Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.5900
Peer-review started: February 25, 2021
First decision: April 14, 2021
Revised: April 19, 2021
Accepted: April 26, 2021
Article in press: April 26, 2021
Published online: July 26, 2021
Processing time: 145 Days and 21.6 Hours
For parturients with paroxysmal uterine contraction pain, rapid analgesia is needed. We used preprocedure ultrasound imaging combined with the palpation technique in epidural analgesia for labor, and evaluated the usefulness of this technique in epidural labor analgesia.
To evaluate the usefulness of preprocedure ultrasound imaging in epidural analgesia for labor.
In this prospective randomized observational study, 72 parturients were assigned to two groups (combined or palpation group). The target interspace of all parturients was first identified by the palpation technique. Then in the combined group, preprocedure ultrasound imaging was used before epidural puncture. In the palpation group, only the traditional anatomical landmarks technique (palpation technique) was performed. The primary outcome was total duration of the epidural procedure (for the ultrasound group, the duration of the preprocedure ultrasound imaging was included). The secondary outcomes were the number of skin punctures, the success rate at first needle pass, the number of needle passes, the depth from the skin to epidural space, and the complications of the procedure.
Total duration of the epidural procedure was similar between the two groups (406.5 ± 92.15 s in the combined group and 380.03 ± 128.2 s in the palpation group; P = 0.318). A significant improvement was demonstrated for epidural puncture and catheterization in the combined group. The number of needle passes was 1.14 in the combined group and 1.72 in the palpation group (P = 0.001). The number of skin puncture sites was 1.20 in the combined group and 1.25 in the palpation group (P = 0.398). The success rate at first needle pass was 88.89% in the combined group and 66.67% in the palpation group (P = 0.045).
This study demonstrated that the total duration of epidural procedures with preprocedure ultrasound imaging combined with the palpation technique was not longer than the traditional anatomical landmarks technique, which were performed by six experienced anesthesiologists in parturients with normal weights undergoing labor analgesia.
Core Tip: This is the first study of preprocedure ultrasound imaging combined with the palpation technique in epidural labor analgesia. This combined technique increases the first-pass success rate of epidural catheterization but does not increase the total procedural time in labor analgesia.
- Citation: Wu JP, Tang YZ, He LL, Zhao WX, An JX, Ni JX. Preprocedure ultrasound imaging combined with palpation technique in epidural labor analgesia. World J Clin Cases 2021; 9(21): 5900-5908
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/5900.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.5900
Epidural analgesia can provide effective pain control in obstetrics[1], but the obesity and edema of parturients can increase challenges in performing the epidural puncture. For parturients with paroxysmal uterine contraction pain who opt to have labor pain relief, rapid analgesia is needed. Therefore, a rapid and effective epidural puncture is particularly important for parturients requiring labor analgesia.
Preprocedure ultrasound imaging can improve the safety and efficacy of epidural puncture especially in difficult cases[2-9], but it requires time and ultrasound imaging of the spine is more complex than imaging of other parts of the body; thus, clinical ultrasound measurement for labor analgesia is not frequently practiced[2].
In previous studies, preprocedure ultrasound imaging needs several steps. First, the paramedian sagittal oblique view was obtained to identify the sacrum, the five lumbar intervertebral spaces, and the target interspace[10,11]. Second, the transverse interlaminar view of the target interspace was obtained, the depth of the epidural space was measured, and the needle insertion point was marked[9,10]. This preprocedure ultrasound imaging needs some time. In our combined technique, first, the target interspace was obtained by landmark palpation. Second, the transverse interlaminar view of the target interspace was obtained, the depth of the epidural space was measured, and needle insertion point was marked. This technique needs less procedure time.
This study was conducted to compare the total duration of the epidural procedure (including the duration of preprocedure ultrasound imaging in the combined group), and the safety of the epidural procedure between the combined and palpation groups. We determined whether the combined technique increased the total duration of the epidural procedure and improved the success rate of epidural analgesia.
This study was a prospective randomized controlled study. After obtaining approval from the institutional ethical committee, this study was conducted with healthy parturients admitted to the Department of Obstetrics and Gynecology. The study was conducted between January and May 2018 and reviewed and approved by the local university’s institutional review board (IRB). All data collection and data management were conducted according to the IRB-approved protocol (ChiCTR1800014782). Informed written consent was obtained from every parturient.
The inclusion criteria were as follows: healthy pregnancy and singleton birth, age ≥ 18 and ≤ 40 years, American Society of Anesthesiologists physical status II or above, active labor (regular contractions and cervical dilation ≥ 2 cm), no history of caesarean for dystocia, absence of contraindications to epidural blockade, absence of previous analgesia with opioids, absence of cephalopelvic disproportion, and absence of psychopathological disorders and substance abuse.
The exclusion criteria were as follows: body mass index ≥ 35 kg/m2; patient refusal; pregnancy-induced hypertension; systemic hypertension; diabetes mellitus; heart disease; previous lower segment caesarean section; or any contraindication to neuraxial anesthesia such as coagulopathy, increased intracranial pressure, un
Standard monitors were applied, and the parturient was placed in the left lateral position throughout the procedure. In two groups, the anatomical landmarks were the intercristal (Tuffier) line, which was assumed to cross the L3–L4 interspace or L4 spinous process. The target interspace was the L3–L4 interspace. In the ultrasound group, preprocedure ultrasound imaging was used before epidural puncture. In the palpation group, the traditional palpation technique was performed.
In the combined group, a 2-5 MHz curved array probe was used for all cases using a three-step approach[12,13] (GE Healthcare, Chalfont St. Giles, United Kingdom). (1) The target interspace of the parturient was identified by the palpation technique. (2) The transverse interlaminar view of the target interspace and the best sonographic image was observed. The depth of the epidural space was measured (distance from the skin surface to the ventral aspect of the ligamentum flavum-dura mater complex). (3) The horizontal and vertical lines were marked at the midpoints of the probe’s short and long sides, respectively[14], and the needle insertion point was marked at the intersection point of the two lines.
With proper aseptic and antiseptic precautions, the puncture site was infiltrated with lidocaine with an an 18-gauge Tuohy needle (Perifix®; Braun, Melsungen, Germany) using the loss of resistance technique to air, and then a multi-hole epidural catheter was inserted at the L3-4 intervertebral space. In the combined group, the loss-of-resistance test was started when the travel distance of the epidural needle was 0.5 cm less than the pre-estimated depth.
The catheter was placed in the epidural space 3-4 cm in the cephalic direction. Then 3 mL of 1.5% lidocaine was administered to exclude intravenous or subarachnoid catheter placement. Next, a dose of 12 mL ropivacaine at a concentration of 0.094% was administered without opioids. Instructions for use of the patient-controlled epidermal analgesia (PCEA) pump (Rehn Medtech Ltd., Jiangsu, China) were provided to the parturient after the epidural catheter was inserted. The instructions included specific directions to each woman to press the button whenever she began to feel discomfort, and to wait a few minutes in order to feel its analgesic effect. The setting of the PCEA was: bolus 6 mL, lockout 12 min, no background infusion[15]. Self-delivered boluses were infused at a standard delivery rate of 60 mL × h-1 (one bolus per 6 min).
In both groups, we measured the total time for the epidural procedures. For the combined group, this included the time for the ultrasound measurements, the epidural puncture and catheterization. For the palpation group, this only included the epidural puncture and catheterization procedures. Warm-up time of the ultrasonography was not evaluated[16]. The duration of procedures was recorded by other investigators (nurses who assisted the anesthesiologist).
We counted the success rate at the first needle pass, the number of needles passes, and the skin puncture sites. A needle pass meant advancement of the needle, and retracement of the puncture needle was counted as one needle pass. If the epidural space could not be punctured in the first puncture site, a neighboring vertebral interspace was selected. A successful puncture at the first needle pass means “direct access” after skin puncture[9].
The complications of the procedure such as unintentional dural and vascular punctures, nerve irritation, backache during the procedure, unilateral or patchy block and failed block were observed by the primary investigators (the anesthesiologist).
The results are presented as the mean ± SD and percentages. The χ2 test was used to compare the categorical/dichotomous variables between the groups. A t-test was used to compare the means of the variables between the groups. P < 0.05 was considered statistically significant. All analyses were carried out using SPSS 19.0 version (Statistical Package for the Social Sciences, Chicago, IL, United States).
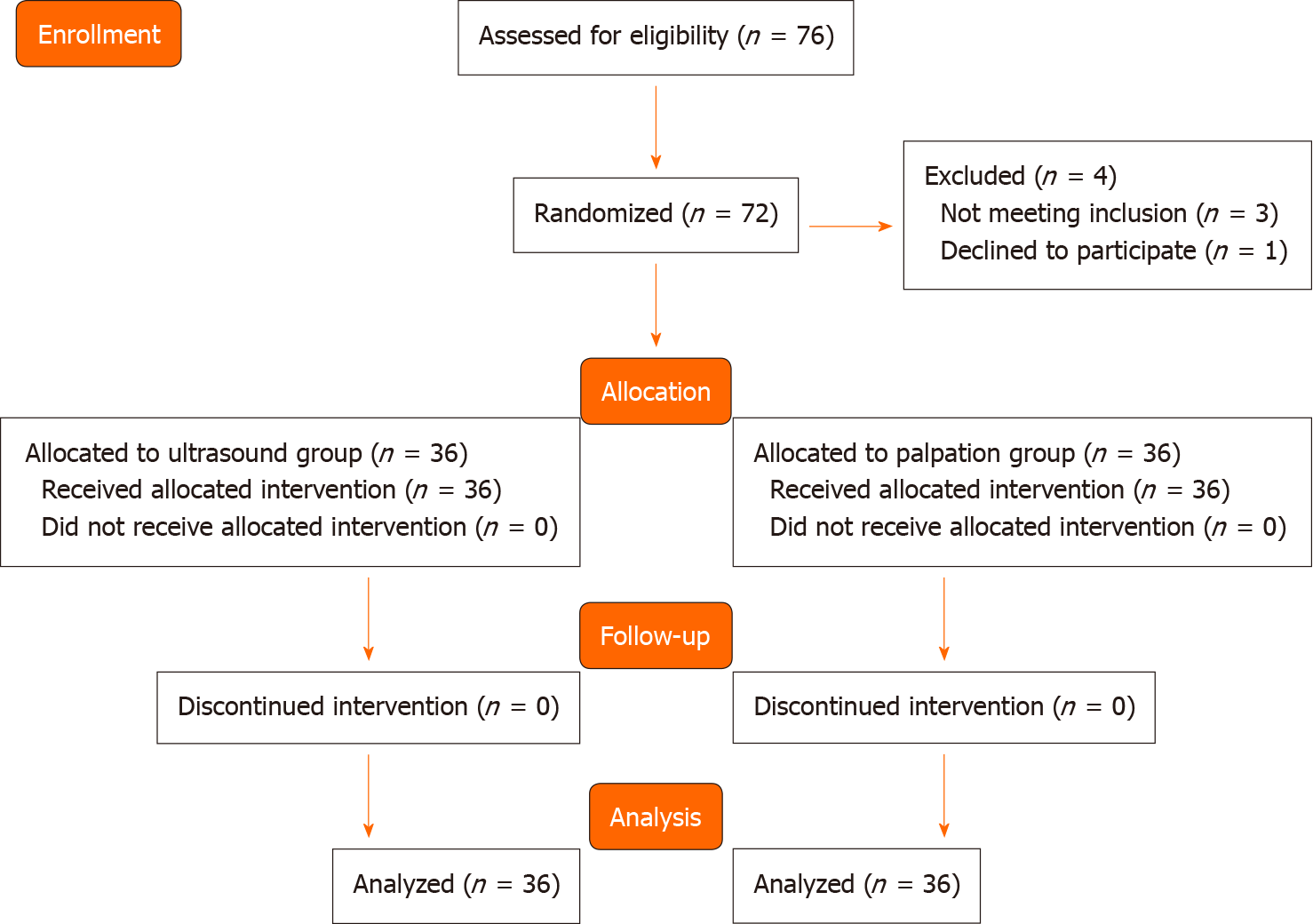
Seventy-six patients were assessed for eligibility. Three did not meet the inclusion criteria and one declined to participate. Data from 72 patients (36 in each group) were analyzed (Figure 1). The baseline characteristics of the patients were similar between two groups (Table 1).
| All parturient | Combined group (n = 36) | Palpation group (n = 36) | P value |
| Age (yr) | 29.25 ± 3.05 | 29.39 ± 2.72 | 0.248 |
| Height (cm) | 162.06 ± 4.65 | 162.08 ± 5.04 | 0.507 |
| Weight (kg) | 72.56 ± 10.2 | 69.33 ± 7.96 | 0.645 |
| BMI (kg/m2) | 27.61 ± 3.59 | 26.37 ± 2.67 | 0.213 |
| ASA classification | 2.0 ± 0.61 | 2.0 ± 0.53 | 0.985 |
The mean total duration of the epidural procedures was 406.5 ± 92.15 s in the combined group and 380.03 ± 128.2 s in the palpation group (P = 0.318). The mean time for preprocedural ultrasound imaging in the combined group was 85.83 ± 3.92 s (Table 2).
| All parturients | Combined group (n = 36) | Palpation group (n = 36) | P value |
| Total duration of the epidural procedure(s) | 406.5 ± 92.15 | 380.0 ± 128.2 | 0.318 |
| Time to perform epidural puncture and catheterization procedure (s) | 320.62 ± 87.33 | 380.0 ± 128.2 | 0.0011 |
| Time to perform ultrasound procedure (s) | 85.83 ± 3.92 | NA | NA |
The number of needle passes was 1.14 in the combined group and 1.72 in the palpation group (P = 0.001). The number of skin puncture sites was 1.20 in the combined group and 1.25 in the palpation group (P = 0.398). The success rate at first needle pass was 88.89% in the combined group and 66.67% in the palpation group (P = 0.045) (Table 3).
The rate of complications from the procedure (nerve irritation during the procedure, backache during the procedure, unintentional dural and vascular punctures, unilateral or patchy block and failed block) was low (Table 4). One unintentional dural puncture occurred in each group. There were 7 cases of unintentional vascular punctures (1 case in the combined group and 6 cases in the palpation group), 5 cases of nerve irritation during the procedure (1 case in the combined group and 4 cases in the palpation group), and 3 cases of backache during the procedure (1 case in the combined group and 2 cases in the palpation group). One case of unilateral block occurred in each group and a second epidural puncture was administered to the patients. There were no significant differences between the two groups regarding the rate of complications from the procedures (Table 4).
| No. of patients with side effects | Combined group (n = 36) | Palpation group (n = 36) | P value |
| Vascular puncture | 1 | 6 | 0.107 |
| Dural puncture | 1 | 1 | 0.754 |
| Nerve irritation during the procedure | 1 | 4 | 0.201 |
| Backache during the procedure | 1 | 2 | 0.555 |
| Unilateral or patchy block | 1 | 1 | 0.754 |
| Failed block | 1 | 2 | 0.555 |
This randomized controlled trial demonstrated no lengthening of the total duration of the epidural procedure with preprocedure ultrasound combined with the palpation technique, which was performed by six experienced anesthesiologists in parturients with normal weights undergoing labor analgesia. The total duration of the epidural procedure included the time for the ultrasound measurements, epidural puncture and catheterization in the combined group and only the epidural puncture and catheterization in palpation group. The total duration of the epidural procedure was com
Our study showed a significant improvement of the epidural puncture and catheterization procedures when using preprocedure ultrasound imaging combined with the palpation technique compared with the traditional palpation technique for labor analgesia. Our outcomes demonstrated significant differences of needle passes (1.14 vs 1.72, respectively; P = 0.001) and first-pass success rate between the combined and palpation group (88.89% vs 66.67%, respectively; P = 0.045). A publication in 2016 based on two meta-analyses reported that the preprocedure spinal ultrasound increased the first-pass success rate compared with the traditional palpation technique[7]. Ansari et al[11] reported that the use of preprocedure ultrasound reduced the number of punctures and was associated with improved efficacy of the neuraxial block and higher patient satisfaction in obstetrics. Our outcome was similar to these studies, and demonstrated that preprocedure ultrasound imaging can facilitate epidural catheterization compared with the traditional palpation technique.
The mean depth from the skin to epidural space was 4.40 ± 0.45 (3.3 to 5.8) cm in the combined group and 4.41 ± 0.52 (3.1 to 5.7) in the palpation group (P = 0.965). There were no significant differences between the two groups. The mean depth to the epidural space from the skin has been recorded as 4.6–5.3 cm in a Michigan parturient[18,19]; in this study, we found that the mean depth to the epidural space from the skin was 4.1-4.7 cm in a Beijing parturient.
In this study, the ultrasound was in the labor room and the anesthesiologist had experience of neuraxial block for more than 6 mo. We showed that using ultrasound did not lengthen the total duration of the epidural procedures compared with the traditional palpation technique, which were performed by three experienced anesthesiologists in parturients with normal weights undergoing labor analgesia. Meanwhile, using ultrasound can improve the safety and efficacy of the epidural puncture, which is meaningful for parturients who need rapid and effective epidural puncture while the painful labor continues. It is also meaningful for the application of ultrasound in obstetrical analgesia.
There were three differences for our study compared with other previous studies. First, we recorded the time taken to perform the ultrasound imaging, the epidural puncture and catheterization in our study. Ansari et al[11] recorded the time from the time of skin puncture to the time of viewing cerebrospinal fluid between the landmark and the ultrasound groups in spinal anesthesia. Tawfik et al[17] recorded the median (range) duration of the epidural procedure in the ultrasound group and in the palpation group. In those studies, the total time for ultrasound imaging, the epidural puncture and catheterization were not recorded. The total procedural time could not be compared in these studies, but this total procedural time is important for the widespread use of ultrasound in obstetrical analgesia. Second, we excluded obese parturients. Many studies have shown that preprocedure ultrasound facilitates the epidural procedure and decreases the complication rate especially in obese parturients[4] or those with difficult landmarks[3]. This study excluded obese parturients to reduce the impact on results. Third, we did not analyze the difficulty level of palpable landmarks for parturients. The difficulty level of the palpable landmarks was associated with the experience of the anesthesiologist and the degree of obesity of the parturient.
Two limitations of this study are worth noting. First, the sample size was relatively small, and it was not sufficient to illustrate the differences in complications such as vascular puncture, dural puncture, and nerve irritation between the two groups. Second, maternal satisfaction was not assessed. The maternal satisfaction to epidural catheterization can show the superiority of preprocedure ultrasound measurement in epidural analgesia for labor[20].
This study demonstrated no lengthening of the total duration of the epidural procedures with preprocedure ultrasound imaging combined with the palpation technique compared with traditional anatomical landmarks technique, which were performed by six experienced anesthesiologists in parturients with normal weights undergoing labor analgesia. A significant improvement in epidural puncture and catheterization with preprocedure ultrasound was demonstrated in this study. An actual clinical benefit was found for preprocedure ultrasound for epidural analgesia for labor.
Rapid and effective epidural puncture is particularly important for parturients requiring labor analgesia.
To determine whether the combined technique increases the total duration of the epidural procedure and improves the success rate of the epidural analgesia.
Seventy-two parturient were assigned to two groups (combined or palpation group). All epidurals were performed by six anesthesiologists.
Preprocedure ultrasound imaging combined with palpation technique was used in this study.
Total duration of the epidural procedure was similar between two groups. A significant improvement was demonstrated for epidural puncture and catheterization in the combined group.
A significant improvement in epidural puncture and catheterization with preprocedure ultrasound was demonstrated.
Ultrasound-guided epidural puncture and catheterization should be studied in future.
Manuscript source: Unsolicited manuscript
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mosquera-Klinger G S-Editor: Wang JL L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Marhofer P, Willschke H, Kettner S. Current concepts and future trends in ultrasound-guided regional anesthesia. Curr Opin Anaesthesiol. 2010;23:632-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Bhatia K, Kochhar P, Clegg I, Maguire S. The availability and use of ultrasound in UK obstetric anaesthesia. Int J Obstet Anesth. 2016;25:91-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Grau T, Leipold RW, Conradi R, Martin E. Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand. 2001;45:766-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 137] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Wang Q, Yin C, Wang TL. Ultrasound facilitates identification of combined spinal-epidural puncture in obese parturients. Chin Med J (Engl). 2012;125:3840-3843. [PubMed] |
| 5. | Sahin T, Balaban O, Sahin L, Solak M, Toker K. A randomized controlled trial of preinsertion ultrasound guidance for spinal anaesthesia in pregnancy: outcomes among obese and lean parturients: ultrasound for spinal anesthesia in pregnancy. J Anesth. 2014;28:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Yoshida T, Shimizu H, Furutani K, Baba H. Unintentional epidural placement of a thoracic paravertebral catheter inserted using an ultrasound-guided technique: a case report. J Anesth. 2016;30:727-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Arzola C. Preprocedure Ultrasonography Before Initiating a Neuraxial Anesthetic Procedure. Anesth Analg. 2017;124:712-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Perlas A, Chaparro LE, Chin KJ. Lumbar Neuraxial Ultrasound for Spinal and Epidural Anesthesia: A Systematic Review and Meta-Analysis. Reg Anesth Pain Med. 2016;41:251-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 147] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 9. | Arzola C, Mikhael R, Margarido C, Carvalho JC. Spinal ultrasound versus palpation for epidural catheter insertion in labour: A randomised controlled trial. Eur J Anaesthesiol. 2015;32:499-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Shaikh F, Brzezinski J, Alexander S, Arzola C, Carvalho JC, Beyene J, Sung L. Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta-analysis. BMJ. 2013;346:f1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 160] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 11. | Ansari T, Yousef A, El Gamassy A, Fayez M. Ultrasound-guided spinal anaesthesia in obstetrics: is there an advantage over the landmark technique in patients with easily palpable spines? Int J Obstet Anesth. 2014;23:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Ecimovic P, Loughrey JP. Ultrasound in obstetric anaesthesia: a review of current applications. Int J Obstet Anesth. 2010;19:320-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Balki M, Lee Y, Halpern S, Carvalho JC. Ultrasound imaging of the lumbar spine in the transverse plane: the correlation between estimated and actual depth to the epidural space in obese parturients. Anesth Analg. 2009;108:1876-1881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 115] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 14. | Vezzani A, Manca T, Brusasco C, Santori G, Cantadori L, Ramelli A, Gonzi G, Nicolini F, Gherli T, Corradi F. A randomized clinical trial of ultrasound-guided infra-clavicular cannulation of the subclavian vein in cardiac surgical patients: short-axis versus long-axis approach. Intensive Care Med. 2017;43:1594-1601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Huang BW, Huang Q, Liao JH. Optimum interval time of intermittent epidural bolus for labor analgesia. Guangdong Yikedaxue Xuebao. 2018;36:647-649. |
| 16. | Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth. 2002;14:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 176] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 17. | Tawfik MM, Atallah MM, Elkharboutly WS, Allakkany NS, Abdelkhalek M. Does Preprocedural Ultrasound Increase the First-Pass Success Rate of Epidural Catheterization Before Cesarean Delivery? Anesth Analg. 2017;124:851-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Warman P, Youngs P. An observational study of the relationship between lumbar epidural space depth and body mass index in Michigan parturients. Int J Obstet Anesth. 2008;17:283; author reply 283-283; author reply 284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Watts RW. The influence of obesity on the relationship between body mass index and the distance to the epidural space from the skin. Anaesth Intensive Care. 1993;21:309-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Melese T, Gebrehiwot Y, Bisetegne D, Habte D. Assessment of client satisfaction in labor and delivery services at a maternity referral hospital in Ethiopia. Pan Afr Med J. 2014;17:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |