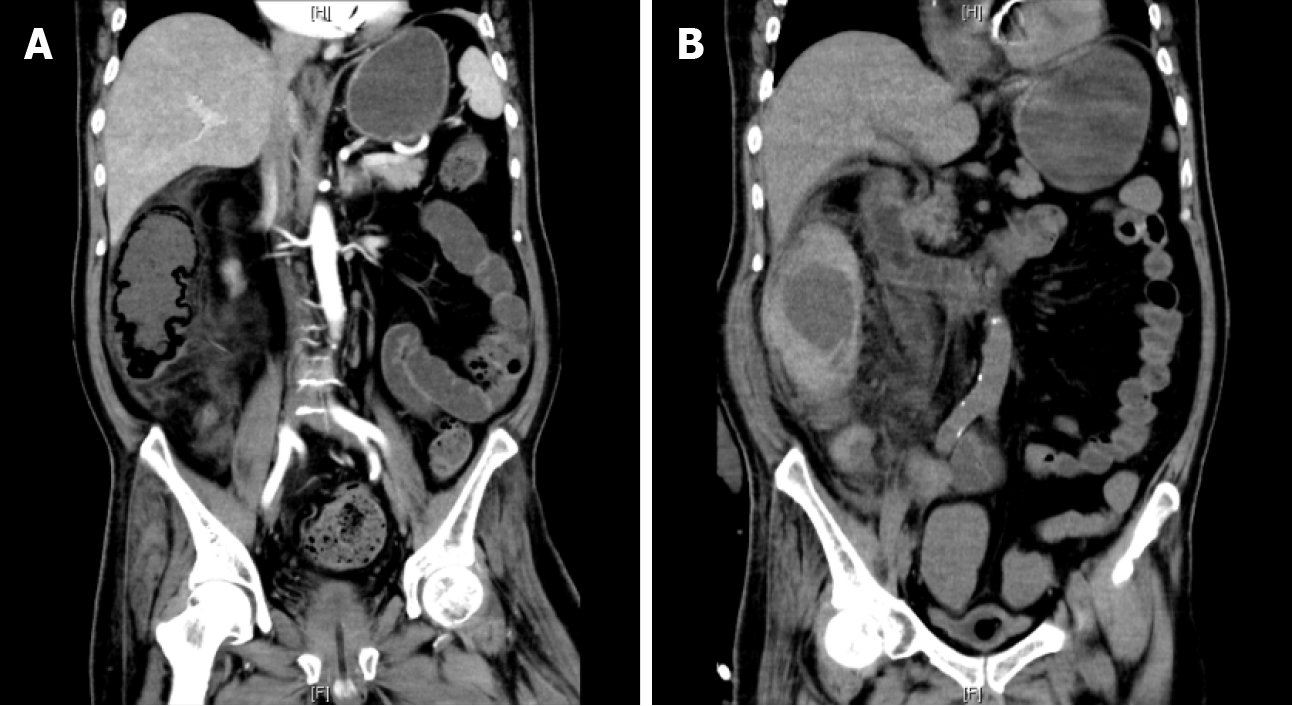
Abdominal computed tomography (CT) showed intestinal emphysema with fluid planes and exudative changes (Figure 3A). The patient was considered to have an abdominal infection with possible intestinal necrosis and obstruction, so we imme
Twenty-eight days later, the patient developed persistent right-sided abdominal pain, fever, and bloody exudate from the stoma, followed by bloody stools. The CT examination of the patient’s abdomen showed thickening of the wall of the ascending colon with multiple exudative changes around it and possible local hematoma (Figure 3B). He was transferred to the ICU again and was treated with anti-infection treatment, fluid resuscitation, and coagulation correction. The symptoms did not improve, the fever and abdominal pain were recurrent, and the inflammatory indexes did not decrease, so after his family provided permission, laparotomy was performed again due to aggravated infection.
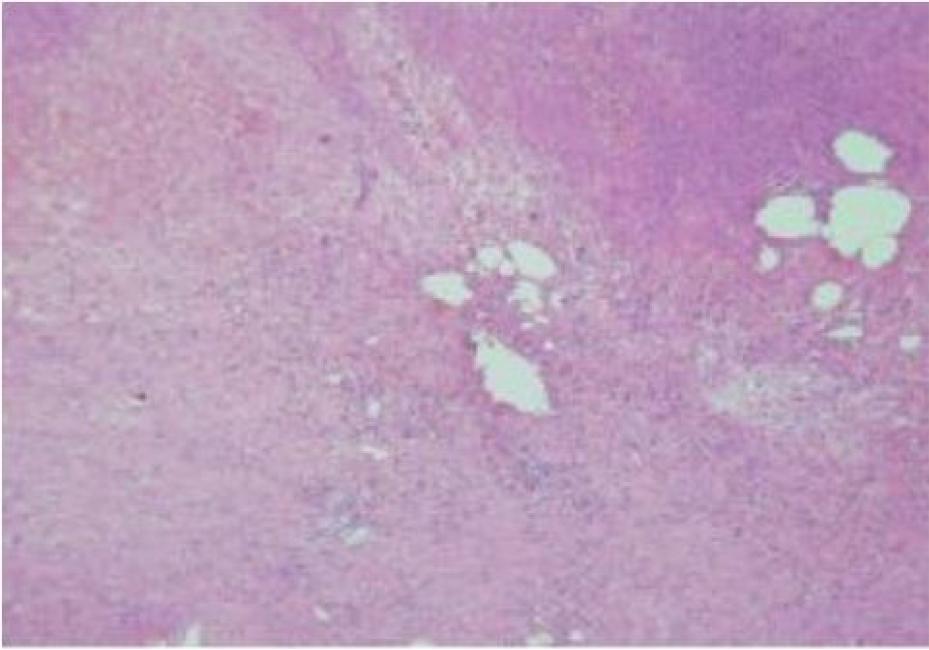
Forty-two days after the first abdominal surgery, we performed laparotomy, intestinal adhesion release, and right hemicolectomy. Intraoperatively, we found congested and edematous thickening of the ascending colon, hemorrhagic exudation of the prerenal fascia, inflammatory changes in the intestinal wall mucosa, and significant local intestinal adhesions; right hemicolectomy was performed, and a pathological exami
The patient was diagnosed with MI after total knee arthroplasty.
After total knee arthroplasty for gouty arthritis, the patient underwent knee de
After the second abdominal surgery with symptomatic treatment, such as anti-infection and rehydration treatment, the patient’s mesenteric ischemic symptoms disappeared, the gastrointestinal function returned to normal, and the patient was eventually discharged from the hospital. The patient returned to the hospital 3 mo after discharge for ileostomy closure.
Since early intervention is crucial for the prognosis of MI, MI needs to be diagnosed early, which can be challenging[5]. When MI is suspected to exist, it can usually be diagnosed on the basis of gastrointestinal signs and symptoms combined with ischemic changes such as exudate and thickening of the intestinal wall on abdominal and bowel CT scans or direct vascular computed tomography angiography (CTA) scans in response to vascular blood flow[6,7]. It is also important to note that other diseases such as appendicitis, gastroduodenal perforation, and acute pancreatitis still need to be ruled out when MI is complicated by acute abdominal conditions such as vomiting of coffee-like contents, bloody stools, or signs of peritoneal irritation. However, in MI cases without gastrointestinal symptoms after major orthopedic surgery, such as that described in this study after total knee replacement, it is difficult to diagnose MI on the basis of only signs of fever and elevated levels of infection markers; these signs are often attributed to prosthetic infection, which is often of utmost concern to orthopedic surgeons postoperatively. When anti-infective treatment is administered for a long period and considered ineffective, it is clear that the period for early intervention has been missed, leading to the development of terminal bowel necrosis. The prognosis after intestinal necrosis is extremely poor, with a high mortality rate[8], but fortunately, with timely surgery and aggressive anti-infective and fluid resuscitation treatment, the patient avoided a worse outcome.
We also did not perform angiography or vascular CTA, and the mechanism of MI in this patient is not clear. We speculate that postoperative thrombosis formed but probably did not involve the macrovascular and major arteries, such as the superior mesenteric artery, because thrombosis in these locations causes ischemic symptoms that are often acute and severe, such as intense spasmodic abdominal pain[3]. Although venous MI is associated with a lower mortality rate than arterial MI, more than one-third of patients require interventions other than anticoagulation[9]. Al
This rare type of concealed MI progresses slowly with an early symptom of fever only, unlike acute mesenteric ischemia and chronic mesenteric ischemia, where abdominal pain is the initial symptom[10], and it is worth thinking about how to make an early diagnosis. In this case, the patient’s only early sign was fever. Considering that the patient had a history of heart valve replacement and abnormal coagulation function, there was a possibility of thromboembolism, and previous studies have shown that an elevated WBC count is a risk factor for MI progression[11,12]. After excluding blood flow disorders in the lower extremities and heart, MI is one of the complications after major surgery that needs to be considered. When patients with coagulation abnormalities present with postoperative fever, abdominal CT should also be performed routinely in the postoperative investigation.
In general, MI progresses rapidly and has a poor prognosis. When elevated levels of inflammatory markers such as WBC are present after major orthopedic surgery without obvious signs of infection around the surgical area, this complication needs to be considered promptly, even in the absence of obvious gastrointestinal symptoms so that early intervention can be performed.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bairwa BL S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Yuan YY
| 1. | Zientara A, Domenghino AR, Schwegler I, Bruijnen H, Schnider A, Weber M, Gutknecht S, Attigah N. Interdisciplinary approach in emergency revascularization and treatment for acute mesenteric ischemia. BMC Surg. 2021;21:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Clair DG, Beach JM. Mesenteric Ischemia. N Engl J Med. 2016;374:959-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 329] [Article Influence: 36.6] [Reference Citation Analysis (1)] |
| 3. | Kühn F, Schiergens TS, Klar E. Acute Mesenteric Ischemia. Visc Med. 2020;36:256-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Luther B, Mamopoulos A, Lehmann C, Klar E. The Ongoing Challenge of Acute Mesenteric Ischemia. Visc Med. 2018;34:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Selim M, Alnaimi MI, Alsadah ZY, AlHarbi GA, Nasr M. Different Treatment Modality in the Management of Acute Mesenteric Ischemia. Cureus. 2021;13:e12490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Sinha D, Kale S, Kundaragi NG, Sharma S. Mesenteric ischemia: a radiologic perspective. Abdom Radiol (NY). 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Klar E, Rahmanian PB, Bücker A, Hauenstein K, Jauch KW, Luther B. Acute mesenteric ischemia: a vascular emergency. Dtsch Arztebl Int. 2012;109:249-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Artamonova ZA, Namokonov EV. [New laboratory parameters in the diagnosis of acute mesenteric ischemia. Klin Lab Diagn. 2019;64:490-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Feldman ZM, Wang LJ, Chou EL, Latz CA, Sumpio BJ, Eagleton MJ, Conrad MF. Venous mesenteric ischemia carries high procedural burden and elevated mortality in patients with severe presentation. J Vasc Surg Venous Lymphat Disord. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Strait A, Gasper W, Dhaliwal G. The Resolution of Abdominal Pain: an Ominous Sign of Mesenteric Ischemia. J Gen Intern Med. 2021;36:216-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Zhao H, Meng Y, Zhang P, Zhang Q, Wang F, Li Y. Predictors and risk factors for intestinal necrosis in patients with mesenteric ischemia. Ann Transl Med. 2021;9:337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Derikx JP, Schellekens DH, Acosta S. Serological markers for human intestinal ischemia: A systematic review. Best Pract Res Clin Gastroenterol. 2017;31:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |