Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6410
Peer-review started: March 11, 2021
First decision: April 13, 2021
Revised: April 25, 2021
Accepted: May 27, 2021
Article in press: May 27, 2021
Published online: August 6, 2021
Processing time: 138 Days and 18 Hours
Ileal hemorrhagic infarction after carotid artery stenting (CAS) is a fatal complication. The prognosis of ileal hemorrhagic infarction after CAS is very poor if not treated in a timely manner. We describe a rare case of ileal hemorrhagic infarction due to acute embolism of the mesenteric artery after CAS.
A 67-year-old man with acute ischemic stroke underwent CAS via the right femoral artery approach 21 d after intensive medical treatment. On the first day after surgery, the patient had abdominal distension and abdominal pain. Abdominal enhanced computed tomography revealed intestinal obstruction, severe stenosis of the superior mesenteric artery, and poor distal angiography. An exploratory laparotomy was performed, and pathological examination showed hemorrhagic ileal infarction. It was subsequently found that the patient had intestinal flatulence. With the guidance of an ultrasound scan, the patient underwent abdominal puncture, drainage, and catheterization. After 58 d of treatment, the patient was discharged from hospital with a National Institutes of Health Stroke Scale score of 2 points, and a Modified Rankin Scale score of 1 point. At the 6-mo follow-up, the patient had an excellent functional outcome without stroke or mesenteric ischemia. Furthermore, computed tomography angiography showed that the carotid stent was patent.
Ileal hemorrhagic infarction is a fatal complication after CAS, usually caused by mesenteric artery embolism. Thus, more attention should be paid to the complications of embolism in the vascular system as well as the nervous system after CAS, and the complications should be identified and treated as early as possible.
Core Tip: Nervous system embolism is a common complication after carotid artery stenting (CAS), and the occurrence of vascular embolism outside the nervous system is rare, especially, mesenteric artery embolism leading to ileal hemorrhagic infarction. However, we should still pay attention to these cases in order to timely find, diagnose, and properly treat them. We report an elderly man who developed intestinal obstruction after CAS. Fortunately, the complication was found and diagnosed in timely. After surgical operation, the symptoms of intestinal obstruction were relieved. As a result, the patient's life was saved. At the 6-mo follow-up, there was no stroke or intestinal infarction.
- Citation: Xu XY, Shen W, Li G, Wang XF, Xu Y. Ileal hemorrhagic infarction after carotid artery stenting: A case report and review of the literature. World J Clin Cases 2021; 9(22): 6410-6417
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6410.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6410
Ischemic stroke is the second leading cause of global death and is the main cause of permanent disability[1]. In patients with disabilities, 20%-30% of ischemic stroke cases are caused by carotid stenosis[2], especially symptomatic carotid stenosis, which increases the recurrence risk of ischemic stroke[3]. The current treatment for carotid artery stenosis mainly includes drugs and invasive treatment, which comprises carotid endarterectomy (CEA) and carotid artery stenting (CAS). However, CEA is superior to drugs in severe symptomatic carotid artery stenosis[4], and is the gold standard for the treatment of carotid stenosis[5]. The CREST (Carotid Revascularization Endarterectomy vs Stenting Trial) and other studies showed that CAS had the same effect as CEA in treating symptomatic and asymptomatic carotid stenosis, and there was no significant difference in the incidence of overall postoperative complications even though CAS was less invasive than CEA[6-9]. Embolism is a common complication after CAS, which is usually reported as nervous system embolism[10]. However, no cases of ileal hemorrhagic infarction caused by mesenteric artery embolism after CAS have been reported.
A 67-year-old man presented with right limb weakness for 5 d.
Five days ago, the patient developed right limb weakness and non-fluent speech, without treatment, but no obviously aggravated trend in symptoms.
The patient had a history of hypertension for 5 years, and was taking nifedipine controlled-release tablets and irbesartan hydrochlorothiazide to control his blood pressure. In addition, he had been suffering from type 2 diabetes for 3 years and was taking acarbose and repaglinide to manage the disease; however, control of his blood sugar level was slightly worse. Furthermore, he had a history of coronary heart disease and was treated with aspirin and atorvastatin.
There was no family history of stroke.
The patient’s temperature was 36.7 ℃, heart rate was 72 bpm, respiratory rate was 19 breaths/min, and blood pressure was 155/95 mmHg. He was conscious with non-fluent speech, the right nasolabial sulcus was shallow and the tongue was extended to the right, the right limb had grade 4 muscle strength, the right Babinski sign was positive, and the National Institutes of Health Stroke Scale (NIHSS) score was 4 points.
The results of laboratory examinations were all within normal limits, including complete blood count, routine urinalysis, coagulation function, kidney function, and liver function. The results of hepatic serology were also negative. The fasting blood glucose level was increased at 9.7 mmol/L (3.9-6.1 mmol/L). No atrial fibrillation was found after dynamic electrocardiography.
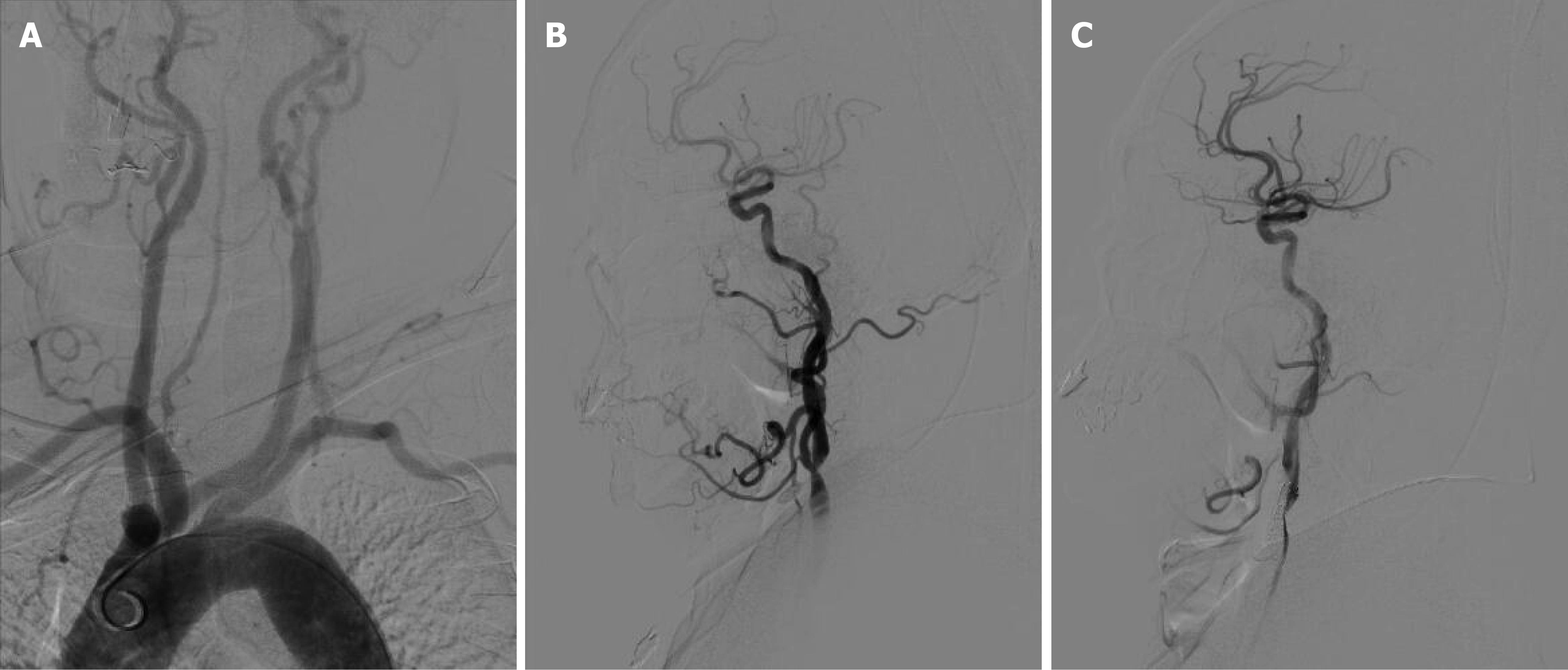
Diffusion-weighted imaging after admission indicated acute left frontal-parietal infarction. Computed tomography angiography (CTA) also revealed severe stenosis of the bifurcation of the left common carotid artery. The patient was maintained on 100 mg aspirin and 75 mg clopidogrel daily for 21 d. The right femoral artery approach was used for digital subtraction angiography (DSA), which showed a type III aortic arch (Figure 1A) and severe stenosis at the bifurcation of the left common carotid artery (Figure 1B). The right femoral artery approach was performed, and an embolic protection device (ev3 Spider FX 5 mm; ev3 Inc, 4600 Nathan Lane North, Plymouth, MN, United States) was placed. The left common carotid artery was dilated with a 5.0 mm balloon ( Aviator 5.0 mm × 30 mm; Cordis Europa N.V, Oosteinde 8,9301 LJ Roden, The Netherland), and a carotid stent (Precise 8 mm × 6 mm × 30 mm; Cordis Corporation, 14201 N.W. 60th Avenue Miami Lakes, FL, United States) was inserted. Angiography after CAS placement showed that the stenosis at the bifurcation of the left common carotid artery was significantly improved (Figure 1C).
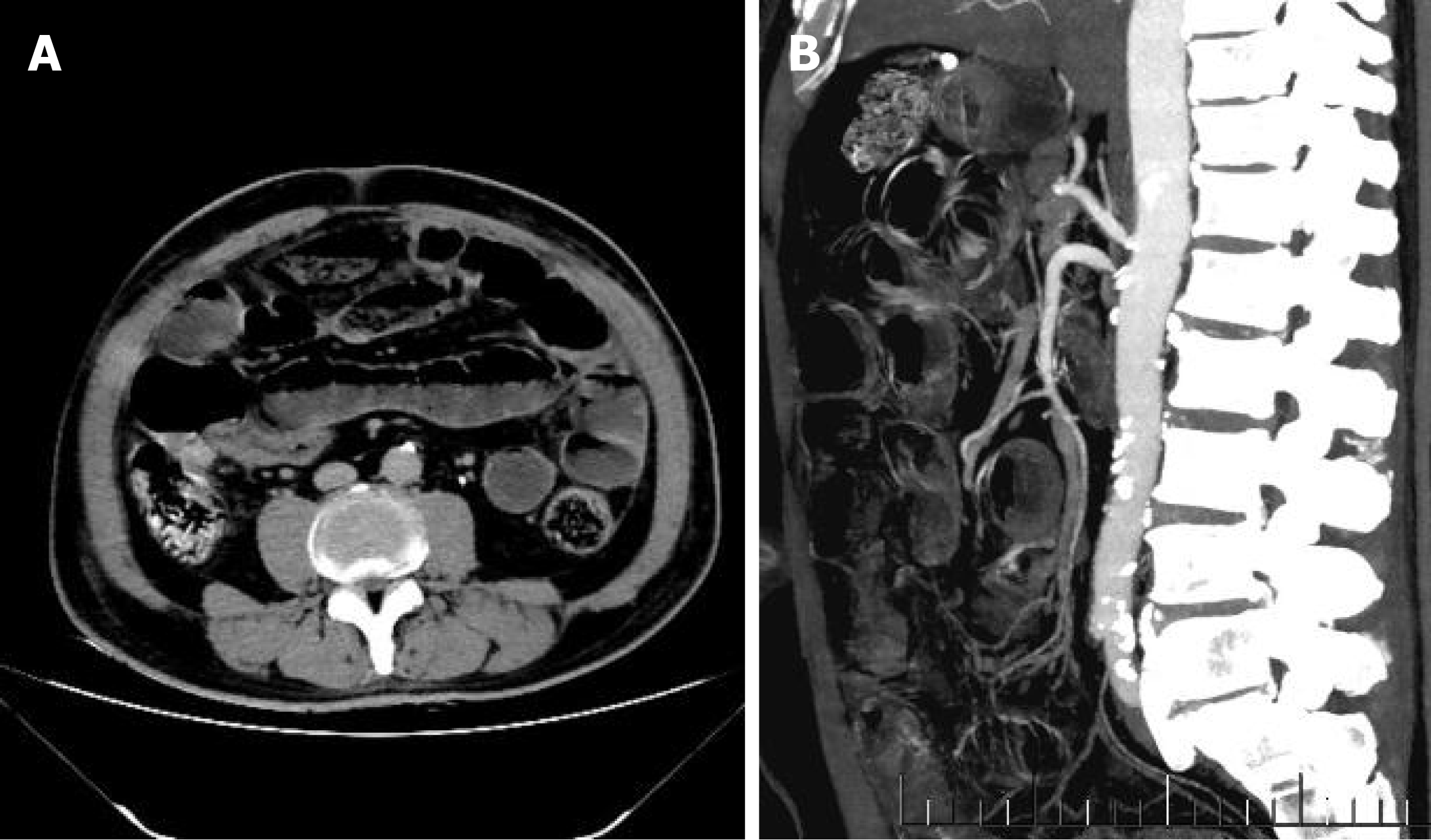
On the first day after surgery, the patient developed abdominal distension and abdominal pain, which were accompanied by inhibited defecation. Even though no vomiting was observed, abdominal enhanced computed tomography (CT) was immediately performed. The results suggested that the structure of the intestinal canal in the abdomen was unclear, and that some parts of the intestine were dilated due to pneumatosis and hydrops. The fluid level could be observed; however, the intestinal wall of the small intestine in the right lower abdomen was slightly thickened, indicating intestinal obstruction and edema of the intestinal wall (Figure 2A). It was also observed that the superior mesenteric artery showed severe stenosis with poor distal angiography (Figure 2B).
After gastrointestinal surgery consultation, emergency exploratory laparotomy was recommended to confirm the diagnosis.
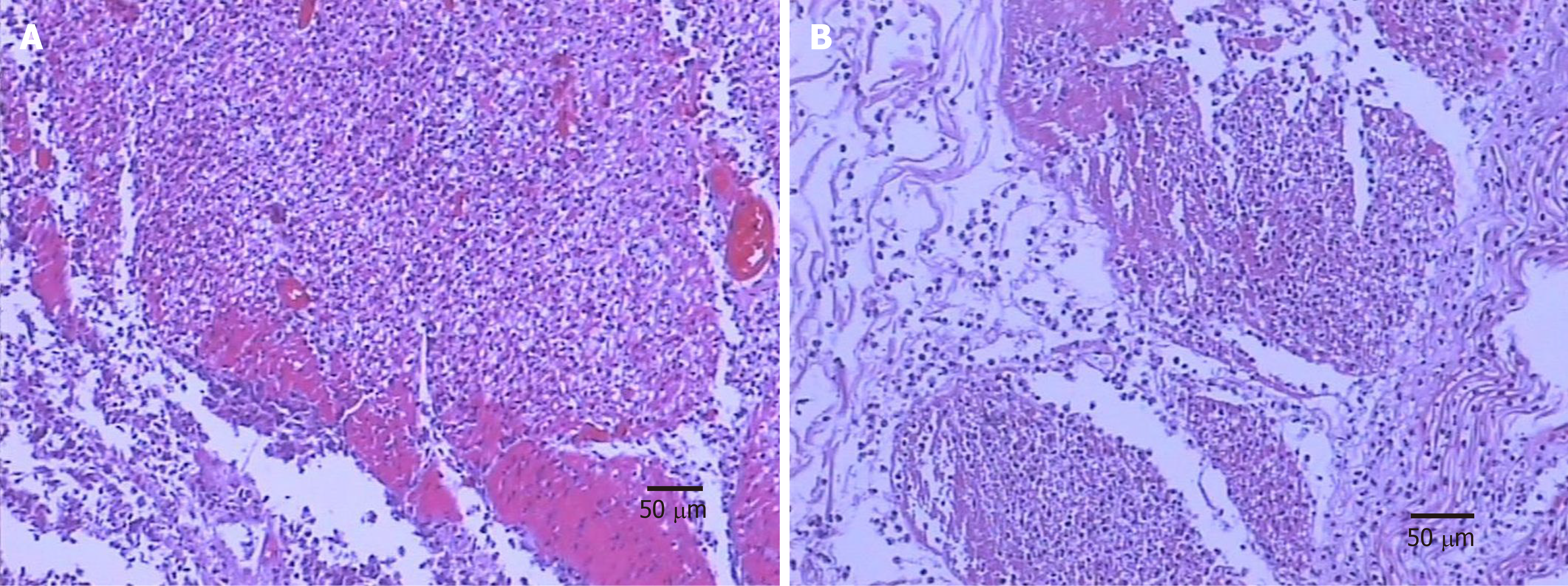
The patient’s family members agreed to the procedure, and the surgeon performed an exploratory laparotomy. A reduction of the volvulus, partial ileectomy, and release of intestinal adhesions were carried out. After surgery, pathology of the ileectomy site showed microscopic intestinal mucosa necrosis, exfoliation, full-thickness vasodilation and hyperemia, fibrinous exudation, and necrosis of serous membrane, thus indicating ileal hemorrhagic infarction (Figure 3).
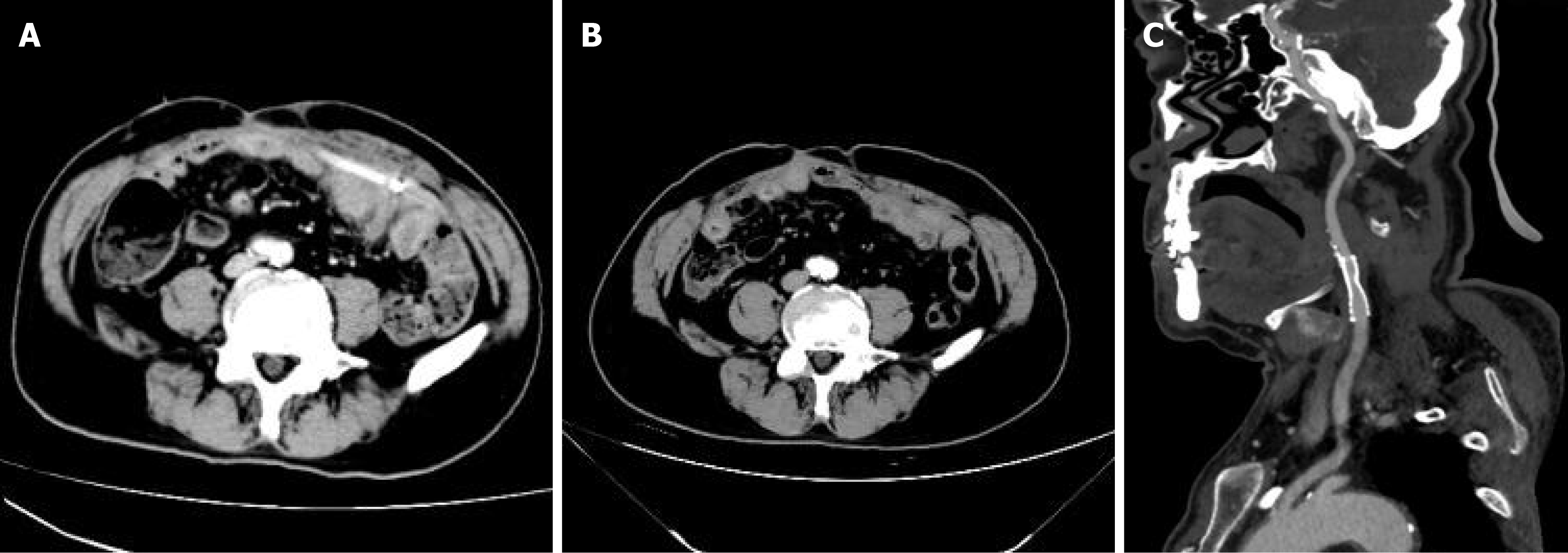
Within 10 d after partial ileal resection, the patient's abdominal pain significantly improved, but his symptoms of abdominal distension were still observed. The results of color Doppler ultrasound examination suggested intra-abdominal intestinal flatulence. Thus, ultrasound-guided abdominal puncture, drainage, and catheterization were performed. A review of abdominal enhanced CT revealed that the drainage tube was unobstructed without intestinal obstruction (Figure 4A). Following the relief of intestinal flatulence, the abdominal drainage tube was removed, and abdominal enhanced CT showed no intestinal obstruction or flatulence (Figure 4B). After 58 d of treatment, the patient was discharged from hospital with a NIHSS score of 2 points and a Modified Rankin Scale (mRS) score of 1 point.
A CTA review at 6 mo after CAS showed that the carotid artery stent was patent (Figure 4C). The NIHSS score of the patient at 6 mo after CAS was 1 point and the mRS score was 1 point, and both stroke and mesenteric ischemia were absent.
CAS is an effective treatment for carotid artery stenosis[6-9]. However, embolism is one of the most common and serious complications during the perioperative period[10]. A clinical study, which retrospectively analyzed 19826 consecutive patients who underwent DSA, showed that embolic complications occurred in 0.05% of all patients[11]. The CREST study findings with a 10-year follow-up period, revealed that the incidence of stroke after CAS was less than 7%[8]. When a patient’s health is complicated by acute cerebral embolism, immediate diagnosis and timely treatment are essential, which includes thrombolysis, interventional intravascular therapy, and other methods[12]. Moreover, the current advances in technology and materials have further reduced the risk of embolic stroke after CAS, especially the use of embolic protection devices during CAS[3,9]. However, embolism of small blood vessels in other parts, such as embolism of the mesenteric artery, is not easily detected. This means that the patient’s life is in danger due to delayed optimal treatment.
The mesenteric circulation is extremely complicated, the superior mesenteric artery, inferior mesenteric artery, and celiac artery are interconnected by collateral networks between the visceral and nonvisceral circulations. These interconnections mean that the loss of a single vessel will lead to catastrophic poor vascular perfusion[13], and the ileum is supplied by the superior mesenteric artery. Acute mesenteric ischemia is usually caused by acute occlusion of the superior mesenteric artery, and embolism is the most common cause of mesenteric ischemia, accounting for approximately 40%-50%[13]. Acute mesenteric ischemia is a catastrophic complication caused by possible inaccurate or delayed diagnosis and treatment, and has a mortality rate of 60%-80%[14]. Long-term ischemia of the mesentery can also activate systemic inflammatory pathways, deteriorate intestinal vasospasm, and can develop into full-thickness injury, infarction, and death of the intestinal wall unless treated in a timely manner[13]. However, abdominal pain and tenderness and other peritoneal irritation signs are not typical in the early stage of acute mesenteric ischemia; therefore, they are often diagnosed as other diseases by clinicians[15]. This is especially true for elderly patients, as their medical history and symptom description could be unclear due to fluctuations in their mental status during the examination, thereby causing diagnostic and treatment delays in these patients[16]. The treatment for acute mesenteric ischemia currently includes mainly heparin, vasodilators, antibiotics, intravascular repair, and open surgical treatment[13]. The purpose of open surgical treatment for acute mesenteric ischemia is to rebuild occlusive blood vessels, assess intestinal viability, and remove necrotic intestine[17]. Studies have shown that up to 57% of all patients eventually undergo bowel resection and about 40% of them need to undergo second-stage surgery[18]. Our patient initially underwent a partial ileectomy, followed by an ultrasound-guided abdominal puncture at a later stage. Regular reexamination is necessary, considering the common recurrence of mesenteric ischemia[13]. Our patient was followed for 6 mo after surgery and abdominal CT showed no bowel obstruction or mesenteric ischemia.
Embolism is a common complication after CAS, and some factors, such as thrombus-containing lesions, heavily calcified lesions, very tortuous vessels, near occlusions, older age, decreased cerebral reserve, and prolonged catheter or guide wire manipulation in the aortic arch, have been associated with increased complications after CAS[19,20]. Further studies have shown that complex vascular anatomy, such as type III aortic arch, increases the incidence of complications after CAS[21-25]. Our patient had a type III aortic arch, which increased the risk of perioperative complications. Although the use of the embolic protection device in CAS can reduce the risk of embolic stroke[3,9], careful surgery is still needed to avoid embolism in other areas. Some studies have shown that transfemoral carotid artery stenting (TCAR) can reduce the incidence of perioperative embolic complications in CAS, especially in high-risk patients requiring treatment with CAS, and has a low incidence of local complications, neurological events, myocardial complications, and mortality during the early postoperative period, and is considered an acceptable alternative in patients treated with CAS[26-29]. Furthermore, transradial carotid artery stenting has demonstrated feasibility and safety in CAS[30-32]. Recently, robotic-assisted CAS has been shown to be technically feasible; however, further studies are warranted to properly establish the safety and benefits of this technique[30,33].
Mesenteric artery embolism can leads to ileal hemorrhagic infarction after CAS, which is a rare and fatal complication. Therefore, more attention needs to be paid to the complications of embolism in areas other than the nervous system after CAS. This means that before CAS, accurate diagnosis and adequate pre-operative preparation are essential, especially in patients with complicated vascular anatomy. In addition, it is important to adopt more refined operations to avoid the occurrence of complications, and these patients require intensive nursing after surgery to ensure that these complications can be identified and urgently addressed.
Manuscript source: Unsolicited manuscript
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsikas D S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Gorelick PB. The global burden of stroke: persistent and disabling. Lancet Neurol. 2019;18:417-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 388] [Article Influence: 64.7] [Reference Citation Analysis (0)] |
| 2. | Boulanger M, Touzé E. Periprocedural risk of myocardial infarction after carotid endarterectomy and carotid angioplasty and stenting. Arch Cardiovasc Dis. 2016;109:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Park JH, Lee JH. Carotid Artery Stenting. Korean Circ J. 2018;48:97-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC, Sackett DL, Thorpe KE, Meldrum HE, Spence JD. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415-1425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2514] [Cited by in RCA: 2268] [Article Influence: 84.0] [Reference Citation Analysis (0)] |
| 5. | Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001;32:2735-2740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 774] [Cited by in RCA: 856] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 6. | Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2408] [Cited by in RCA: 2083] [Article Influence: 138.9] [Reference Citation Analysis (0)] |
| 7. | Al-Damluji MS, Nagpal S, Stilp E, Remetz M, Mena C. Carotid revascularization: a systematic review of the evidence. J Interv Cardiol. 2013;26:399-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Brott TG, Howard G, Roubin GS, Meschia JF, Mackey A, Brooks W, Moore WS, Hill MD, Mantese VA, Clark WM, Timaran CH, Heck D, Leimgruber PP, Sheffet AJ, Howard VJ, Chaturvedi S, Lal BK, Voeks JH, Hobson RW 2nd; CREST Investigators. Long-Term Results of Stenting versus Endarterectomy for Carotid-Artery Stenosis. N Engl J Med. 2016;374:1021-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 515] [Article Influence: 57.2] [Reference Citation Analysis (0)] |
| 9. | Rosenfield K, Matsumura JS, Chaturvedi S, Riles T, Ansel GM, Metzger DC, Wechsler L, Jaff MR, Gray W; ACT I Investigators. Randomized Trial of Stent versus Surgery for Asymptomatic Carotid Stenosis. N Engl J Med. 2016;374:1011-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 423] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 10. | Millet JD, Cavallo JJ, Scoutt LM, Gunabushanam G. Sonographic Evaluation of Complications of Extracranial Carotid Artery Interventions. J Ultrasound Med. 2018;37:769-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Kaufmann TJ, Huston J 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology. 2007;243:812-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 432] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 12. | Owens EL, Kumins NH, Bergan JJ, Sparks SR. Surgical management of acute complications and critical restenosis following carotid artery stenting. Ann Vasc Surg. 2002;16:168-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Clair DG, Beach JM. Mesenteric Ischemia. N Engl J Med. 2016;374:959-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 329] [Article Influence: 36.6] [Reference Citation Analysis (1)] |
| 14. | Kassahun WT, Schulz T, Richter O, Hauss J. Unchanged high mortality rates from acute occlusive intestinal ischemia: six year review. Langenbecks Arch Surg. 2008;393:163-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 167] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 15. | Kärkkäinen JM, Lehtimäki TT, Manninen H, Paajanen H. Acute Mesenteric Ischemia Is a More Common Cause than Expected of Acute Abdomen in the Elderly. J Gastrointest Surg. 2015;19:1407-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 16. | Silva JA, White CJ. Ischemic bowel syndromes. Prim Care. 2013;40:153-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Plumereau F, Mucci S, Le Naoures P, Finel JB, Hamy A. Acute mesenteric ischemia of arterial origin: importance of early revascularization. J Visc Surg. 2015;152:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Kougias P, Lau D, El Sayed HF, Zhou W, Huynh TT, Lin PH. Determinants of mortality and treatment outcome following surgical interventions for acute mesenteric ischemia. J Vasc Surg. 2007;46:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 163] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 19. | White CJ, Ramee SR, Collins TJ, Jenkins JS, Reilly JP, Patel RA. Carotid artery stenting: patient, lesion, and procedural characteristics that increase procedural complications. Catheter Cardiovasc Interv. 2013;82:715-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Vatan MB, Acar BA, Aksoy M, Can Y, Varım C, Agac MT, Kilic H, Tatli E, Gunduz H, Akdemir R. Predictors of periprocedural complications of carotid artery stenting - a multivariate analysis of a single-centre experience. Vasa. 2016;45:387-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Khan M, Qureshi AI. Factors Associated with Increased Rates of Post-procedural Stroke or Death following Carotid Artery Stent Placement: A Systematic Review. J Vasc Interv Neurol. 2014;7:11-20. [PubMed] |
| 22. | Müller MD, Ahlhelm FJ, von Hessling A, Doig D, Nederkoorn PJ, Macdonald S, Lyrer PA, van der Lugt A, Hendrikse J, Stippich C, van der Worp HB, Richards T, Brown MM, Engelter ST, Bonati LH. Vascular Anatomy Predicts the Risk of Cerebral Ischemia in Patients Randomized to Carotid Stenting Versus Endarterectomy. Stroke. 2017;48:1285-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 23. | Fanous AA, Jowdy PK, Morr S, Vakharia K, Shallwani H, Lorincz K, Hopkins LN, Davies JM, Snyder KV, Siddiqui AH, Levy EI. Vascular Anatomy and Not Age is Responsible for Increased Risk of Complications in Symptomatic Elderly Patients Undergoing Carotid Artery Stenting. World Neurosurg. 2019;128:e513-e521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Marrocco-Trischitta MM, Baroni I, Vitale R, Nava G, Nano G, Secchi F. Type III Arch Configuration as a Risk Factor for Carotid Artery Stenting: A Systematic Review of Contemporary Guidelines on Management of Carotid Artery Stenosis. Ann Vasc Surg. 2020;68:505-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Casana R, Bissacco D, Malloggi C, Tolva VS, Odero A Jr, Domanin M, Trimarchi S, Silani V, Parati G. Aortic arch types and postoperative outcomes after carotid artery stenting in asymptomatic and symptomatic patients. Int Angiol. 2020;39:485-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Naazie IN, Cui CL, Osaghae I, Murad MH, Schermerhorn M, Malas MB. A Systematic Review and Meta-Analysis of Transcarotid Artery Revascularization with Dynamic Flow Reversal Versus Transfemoral Carotid Artery Stenting and Carotid Endarterectomy. Ann Vasc Surg. 2020;69:426-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 27. | Nana PN, Brotis AG, Spanos KT, Kouvelos GN, Matsagkas MI, Giannoukas AD. A systematic review and meta-analysis of carotid artery stenting using the transcervical approach. Int Angiol. 2020;39:372-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Paraskevas KI, Antonopoulos CN, Kakisis JD, Geroulakos G. An updated systematic review and meta-analysis of results of transcervical carotid artery stenting with flow reversal. J Vasc Surg. 2020;72:1489-1498.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Teter K, Lamparello PJ, Barfield M, Rockman CB, Macdonald S, Maldonado TS. Low-frequency avoidable errors during transcarotid artery revascularization. J Vasc Surg. 2021;73:1658-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Weinberg JH, Sweid A, Sajja K, Gooch MR, Herial N, Tjoumakaris S, Rosenwasser RH, Jabbour P. Comparison of robotic-assisted carotid stenting and manual carotid stenting through the transradial approach. J Neurosurg. 2020;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 31. | Almallouhi E, Leary J, Wessell J, Al Kasab S, Pai S, Sattur MG, Lena JR, Spiotta AM. Fast-track incorporation of the transradial approach in endovascular neurointervention. J Neurointerv Surg. 2020;12:176-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 32. | Jaroenngarmsamer T, Bhatia KD, Kortman H, Orru E, Krings T. Procedural success with radial access for carotid artery stenting: systematic review and meta-analysis. J Neurointerv Surg. 2020;12:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | Nogueira RG, Sachdeva R, Al-Bayati AR, Mohammaden MH, Frankel MR, Haussen DC. Robotic assisted carotid artery stenting for the treatment of symptomatic carotid disease: technical feasibility and preliminary results. J Neurointerv Surg. 2020;12:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |