Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.6009
Peer-review started: February 3, 2021
First decision: April 25, 2021
Revised: May 6, 2021
Accepted: May 27, 2021
Article in press: May 27, 2021
Published online: July 26, 2021
Processing time: 167 Days and 21.6 Hours
Prostatitis caused by Brucella infection is rare and usually lacks typical lower urinary tract symptoms. However, Brucella infection can cause serum prostate-specific antigen levels to become abnormally elevated. When concurrent with lumbar vertebra infection and erosion, brucellosis can easily be misdiagnosed as prostate cancer with bone metastasis.
A 45-year-old man complained of recurrent low back pain and fever for 2 wk. Magnetic resonance imaging of the lumbar vertebrae showed abnormal signs at the rear of the L4–5 vertebral body. Serum prostate-specific antigen level was 17.64 ng/mL, and positron emission tomography/computed tomography suggested the possibility of prostate cancer with liver and lumbar metastases. The patient was transferred to our department for further treatment. He experienced repeated bouts of fever and low back pain during hospitalization. Biopsy results indicated prostatitis. There was no significant increase in white blood cell count or procalcitonin levels. The Mycobacterium tuberculosis smear and antibody detection results were negative. Cefoperazone sulbactam was not effective. Blood culture test results were positive for brucellosis, confirming the diagnosis of brucellosis. After oral anti-infection treatment with doxycycline and rifampicin, the body temperature gradually returned to normal, and lumbago improved. After continuous treatment for 6 mo, the patient recovered.
In patients with low back pain and fever accompanied by elevated prostate-specific antigen levels and lesions of the prostate and lumbar spine, a detailed medical history and blood and urine cultures should be obtained, and attention should be given to the local epidemic infectious disease situation.
Core Tip: Brucella infection of both the prostate and lumbar spine is rare. We present a case of such an atypical presentation accompanied by fever and low back pain. Abnormally elevated serum prostate-specific antigen levels and abnormally high metabolic signals in the prostate and lumbar spine were indicated on positron emission tomography/computed tomography scans, which were suggestive of a diagnosis of prostate cancer with lumbar metastases, except for the unexplained periodic fever. Blood culture and agglutination tests were used to confirm brucellosis. This case highlights the need to pay more attention to and identify the atypical symptoms caused by Brucella infection.
- Citation: Yan JF, Zhou HY, Luo SF, Wang X, Yu JD. Rare case of brucellosis misdiagnosed as prostate carcinoma with lumbar vertebra metastasis: A case report. World J Clin Cases 2021; 9(21): 6009-6016
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/6009.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.6009
Brucellosis is a zoonotic disease caused by a Brucella infection that mainly occurs in occupational exposure groups, such as herdsmen, veterinarians, and slaughterhouse workers. Brucellosis may invade every system of the body and has diverse clinical manifestations and a high misdiagnosis rate[1]. Prostate infection caused by brucellosis is relatively rare, and when accompanied by the destruction of the lumbar vertebral body, imaging examination can easily lead to a misdiagnosis of prostate cancer with lumbar metastasis. This case report describes a rare case of Brucella prostatitis and lumbar vertebrae destruction.
A 45-year-old man was admitted to our hospital with recurrent low back pain and fever for 2 wk.
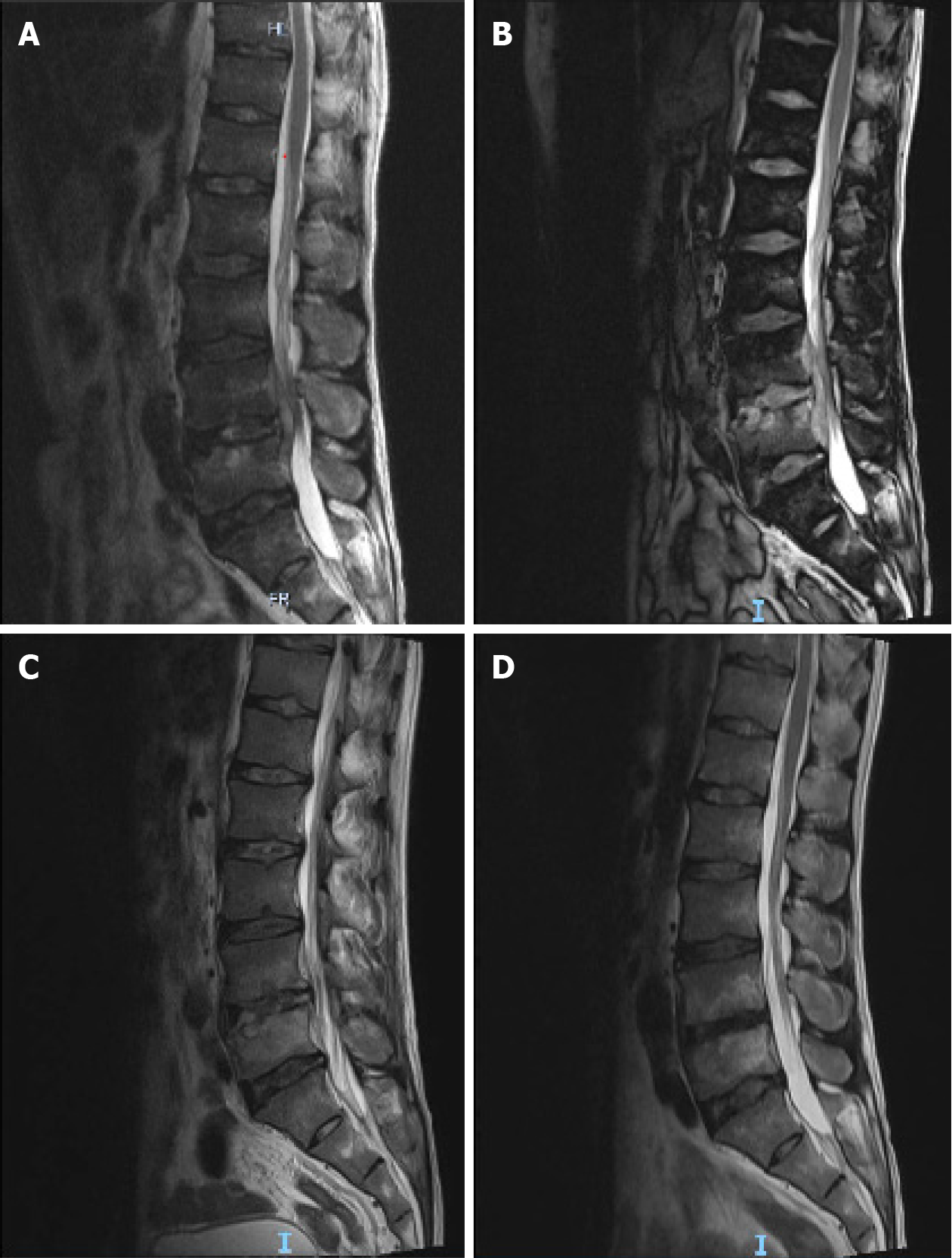
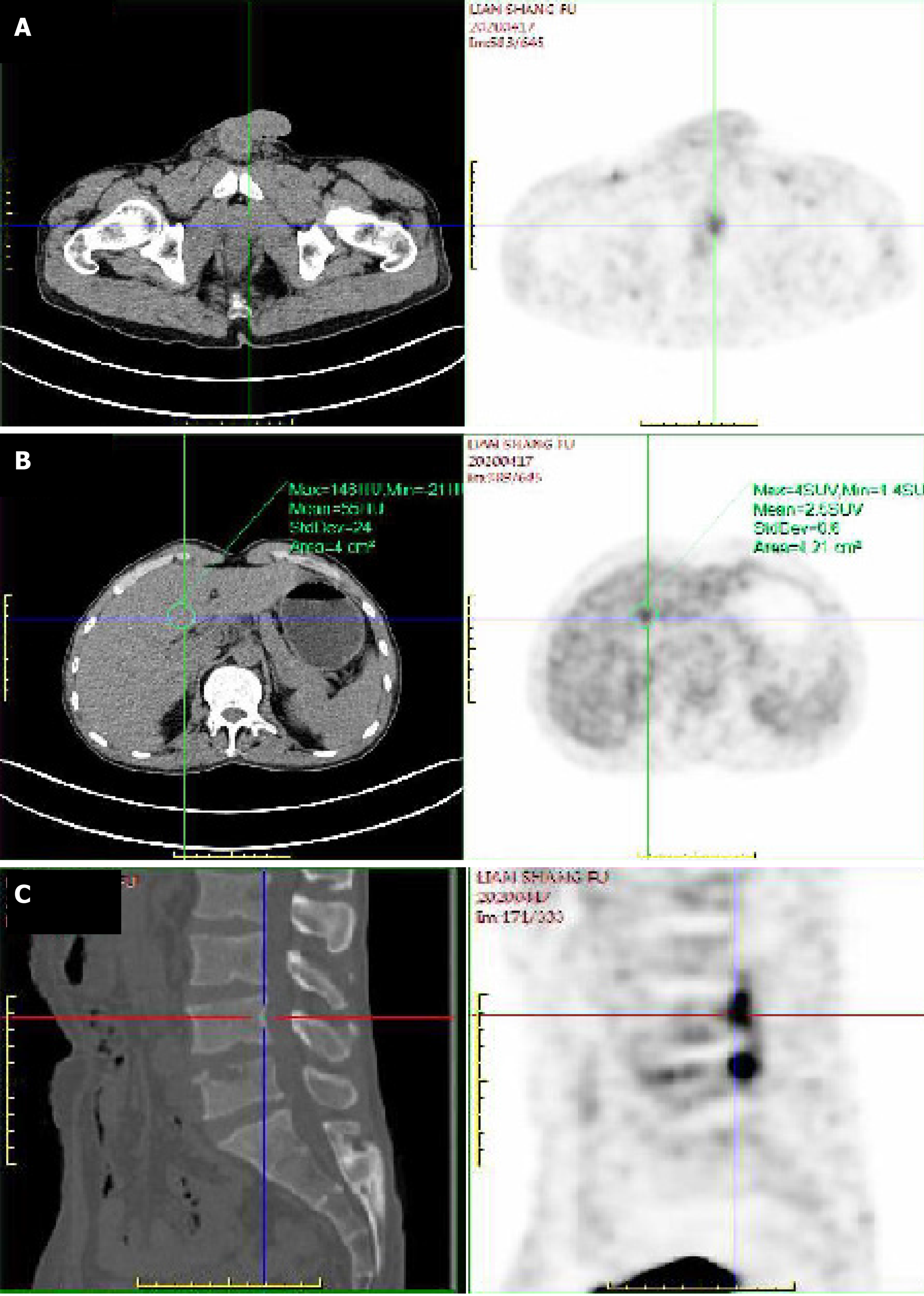
The patient reported recurrent fever with low back pain for 2 wk. The highest temperature was approximately 39 C, and he experienced no other discomfort. One week prior to his admission, the patient attended a local hospital for examination, and an elevated serum prostate-specific antigen (PSA) (17.64 ng/mL) level was found. Magnetic resonance imaging of the lumbar vertebrae showed an abnormal signal at the rear of the L4–5 vertebral body (Figure 1A). Further, whole-body positron emission tomography/computed tomography showed a slightly low-density nodule on the left side of the prostate, with an uneven increase in fluorodeoxyglucose metabolism, which indicated prostate cancer and the need for a prostate puncture biopsy. Moreover, the left lateral lobe of the liver had a slightly low-density nodule, and L3/4/5 vertebral bone destruction was detected with high fluorodeoxyglucose metabolism (Figure 2). The local hospital considered the possibility of a prostate tumor, and the patient was referred to our hospital for further treatment.
The patient’s previous medical history was uneventful.
The patient and his family members had no previous episodes of similar diseases.
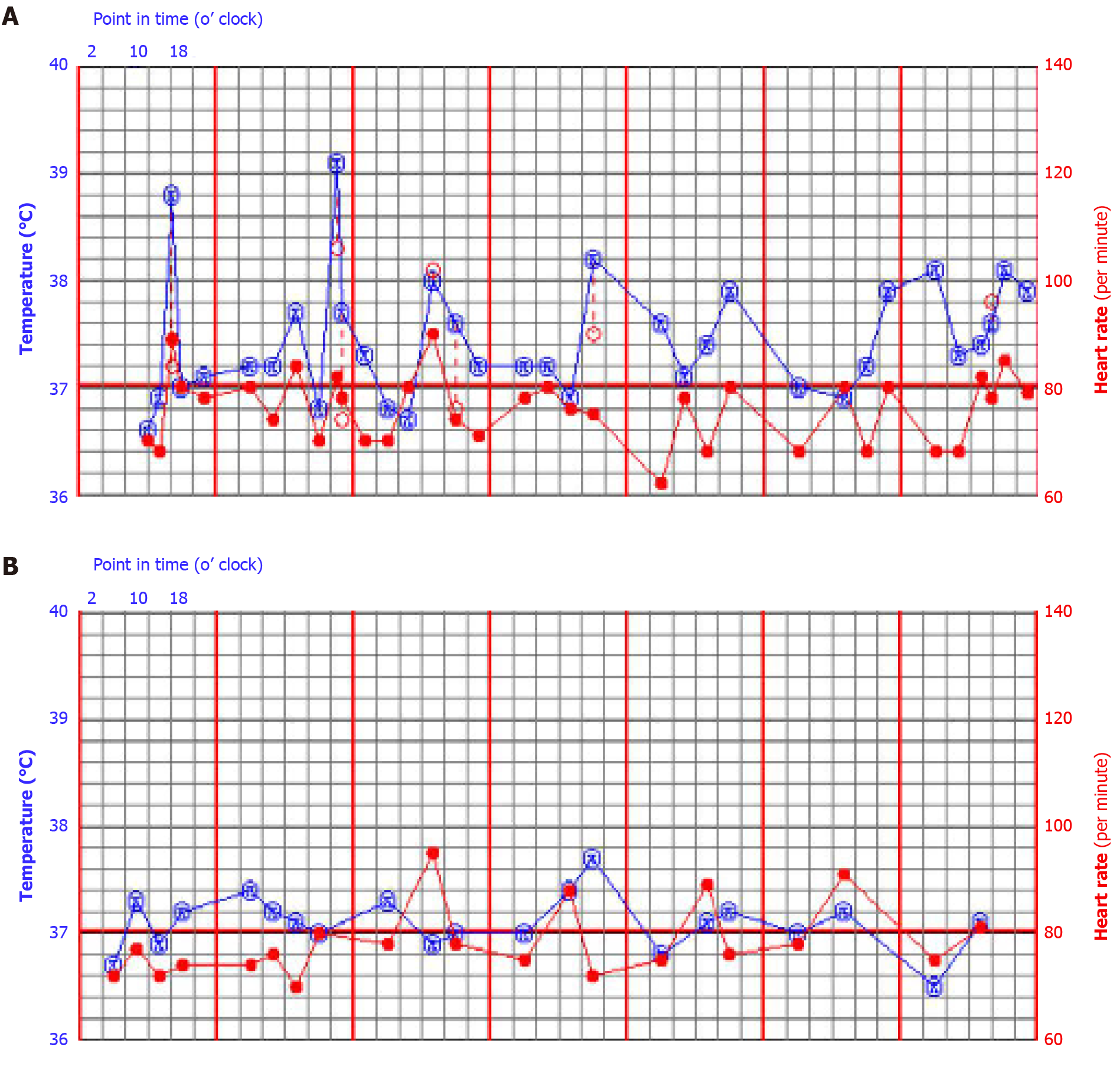
The patient had recurrent signs of fever with a peak body temperature of 39 °C, and most occurrences of fever occurred in the first half of the night (Figure 3). Pulse rate, blood pressure, and respiratory rhythm were normal. There was no percussion pain in the lower back, no scleroma observed on rectal examination of the prostate and no positive nervous system signs on physical examination.
On re-examination after admission, the serum PSA level was 8.36 ng/mL, and the proportion of free PSA was 0.046. Routine blood examination showed that the neutrophil ratio increased to 88.8% (normal range, 40.0%–75.0%), and the lymphocyte ratio decreased to 9.3% (normal range, 20.0%–50.0%) with the absolute value decreasing to 0.5 × 109/L. Leukocyte, thrombocyte, and hemoglobin values were normal, and serum C-reactive protein levels had increased to 47.84 mg/L (normal value, < 4 mg/L). No abnormalities were found in routine urine, liver, and kidney function tests, bacterial and fungal culture in urine tests, and HIV-related tests. The test result for COVID-19 nucleic acids and antibodies was also negative.
Chest and abdominal computed tomography showed no obvious abnormalities.
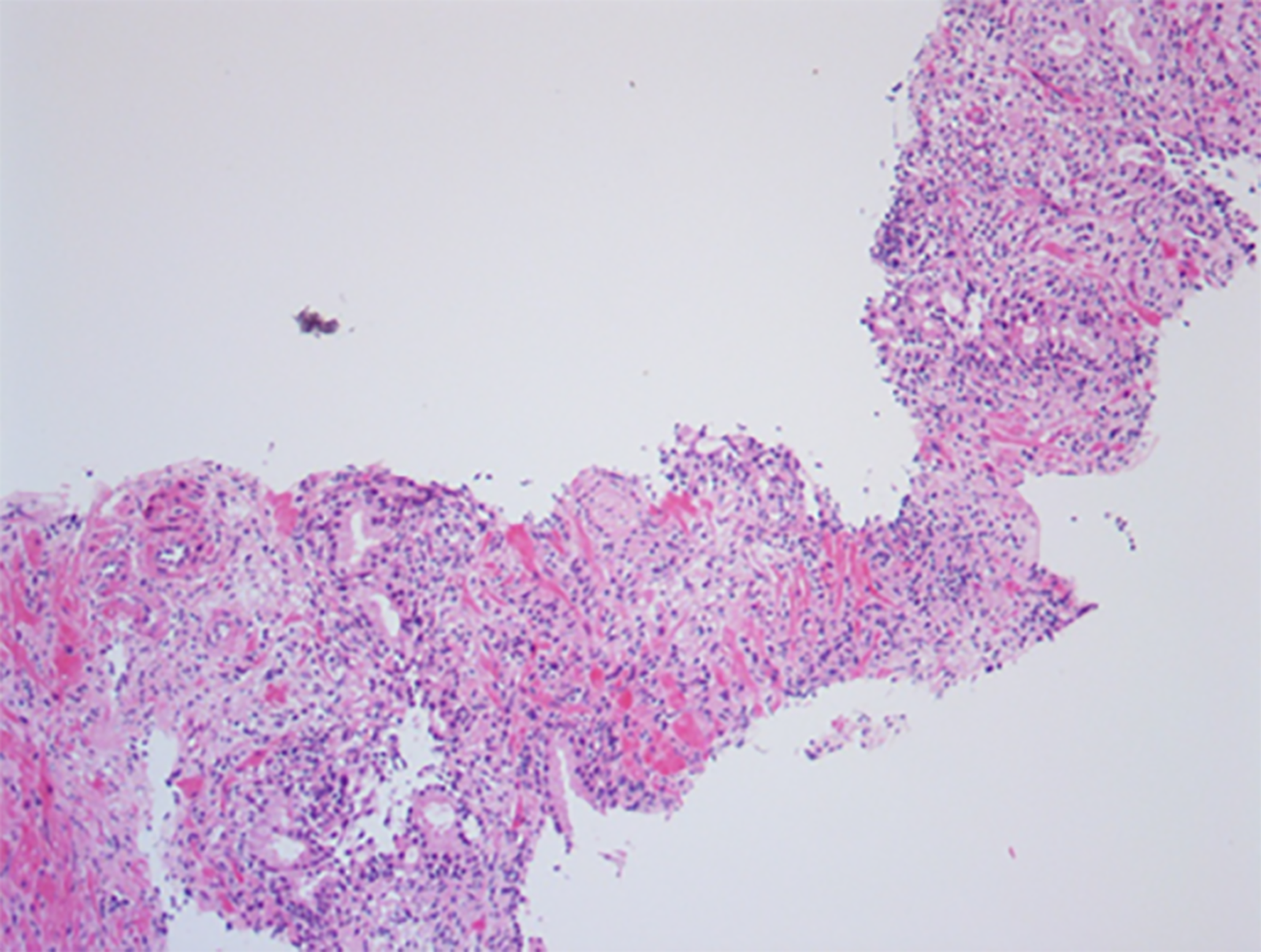
After a prostate puncture, histological examination showed that there were more inflammatory cells in the prostate tissue (Figure 4). However, tumor cells were not detected.
The final diagnoses were Brucella prostatitis infection and Brucella lumbar infection.
We initially administered cefoperazone sulbactam intravenously as an anti-infective treatment; however, it was ineffective. Blood culture results indicated Brucella, and the standard tube agglutination test results were positive (> 1:200). We further enquired about the patient’s history of exposure to cattle and sheep in the last 2 mo prior to his illness. We subsequently confirmed that the patient’s disease was brucellosis. The patient was administered rifampicin (0.45 g capsule; once daily, in the morning), doxycycline enteric-coated (0.1g capsule; twice daily), reduced glutathione injection (1200 mg; once daily) to protect the liver, and other symptomatic support treatment. Subsequently, the patient’s body temperature gradually decreased to normal, and the low back pain was significantly relieved. After 1 wk of treatment, a repeat lumbar magnetic resonance imaging showed damage of the L4 and L5 vertebral bodies and compression stenosis of the L4–5 Level vertebral canal, which were consistent with previous images (Figure 1B). The patient’s condition was stable, and he was discharged and advised to continue with the above-mentioned drugs.
After discharge, the patient continued to receive oral treatment for 6 mo without fever and discomfort. He returned to the hospital for re-examination 2 mo and 6 mo after discharge. Routine blood and urine, liver, and kidney function test results were normal. Lumbar magnetic resonance imaging examination showed that the scope of bone destruction of the L4/5 vertebral body reduced and spinal stenosis improved (Figure 1C and 1D). Drug treatment was then discontinued.
Brucellosis is one of the most important zoonotic infectious diseases worldwide. The incidence of brucellosis in developing countries is significantly higher than that in developed countries. According to statistics, there are approximately 500000 new cases every year[2]. Brucellosis was first reported in China in the 1950s[3]. In recent years, the incidence of human brucellosis has increased sharply. An epidemiological investigation showed that the incidence rate of human brucellosis in mainland China had increased to 4.2 cases/100000 people in 2014 and showed a further upward trend[4,5]. Approximately 80% of patients report a history of contact with sick animals, and 11% of patients report using uncooked animal products before the onset of the disease; consumption of unsterile animal products is the main transmission route[6].
In humans, Brucella infection can cause many systemic and organ lesions, and its clinical manifestations are diverse and nonspecific[7]; this makes brucellosis easily misdiagnosed as other diseases. The reproductive system is a rare site of human Brucella infection, accounting for 2.7% of all cases[8]. The most common genital system infections involve the testis and epididymis[9]. Only a few cases of prostate infection have been reported[10-12].
Clinical manifestations and complications of brucellosis include fever, arthralgia, fatigue, and muscle pain, which are also common reproductive system complications[8]. Prostatitis can also occur and mainly manifests as an enlarged prostate, inflammatory or purulent secretions, and discomfort when urinating. This patient did not present with typical symptoms of prostate infection described above. The patient presented with only recurrent fever and low back pain. There was only a slight increase in C-reactive protein levels in the blood with fever, while the white blood cell and procalcitonin indexes were normal, which could not be explained by a common bacterial infection. At the same time, the elevated PSA levels were associated with low back pain. Imaging examination was also consistent with the manifestations of prostate tumor and lumbar metastatic tumor. Therefore, we initially considered the diagnosis to be prostate cancer. In the process of diagnosis and treatment, the patient’s abnormal fever symptoms and epidemiological history were ignored, and blood culture testing was not conducted in the early stage of treatment; this led to the initial misdiagnosis.
Multiorgan involvement in Brucella infection is probably underrecognized[13]. The central nervous system, bone, and epididymis are the most commonly included organs[14]. Such coinfection of the prostate and lumbar spine is extremely rare and can lead to misdiagnosis. One challenge in the diagnosis of brucellosis is that the most common laboratory abnormalities are nonspecific. Most patients have normal blood cell counts on presentation. Brucella bacterial culture is the “gold standard” for the diagnosis of brucellosis[15]. Therefore, to reduce the rate of misdiagnosis, it is necessary to broaden the possible clinical diagnoses with a detailed history and perform agglutination tests and blood cultures as early as possible for patients with fever.
In patients with elevated serum PSA levels accompanied by fever, it is very important to consider the possibility of prostatitis caused by common infections and prostate cancer as well as the possibility of prostatitis caused by non-abnormal infections. Detailed epidemiological investigations and laboratory examinations are very important.
In clinical practice, there is a low incidence of prostatic inflammation caused by Brucella. Therefore, the clinical diagnosis is difficult, and misdiagnoses are common. Clinicians should carefully examine the medical history of patients with unexplained recurrent fever, low back pain, and abnormal serum PSA levels and pay attention to the epidemic situation in the territory and contact history with cattle and sheep. Blood culture and other related tests can help confirm the diagnosis, and a regular and full course of drug treatment is the key to the resolution of the disease.
We are grateful to our colleagues from the Department of Imaging, Laboratory, Pathology, and Infection for providing diagnostic and therapeutic help.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Candelli M S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Xing YX
| 1. | Dean AS, Crump L, Greter H, Hattendorf J, Schelling E, Zinsstag J. Clinical manifestations of human brucellosis: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2012;6:e1929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 350] [Cited by in RCA: 310] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 2. | Perkins SD, Smither SJ, Atkins HS. Towards a Brucella vaccine for humans. FEMS Microbiol Rev. 2010;34:379-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Deqiu S, Donglou X, Jiming Y. Epidemiology and control of brucellosis in China. Vet Microbiol. 2002;90:165-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 175] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Lai S, Zhou H, Xiong W, Gilbert M, Huang Z, Yu J, Yin W, Wang L, Chen Q, Li Y, Mu D, Zeng L, Ren X, Geng M, Zhang Z, Cui B, Li T, Wang D, Li Z, Wardrop NA, Tatem AJ, Yu H. Changing Epidemiology of Human Brucellosis, China, 1955-2014. Emerg Infect Dis. 2017;23:184-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 176] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 5. | Jiang H, O'Callaghan D, Ding JB. Brucellosis in China: history, progress and challenge. Infect Dis Poverty. 2020;9:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 6. | Zheng R, Xie S, Lu X, Sun L, Zhou Y, Zhang Y, Wang K. A Systematic Review and Meta-Analysis of Epidemiology and Clinical Manifestations of Human Brucellosis in China. Biomed Res Int. 2018;2018:5712920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 123] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 7. | Yagupsky P, Morata P, Colmenero JD. Laboratory Diagnosis of Human Brucellosis. Clin Microbiol Rev. 2019;33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 190] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 8. | Zhou Y, Xie S, Zheng R, Dai Q, Xu Z, Zuo W, Ding J, Zhang Y. Brucellar reproductive system injury: A retrospective study of 22 cases and review of the literature. J Int Med Res. 2020;48:300060520924548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Navarro-Martínez A, Solera J, Corredoira J, Beato JL, Martínez-Alfaro E, Atiénzar M, Ariza J. Epididymoorchitis due to Brucella mellitensis: a retrospective study of 59 patients. Clin Infect Dis. 2001;33:2017-2022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | O'LEARY J, SPINK WW. Failure to isolate Brucella from prostatic tissue of individuals living in an endemic area. Proc Soc Exp Biol Med. 1950;75:41-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Aksoy F, Aksoy HZ, Sözen EE, Yilmaz G, Köksal I. [A case of Brucella prostatitis misdiagnosed as prostate carcinoma]. Mikrobiyol Bul. 2009;43:493-497. [PubMed] |
| 12. | Alenazi AH, Alfhaidi FM, Aljumaah AAS, Alenzi MJ, AlOtaibi MM. A rare case of prostatic abscess caused by Brucella organisms: First report in Saudi Arabia. Urol Ann. 2018;10:106-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Herrick JA, Lederman RJ, Sullivan B, Powers JH, Palmore TN. Brucella arteritis: clinical manifestations, treatment, and prognosis. Lancet Infect Dis. 2014;14:520-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Buzgan T, Karahocagil MK, Irmak H, Baran AI, Karsen H, Evirgen O, Akdeniz H. Clinical manifestations and complications in 1028 cases of brucellosis: a retrospective evaluation and review of the literature. Int J Infect Dis. 2010;14:e469-e478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 321] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 15. | Barua A, Kumar A, Thavaselvam D, Mangalgi S, Prakash A, Tiwari S, Arora S, Sathyaseelan K. Isolation & characterization of Brucella melitensis isolated from patients suspected for human brucellosis in India. Indian J Med Res. 2016;143:652-658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |