Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.5955
Peer-review started: October 29, 2020
First decision: February 12, 2021
Revised: February 16, 2021
Accepted: May 15, 2021
Article in press: May 15, 2021
Published online: July 26, 2021
Processing time: 262 Days and 19.4 Hours
As a highly contagious disease, coronavirus disease 2019 (COVID-19) is wreaking havoc around the world due to continuous spread among close contacts mainly via droplets, aerosols, contaminated hands or surfaces. Therefore, centralized isolation of close contacts and suspected patients is an important measure to prevent the transmission of COVID-19. At present, the quarantine duration in most countries is 14 d due to the fact that the incubation period of severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) is usually identified as 1-14 d with median estimate of 4-7.5 d. Since COVID-19 patients in the incubation period are also contagious, cases with an incubation period of more than 14 d need to be evaluated.
A 70-year-old male patient was admitted to the Department of Respiratory Medicine of The First Affiliated Hospital of Harbin Medical University on April 5 due to a cough with sputum and shortness of breath. On April 10, the patient was transferred to the Fever Clinic for further treatment due to close contact to one confirmed COVID-19 patient in the same room. During the period from April 10 to May 6, nucleic acid and antibodies to SARS-CoV-2 were tested 7 and 4 times, respectively, all of which were negative. On May 7, the patient developed fever with a maximum temperature of 39℃, and his respiratory difficulties had deteriorated. The results of nucleic acid and antibody detection of SARS-CoV-2 were positive. On May 8, the nucleic acid and antibody detection of SARS-CoV-2 by Heilongjiang Provincial Center for Disease Control were also positive, and the patient was diagnosed with COVID-19 and reported to the Chinese Center for Disease Control and Prevention.
This case highlights the importance of the SARS-CoV-2 incubation period. Further epidemiological investigations and clinical observations are urgently needed to identify the optimal incubation period of SARS-CoV-2 and formulate rational and evidence-based quarantine policies for COVID-19 accordingly.
Core Tip: As the quarantine duration of coronavirus disease 2019 (COVID-19) in most countries is currently 14 d, cases with an incubation period of more than 14 d in the clinic may trigger rapid spread of the epidemic, which requires us to be highly vigilant. We present a COVID-19 patient with an incubation period of 27 d confirmed in the Fever Clinic of The First Affiliated Hospital of Harbin Medical University. Further epidemiological investigations and clinical observations are urgently needed to identify the optimal incubation period of severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) and formulate rational and evidence-based quarantine policies for COVID-19 accordingly.
- Citation: Du X, Gao Y, Kang K, Chong Y, Zhang ML, Yang W, Wang CS, Meng XL, Fei DS, Dai QQ, Zhao MY. COVID-19 patient with an incubation period of 27 d: A case report. World J Clin Cases 2021; 9(21): 5955-5962
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/5955.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.5955
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) infection, has been officially identified as a Class B infectious disease mainly involving the respiratory system. In China, the prevention and control measures for COVID-19 are required to be in accordance with Class A infectious disease[1]. SARS-CoV-2 is a novel coronavirus[2], and all indivi
A 70-year-old male patient was admitted to the Department of Respiratory Medicine of The First Affiliated Hospital of Harbin Medical University on April 5 due to a cough with sputum and shortness of breath.
Cough with sputum and shortness of breath appeared 2 mo ago, and the cough and dyspnea were then further aggravated.
The patient had a medical history of hypertension and vitiligo.
The patient had no personal or family history.
The patient’s vital signs were stable. Rales could be heard on auscultation of both lungs.
Laboratory tests revealed the following results on admission: White blood cell count of 9.06 × 109/L, neutrophil (NEUT) count of 7.34 × 109/L, NEUT% of 80.90%, lymphocyte (LYMPH) count of 0.47 × 109/L and percentage of lymphocytes (LYM%) of 5.20%. During the period from April 10 to May 7, blood cell analyses were reexamined (Table 1), in which LYMPH and LYM% significantly decreased.
| Day of illness | 1 | 2 | 3 | 6 | 7 | 8 | 10 | 11 | 13 | 17 | 20 | 21 | 27 | ||||
| Disease Course | Hospitalization | Close contact | The Fever Clinic | Positive PCR | |||||||||||||
| White blood cell count (× 109/L) | 9 | 6.87 | 8.67 | 8.62 | 9.69 | 6.63 | |||||||||||
| Lymphocyte count (× 109/L) | 0.47 | 0.55 | 0.73 | 0.24 | 0.18 | 0.12 | |||||||||||
| Lymphocyte percentage (%) | 5.2 | 8 | 8.42 | 2.82 | 1.92 | 1.8 | |||||||||||
| Nucleic acid detection | Negative | Negative | Negative | Negative | Negative | Negative | Negative | Positive | Positive | ||||||||
| Antibody detection IgM | Negative | Negative | Negative | Negative | Positive | Positive | |||||||||||
| Antibody detection IgG | Negative | Negative | Negative | Negative | Positive | Positive | |||||||||||
| Oxygen therapy | Oxygen therapy | HFNC | Invasive mechanical ventilation | ||||||||||||||
| CT | CT | CT | CT | CT | CT | ||||||||||||
| Date | Apri l5 | April 10 | April 11 | April 12 | April 15 | April 16 | April 17 | April 19 | April 20 | April 22 | April 26 | April 29 | April 30 | May 6 | May 7 | May 8 | May 11 |
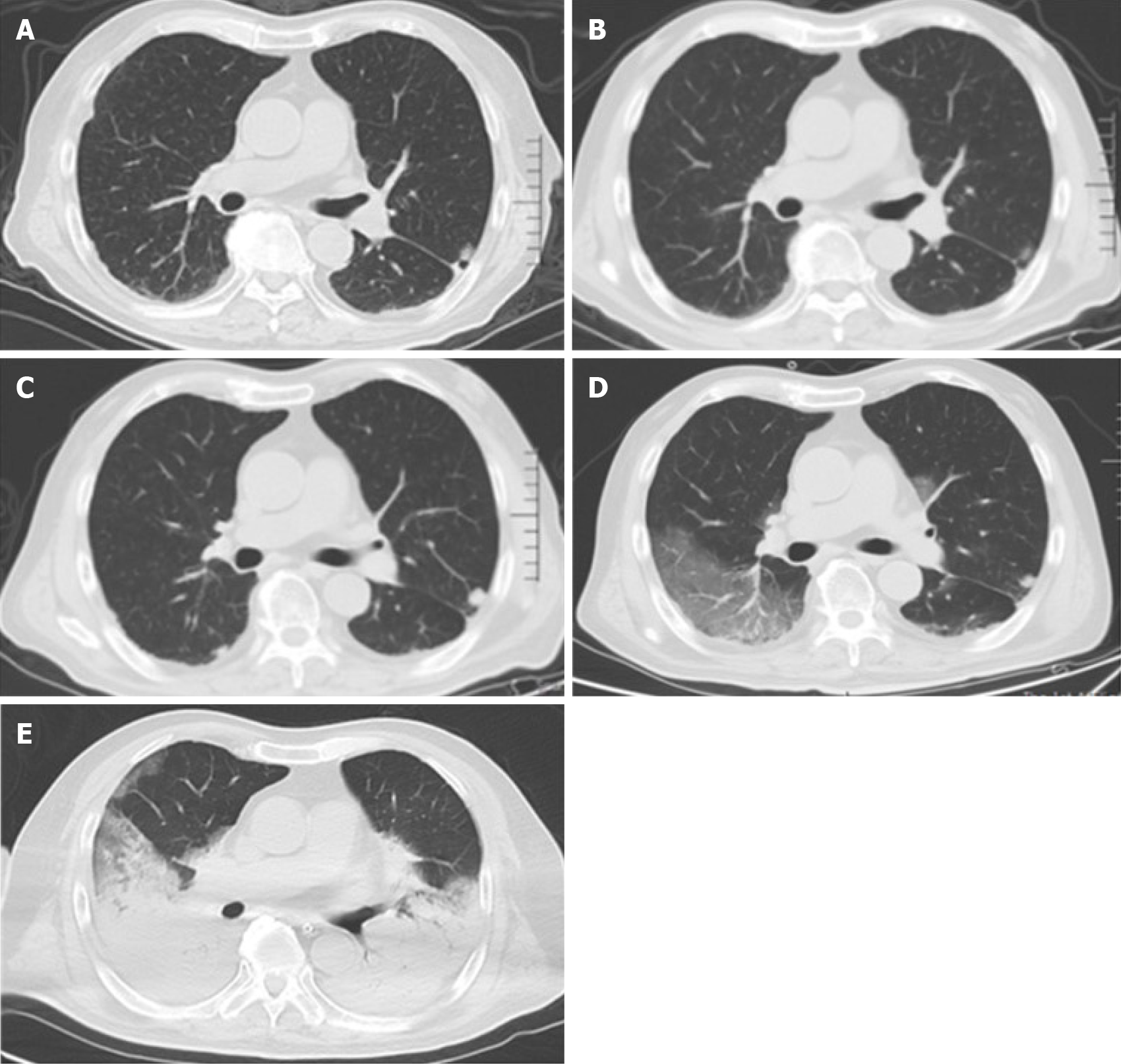
The initial lung computed tomography (CT) indicated pneumonia and multiple nodules in the lungs, bilateral pleural effusion and pericardial effusion. On May 7, reexamination of the lung CT showed patchy shadows and interstitial changes. On May 11, lung CT imaging showed that the lung lesions had rapidly deteriorated (Figure 1).
On May 7, the results of nucleic acid and antibody detection of SARS-CoV-2 were positive. On May 8, the nucleic acid and antibody detection of SARS-CoV-2 by Heilongjiang Provincial Center for Disease Control were also positive, and the patient was diagnosed with COVID-19 and reported to the Chinese Center for Disease Control and Prevention.
In the initial stage of disease, the patient occasionally had shortness of breath but did not need oxygen therapy. On April 10, the patient was transferred to the Fever Clinic for further treatment due to close contact to one confirmed COVID-19 patient in the same room. During the period from April 10 to May 6, lung CT was reviewed on April 26 and 30 (Figure 1), and nucleic acid and antibody of SARS-CoV-2 were tested 7 and 4 times, respectively, all of which were negative (Table 1). Surprisingly, on May 7, the patient developed fever with a maximum temperature of 39℃, and his respiratory difficulties had deteriorated. Continuous oxygen therapy was then provided. Due to continuous deterioration of the patient's condition, a high-flow nasal cannula and invasive mechanical ventilation were given to the patient on May 7 and 11 to enhance respiratory support. In addition, comprehensive treatment measures also included antibiotic agents, analgesic and sedative drug injections, vasopressor support and immunotherapy.
Unfortunately, despite timely comprehensive treatment measures were taken, the patient's immune function and condition did not improve, and he eventually died.
In April 2020, a cluster of SARS-CoV-2 infections occurred in two tertiary general hospitals in Harbin city, resulting in 66 newly confirmed patients including this case and 21 asymptomatic patients. Due to close contact to a confirmed COVID-19 patient, our patient had received relevant treatment in the Fever Clinic of our hospital for 27 d. As our hospital is the treatment center for COVID-19 in Heilongjiang Province, the ward layout, regulations, work arrangements, operation specifications and disinfection procedures in the Fever Clinic of our hospital were all in line with national regulations and standards; thus, the possibility of cross-infection in the Fever Clinic was extremely low. Therefore, by staying in the same room with a confirmed COVID-19 patient from April 5th to 10th, there was a chance of contracting SARS-CoV-2.
Currently, the diagnosis of COVID-19 mainly depends on detection of SARS-CoV-2 nucleic acid on oropharyngeal and/or nasopharyngeal swabs by real-time polymerase chain reaction (RT-PCR)[9,10], although there is still a possibility of false-positive and false–negative results[11-13]. Therefore, lung CT has been proposed as an auxiliary method for the rapid diagnosis of COVID-19 due to its low rate of missed diagnosis[14]. In addition to a CT scan, abnormal findings on fluorodeoxyglucose-positron emission tomography/CT scans may confirm or exclude the presence of SARS-CoV-2 infection[15]. Bilateral and peripheral ground-glass opacities and consolidation are the most common features of COVID-19 on lung CT imaging[16-18], which were not found in the three lung CT examinations before our patient was diagnosed with COVID-19. In addition, the patient's seven nucleic acid tests and four antibody tests for SARS-CoV-2 were all negative during the quarantine period. Following the diagnosis of COVID-19, CT imaging revealed rapid deterioration of the lungs with the typical imaging characteristics of COVID-19 over a short period of time compared with the previous CT scans[19]. Based on the above history, it was concluded that the patient had acquired SARS-CoV-2 infection due to sharing the same room with a confirmed COVID-19 patient from April 5th to 10th, he then developed worse symptoms on May 7th and was confirmed to have COVID-19 on May 8th. Thus, the incubation period was 27 d, which is very rare in clinical practice.
The prerequisite for determining the optimal quarantine duration is a good understanding of the incubation period. The incubation period usually refers to the time between infection and the onset of corresponding symptoms and signs or when the disease is confirmed[20], which determines the adjustment in quarantine policies. The mainstream view is that the incubation period of SARS-CoV-2 is usually identified as 1-14 d with a median estimate of 4-7.5 d[6,21-23], and thus the current clinical practice of 14-d quarantine duration in most countries seems reasonable. However, there is a different opinion that a small proportion of COVID-19 patients have an incubation period of more than 14 d based on the estimated incubation distribution[6,20], which will be an enormous figure considering the surge in COVID-19 patients and its rising trend. Age may be one of the explanations for the longer incubation period of COVID-19[24], while the other mechanisms are still unclear.
Definitive close contact, as shown in this case report, and some extreme cases should be considered to extend the quarantine duration during the outbreak stage of the epidemic[25,26]. When the epidemic recurred in Heilongjiang Province in April 2020, the quarantine duration was extended and the SARS-CoV-2 nucleic acid test was popularized for entry personnel, referred to as “14 + 7 + 14”. Fourteen days of centralized isolation and 2 nucleic acid tests, and 7 d of centralized isolation and one nucleic acid test should be carried out at the entry point and the local region, respectively, and then 14 d of home isolation and observation should be carried out and incorporated into the grid management of the local community[27]. Prolonged quarantine duration can effectively prevent SARS-CoV-2 from spreading during the incubation period. Obviously, an extension of quarantine duration will make the already overwhelmed medical system even more overstretched, and increase the burden on society and individuals during the COVID-19 epidemic. Further epidemiological investigations and clinical observations are urgently needed to identify the optimal incubation period of SARS-CoV-2 and formulate rational and evidence-based quarantine policies for COVID-19 accordingly.
As the quarantine duration for COVID-19 in most countries is currently 14 d, cases with an incubation period of more than 14 d in the clinic may trigger rapid spread of the epidemic, which requires us to be highly vigilant. Further studies are needed to determine the proportion of COVID-19 patients with an incubation period of more than 14 d, and weigh the costs of extending quarantine duration and the potential risks and consequences of the spread of the epidemic during the incubation period. These findings will have important implications for optimal prevention and control of COVID-19.
We are grateful to all colleagues who worked with us in the COVID-19 treatment center of Heilongjiang Province, and all those who provided selfless advice and help for this article. We pay tribute to the medical staff who lost their lives in the national fight against the COVID-19 epidemic.
Manuscript source: Unsolicited manuscript
Specialty type: Critical Care Medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karcioglu Ö, Maurea S S-Editor: Wang JL L-Editor: Webster JR P-Editor: Liu JH
| 1. | National Health Commission of the People’s Republic of China. Novel coronavirus infection pneumonia is included in the management of notifiable infectious diseases. Available from: http://www.nhc.gov.cn/jkj/s7916/202001/44a3b8245e8049d2837a4f27529cd386.shtml. |
| 2. | Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, Guo L, Guo R, Chen T, Hu J, Xiang Z, Mu Z, Chen X, Chen J, Hu K, Jin Q, Wang J, Qian Z. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11:1620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2003] [Cited by in RCA: 2290] [Article Influence: 458.0] [Reference Citation Analysis (0)] |
| 3. | Li H, Liu SM, Yu XH, Tang SL, Tang CK. Coronavirus disease 2019 (COVID-19): current status and future perspectives. Int J Antimicrob Agents. 2020;55:105951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 692] [Cited by in RCA: 582] [Article Influence: 116.4] [Reference Citation Analysis (0)] |
| 4. | Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, Sun C, Sylvia S, Rozelle S, Raat H, Zhou H. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1355] [Cited by in RCA: 1088] [Article Influence: 217.6] [Reference Citation Analysis (0)] |
| 5. | Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, Huang J, He N, Yu H, Lin X, Wei S, Wu T. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020;323:1915-1923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1200] [Cited by in RCA: 1072] [Article Influence: 214.4] [Reference Citation Analysis (0)] |
| 6. | Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, Azman AS, Reich NG, Lessler J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann Intern Med. 2020;172:577-582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4286] [Cited by in RCA: 3369] [Article Influence: 673.8] [Reference Citation Analysis (1)] |
| 7. | Huang L, Zhang X, Wei Z, Zhang L, Xu J, Liang P, Xu Y, Zhang C, Xu A. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J Infect. 2020;80:e1-e13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 251] [Cited by in RCA: 235] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 8. | Yu P, Zhu J, Zhang Z, Han Y. A Familial Cluster of Infection Associated With the 2019 Novel Coronavirus Indicating Possible Person-to-Person Transmission During the Incubation Period. J Infect Dis. 2020;221:1757-1761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 422] [Cited by in RCA: 414] [Article Influence: 82.8] [Reference Citation Analysis (0)] |
| 9. | Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689-697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3012] [Cited by in RCA: 2504] [Article Influence: 500.8] [Reference Citation Analysis (0)] |
| 10. | Escalera-Antezana JP, Lizon-Ferrufino NF, Maldonado-Alanoca A, Alarcón-De-la-Vega G, Alvarado-Arnez LE, Balderrama-Saavedra MA, Bonilla-Aldana DK, Rodríguez-Morales AJ; LANCOVID. Clinical features of the first cases and a cluster of Coronavirus Disease 2019 (COVID-19) in Bolivia imported from Italy and Spain. Travel Med Infect Dis. 2020;35:101653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 11. | Qiu G, Gai Z, Tao Y, Schmitt J, Kullak-Ublick GA, Wang J. Dual-Functional Plasmonic Photothermal Biosensors for Highly Accurate Severe Acute Respiratory Syndrome Coronavirus 2 Detection. ACS Nano. 2020;14:5268-5277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 774] [Cited by in RCA: 679] [Article Influence: 135.8] [Reference Citation Analysis (0)] |
| 12. | Xiao AT, Tong YX, Zhang S. False negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: Rather than recurrence. J Med Virol. 2020;92:1755-1756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 352] [Cited by in RCA: 366] [Article Influence: 73.2] [Reference Citation Analysis (0)] |
| 13. | Li Y, Yao L, Li J, Chen L, Song Y, Cai Z, Yang C. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. 2020;92:903-908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 394] [Cited by in RCA: 446] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 14. | Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. AJR Am J Roentgenol. 2020;214:1280-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 662] [Cited by in RCA: 653] [Article Influence: 130.6] [Reference Citation Analysis (0)] |
| 15. | Maurea S, Mainolfi CG, Bombace C, Annunziata A, Attanasio L, Petretta M, Del Vecchio S, Cuocolo A. FDG-PET/CT imaging during the Covid-19 emergency: a southern Italian perspective. Eur J Nucl Med Mol Imaging. 2020;47:2691-2697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020;295:200463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1728] [Cited by in RCA: 1597] [Article Influence: 319.4] [Reference Citation Analysis (1)] |
| 17. | Bao C, Liu X, Zhang H, Li Y, Liu J. Coronavirus Disease 2019 (COVID-19) CT Findings: A Systematic Review and Meta-analysis. J Am Coll Radiol. 2020;17:701-709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 294] [Cited by in RCA: 270] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 18. | Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R, Hu T, Ding Y, Lin L, Gan Q, Luo L, Tang X, Liu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275-1280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 457] [Cited by in RCA: 491] [Article Influence: 98.2] [Reference Citation Analysis (0)] |
| 19. | Li X, Zeng W, Li X, Chen H, Shi L, Xiang H, Cao Y, Liu C, Wang J. CT imaging changes of corona virus disease 2019(COVID-19): a multi-center study in Southwest China. J Transl Med. 2020;18:154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 118] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 20. | Qin J, You C, Lin Q, Hu T, Yu S, Zhou XH. Estimation of incubation period distribution of COVID-19 using disease onset forward time: a novel cross-sectional and forward follow-up study. medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Yang L, Dai J, Zhao J, Wang Y, Deng P, Wang J. Estimation of incubation period and serial interval of COVID-19: analysis of 178 cases and 131 transmission chains in Hubei province, China. Epidemiol Infect. 2020;148:e117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 22. | Ye Q, Wang B, Mao J, Fu J, Shang S, Shu Q, Zhang T. Epidemiological analysis of COVID-19 and practical experience from China. J Med Virol. 2020;92:755-769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 23. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9315] [Article Influence: 1863.0] [Reference Citation Analysis (0)] |
| 24. | Kong TK. Longer incubation period of coronavirus disease 2019 (COVID-19) in older adults. Aging Med (Milton). 2020;3:102-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | Cimolai N. More data are required for incubation period, infectivity, and quarantine duration for COVID-19. Travel Med Infect Dis. 2020;37:101713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Khalili M, Karamouzian M, Nasiri N, Javadi S, Mirzazadeh A, Sharifi H. Epidemiological characteristics of COVID-19: a systematic review and meta-analysis. Epidemiol Infect. 2020;148:e130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 27. | Chen Q, Gao Y, Wang CS, Kang K, Yu H, Zhao MY, Yu KJ. Exploration of transmission chain and prevention of the recurrence of coronavirus disease 2019 in Heilongjiang Province due to in-hospital transmission. World J Clin Cases. 2021;9:5420-5426. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |