Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.6110
Peer-review started: March 25, 2021
First decision: May 11, 2021
Revised: May 20, 2021
Accepted: June 1, 2021
Article in press: June 1, 2021
Published online: July 26, 2021
Processing time: 118 Days and 0.8 Hours
Generalized periodontitis is a severe periodontal disease characterized by rapid periodontal destruction in healthy persons. This case report describes the treatment of a severe crowding, large overjet, and occlusal collapse due to the loss of anterior guidance with generalized periodontitis.
A 35-year-old female patient with a chief complaint of crowding and maxillary protrusion was diagnosed with generalized periodontitis by clinical and radiographic examinations. To improve crowding and overjet, orthodontic treatment was performed after basic periodontal therapy. Severely damaged upper right lateral incisor and left canine were extracted, and lower right first premolar and left second premolar were also removed to treat severe crowding. After orthodontic treatment, periodontal flap surgery for upper left molars and guided tissue regeneration for the lower left second molar was performed. Then, a dental implant was inserted in the upper left canine legion. The esthetics of the maxillary anterior tooth was improved by prosthetic restorations. The treatment result showed a well-improved occlusion with proper anterior guidance and healthy periodontal tissue after a retention period of 10 years.
Periodontal, orthodontic, and prosthodontic treatments are extremely useful to improve function and stable periodontal tissue for generalized periodontitis.
Core Tip: Generalized periodontitis causes malocclusion by severe periodontal destruction. Little information is available on the long-term occlusal stability for generalized periodontitis. In this case report, we demonstrated that periodontal, orthodontic and prosthodontics are useful to improve long-term stability of occlusal function and healthy periodontal tissue for generalized periodontitis.
- Citation: Kaku M, Matsuda S, Kubo T, Shimoe S, Tsuga K, Kurihara H, Tanimoto K. Generalized periodontitis treated with periodontal, orthodontic, and prosthodontic therapy: A case report. World J Clin Cases 2021; 9(21): 6110-6124
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/6110.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.6110
Generalized periodontitis was first introduced as diffuse atrophy of the alveolar bone in 1923 by Gottlieb[1] and finally named as aggressive periodontitis in 1999 [2,3]. It is a rare and severe periodontal disease characterized by rapid periodontal destruction with loss of attachment in healthy persons[4]. Therefore, initial periodontal treatment and additional periodontal surgery should be performed if required for generalized periodontitis. Although it is considered that generalized periodontitis is a multi
Treatment planning in patients with generalized periodontitis are almost same as those in chronic periodontitis patients. The treatment phases are divided into general examination, initial treatment, re-evaluation, surgical treatment and maintenance for both types of periodontitis. The treatment goal of generalized periodontitis is to generate a health periodontal condition that can retain many teeth as long as possible[7]. Orthodontic treatment is essential for patients with generalized periodontitis to inhibit progression of periodontitis, because generalized periodontitis causes some pathologic tooth migration such as labial inclination, severe crowding and pathologic extrusion of anterior teeth as well as posterior occlusal collapse. B. Schacher, F. Baron, M. Roßberg, M. Wohlfeil, R. Arndt, and P. Eickholz, “Aggregatibacter actinomycetemcomitans as indicator for aggressive periodontitis by two analysing strategies,” Journal of Clinical Periodontology, vol. 34, no. 7, pp. 566–573, 2007. View at: Publisher SiteGoogle ScholarSee in References Generalized periodontitis sometimes induces posterior occlusal trauma caused by occlusal interference due to unfavorable anterior guidance. It is reported that an important factor for long-term occlusal stability is proper anterior guidance, and overjet and overbite is considered to control anterior guidance[8]. Hence, orthodontic treatment is necessary for these patients to improve overjet and overbite and restore posterior bite collapse along with esthetic problems. Although an orthodontic tooth movement for generalized periodontitis is challenging because of the possibility of deteriorating the periodontal condition, there are some case reports of this disease treated by orthodontic therapy[9,10]. However, little information is available on the long-term occlusal stability for generalized periodontitis by comprehensive dental treatment. In this case report, we demonstrated that periodontal, orthodontic, and prosthodontics treatments are useful to improve the long-term stability of occlusal function and healthy periodontal tissue for generalized periodontitis.
A 35-year and 6-mo-old female patient came to our hospital with a chief complaint, “My teeth are wobbly, and I have crooked and protruding teeth”.
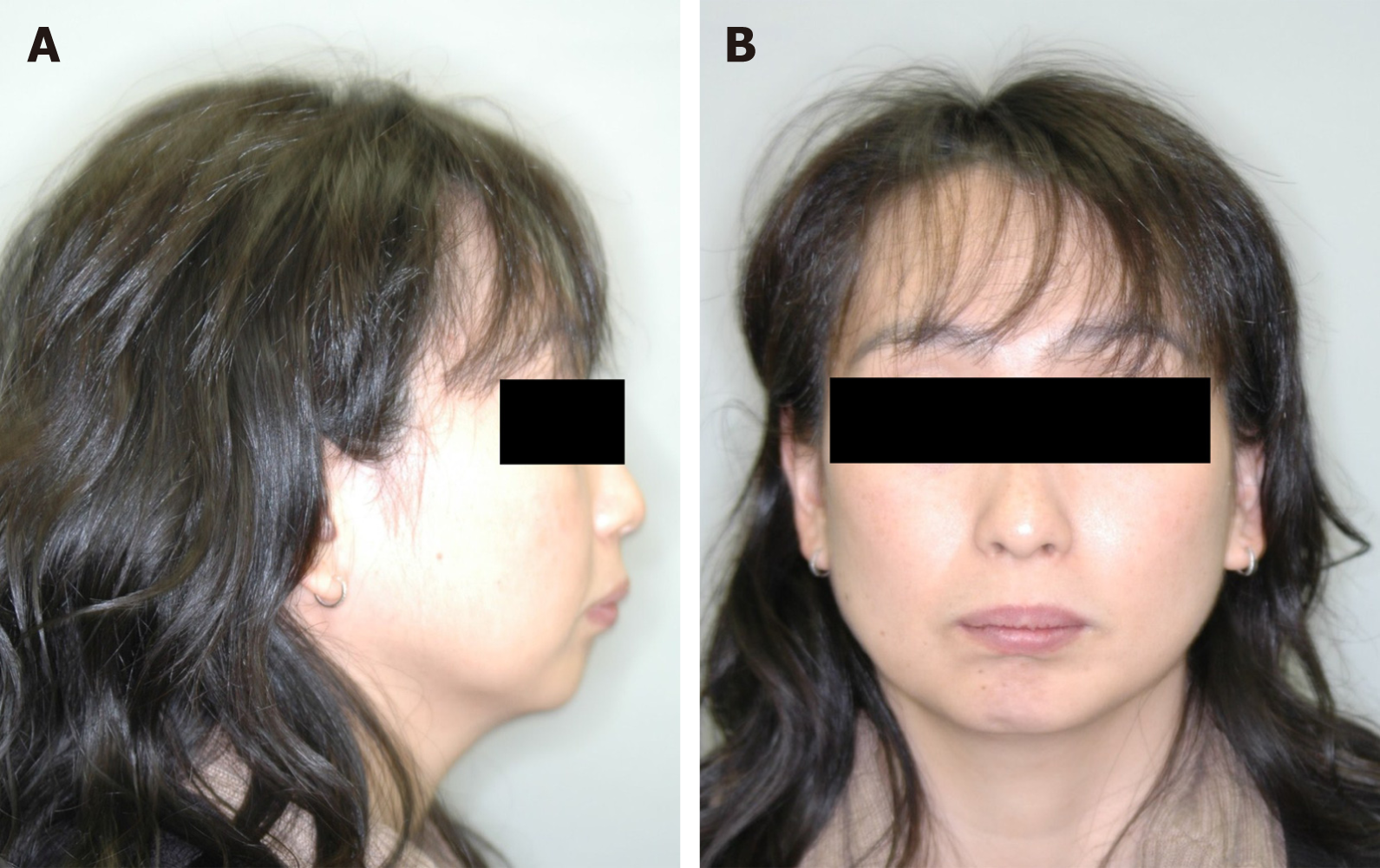
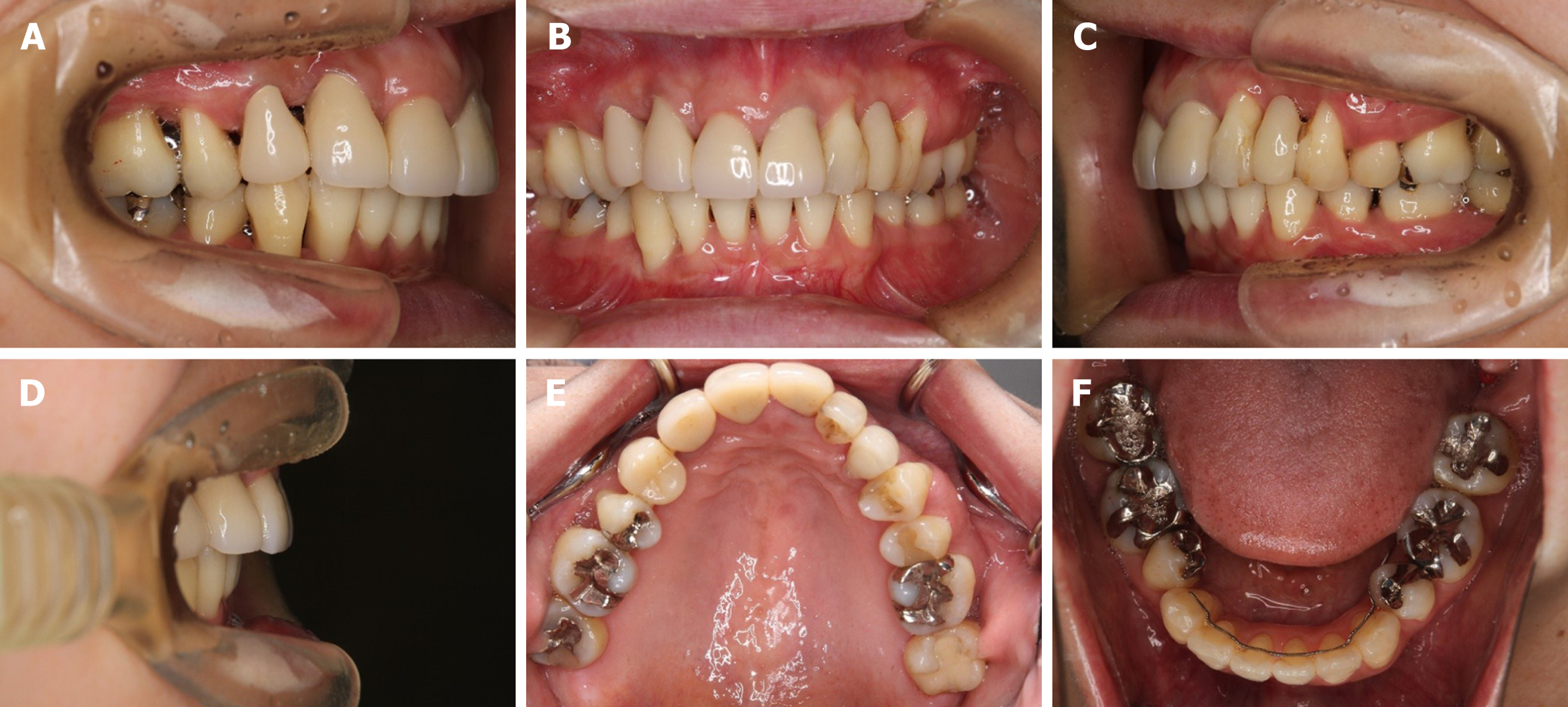
The patient complained teeth mobility in the upper anterior teeth region from the past 3 years. Although she was treated at a private practice, teeth mobility was not improved. So, the patient was referred to Hiroshima University Hospital by a general dentist for a full mouth periodontal evaluation and treatment. The pre-treatment facial photographs showed an average angle type and a convex profile with a retrognathic mandible (Figure 1). The intraoral photographs revealed a 9.5 mm overjet and 6.0 mm overbite. Both the right and left molar relationships were Class II. The upper incisors displaced labially and severe crowding was observed in the lower arch.
She did not have any history of systemic illness. Temporary splinting was applied from the upper right canine to the left first premolar to immobilize the loose tooth (Figure 2).
The patient did not have any history of smoking and her oral hygiene was poor. The patient’s father wore removable partial dentures.
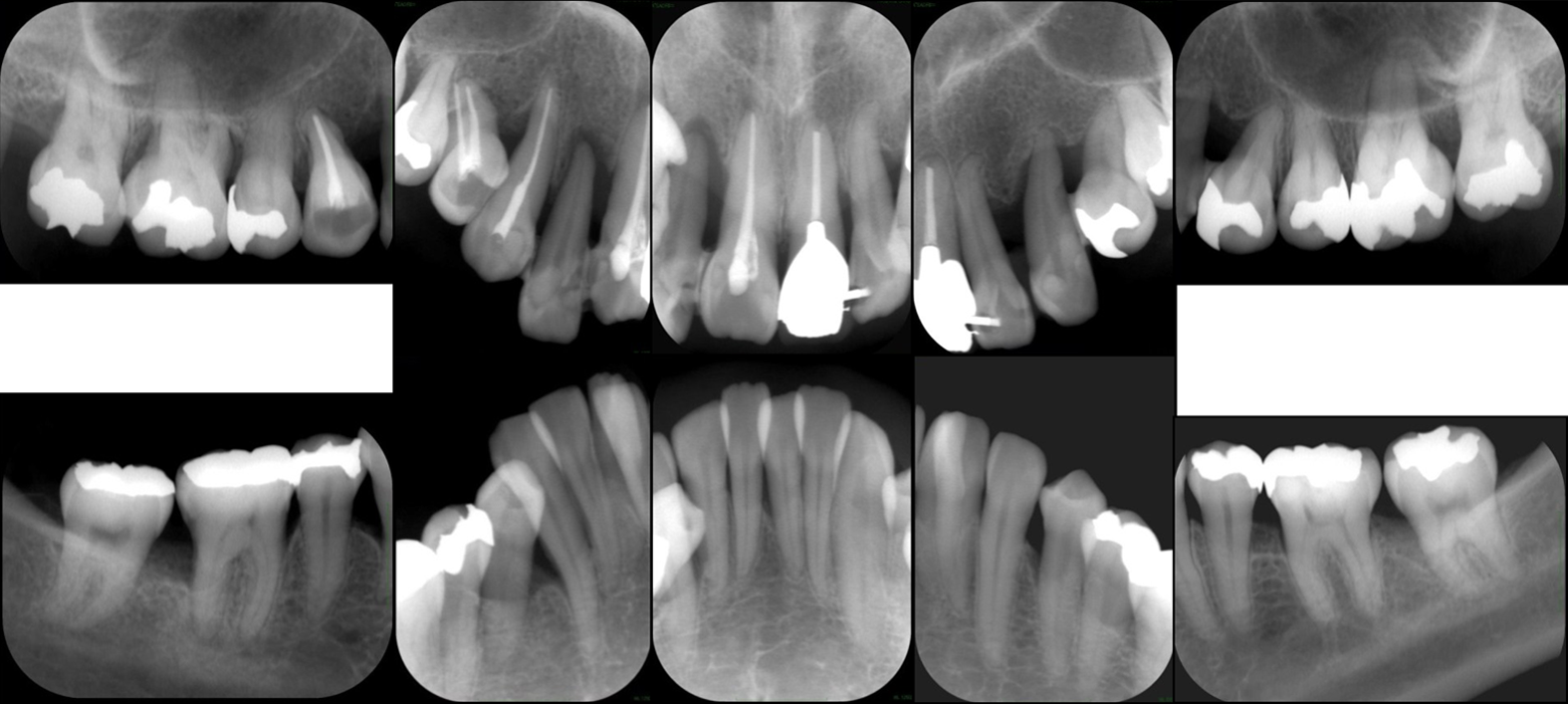
A panoramic radiograph and full-mouth set of dental radiographs showed severe alveolar bone loss; especially, the upper right lateral incisor and left canine were severely damaged without any alveolar bone support (Figure 3 and 4). Posterior occlusal interference on both sides was observed in the anterior and lateral guidance due to unfavorable anterior guidance. Redness and swelling were observed on upper gingiva. Initial periodontal examination showed dental plaque index; 50.9%, mean probing pocket depth; 4.3 mm, 4-6 mm; 40.5%, more than 7 mm; 14.3%, bleeding on probing; 61.9%, periodontal inflamed surface area[11]; 1725.7 mm2, tooth mobility of Miller classification (class 0; 2 teeth, class 1; 18 teeth, class 2; 7 teeth, class 3; 1 tooth) (Table 1).
| Maxilla | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (buccal) | 323 | 857 | 754 | 646 | 654 | 758 | 322 | 346 | 576 | 325 | 653 | 423 | 458 | 833 |
| Bleeding on probing | ++ | +++ | +++ | +++ | +++ | +++ | + | +++ | +++ | ++ | ++ | ++ | ++ | + |
| Pocket depth (palatal) | 834 | 448 | 324 | 466 | 664 | 579 | 433 | 438 | 586 | 888 | 663 | 333 | 368 | 633 |
| Bleeding on probing | ++ | +++ | ++ | +++ | +++ | +++ | + | ++ | +++ | +++ | ++ | ++ | ++ | |
| Tooth mobility | 1 | 1 | 1 | 2 | 2 | 3 | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 0 |
| Mandible | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (lingual) | 337 | 838 | 334 | 534 | 435 | 533 | 335 | 622 | 222 | 223 | 553 | 355 | 633 | 733 |
| Bleeding on probing | +++ | ++ | + | +++ | +++ | ++ | + | + | ++ | + | + | + | ||
| Pocket depth (buccal) | 434 | 934 | 333 | 556 | 554 | 423 | 324 | 463 | 323 | 323 | 423 | 323 | 423 | 834 |
| Bleeding on probing | + | ++ | + | +++ | + | + | + | +++ | + | + | + | +++ | ||
| Tooth mobility | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
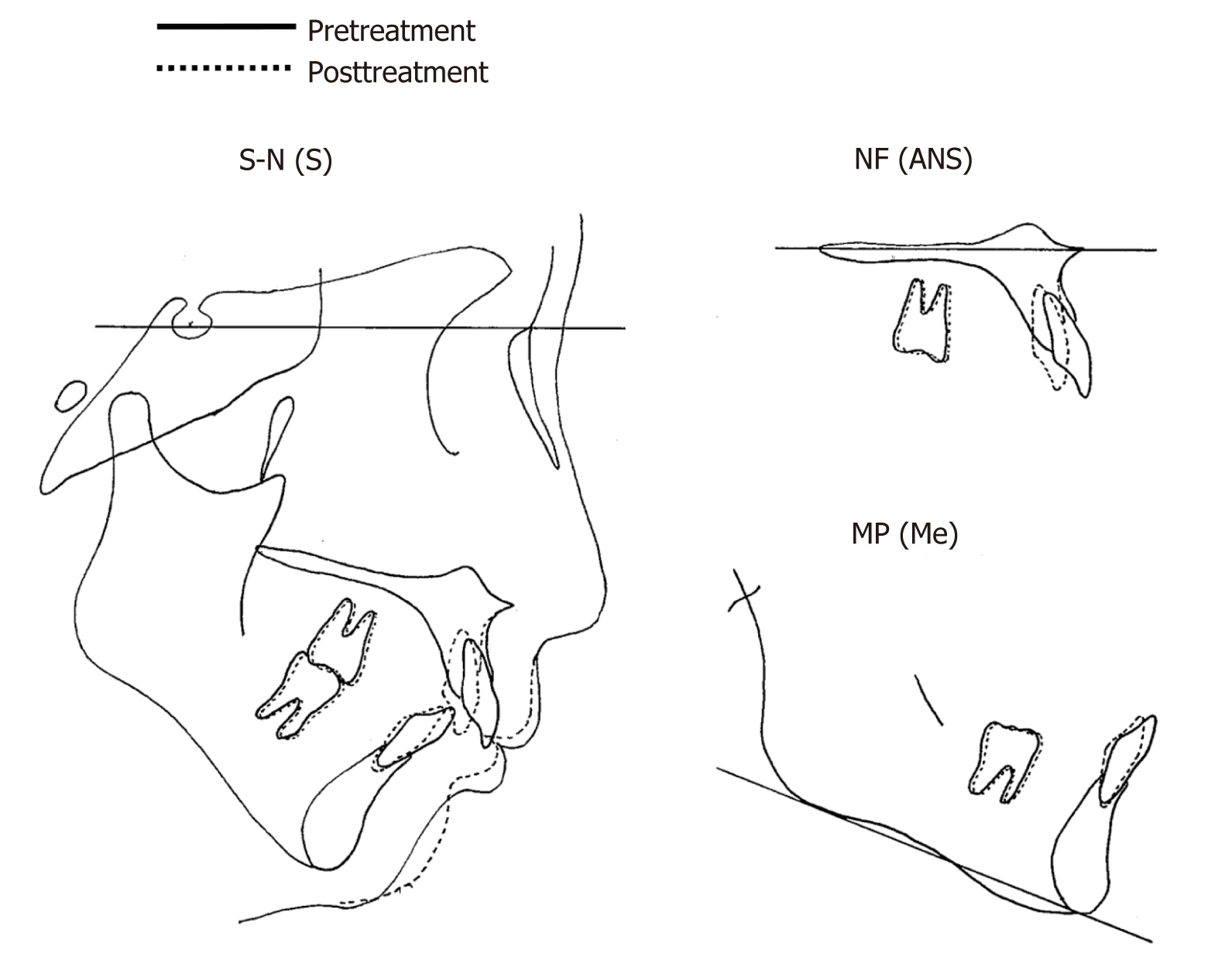
As shown in the cephalometric measurements, a skeletal Class II relationship (ANB angle, 10.0°) with a retrognathic mandible was observed. The labial inclination of the lower incisors (IMPA, 101.1°) was also evident (Table 2 and Figure 5).
| Measurements | Pre-treatment | Post-treatment | After 10 yr of retention |
| SNA (°) | 81.9 | 81.1 | 81.2 |
| SNB (°) | 71.9 | 72.0 | 72.0 |
| ANB (°) | 10.0 | 9.1 | 9.2 |
| FMA (°) | 32.0 | 32.1 | 32.1 |
| FMIA (°) | 46.9 | 54.4 | 54.2 |
| IMPA (°) | 101.1 | 93.5 | 93.6 |
| U1-FH (°) | 109.9 | 98.6 | 98.8 |
| Over jet (mm) | 9.5 | 5.0 | 5.2 |
| Over bite (mm) | 6.0 | 4.0 | 4.3 |
Based on the information, the patient was diagnosed with a generalized Stage III Grade C periodontitis[12] with skeletal Class II maxillary protrusion and severe crowding. First, we recommended initial periodontal therapy to reduce periodontal inflammation before orthodontic treatment. The treatment objectives essentially consisted of inflammation management and restoration of occlusal function. The treatment plan was as follows: (1) Initial periodontal treatment (full-mouth scaling and root planing, tooth brushing instruction); (2) Reexamination of periodontal condition; (3) Orthodontic treatment: (a) Extraction of the hopeless upper right lateral incisor and left canine; (b) Extraction of the lower right first premolar and left second premolar for orthodontic reasons; (c) Insertion of miniscrews into the mid-palatal area with a transpalatal arch; and (d) Lingual movement of the upper incisors and alignment of the lower arch; (4) Periodontal surgery; (5) Insert dental implant in the upper left canine legion; (6) Prosthodontic treatment; and (7) Supportive periodontal therapy.
Before the orthodontic treatment, an initial periodontal treatment including full-mouth scaling, root planing, and tooth brushing instruction was performed. One year after initiating the initial periodontal treatment, the patient showed significant improvement in the periodontal condition compared to that at the first examination; dental plaque index; 11.6%, mean probing pocket depth; 4.3 mm, 4-6 mm; 13.1%, more than 7 mm; 2.4%, bleeding on probing; 12.5%, periodontal inflamed surface area; 309.3 mm2, tooth mobility of Miller classification (class 0; 14 teeth, class 1; 13 teeth, class 2; 1 tooth, class 3; 0) (Table 3). Based on this reexamination, we decided to start orthodontic treatment (6 mo after the end of initial periodontal treatment).
| Maxilla | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (buccal) | 133 | 635 | 433 | 535 | 323 | 338 | 323 | 233 | 334 | 223 | 532 | 222 | 335 | 333 |
| Bleeding on probing | + | ++ | + | + | + | + | + | |||||||
| Pocket depth (palatal) | 333 | 335 | 333 | 335 | 533 | 338 | 333 | 333 | 335 | 345 | 332 | 323 | 233 | 323 |
| Bleeding on probing | + | + | ++ | + | + | + | ||||||||
| Tooth mobility | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 0 |
| Mandible | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (lingual) | 336 | 333 | 323 | 533 | 333 | 222 | 222 | 222 | 222 | 223 | 333 | 336 | 533 | 633 |
| Bleeding on probing | + | + | + | + | + | |||||||||
| Pocket depth (buccal) | 638 | 336 | 333 | 335 | 333 | 322 | 212 | 212 | 212 | 222 | 333 | 322 | 333 | 733 |
| Bleeding on probing | + | |||||||||||||
| Tooth mobility | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 |
The patient frequently received periodontal maintenance program during orthodontic treatment. The upper right lateral incisor, left canine, lower right first premolar and left second premolar were extracted. A 0.018-inch standard edgewise bracket was bonded on the upper and lower teeth. Under local anesthesia, two self-drilling titanium alloy miniscrews (2.0 mm in diameter and 6 mm in length, Dual Top Auto Screw; Jeil Medical Corp., South Korea) were inserted into the mid-palatal area. A transpalatal arch was placed and combined with miniscrews to prevent the mesial movement of the maxillary molars. After 2 years, the overjet and overbite decreased to 3.0 mm and 3.5 mm, respectively. The teeth were well aligned and proper anterior guidance was achieved. The edgewise bracket was removed and provisional restorations were set on the upper anterior tooth. After orthodontic treatment, the patient’s periodontal condition improved significantly: dental plaque index; 9.0%, mean probing pocket depth; 2.8 mm, 1-3 mm; 88.2%, 4-6 mm; 11.8%, more than 7 mm; 0%, bleeding on probing; 16.0%, periodontal inflamed surface area; 270.1 mm2, tooth mobility of Miller classification (class 0; 24 teeth, class 1; 0, class 2; 0, class 3; 0) (Table 4).
| Maxilla | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (buccal) | 323 | 434 | 323 | 323 | 322 | - | 322 | 323 | 323 | - | 533 | 323 | 335 | 533 |
| Bleeding on probing | + | + | + | + | ||||||||||
| Pocket depth (palatal) | 323 | 333 | 433 | 332 | 333 | - | 323 | 323 | 323 | - | 433 | 323 | 336 | 623 |
| Bleeding on probing | + | ++ | + | + | + | + | + | ++ | ||||||
| Tooth mobility | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Mandible | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (lingual) | 334 | 333 | 323 | - | 212 | 212 | 212 | 212 | 212 | 212 | - | 323 | 533 | 533 |
| Bleeding on probing | + | + | + | + | ||||||||||
| Pocket depth (buccal) | 334 | 434 | 323 | - | 323 | 412 | 222 | 323 | 312 | 212 | - | 323 | 333 | 623 |
| Bleeding on probing | + | + | + | + | + | |||||||||
| Tooth mobility | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
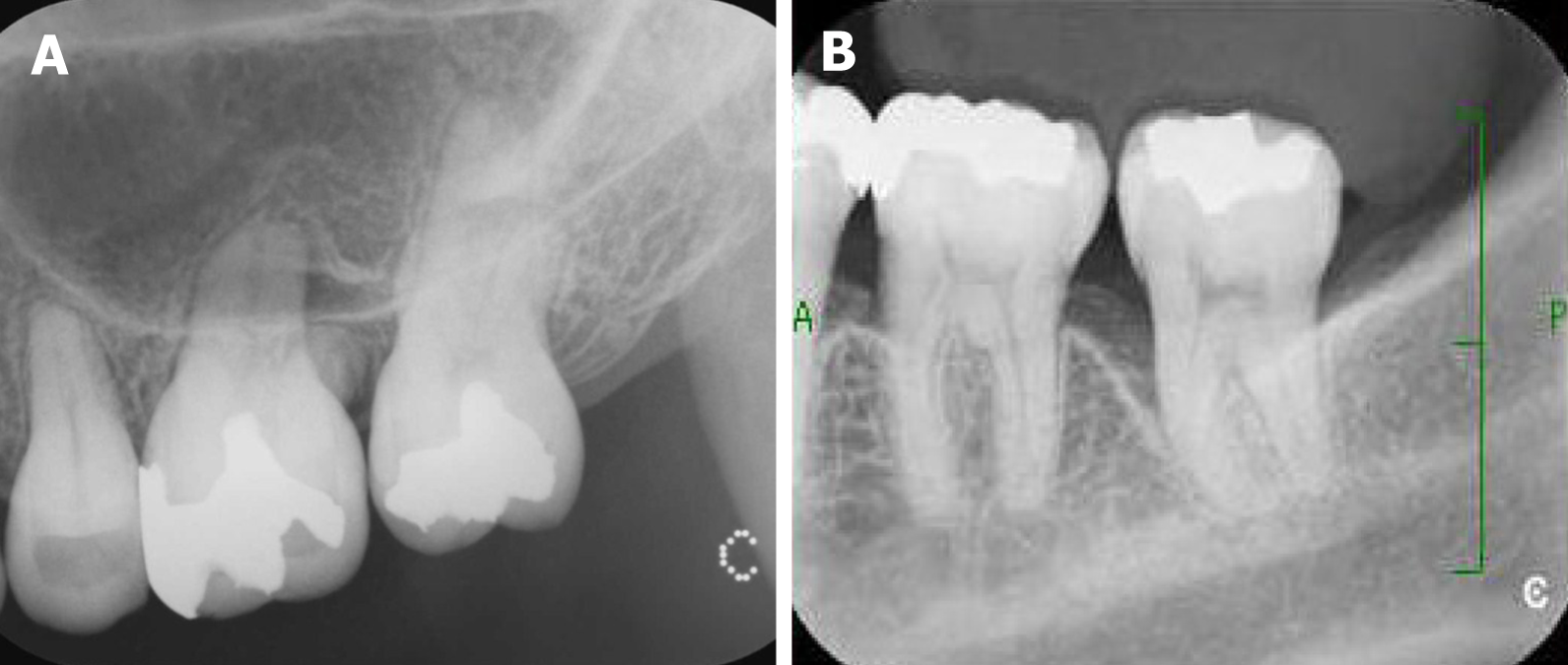
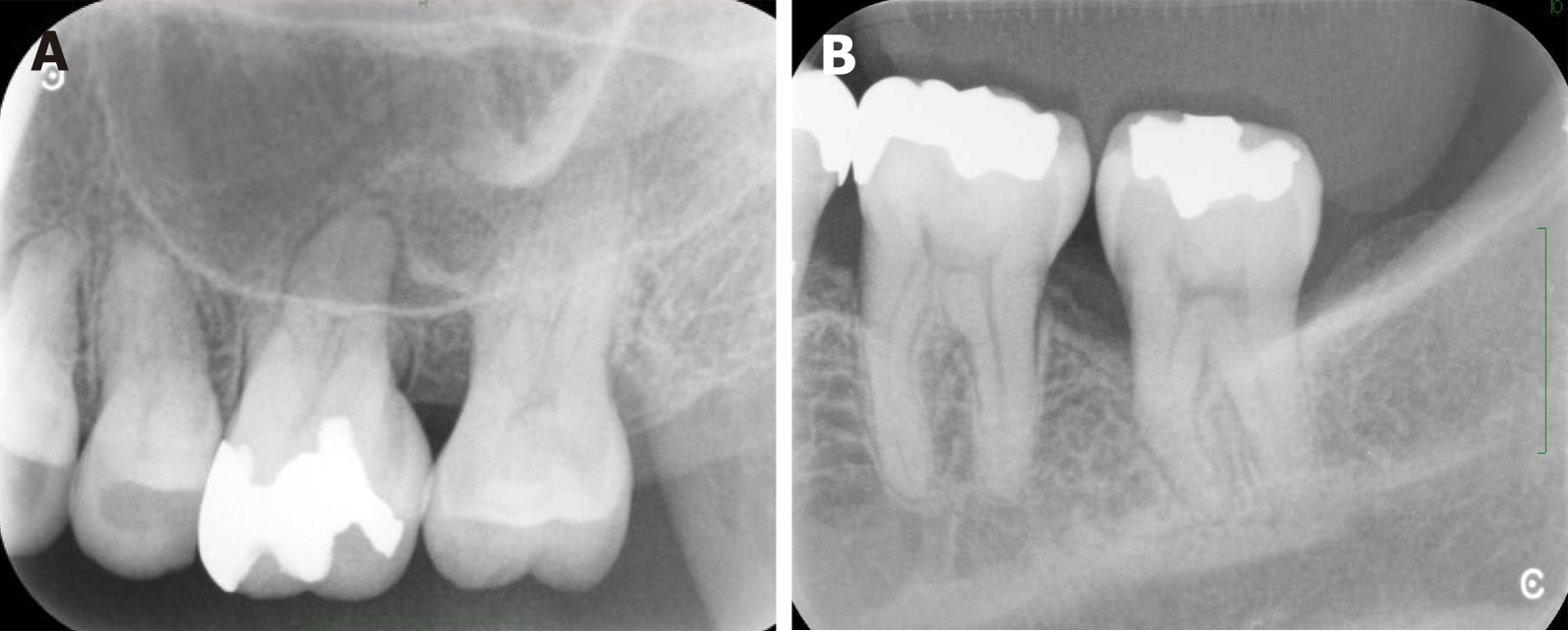
More than 5 mm of probing pocket depth area alveolar bone defect remained at both upper and lower left molars (Figure 6). Thus, periodontal flap surgery for the upper left first and second molars was performed. The surgery area was anesthetized by 2% lidocaine. The sulcular incision was made from mesial end of upper left first molar to distal end of upper left second molar. Next, a vertical incision was made and a periosteal flap was raised both on buccal and lingual part. Then, this area was completely debrided by curettes, and debris of calculus on the root surface was removed by scaling and root planning. Guided tissue regeneration for the lower left second molar was then performed. The 2% lidocaine was injected to buccal and lingual part of lower molars. The sulcular incision was performed both on the buccal and lingual sides of lower left first and second molars. Full-thickness elevations were made past the mucogingival junction both on the buccal and lingual side. The bony defect area and root surface were completely debrided. A bioresorbable poly lactic-co-glycolic acid membrane (GC MEMBRANE, GC Corp., Tokyo, Japan) was shaped appropriately and set on the bone defect area.
A dental implant (3.3 mm in diameter and 13 mm in length, Brånemark System Mk III, Nobel Biocare, Sweden) was inserted in the upper left canine legion and the final prosthetic restorations were set on the maxillary anterior tooth. The tooth remained stable, and healthy periodontal tissue was observed 10 years from the beginning of the retention by supportive periodontal therapy.
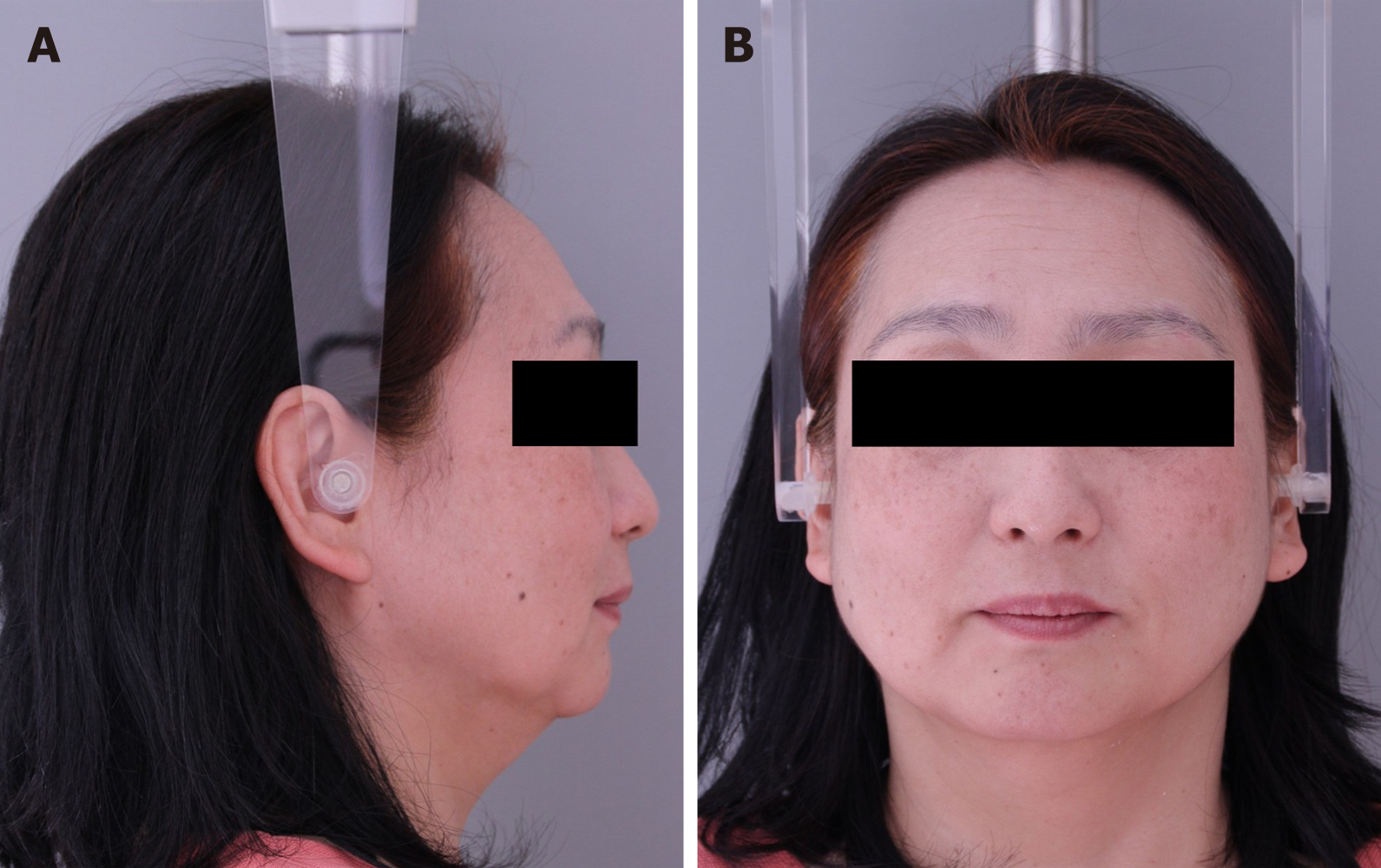
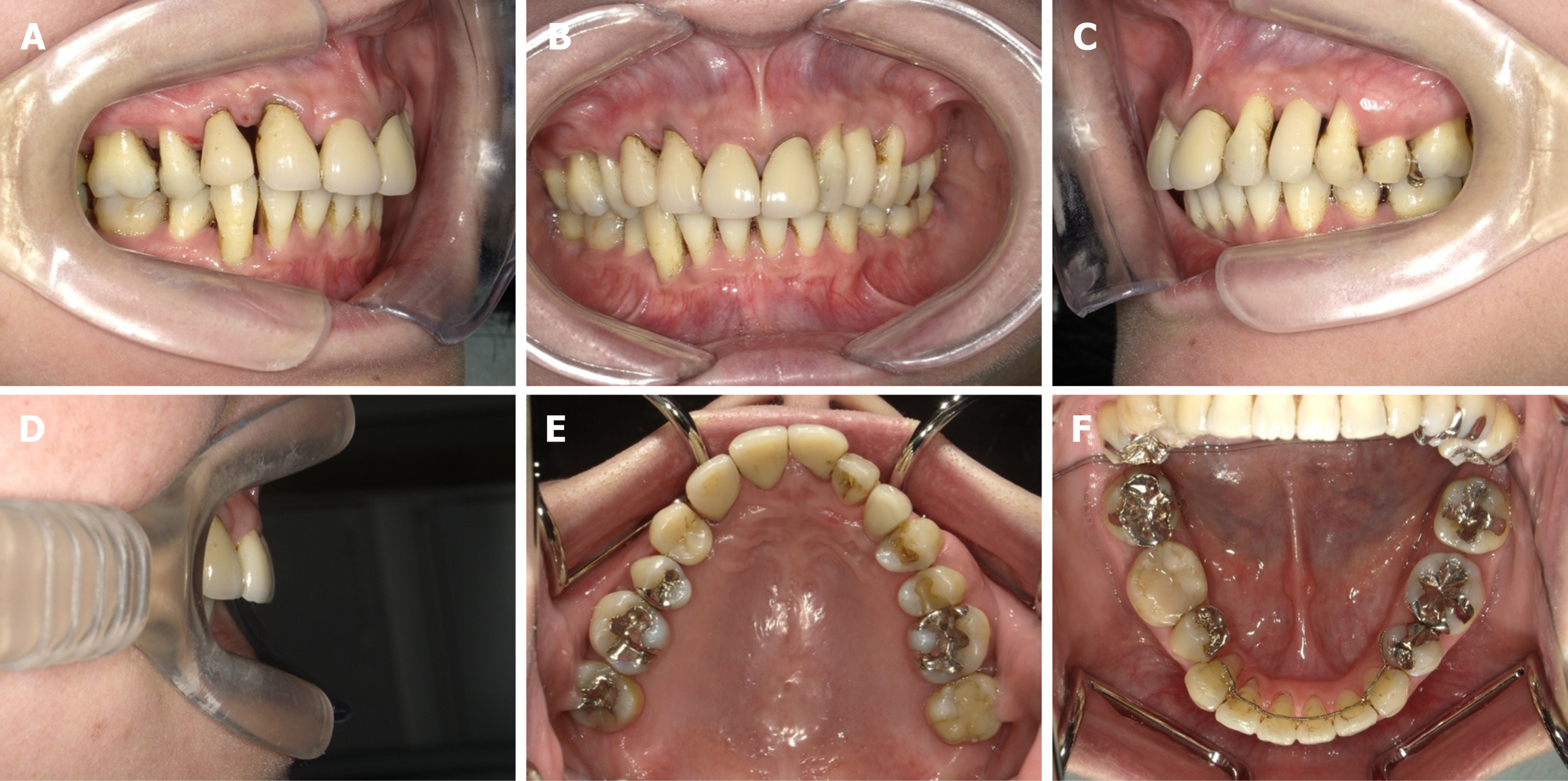
The facial profile significantly changed and the strain of the mentalis muscle became more relaxed than before (Figure 7). The overjet and overbite improved and proper anterior guidance was achieved (Figure 8). The post-treatment panoramic radiograph showed that all the roots were almost parallel (Figure 9). The cephalometric analysis showed that IMPA changed from 101.1° to 93.5° and the ANB angle changed from 10.0° to 9.1° (Table 2 and Figure 10 and 11). The dental radiograph on the upper and lower left molars showed alveolar bone regeneration by periodontal surgery (Figure 12). The patient’s periodontal examination at the beginning of supportive periodontal therapy showed dental plaque index; 8.0%, mean probing pocket depth; 2.5 mm (1-3 mm; 98.6%, 4-6 mm; 1.4%, more than 7 mm; 0%), bleeding on probing; 9.7%, periodontal inflamed surface area; 107.2 mm2, tooth mobility of Miller classification (class 0; 22 teeth, class 1; 2, class 2; 0, class 3; 0) (Table 5). No clinical changes were found after 10 years of retention when compared to the beginning of the retention (Table 2 and 6 and Figure 13).
| Maxilla | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (buccal) | 333 | 323 | 212 | 213 | 322 | - | 212 | 212 | 212 | - | 222 | 323 | 333 | 333 |
| Bleeding on probing | + | + | ||||||||||||
| Pocket depth (palatal) | 333 | 323 | 323 | 222 | 313 | - | 323 | 323 | 312 | - | 323 | 323 | 323 | 323 |
| Bleeding on probing | + | + | ++ | + | ||||||||||
| Tooth mobility | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Mandible | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (lingual) | 323 | 333 | 323 | - | 323 | 212 | 323 | 323 | 323 | 323 | - | 323 | 323 | 333 |
| Bleeding on probing | + | + | ++ | + | + | |||||||||
| Pocket depth (buccal) | 322 | 333 | 323 | - | 523 | 323 | 323 | 323 | 212 | 212 | - | 323 | 433 | 323 |
| Bleeding on probing | + | |||||||||||||
| Tooth mobility | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maxilla | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (buccal) | 333 | 323 | 212 | 212 | 322 | - | 212 | 212 | 212 | - | 323 | 212 | 223 | 223 |
| Bleeding on probing | + | |||||||||||||
| Pocket depth (palatal) | 323 | 323 | 212 | 222 | 212 | - | 212 | 222 | 212 | - | 212 | 323 | 323 | 323 |
| Bleeding on probing | + | |||||||||||||
| Tooth mobility | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | ||
| Mandible | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Pocket depth (lingual) | 323 | 323 | 323 | - | 323 | 322 | 212 | 212 | 212 | 212 | - | 212 | 323 | 323 |
| Bleeding on probing | + | |||||||||||||
| Pocket depth (buccal) | 322 | 323 | 212 | - | 323 | 212 | 212 | 212 | 212 | 212 | - | 212 | 323 | 323 |
| Bleeding on probing | + | |||||||||||||
| Tooth mobility | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
In the present case, the patient was middle-aged with no systemic disorders with a familial history of periodontal issues. Moreover, because attachment loss affecting at least three permanent teeth characterizing generalized periodontitis[13] was observed, we diagnosed this patient with a generalized periodontitis. For the treatment of generalized periodontitis, which shows a wide-ranging decrease in the surrounding alveolar bone and pathologic migration of the tooth, control of the periodontal inflammation and restoration of occlusal function are important[10]. Especially, in this patient, posterior occlusal interference was observed in the anterior and lateral guidance. Therefore, we planned occlusal reconstruction by orthodontic treatment after periodontal therapy. Usually, to reduce microorganisms, non-surgical and surgical treatment is provided[14], and this is divided into two periodontal treatment times. One is to perform the periodontal treatment before the beginning of orthodontic treatment, and the other is to provide periodontal treatment simultaneously with the orthodontic treatment. In patients with active periodontal disease, it is possible that orthodontic treatment may cause further progressive periodontal destruction[15]. On the other hand, tooth movement can improve attachment levels in reduced periodontium, suggesting that orthodontic treatment should be performed at an early stage. Zasčiurinskienė et al[16] compared the effect of orthodontic treatment on the periodontal status between control patients who received periodontal treatment before the beginning of orthodontic treatment and a test group that received periodontal treatment simultaneously with orthodontic treatment. Their results showed that both groups exhibited an increase in the clinical attachment level and reduction in the probing depth. No difference in gingival recession development was observed between the two groups. However, total periodontal-orthodontic treatment time was significantly longer for the control group. Accordingly, they recommended that orthodontic treatment and periodontal treatment should be performed simultaneously. Therefore, we provided orthodontic treatment immediately after the initial periodontal treatment, and not after surgical periodontal therapy.
In this patient, 1-year of initial periodontal treatment with full-mouth scaling, root planing and tooth brushing instruction were effective for the periodontal condition. Thus, we initiated orthodontic treatment for proper anterior guidance and to improve crowding. In cases of severe periodontitis in adults, s skeletal anchorage system is useful for the retraction of incisors, because it is difficult to obtain suitable molar anchorage in patients with periodontitis without proper periodontal support. Fukunaga et al[17] reported that skeletal anchorage is useful for the retraction and intrusion of upper incisors in cases of maxillary protrusion with severe adult periodontitis. Miniplates[18-20] and miniscrews[21-23] are now frequently used to establish absolute anchorage for adult orthodontic patients. However, miniscrews have been frequently used because surgical invasion is minimal compared to miniplates. Thus, we chose miniscrews in this patient with loss of alveolar bone to gain proper anchorage. As a result of the orthodontic treatment, the overjet improved and proper anterior guidance was achieved. The patient’s periodontal condition improved overall, except in both the upper and lower left molars. These results suggested that reconstruction of proper anterior guidance by orthodontic treatment is very important to disclude the balancing side, which resulting in the improvement of overall clinical attachment level especially in patients with generalized periodontitis. However, because the improvement in flap surgery and guided tissue regeneration was better at the upper and lower left molar sections of this patient, it is clear that periodontal surgery is necessary for cases of severe generalized periodontitis.
Recently, dental implants have been widely used to treat patients who lost their teeth, and long-term prognosis for implant therapy have been provided[24,25]. Although implant restoration is challenging in patients with generalized periodontitis[26], it is reported that implant loss and surrounding bone loss in patients with generalized periodontitis were not significantly larger than that in periodontally healthy patients or patients with chronic periodontitis[27]. For patients with generalized periodontitis, implant treatment should be recommended in patients who can receive continuous periodontal therapy. Additionally, in the present case, a dental implant in the upper left canine legion survived without any clinical symptoms such as peri-implantitis by continuous supportive periodontal therapy. Thus, healthy periodontal tissue and occlusal reconstruction for patients with generalized periodontitis can be achieved by periodontal, orthodontic, and prosthodontic treatment.
This case report showed that a comprehensive treatment including periodontal, orthodontic, and prosthodontic treatments can be useful in improving occlusal function and achieving long-term stability in periodontal tissue for generalized periodontitis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhatsange A, Dharmarajan G S-Editor: Gao CC L-Editor: A P-Editor: Zhang YL
| 1. | Gottlieb B. Die diffuse atrophy des alveolarknochens. Z Stomatol. 1923;21:195. |
| 2. | Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3229] [Cited by in RCA: 3305] [Article Influence: 127.1] [Reference Citation Analysis (0)] |
| 3. | Guzeldemir E, Toygar HU. From alveolar diffuse atrophy to aggressive periodontitis: a brief history. J Hist Dent. 2006;54:96-99. [PubMed] |
| 4. | on aggressive periodontitis. American Academy of Periodontology. J Periodontol. 2000;71:867-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 77] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Schacher B, Baron F, Rossberg M, Wohlfeil M, Arndt R, Eickholz P. Aggregatibacter actinomycetemcomitans as indicator for aggressive periodontitis by two analysing strategies. J Clin Periodontol. 2007;34:566-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 6. | Armitage GC. Comparison of the microbiological features of chronic and aggressive periodontitis. Periodontol 2000. 2010;53:70-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Teughels W, Dhondt R, Dekeyser C, Quirynen M. Treatment of aggressive periodontitis. Periodontol 2000. 2014;65:107-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Schuyler CH. The function and importance of incisal guidance in oral rehabilitation. 1963. J Prosthet Dent. 2001;86:219-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Maeda S, Maeda Y, Ono Y, Nakamura K, Sasaki T. Interdisciplinary treatment of a patient with severe pathologic tooth migration caused by localized aggressive periodontitis. Am J Orthod Dentofacial Orthop. 2005;127:374-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 10. | Ishihara Y, Tomikawa K, Deguchi T, Honjo T, Suzuki K, Kono T, Kuboki T, Kamioka H, Takashiba S, Yamashiro T. Interdisciplinary orthodontic treatment for a patient with generalized aggressive periodontitis: Assessment of IgG antibodies to identify type of periodontitis and correct timing of treatment. Am J Orthod Dentofacial Orthop. 2015;147:766-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol. 2018;89 Suppl 1:S159-S172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 700] [Cited by in RCA: 1303] [Article Influence: 217.2] [Reference Citation Analysis (0)] |
| 12. | Nesse W, Abbas F, van der Ploeg I, Spijkervet FK, Dijkstra PU, Vissink A. Periodontal inflamed surface area: quantifying inflammatory burden. J Clin Periodontol. 2008;35:668-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 358] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 13. | Armitage GC. Periodontal diagnoses and classification of periodontal diseases. Periodontol 2000. 2004;34:9-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 461] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 14. | Deas DE, Moritz AJ, Sagun RS Jr, Gruwell SF, Powell CA. Scaling and root planing vs. conservative surgery in the treatment of chronic periodontitis. Periodontol 2000. 2016;71:128-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 15. | Melsen B. Tissue reaction to orthodontic tooth movement--a new paradigm. Eur J Orthod. 2001;23:671-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 135] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Zasčiurinskienė E, Basevičienė N, Lindsten R, Slotte C, Jansson H, Bjerklin K. Orthodontic treatment simultaneous to or after periodontal cause-related treatment in periodontitis susceptible patients. Part I: Clinical outcome. A randomized clinical trial. J Clin Periodontol. 2018;45:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Fukunaga T, Kuroda S, Kurosaka H, Takano-Yamamoto T. Skeletal anchorage for orthodontic correction of maxillary protrusion with adult periodontitis. Angle Orthod. 2006;76:148-155. [PubMed] |
| 18. | Costa A, Raffainl M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201-209. [PubMed] |
| 19. | Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, Kawamura H, Mitani H. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 2004;125:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 160] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 20. | Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: a cephalometric evaluation. Angle Orthod. 2004;74:381-390. [PubMed] |
| 21. | Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997;31:763-767. [PubMed] |
| 22. | Paik CH, Woo YJ, Boyd RL. Treatment of an adult patient with vertical maxillary excess using miniscrew fixation. J Clin Orthod. 2003;37:423-428. [PubMed] |
| 23. | Kaku M, Kojima S, Sumi H, Koseki H, Abedini S, Motokawa M, Fujita T, Ohtani J, Kawata T, Tanne K. Gummy smile and facial profile correction using miniscrew anchorage. Angle Orthod. 2012;82:170-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res. 2012;23 Suppl 6:2-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 745] [Cited by in RCA: 614] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 25. | Donos N, Laurell L, Mardas N. Hierarchical decisions on teeth vs. implants in the periodontitis-susceptible patient: the modern dilemma. Periodontol 2000. 2012;59:89-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Al-Zahrani MS. Implant therapy in aggressive periodontitis patients: a systematic review and clinical implications. Quintessence Int. 2008;39:211-215. [PubMed] |
| 27. | Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 2007;18:669-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |