Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6380
Peer-review started: February 6, 2021
First decision: April 25, 2021
Revised: May 5, 2021
Accepted: May 27, 2021
Article in press: May 27, 2021
Published online: August 6, 2021
Processing time: 171 Days and 8.6 Hours
Rupture of an intracranial aneurysm is a type of acute stroke that is a serious threat to human health. Misdiagnosis of ruptured intracranial aneurysms is a serious clinical event that may have disastrous consequences in some patients. To date, ruptured intracranial aneurysms have been misdiagnosed as meningitis, tumors, stroke, or trauma, among other conditions. Here, we report what appears to be the first case of a ruptured intracranial aneurysm that presented as cerebral circulation insufficiency.
A middle-aged man was admitted to our hospital because of a parasellar lesion identified on a noncontrast computed tomography (CT) image after a mild traffic accident that was caused by a brief loss of consciousness. Notably, he was diagnosed with cerebral circulation insufficiency after two unexplained episodes of a transient loss of consciousness within the past 8 mo. The patient was diagnosed with right internal carotid artery aneurysm based on CT angiography and completely recovered after a craniotomy at our hospital. A few clots and severe adhesions around the aneurysm were observed in the subarachnoid space during the operation, suggesting that the aneurysm had ruptured and may had been misdiagnosed as cerebral circulation insufficiency.
Ruptured intracranial aneurysms may show negative imaging results and present as cerebral circulation insufficiency, which should be recognized as soon as possible to ensure timely management.
Core Tip: This paper reports a case of ruptured intracranial aneurysm presenting as cerebral circulation insufficiency. Furthermore, the causes of misdiagnosis and experiences about the diagnosis and management are discussed by literature review. To the best of our knowledge, this is the first report of intracranial aneurysmal rupture presenting as cerebral circulation insufficiency. Our report also demonstrates a rare case of short-term dilated intracranial cystic aneurysm.
- Citation: Zhao L, Zhao SQ, Tang XP. Ruptured intracranial aneurysm presenting as cerebral circulation insufficiency: A case report. World J Clin Cases 2021; 9(22): 6380-6387
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6380.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6380
Subarachnoid hemorrhage (SAH) is the most common form of ruptured intracranial aneurysm and has clinical presentations that range from a simple headache to obvious neurological deficits. SAH is easily suspected and diagnosed based on imaging findings in patients who present with sudden severe headaches, vomiting, disturbance of consciousness, and other typical clinical manifestations. However, a small number of patients may have extremely rare clinical or imaging manifestations, leading to a difficulty in determining the diagnosis or even misdiagnosis. Due to atypical clinical or imaging manifestations, ruptured intracranial aneurysms have been reported to be misdiagnosed as meningitis, tumors, stroke, or trauma, among other conditions[1-3]. Here, we report what appears to be the first case of a ruptured intracranial aneurysm presenting as cerebral circulation insufficiency. The literature on the misdiagnosis of intracranial aneurysms with atypical clinical manifestations is reviewed.
A 45-year-old man was admitted to our hospital with recurrent transient losses of consciousness and a serendipitous parasellar lesion.
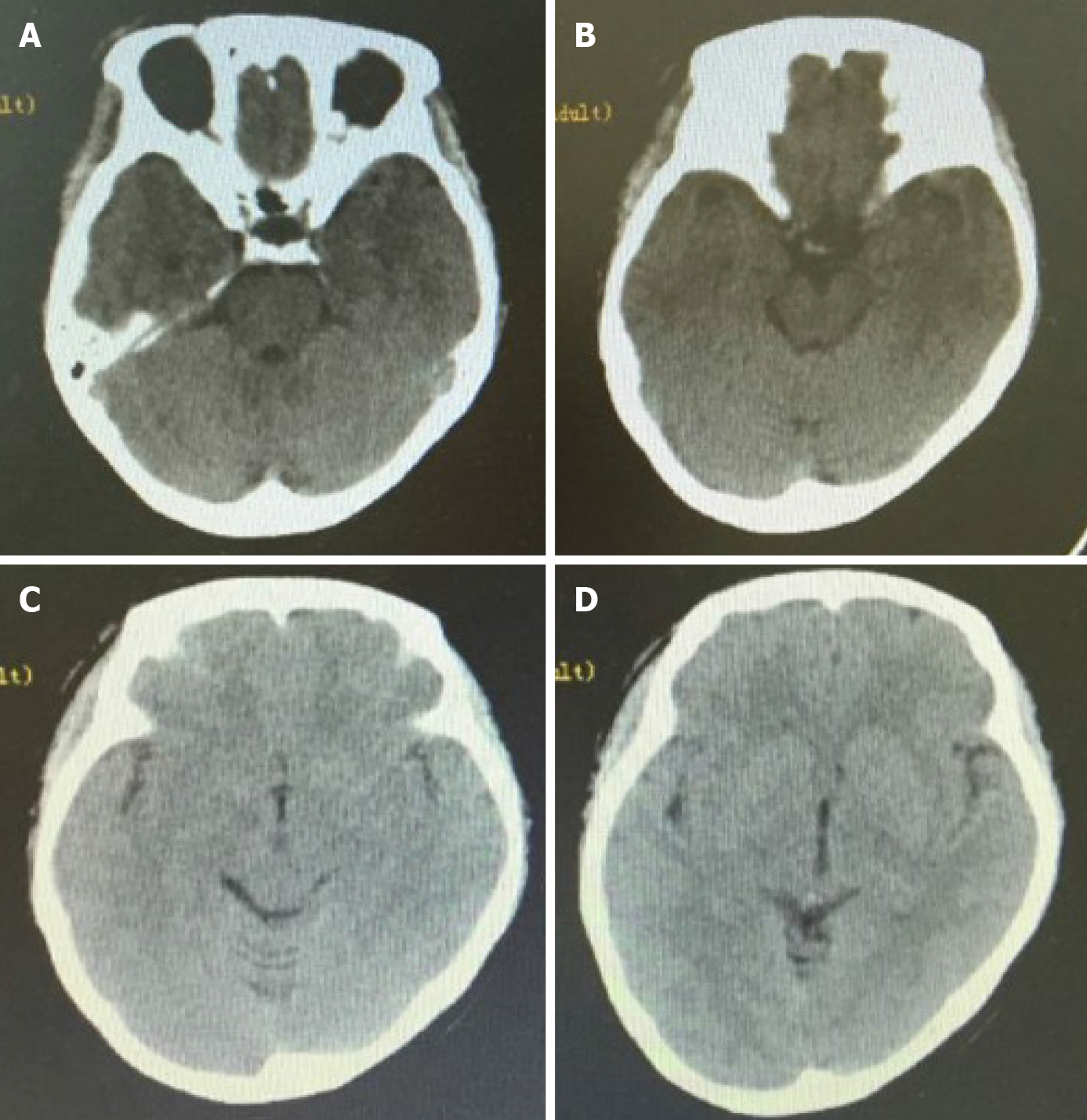
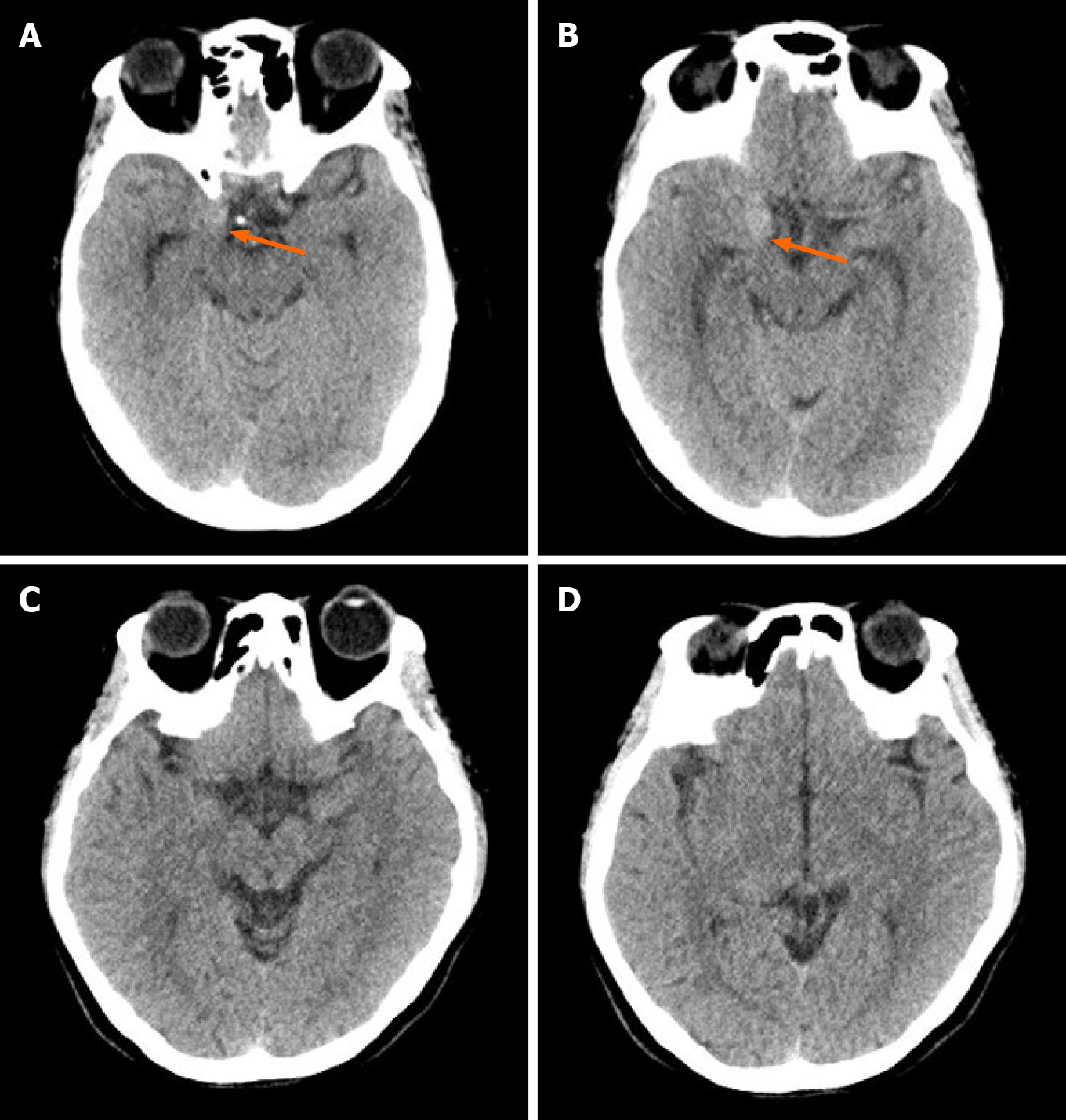
According to his account, the patient had suffered three brief periods (tens of seconds) of an unexplained loss of consciousness within 8 mo. No attack was accompanied by headaches, vomiting, or convulsions. On the first two occasions, he was admitted to two local hospitals and underwent repeated noncontrast computed tomography (CT) scans (Figure 1), electroencephalograms, electrocardiograms, carotid ultrasound, cardiac ultrasound, transcranial Doppler, and measurements of blood glucose, blood lipid, and hemoglobin levels. Since no abnormality was detected in the previous examinations, he was diagnosed with and treated for cerebral circulation insufficiency twice. During the last event, the patient had suddenly lost consciousness for tens of seconds while riding a motorcycle and caused an accident. An emergency CT scan did not reveal subarachnoid hemorrhage (SAH), but unexpectedly showed an abnormal density on the right side of the sella while the patient received trauma-related treatment at the nearest emergency center (Figure 2). Therefore, he was advised to go to a superior hospital.
This patient did not have a history of cardio-cerebrovascular diseases or neurological diseases.
The patient denied a family history of hypertension, stroke, or psychiatric disorders.
Upon admission, no abnormalities in the central nervous system were identified.
Upon admission, the patient underwent a blood cell analysis and examinations of blood electrolyte, blood glucose, blood lipid, liver function, renal function, and adenohypophysial hormone levels. The test results were all normal, except for a slight increase in the white blood cell count (11.56 × 109/L) and neutrophil count (6.65 × 109/L).
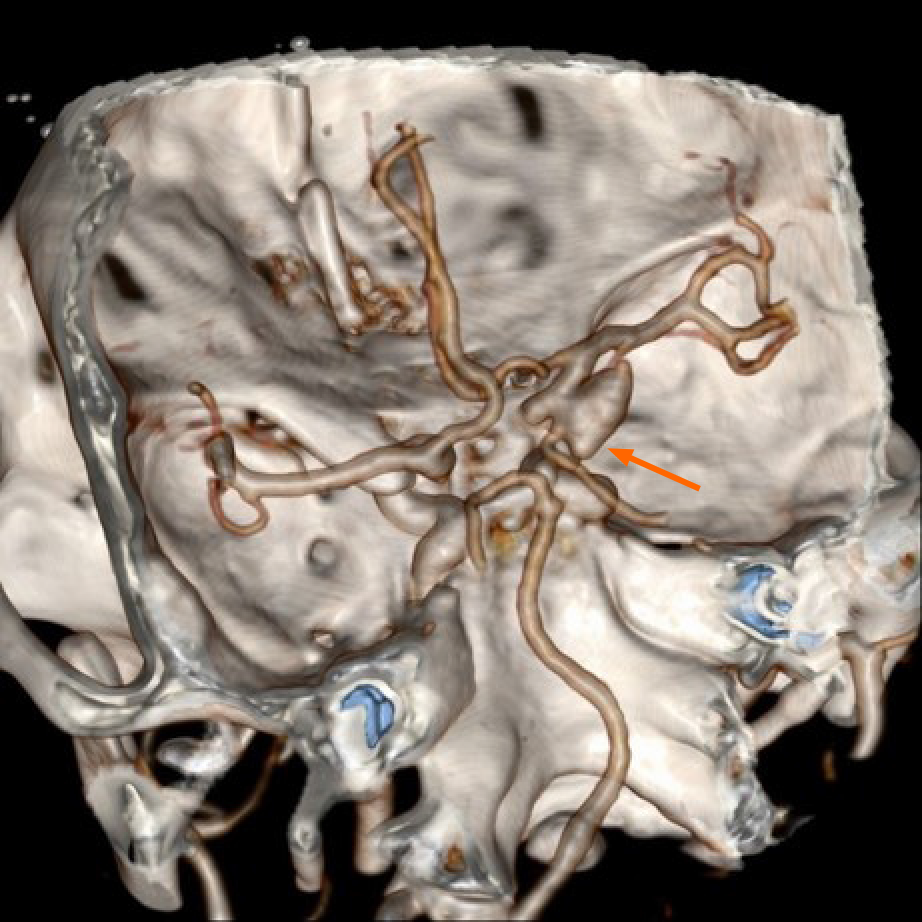
CT angiography (CTA) was performed immediately and revealed a morphologically irregular cystic aneurysm of the right internal carotid artery. The aneurysm had multiple sacs pointing in different directions, and the longest diameter of the aneurysm was approximately 11 mm (Figure 3).
The patient was ultimately diagnosed with an aneurysm in the right internal carotid artery. According to the characteristics of aneurysmal images, the aneurysm was judged to be prone to bleeding.
The patient was treated by a pterional craniotomy and clipping of the aneurysm neck under general anesthesia on the fifth day after the accident. During the operation, we observed a few scattered blood clots in the subarachnoid space, obvious adhesions around the aneurysm neck and sac, and a definite crevasse at the location of the aneurysmal apex. After the aneurysm neck was carefully separated and exposed, an arc-shaped aneurysm clip was used to close the aneurysmal neck away from the internal carotid artery. We temporarily blocked the internal carotid artery and adjusted the clip many times to completely clip the aneurysm neck and protect the posterior communicating artery, but the aneurysm did not rupture. Therefore, we confirmed that the aneurysm was a saccular ‘‘true’’ aneurysm that had ruptured before.
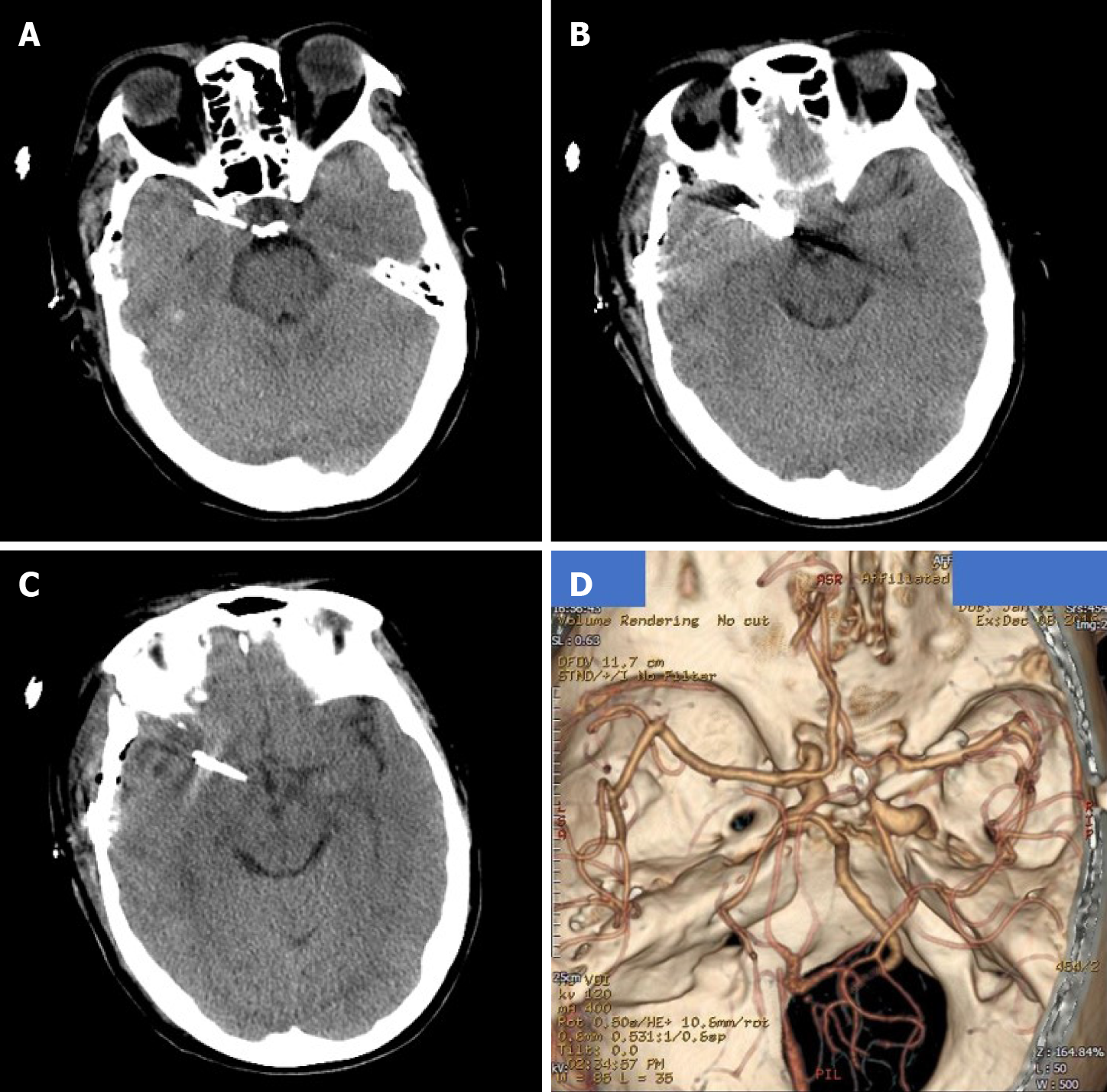
The patient completely recovered and was discharged without neurological deficits after 14 d. Both noncontrast CT (Figure 4A-C) and CTA images (Figure 4D) recorded before discharge showed satisfactory results. The 6-mo telephone follow-up revealed a good prognosis.
The rate of aneurysmal misdiagnosis reported in the literature has decreased from as high as 25% 20 years ago to 1.14% recently[4,5]. However, once misdiagnosed, aneurysmal rebleeding may cause very serious consequences and even death, and clinicians should therefore still focus on the occurrence of an aneurysmal misdiagnosis. Regarding the reasons for the misdiagnosis of ruptured intracranial aneurysms, a retrospective analysis of 2898 patients with aneurysmal SAH performed by Oh et al[5] showed that patients who presented with an initially good Hunt-Hess grade and a lower Fisher’s grade who were visiting non-teaching hospital for their initial contact were at risk of being misdiagnosed. The conclusions of the studies by Takagi et al[6] and Inagawa et al[7] are also consistent with this hypothesis. In addition, ruptured intracranial aneurysms are often misdiagnosed and missed because they are combined with craniocerebral trauma. Between 2.8% and 28% of ruptured aneurysms may be associated with a traumatic brain injury, and in a large series, SAH was detected in 39% of 753 patients with a severe head injury[8,9]. However, the relationship between trauma and the rupture of the aneurysm is controversial, and a causal relationship might be difficult to ascertain. The relationships between head injury and pre-existing aneurysms are summarized below. First, the rupture of the aneurysm causes the trauma. Second, a head impact causes the rupture of the aneurysm. Third, an unruptured aneurysm is incidentally discovered during the evaluation of head trauma. Kim et al[10] suggested that from the perspective of CT findings, SAH in the basal cisterns extended into the bilateral sylvian fissures and anterior interhemispheric fissure, and SAH in the unilateral sylvian fissure or associated with intraparenchymal hemorrhage identified on the initial CT scan might predict the rupture of a pre-existing cerebral aneurysm.
In our case, no obvious SAH was observed on either CT scan after the first two episodes, and the patient was misdiagnosed with cerebral circulatory dysfunction twice. However, according to the intraoperative conditions and the final diagnosis, the possibility of aneurysm rupture should have been considered in the first two attacks. Another hypothesis is that the patient experienced premonitory symptoms of the rupture of intracranial aneurysms twice. We were unable to clearly determine whether SAH was not present on these CT scans. According to the literature, in addition to equipment factors, some minor signs of SAH may be ignored by inexperienced clinical or imaging doctors who may, for example, misread the presence of a low level of hemorrhaging, fissure or sulci obliteration, or both low levels of hemorrhaging and fissure obliteration[5]. After the third episode, a lesion with an abnormal density was observed on the right side of the sella that had not been detected on the previous two CT scans. We speculate that the patient may have experienced a rare sudden enlargement of the aneurysm after the second onset of symptoms, as previously described by Miller et al[11] and Khan et al[12]. Previous reports of the rapid growth of cystic aneurysms show that this condition often occurs in patients with atrial myxoma, inflammatory aneurysms, drug abuse, and blood vesicular aneurysms[13-16], and its causes have been reported to be related to pregnancy, surgery, hypertension, and sex[17,18]. However, all of the aforementioned factors were excluded based on the patient’s medical history, except a suspicious history of trauma. Moreover, the relationship between the rapid growth of the aneurysms and trauma is uncertain. Based on the available information, we were unable to clearly determine whether the sudden enlargement of the aneurysm was caused by trauma or led to the trauma.
In general, the possibility of traumatic aneurysms should be considered when intracranial aneurysms are detected after head trauma in patients with no positive results on previous CT scans. However, in our patient, an intracranial aneurysm was detected on a CT examination performed within 24 h, and no clinical symptoms or imaging findings indicating a skull base fracture were identified after injury. In addition, we observed a gap between the aneurysm, the cavernous sinus, and the anterior bed process on the CTA scan. None of the information presented above supported a preoperative diagnosis of a traumatic aneurysm. The intraoperative findings also confirmed our diagnosis. Traumatic aneurysms account for less than 1% of all intracranial aneurysms, and its incidence is slightly higher in adolescent and infant patients than in adults[19]. Traumatic pseudoaneurysms are usually associated with blunt or shearing forces on a vessel lying against a fixed surface, such as the skull base, or due to a direct injury over the convex surface of the skull, and always present a unique challenge during both the diagnosis and treatment phases. The average time from the initial trauma to the onset of traumatic aneurysm bleeding is approximately 3 wk[20]. Due to the absence of a neck, the presence of a poorly defined wall, and the association of arachnoid adhesions in the former, traumatic aneurysms are more likely to rupture during surgical clipping than a congenital aneurysm[21]. Surgical intervention is needed as soon as a traumatic aneurysm is diagnosed. Surgery has been shown to reduce the mortality rate of patients with posttraumatic aneurysms from 40-50% to 18%[22]. To our knowledge, very few studies have compared the outcomes of surgical clipping with endovascular occlusion in patients with these aneurysms. Due to the atypical characteristics of these aneurysms, treatment should be individualized.
To the best of our knowledge, this case study is the first to report a patient with an intracranial aneurysmal rupture presenting as cerebral circulation insufficiency. Our report also describes a rare case of short-term dilated intracranial cystic aneurysm. Consistent with previous reports, mild clinical symptom is an important cause of misdiagnosis and missed diagnosis, while a combined history of trauma increases the difficulty of determining a differential diagnosis. A detailed understanding of the trauma process and imaging data is very important to achieve a timely and correct diagnosis. In addition, active CTA screening in patients with suspected SAH is helpful to avoid missing intracranial aneurysms.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Chinese Medical Association, No. 2300000870.
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Matowicka-Karna J S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Michael PG, Jamkhandikar RM, Memon IK, Al-Saadi T, Al-Aghbari S, Al-Muqaimi M, Ansari M, Al-Shamakhi A, Ahmad A. Unusual Case of an Intracranial Aneurysm Misdiagnosed as Focal Basal Meningitis. Sultan Qaboos Univ Med J. 2017;17:e363-e365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Song SY, Kim DW, Park JT, Kang SD. Delayed Rebleeding of Cerebral Aneurysm Misdiagnosed as Traumatic Subarachnoid Hemorrhage. J Cerebrovasc Endovasc Neurosurg. 2016;18:253-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Xu K, Yuan Y, Zhou J, Yu J. Pituitary adenoma apoplexy caused by rupture of an anterior communicating artery aneurysm: case report and literature review. World J Surg Oncol. 2015;13:228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Mayer PL, Awad IA, Todor R, Harbaugh K, Varnavas G, Lansen TA, Dickey P, Harbaugh R, Hopkins LN. Misdiagnosis of symptomatic cerebral aneurysm. Prevalence and correlation with outcome at four institutions. Stroke. 1996;27:1558-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 102] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Oh SY, Lim YC, Shim YS, Song J, Park SK, Sim SY, Kim MJ, Shin YS, Chung J. Initial misdiagnosis of aneurysmal subarachnoid hemorrhage: associating factors and its prognosis. Acta Neurochir (Wien). 2018;160:1105-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Takagi Y, Hadeishi H, Mineharu Y, Yoshida K, Ogasawara K, Ogawa A, Miyamoto S. Initially Missed or Delayed Diagnosis of Subarachnoid Hemorrhage: A Nationwide Survey of Contributing Factors and Outcomes in Japan. J Stroke Cerebrovasc Dis. 2018;27:871-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Inagawa T. Delayed diagnosis of aneurysmal subarachnoid hemorrhage in patients: a community-based study. J Neurosurg. 2011;115:707-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Hsieh CT, Lin EY, Tsai TH, Chiang YH, Ju DT. Delayed rupture of pre-existing cerebral aneurysm in a young patient with minor head trauma. J Clin Neurosci. 2007;14:1120-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Eisenberg HM, Gary HE Jr, Aldrich EF, Saydjari C, Turner B, Foulkes MA, Jane JA, Marmarou A, Marshall LF, Young HF. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg. 1990;73:688-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 397] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 10. | Kim YO, Kim GT, Choi HJ. Prediction of Rupture of Pre-existing Cerebral Aneurysm by CT Findings in Patients with Traumatic Brain Injury. J Korean Soc Emerg Med. 2014;25:602-610. |
| 11. | Miller NR, Savino PJ, Schneider T. Rapid growth of an intracranial aneurysm causing apparent retrobulbar optic neuritis. J Neuroophthalmol. 1995;15:212-218. [PubMed] |
| 12. | Khan RB, Laster RE, Bertorini TE. Rapid growth of a basilar aneurysm. Am J Med Sci. 2000;320:281-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Suzuki T, Nagai R, Yamazaki T, Shiojima I, Maemura K, Yamaoki K, Tanaka N, Machida T, Kotsuka Y, Furuse A. Rapid growth of intracranial aneurysms secondary to cardiac myxoma. Neurology. 1994;44:570-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Lee CC, Hsieh TC, Wang YC, Lo YL, Lee ST, Yang TC. Ruptured symptomatic internal carotid artery dorsal wall aneurysm with rapid configurational change. Clinical experience and management outcome: an original article. Eur J Neurol. 2010;17:1277-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Koffie RM, Stapleton CJ, Torok CM, Yoo AJ, Leslie-Mazwi TM, Codd PJ. Rapid growth of an infectious intracranial aneurysm with catastrophic intracranial hemorrhage. J Clin Neurosci. 2015;22:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Fowler J, Fiani B, Quadri SA, Cortez V, Frooqui M, Zafar A, Ahmed FS, Ikram A, Ramachandran A, Siddiqi J. Impact of Methamphetamine Abuse: A Rare Case of Rapid Cerebral Aneurysm Growth with Review of Literature. Case Rep Neurol Med. 2018;2018:1879329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Anda T, Yonekura M, Baba H, Suyama K, Toda K, Kamada K, Ono T, Yoshida K, Baba S, Onizuka M. Factors affecting rapid growth of unruptured cerebral aneurysms during the acute stage of subarachnoid hemorrhage. Neurol Res. 2006;28:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Prandini MN, Lacanna SN, Tella OI, Bonatelli AP. Aneurysm growth after brain tumor removal: case report. Arq Neuropsiquiatr. 2004;62:722-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Bhaisora KS, Behari S, Godbole C, Phadke RV. Traumatic aneurysms of the intracranial and cervical vessels: A review. Neurol India. 2016;64 Suppl:S14-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Holmes B, Harbaugh RE. Traumatic intracranial aneurysms: A contemporary review. J Trauma. 1993;35:855-860. [PubMed] |
| 21. | Levy ML, Rezai A, Masri LS, Litofsky SN, Giannotta SL, Apuzzo ML, Weiss MH. The significance of subarachnoid hemorrhage after penetrating craniocerebral injury: correlations with angiography and outcome in a civilian population. Neurosurgery. 1993;32:532-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Mao Z, Wang N, Hussain M, Li M, Zhang H, Zhang Q, Zhang P, Zhi X, Ling F. Traumatic intracranial aneurysms due to blunt brain injury-a single center experience. Acta Neurochir (Wien). 2012;154:2187-2193; discussion 2193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |