Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6428
Peer-review started: April 13, 2021
First decision: May 11, 2021
Revised: May 24, 2021
Accepted: June 1, 2021
Article in press: June 1, 2021
Published online: August 6, 2021
Processing time: 105 Days and 23.1 Hours
Heterotopic cesarean scar pregnancy (HCSP) is very rare and has a high risk of massive uterine bleeding. Preservation of concurrent intrauterine pregnancy (IUP) is one of the great challenges in the management of HCSP. No universal treatment protocol has been established when IUP is desired to be preserved.
We report a case of HCSP at 8+ wk gestation in a 34-year-old woman with stable hemodynamics. A two-step intervention was applied. Selective embryo aspiration was performed first, and surgical removal of ectopic gestational tissue by suction and curettage was performed 2 d later. Both steps were performed under ultrasound guidance. The patient had an uneventful course, and a healthy baby was delivered at 34+6 wk gestation.
Selective embryo aspiration followed by suction and curettage was successful in the preservation of IUP in the management of HCSP. This approach is an alternative option for HCSP in the first trimester when the IUP is desired to be preserved.
Core Tip: Preservation of intrauterine pregnancy (IUP) is challenging in the management of heterotopic cesarean scar pregnancy (HCSP). A consensus for the management of HCSP has not been established. We present that selective embryo aspiration followed by suction and curettage is a reliable and minimally invasive approach for the preservation of IUP. It is suggested to be an alternative option for HCSP in the first trimester when the IUP is desired to be preserved.
- Citation: Chen ZY, Zhou Y, Qian Y, Luo JM, Huang XF, Zhang XM. Management of heterotopic cesarean scar pregnancy with preservation of intrauterine pregnancy: A case report. World J Clin Cases 2021; 9(22): 6428-6434
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6428.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6428
Cesarean scar pregnancy (CSP) is one of the rarest forms of ectopic pregnancy and is located in the scar of a cesarean section. It is considered a precursor for a morbidly adherent placenta and predisposes a woman to life-threatening complications such as uterine rupture and severe bleeding[1,2]. Management of CSP is challenging, and immediate intervention is strongly recommended[2]. Heterotopic pregnancy (HP) is defined as the simultaneous presence of intrauterine pregnancy (IUP) and ectopic pregnancy. The incidence of HP has been estimated to be between 1 in 50000 and 1 in 10000. It has become more common with the implementation of assisted reproductive technology in recent years[3]. Heterotopic CSP (HCSP) is CSP combined with an IUP, which is even rarer than CSP alone. Preservation of concurrent IUP is one of the great challenges in the management of HCSP[4-6]. The most important priority is to decrease the risk of massive uterine bleeding and uterine rupture during treatment and ongoing pregnancy[7]. Expectant management was reported to be successful in HCSP with loss of cardiac activity of the scar pregnancy[8]. Selective embryo reduction has been a predominant option[4,5]. However, morbidly adherent placenta and massive bleeding during ongoing pregnancy are common obstetric complications[5,9]. Surgical management has been preferred by some authors[6,10,11]. Because of the rarity of HCSP, no universal treatment guidelines have been established when IUP is desired to be preserved.
In the present study, we report an optimized approach with successful preservation of the IUP in one HCSP case at 8 wk of gestation. Written informed consent was obtained from the couple, and approval for this study was obtained from the ethics committee of the Women's Hospital, School of Medicine, Zhejiang University (IRB-20210002-R).
In September 2019, a 34-year-old woman (gravida 2, para 1) at 8 wk of gestation was transferred to our hospital for further treatment.
The patient had a menstrual delay of 8 wk. She was suspected of having HCSP at a local hospital. The current pregnancy was spontaneously conceived. She manifested no abdominal pain or vaginal bleeding and had a strong desire to preserve the concurrent IUP.
She had a history of one cesarean delivery 7 years earlier.
The personal history and family history were unremarkable.
The patient’s vital signs were normal. Physical examination revealed a normal uterine cervix and abdomen and an 8-wk sized uterus with no tenderness. There was no vaginal bleeding or fluid.
The serum beta-human chorionic gonadotropin was 181231 UI/L. Blood tests for complete blood count, coagulation, and liver function were within normal limits.
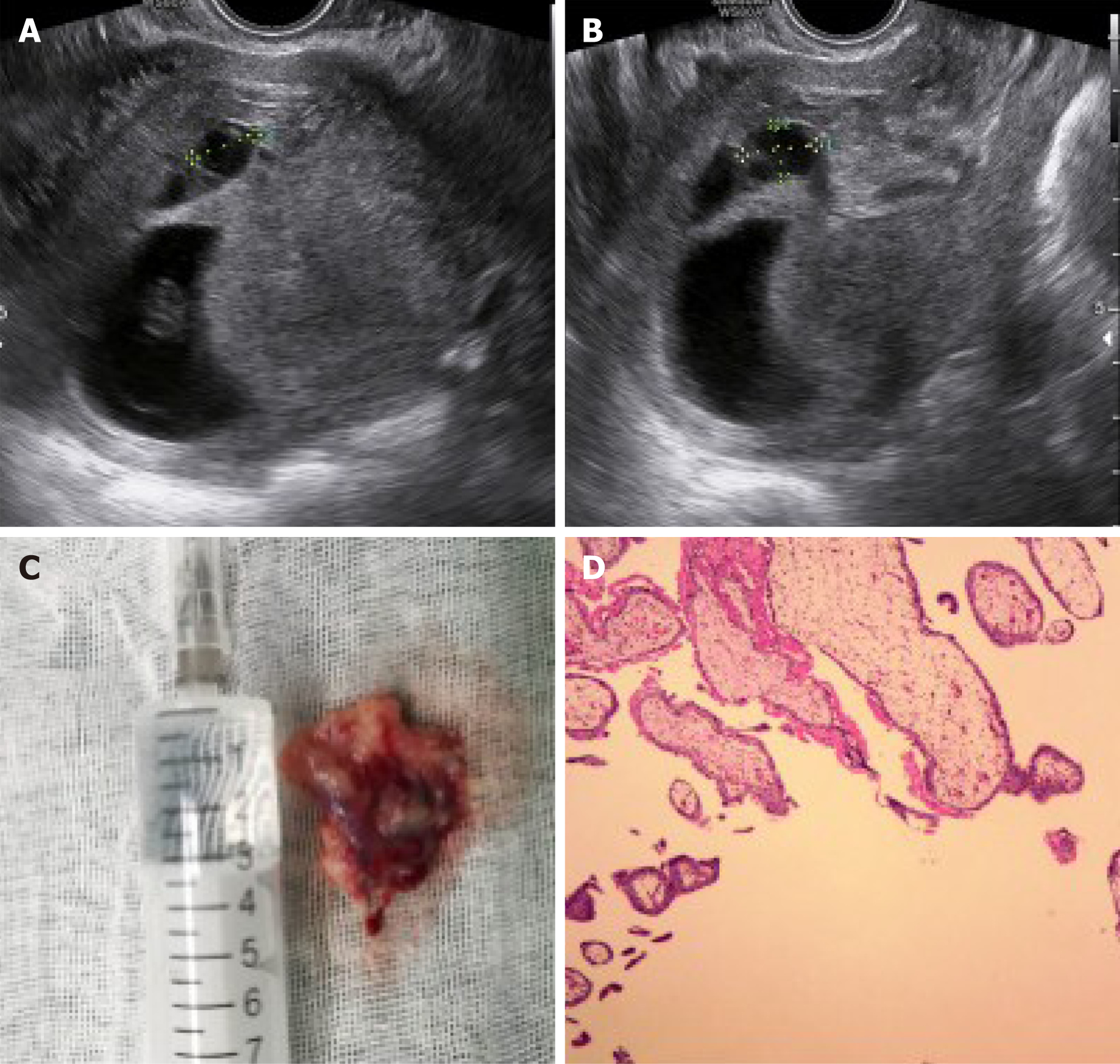
Transvaginal ultrasonography showed two gestational sacs with fetal activity, one located in the uterine fundus measuring 60 mm in diameter and the other in the previous cesarean scar measuring 51 mm in diameter (Figure 1). There was fluid buildup between the two gestational sacs. Ultrasonography revealed a thin layer of myometrium measuring 20 mm in thickness with a rich blood supply, which separated the gestational sac from the bladder.
HCSP was confirmed.
The patient and her husband were counseled on the potential complications of the maternal and fetal risks related to the intervention and to an ongoing pregnancy, including massive bleeding, abortion, and ultimately hysterectomy. We suggested the use of selective embryo aspiration followed by vacuum suction and curettage to terminate the ectopic pregnancy without delay.
Under transvaginal ultrasound guidance, 2 mL hyperosmolar glucose was injected using a 20-gauge double-lumen ovum aspiration needle inserted via the vaginal anterior fornix into the gestational sac located in the cesarean scar, and then embryo aspiration was accomplished at 8+2 wk gestation. Cessation of fetal activity of the ectopic pregnancy was confirmed by ultrasonography. Two days later, normal growth of the IUP in the uterine fundus and decreased size of the ectopic pregnancy sac measuring 13.5 mm × 11.4 mm × 10.2 mm was demonstrated by ultrasonography (Figure 2A and B). Surgical removal of the ectopic gestational tissue by vacuum suction and curettage was performed and guided by transabdominal ultrasound under spinal anesthesia. The cervix was carefully dilated by Hegel dilators to 8 mm. Gestational tissue in the lower uterine segment was gently removed by suction and curettage (Figure 2C). Trophoblastic tissue was confirmed by histopathologic examination (Figure 2D). Vaginal bleeding was minimal during the surgery. Finally, a normal IUP with disappearance of the ectopic pregnancy was confirmed by ultrasonography. Prophylactic antibiotics and progesterone were used for 2 d.
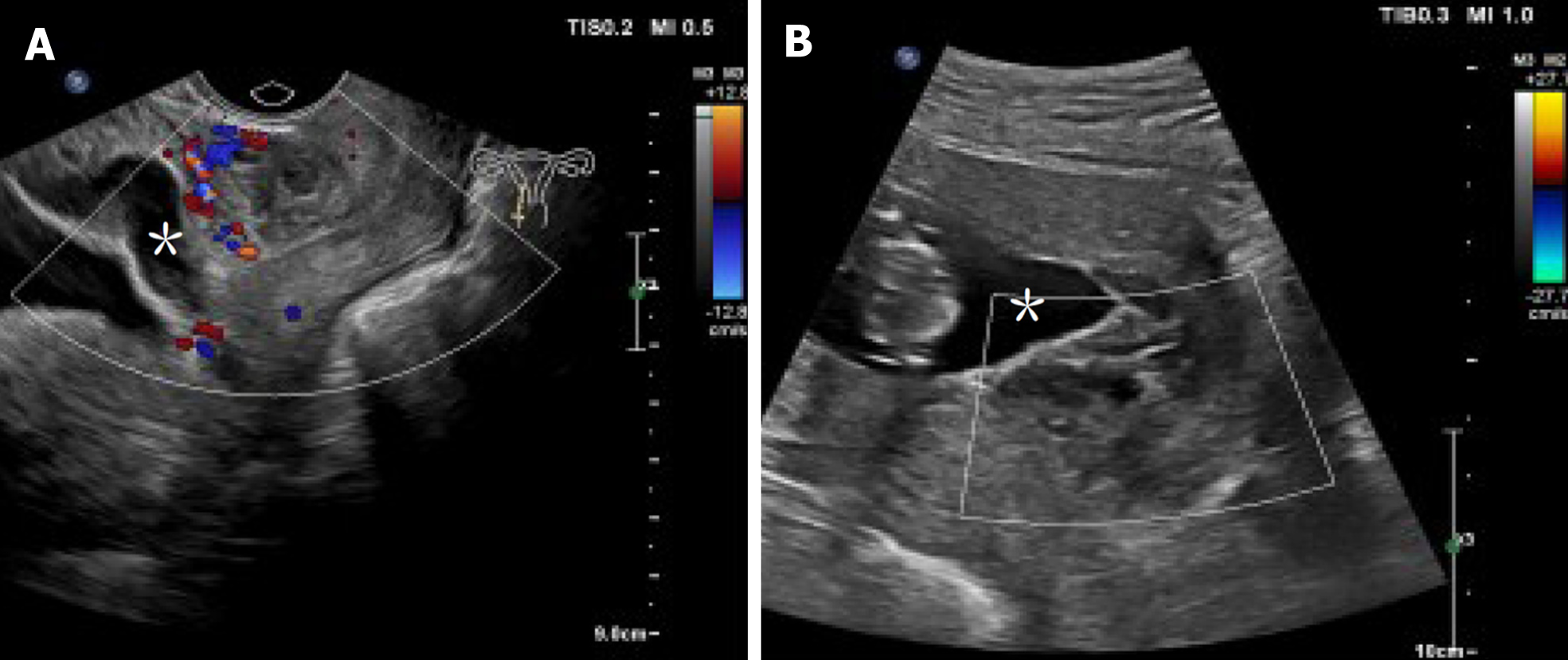
The patient experienced vaginal blood spotting for 8 wk. Subsequent serial sonographic scans confirmed a single ongoing pregnancy with normal growth parameters and placental site. A hematoma with a rich blood supply at the site of ectopic pregnancy implantation was revealed at 10 wk gestation (Figure 3A). After 3 wk, the hematoma persisted, while significantly diminished vascular flow was demonstrated (Figure 3B). The hematoma gradually subsided, and no hematoma was revealed at 20 wk gestation. The prenatal course was uneventful. Cesarean section was performed at 34+6 wk of gestation because of preterm membrane rupture. A healthy male baby weighing 2750 g was delivered. The patient had an unremarkable postoperative course.
To the best of our knowledge, this is the first case treated successfully by vacuum suction and curettage following selective embryo aspiration without any complications. We provide an alternative treatment option for HCSP when the IUP is desired to be preserved in the first trimester.
The increase in HCSP incidence and the patient’s desire to preserve the IUP emphasize the importance of improving treatment. A review of the literature up to January 2021 revealed 52 HCSP cases with a desire to preserve intrauterine gestation using a list of keywords including “Cesarean section scar,” “Ectopic pregnancy,” “CSP”, and “HCSP”. A consensus for the management of HCSP has not been established. Three treatment options have been reported, including expectant management, selective embryo reduction, and surgical intervention. Management options for HCSP are determined by patient characteristics, including clinical presentation, gestational age, viability of the HCSP, and the physician's experience. With increasing time of gestation, the risk of massive bleeding and uterine rupture increases. Expectant management is generally not recommended, while it might be an alternative option for a HCSP with loss of cardiac activity of the scar pregnancy[12]. Immediate intervention is suggested for HCSP cases. The earlier the intervention is implemented, the better the likely pregnancy outcome[4].
Selective embryo reduction was the main treatment modality for HCSP with a gestational age of less than 7 wk[4-6]. This method is performed by ultrasound guidance embryo aspiration, with or without simultaneous potassium chloride or hyperosmolar glucose injection[13-15]. Favorable pregnancy outcomes have been reported[4,16,17]. Out of 22 cases treated by selective embryo reduction, 19 (86.4%) had live births, and six (27.3%) had full-term births. However, the resolution of ectopic gestational tissue was uncertain after selective embryo aspiration. Seven patients (31.8%) were complicated with placenta previa and/or placenta accreta and 10 (45.5%) had massive bleeding during the ongoing pregnancy[5,9,13]. Other complications such as increasing size of residual mass and septic abortion were reported[9,18]. Hysterectomy was performed in three cases with uncontrollable bleeding[9,14,18]. These obstetric complications were attributed to the retained product of conception in the lower segment of the uterus. No appropriate treatment has been recommended when the retained ectopic trophoblastic tissue continues to grow to advanced gestational age.
Some authors prefer surgical intervention as an initial treatment for HCSP to reduce the risk of morbidly adherent placenta and massive bleeding during ongoing pregnancy[10,19,20]. Surgical intervention has been reported in six cases. Of these cases, five (83.33%) had live births, four (66.67%) had full-term births, and two (33.33%) were complicated by massive uterine bleeding. No morbidly adherent placenta or hysterectomy was reported in these patients. Surgical intervention seems to have improved pregnancy outcomes compared with selective embryo reduction, although the sample size was small. Even so, no recommended surgical approach is available. Difficultly visualizing HCSP was reported during the abdominal procedure[19]. Out of the 6 cases, two were managed by transvaginal approaches. Hysteroscopy was successfully performed at 7 wk gestation with a term delivery[20]. Curettage was performed in one emergency HCSP case at 9 wk of gestation; nevertheless, subsequent laparotomy was implemented because of persistent bleeding[6]. Compared with abdominal procedures, the transvaginal approach for the management of CSP is not only effective but also minimally invasive[21]. Successful hysteroscopic management indicates that transvaginal intervention is feasible in the management of HCSP when the IUP is desired to be preserved.
The present case was diagnosed at 8 wk gestation and had a high risk of massive bleeding. Preventative uterine artery embolism was not appropriate in this case. Considering the corresponding disadvantages of selective embryo reduction and surgical intervention, a two-step intervention was applied. Selective embryo aspiration was implemented first to reduce the viability of the ectopic pregnancy. Then, transvaginal surgical intervention was performed to remove the ectopic pregnancy tissue. For this case, we prefer vacuum suction and curettage rather than hysteroscopy considering that the intrauterine embryo might be disturbed by the upward force of the distended medium during hysteroscopy. A good pregnancy course and outcome were achieved as expected. This study indicates that vacuum suction and curettage are reliable when selective embryo aspiration is performed first. It could be an alternative option for HCSP patients with a high risk of bleeding and with a desire to preserve the IUP. It is worth mentioning that sonography was an important tool. It could help precisely locate the ectopic pregnancy during the intervention and monitor the vascular flow at the anterior wall of the lower segment of the uterus[14-16].
This two-step intervention reported in this study requires both the sonographer and the surgeon to have extensive experience. It is also suggested to be performed in a tertiary hospital. The possible risk of surgically induced abortion also requires attention. This two-step intervention has so far been applied to only this one case. It requires validation in more patients. Further studies are needed to define the best treatment options for HCSP when the IUP is desired to be preserved.
In conclusion, we present an optimized approach for the management of HCSP with successful preservation of the IUP. Selective embryo aspiration followed by vacuum suction and curettage could enable complete removal of the ectopic pregnancy and reduce the risk of uterine bleeding. The proposed approach is reliable and minimally invasive and is suggested to be an alternative option for HCSP in the first trimester when the IUP is desired to be preserved.
Special thanks to Chris Wood from the Life Science College of Zhejiang University for language support. We also thank the nurses and physicians for their care of this patient.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sel G S-Editor: Fan JR L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Zosmer N, Fuller J, Shaikh H, Johns J, Ross JA. Natural history of early first-trimester pregnancies implanted in Cesarean scars. Ultrasound Obstet Gynecol. 2015;46:367-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 2. | Birch Petersen K, Hoffmann E, Rifbjerg Larsen C, Svarre Nielsen H. Cesarean scar pregnancy: a systematic review of treatment studies. Fertil Steril. 2016;105:958-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 274] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 3. | Dor J, Seidman DS, Levran D, Ben-Rafael Z, Ben-Shlomo I, Mashiach S. The incidence of combined intrauterine and extrauterine pregnancy after in vitro fertilization and embryo transfer. Fertil Steril. 1991;55:833-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Wang Y, Niu Z, Tao L, Yang Y, Ma C, Li R. Early intervention for heterotopic caesarean scar pregnancy to preserve intrauterine pregnancy may improve outcomes: a retrospective cohort study. Reprod Biomed Online. 2020;41:290-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Yu H, Luo H, Zhao F, Liu X, Wang X. Successful selective reduction of a heterotopic cesarean scar pregnancy in the second trimester: a case report and review of the literature. BMC Pregnancy Childbirth. 2016;16:380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Laing-Aiken Z, Robson D, Wu J. Surgical management of first-trimester bleeding in a heterotopic caesarean scar pregnancy: A case report and review of literature. Case Rep Womens Health. 2020;27:e00209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Lincenberg KR, Behrman ER, Bembry JS, Kovac CM. Uterine Rupture with Cesarean Scar Heterotopic Pregnancy with Survival of the Intrauterine Twin. Case Rep Obstet Gynecol. 2016;2016:6832094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Vikhareva O, Nedopekina E, Herbst A. Normal vaginal delivery at term after expectant management of heterotopic caesarean scar pregnancy: a case report. J Med Case Rep. 2018;12:179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Miyague AH, Chrisostomo AP, Costa SL, Nakatani ET, Kondo W, Gomes CC. Treatment of heterotopic caesarean scar pregnancy complicated with post termination increase in size of residual mass and morbidly adherent placenta. J Clin Ultrasound. 2018;46:227-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Armbrust R, Krätschell R, Henrich W, David M. Operative Therapy for Heterotopic Scar Pregnancy and Successful Birth of the Intrauterine Foetus - Case Report and Review of the Literature. Geburtshilfe Frauenheilkd. 2015;75:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Vetter MH, Andrzejewski J, Murnane A, Lang C. Surgical Management of a Heterotopic Cesarean Scar Pregnancy With Preservation of an Intrauterine Pregnancy. Obstet Gynecol. 2016;128:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Ouyang Y, Chen H, Lin G, Xiang S, Qin J, Gong F, Li X. Heterotopic Cesarean Scar Pregnancy: An Analysis of 20 Cases Following in vitro Fertilization-Embryo Transfer. J Ultrasound Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Lui MW, Shek NW, Li RH, Chu F, Pun TC. Management of heterotopic cesarean scar pregnancy by repeated transvaginal ultrasonographic-guided aspiration with successful preservation of normal intrauterine pregnancy and complicated by arteriovenous malformation. Eur J Obstet Gynecol Reprod Biol. 2014;175:209-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Ugurlucan FG, Bastu E, Dogan M, Kalelioglu I, Alanya S, Has R. Management of cesarean heterotopic pregnancy with transvaginal ultrasound-guided potassium chloride injection and gestational sac aspiration, and review of the literature. J Minim Invasive Gynecol. 2012;19:671-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Chong YW, Ma CH. Heterotopic caesarean scar pregnancy: a case report. Zhonghua Fu Chan Ke Za Zhi. 2013;48:397. [DOI] [Full Text] |
| 16. | Uysal F, Uysal A. Spontaneous heterotopic cesarean scar pregnancy: conservative management by transvaginal sonographic guidance and successful pregnancy outcome. J Ultrasound Med. 2013;32:547-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Salomon LJ, Fernandez H, Chauveaud A, Doumerc S, Frydman R. Successful management of a heterotopic Caesarean scar pregnancy: potassium chloride injection with preservation of the intrauterine gestation: case report. Hum Reprod. 2003;18:189-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Tymon-Rosario J, Chuang M. Selective Reduction of a Heterotopic Cesarean Scar Pregnancy Complicated by Septic Abortion. Case Rep Obstet Gynecol. 2018;2018:6478589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Demirel LC, Bodur H, Selam B, Lembet A, Ergin T. Laparoscopic management of heterotopic cesarean scar pregnancy with preservation of intrauterine gestation and delivery at term: case report. Fertil Steril. 2009;91:1293.e5-1293.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Wang CJ, Tsai F, Chen C, Chao A. Hysteroscopic management of heterotopic cesarean scar pregnancy. Fertil Steril. 2010;94:1529.e15-1529.e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Jurkovic D, Knez J, Appiah A, Farahani L, Mavrelos D, Ross JA. Surgical treatment of Cesarean scar ectopic pregnancy: efficacy and safety of ultrasound-guided suction curettage. Ultrasound Obstet Gynecol. 2016;47:511-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |