Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6510
Peer-review started: April 1, 2021
First decision: April 28, 2021
Revised: May 11, 2021
Accepted: May 15, 2021
Article in press: May 15, 2021
Published online: August 6, 2021
Processing time: 117 Days and 23.7 Hours
Abdominal hemorrhage is a complication of peritoneal dialysis catheter (PDC) insertion that cannot be neglected, and its causes are mainly related to surgical injury. This article reports a case of massive abdominal hemorrhage that was caused by a rare rupture of corpus luteum shortly after PDC during the initiation of peritoneal dialysis (PD) insertion.
A 37-year-old woman was surgically placed a Tenckhoff catheter because of end-stage renal disease. On the third postoperative day, the color of the abdominal drainage fluid was pink, and deepened gradually. It turned pale after initiating conservative treatment. On the tenth postoperative day, the color of the abdominal drainage fluid suddenly turned dark red, and the color progressively deepened. The patient’s hemoglobin dropped from 88 g/L to 57 g/L. Abdominal computed tomography (CT) indicated abdominal effusion and a high-density shadow in the abdominal cavity. The surgeon performed a laparotomy and found that the corpus luteum had ruptured on the right side and a left ovarian blood body had formed. The gynecologist repaired the ovary and performed a bilateral oophoroplasty. After the operation, the patient stopped bleeding and hemo
If abdominal hemorrhage occurs in women of childbearing age after PDC inser
Core Tip: This article presents a rare case of abdominal hemorrhage during the induction of peritoneal dialysis (PD) shortly after PD catheter (PDC) insertion. Rupture of the corpus luteum was found to be the cause. We suggested that rare causes such as luteal rupture should be considered when abdominal hemorrhage occurs after PDC insertion, especially in women of childbearing age. Abdominal hemorrhage is difficult to control. and it is very important to understand the indications for exploratory laparotomy when progressive massive abdominal hemorrhage occurs after PDC insertion and conventional treatment is ineffective.
- Citation: Gan LW, Li QC, Yu ZL, Zhang LL, Liu Q, Li Y, Ou ST. Abdominal hemorrhage after peritoneal dialysis catheter insertion: A rare cause of luteal rupture: A case report. World J Clin Cases 2021; 9(22): 6510-6514
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6510.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6510
Abdominal hemorrhage is a complication of peritoneal dialysis catheter (PDC) insertion that cannot be neglected. Its common causes include intraoperative hemorrhage, catheter injury, rupture of abdominal organs, and abnormal coagulation function. Here, we present a case of abdominal hemorrhage during the induction of peritoneal dialysis (PD) shortly after PDC insertion in which a rare cause of rupture of the corpus luteum was found.
The patient was a 37-year-old woman who was admitted to the hospital because of end-stage renal disease. She wanted to receive PD treatment.
Ten months previously, the patient was diagnosed with chronic kidney disease. Her kidney disease progressed gradually.
The patient reported that she had suffered from thrombocytopenia for more than 10 years. As she refused bone marrow biopsy, the cause was unknown. She received conservative therapy because she had no obvious bleeding tendency. Her platelet level was maintained at approximately 70 × 109/L.
Her last menstrual period was on June 29, 2019, 10 d before PDC insertion.
The patient’s temperature was 36.5ºC, her heart rate was 86 bpm, respiratory rate was 15 breaths per minute, blood pressure was 133/98 mmHg, and oxygen saturation in room air was 99%. The patient had slight bilateral symmetrical dorsal pitting edema of the feet. No other positive signs were found on physical examination.
Blood analysis showed that hemoglobin was 88 g/L, the platelet count was 74 × 109/L, serum creatinine was 803.3 mmol/L, and the glomerular filtration rate was 5.1 mL/min. Urinalysis was 2+ in both protein and occult blood. Both Liver function and blood coagulation tests were normal.
Color Doppler showed bilateral kidney atrophy.
A Tenckhoff catheter was surgically placed on July 10, 2019, and after successful insertion, the patient received routine hemostatic therapy with etamsylate injection. On the third postoperative day, we initiated PD fluid for abdominal flushing and found that it was pink, with 2520 × 106 erythrocytes/L in the rinse solution. Because the bleeding was slight, we did not administer any specific treatment. The patient was started on automated PD on the fourth postoperative day. The drainage liquid was still pink, the erythrocyte number rose to 12460 × 106/L, the hemoglobin dropped from 88 g/L to 74 g/L, and the platelet count was 74 × 109/L. We considered that this may have been caused by small-vessel hemorrhaging in the abdominal cavity, and administered intravenous hemagglutinase to strengthen the hemostatic treatment and continued the PD. The color of the drainage fluid did not change significantly. On the sixth postoperative day, the patient began to complain of dizziness and fatigue, and the color of the drainage liquid became bright red. The erythrocyte number in the rinse solution increased to 53900 × 106/L, the hemoglobin dropped to 69 g/L, the platelet count was 77 × 109/L, fibrinogen degradation products were 66.27 µg/mL and D-dimer was > 20 µg/mL. We considered that this may have been caused by active small-vessel hemorrhaging and acquired coagulation dysfunction in the abdominal omentum. We administered 200 mL fresh frozen plasma, 1.5 units of red blood cells, and 50 U cryoprecipitate. After treatment, the patient’s symptoms were improved and the color of the dialysis solution gradually became pale. The erythrocyte number in the rinse solution dropped to 240 × 106/L, the hemoglobin level increased to 72 g/L, the platelet count was 51 × 109/L, and disseminated intravascular coagulation improved. On the tenth postoperative day, the color of the PD fluid suddenly became dark red. Microscopic examination found that the erythrocyte number of the rinse solution had reached the upper limit of detection, the hemoglobin dropped to 57 g/L, and the platelet count was 49 × 109/L. After multidisciplinary consultation with the de
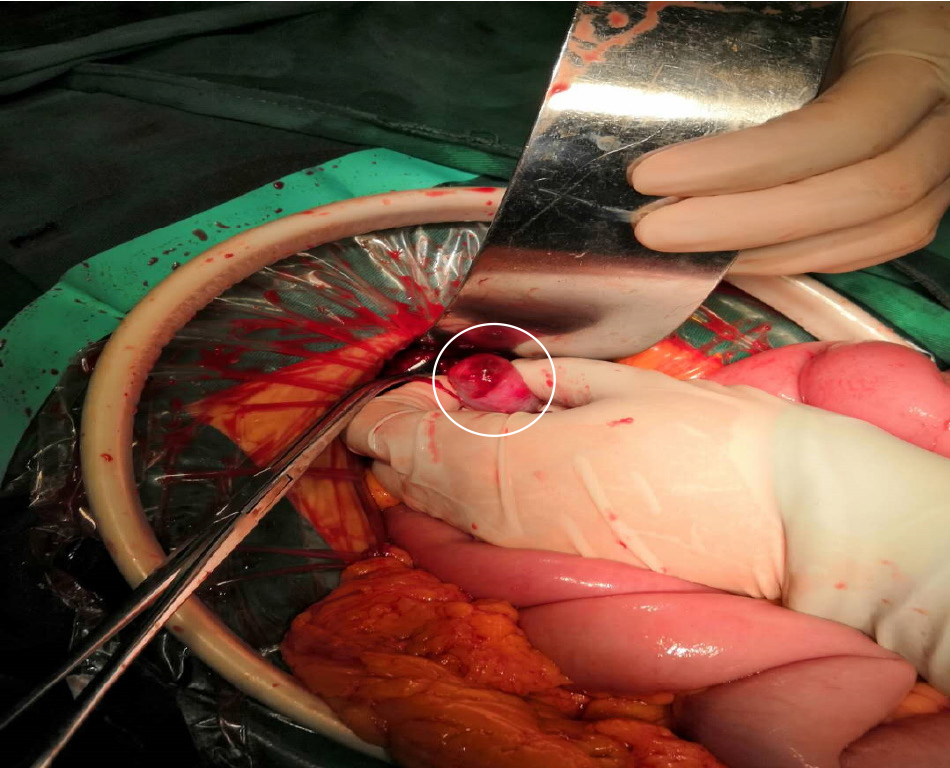
Angiography of the abdominal aorta, right superior epigastric artery, right internal thoracic artery, and mesenteric artery did not find any bleeding sites. A laparotomy found that the bleeding volume was approximately 500 mL and removed an approximately 500 g blood clot. After careful exploration, the laparotomy found that the corpus luteum had ruptured on the right side and that a left ovarian blood body had formed (Figure 1). The gynecologist repaired the ovary and performed a bilateral oophoroplasty.
After the operation, the bleeding stopped. The patient was temporarily transferred for hemodialysis and resumed PD after half a month. Her condition improved, and she was discharged 14 d after the laparotomy.
There are many complications of PDC insertion. Bleeding is one of the most common complications, and estimates of the incidence of bleeding events range from 0% to 7.5% because of different study criteria, with PDC insertion performed by open surgery[1-6]. Abdominal hemorrhage after PDC insertion is a potentially serious complication, but the incidence shortly after PDC insertion has not been clearly reported.
In uremia patients, platelet function is defective[7], with enhanced platelet apoptosis[8] that leads to platelet dysfunction. In addition, coagulation disorders in uremia patients caused by dysfunction of clotting factors II, VII, IX, and X leads to bleeding tendency. In this case, the patient developed an abdominal hemorrhage shortly after PDC insertion, but the bleeding volume was low. The main reasons were considered to be related to surgical injury and uremia-related coagulation dysfunction. The patient’s abdominal hemorrhage improved with conservative medical treatment for a time, but she experienced a sudden exacerbation of abdominal hemorrhage that did not respond to treatment. The bleeding was difficult to control and no bleeding site was found by angiography. An exploratory laparotomy found that the cause of the second abdo
Luteal cyst rupture is a cause of hemorrhage and is not uncommon in women of childbearing age. Massive hemorrhage may lead to circulation failure or even death[9]. A number of factors can lead to luteal rupture, such as spontaneous luteal rupture caused by increased intraluminal pressure[10], abnormal coagulation function caused by excess anticoagulant activity, lack of coagulation factors[10-13], increased external force during sexual intercourse, strenuous exercise, and increased intraperitoneal pressure from forced stools and coughing. There have also been reports of luteal rupture during pregnancy[14]. Luteal rupture has also been reported in patients with thrombocytopenia[15,16]. There has been a report of primary malfunction of a PDC as a cause of encasement in a hemorrhagic corpus luteum[17]. However, there have been no reports of luteal rupture during the induction of PD shortly after PDC insertion. We speculated that the cause of the luteal rupture in the patient was related to coagulation dysfunction and uremic thrombocytopenia itself. PD fluid perfusion might have also increased abdominal pressure. Hemorrhage from a luteal rupture occurring after PDC insertion is sometimes difficult to distinguish from hemorrhage caused by surgical injury. Fortunately, a timely exploratory laparotomy was performed, and the cause of the abdominal hemorrhage was finally determined. It is necessary to carefully observe the clinical symptoms and signs and the color of the abdominal drainage fluid after PDC insertion and to monitor changes in the blood hemoglobin and red blood cell count of the abdominal flushing fluid. If an abdominal hemorrhage is difficult to control, some rare causes should be considered, especially in women of childbearing age, such as luteal rupture, endometriosis[18], and ruptured ectopic pregnancy[19].
In conclusion, massive abdominal hemorrhage after PDC insertion is a rare and serious complication. Some rare causes as well as common causes such as surgical injury should be excluded. It is very important to understand the indications for exploratory laparotomy if progressive massive abdominal hemorrhage occurs after PDC insertion and conventional treatment is ineffective.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mizuno M S-Editor: Yan JP L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Mital S, Fried LF, Piraino B. Bleeding complications associated with peritoneal dialysis catheter insertion. Perit Dial Int. 2004;24:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Jwo SC, Chen KS, Lee CC, Chen HY. Prospective randomized study for comparison of open surgery with laparoscopic-assisted placement of Tenckhoff peritoneal dialysis catheter--a single center experience and literature review. J Surg Res. 2010;159:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Qiao Q, Lu GY, Xu DY, Zhou XJ. A comparison of two methods for catheterization in peritoneal dialysis. Jiangsu Yiyao. 2012;38:2812-2814. |
| 4. | Tu QD, He Q, Shen XG, Jiang XX, Liu YM, Shen QQ, Zhang HJ, Chen WF, Yao LX. [Clinical comparison of modified laparoscopic and conventional placement of peritoneal dialysis catheters]. Zhonghua Yi Xue Za Zhi. 2016;96:3586-3589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Qu JY, Hu GQ. Clinical study of modified open peritoneal dialysis catheterization and laparoscopic catheterization. Shenzhen Zhongxiyi Jiehe Zazhi. 2017;27:166-168. |
| 6. | van Laanen JHH, Cornelis T, Mees BM, Litjens EJ, van Loon MM, Tordoir JHM, Peppelenbosch AG. Randomized Controlled Trial Comparing Open Versus Laparoscopic Placement of a Peritoneal Dialysis Catheter and Outcomes: The CAPD I Trial. Perit Dial Int. 2018;38:104-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Vecino AM, Teruel JL, Navarro JL, Cesar JM. Phospholipase A2 activity in platelets of patients with uremia. Platelets. 2002;13:415-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Li M, Wang Z, Ma T, Lu G, Yan R, Zhao L, Deng K, Dai K. Enhanced platelet apoptosis in chronic uremic patients. Ren Fail. 2014;36:847-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Hibbard LT. Corpus luteum surgery. Am J Obstet Gynecol. 1979;135:666-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Gupta N, Dadhwal V, Deka D, Jain SK, Mittal S. Corpus luteum hemorrhage: rare complication of congenital and acquired coagulation abnormalities. J Obstet Gynaecol Res. 2007;33:376-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Dafopoulos K, Galazios G, Georgadakis G, Boulbou M, Koutsoyiannis D, Plakopoulos A, Anastasiadis P. Two episodes of hemoperitoneum from luteal cysts rupture in a patient with congenital factor X deficiency. Gynecol Obstet Invest. 2003;55:114-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Meili EO. [Clinical course and management of severe congenital factor XIII deficiency]. Hamostaseologie. 2002;22:48-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 13. | Akdemir A, Ergenoğlu AM, Yeniel AÖ, Akman L. Life-long oral anticoagulant therapy and rupture of corpus luteum. Anadolu Kardiyol Derg. 2013;13:407-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Takeda A, Sakai K, Mitsui T, Nakamura H. Management of ruptured corpus luteum cyst of pregnancy occurring in a 15-year-old girl by laparoscopic surgery with intraoperative autologous blood transfusion. J Pediatr Adolesc Gynecol. 2007;20:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Wang H, Guo L, Shao Z. Hemoperitoneum from corpus luteum rupture in patients with aplastic anemia. Clin Lab. 2015;61:427-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Levin C, Zalman L, Tamary H, Krasnov T, Khayat M, Shalev S, Salama I, Koren A. Small-platelet thrombocytopenia in a family with autosomal recessive inheritance pattern. Pediatr Blood Cancer. 2013;60:E128-E130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Zerbini L, Minari M, Manili L. Primary malfunction of a peritoneal dialysis catheter because of encasement in a hemorrhagic corpus luteum. Perit Dial Int. 2011;31:498-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Greenberg A, Bernardini J, Piraino BM, Johnston JR, Perlmutter JA. Hemoperitoneum complicating chronic peritoneal dialysis: single-center experience and literature review. Am J Kidney Dis. 1992;19:252-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Kohn OF, Culbertson S, Becker YT. Hemoperitoneum in a Peritoneal Dialysis Patient: Ruptured Ectopic Pregnancy. Perit Dial Int. 2018;38:455-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |