Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5695
Peer-review started: March 5, 2021
First decision: April 13, 2021
Revised: April 21, 2021
Accepted: April 23, 2021
Article in press: April 23, 2021
Published online: July 16, 2021
Processing time: 123 Days and 23.1 Hours
Biliary ascariasis is rare but remains the most common parasitic infection in remote areas and in people with poor medical conditions. Here, we reported a case of biliary ascariasis in order to raise awareness of possible parasitic infections.
A 68-year-old female was admitted to the emergency room of the Affiliated Hospital of Guizhou Medical University on 28 September 2017, with chief complaint of pain in the right upper abdomen. Ultrasonography of the abdomen showed that the upper segment of the common bile duct was slightly dilated with parallel tubular structures, indicative of biliary ascariasis. Endoscopic retrograde cholangiopancreatography was performed under general anesthesia on 29 September 2017, and an adult Ascaris lumbricoides worm was observed. After the worm was removed from the bile duct, the patient’s pain immediately subsided. The patient was successfully cured, without any complications.
This report emphasizes the need for physicians to consider biliary ascariasis as a possible cause when treating cases of biliary colic.
Core Tip: As far as we know, biliary ascariasis is an extremely rare infectious disease. The clinical symptoms of biliary ascariasis are similar to those of biliary calculi, so the differential diagnosis is very important. This case is a typical biliary ascariasis. After detailed physical examination, biochemical examination, abdominal ultrasound and endoscopic retrograde cholangiopancreatography technology, we finally successfully diagnosed and treated biliary ascariasis. In order to attract clinical attention and effective treatment, this article reviews the literature on the diagnosis and treatment of biliary ascariasis.
- Citation: Wang X, Lv YL, Cui SN, Zhu CH, Li Y, Pan YZ. Endoscopic management of biliary ascariasis: A case report. World J Clin Cases 2021; 9(20): 5695-5700
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5695.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5695
Ascaris infections are usually asymptomatic. However, among the surgical complications of ascariasis, biliary metastasis is the most common. It not only causes severe pain but even endangers the patient’s life. Although the natural habitat of ascaris is usually in the jejunum, they can still enter the biliary tract, causing biliary colic, obstructive jaundice, and cholelithiasis. Biliary ascaris itself not only causes severe pain but it too can even endanger the life of the patient. We report this rare case of biliary ascariasis in order to improve the understanding of ascariasis and make a differential diagnosis for patients with abdominal colic.
A 68-year-old female was admitted to the Emergency Department of the Affiliated Hospital of Guizhou Medical University on 28 September 2017, with chief complaint of colic in the right upper abdomen that radiated into the back. She had no nausea, vomiting, fever, night sweats, chest tightness nor palpitations.
Upon enquiry, the patient revealed that she had been suffering from recurrent pain in the right upper abdomen for 2 years and received no special treatment for her symptoms. The pain had worsened in the past 2 d.
Additionally, the patient had a history of gastritis and urethritis for many years. She mentioned that she enjoyed eating raw and cold vegetables and fruits.
The patient had no remarkable personal or family history.
The patient’s vital signs were normal and abdominal examination revealed a soft abdomen, mild tenderness in the right upper abdomen, with no rebound pain or cholecystitis.
The vital parameters were recorded as follows: eosinophils 0.54 G/L; red blood cells 3.52 T/L; and, hemoglobin 112.00 g/L. Normal results were acquired for testing of hepatic and kidney functions, electrolyte levels and blood coagulation function.
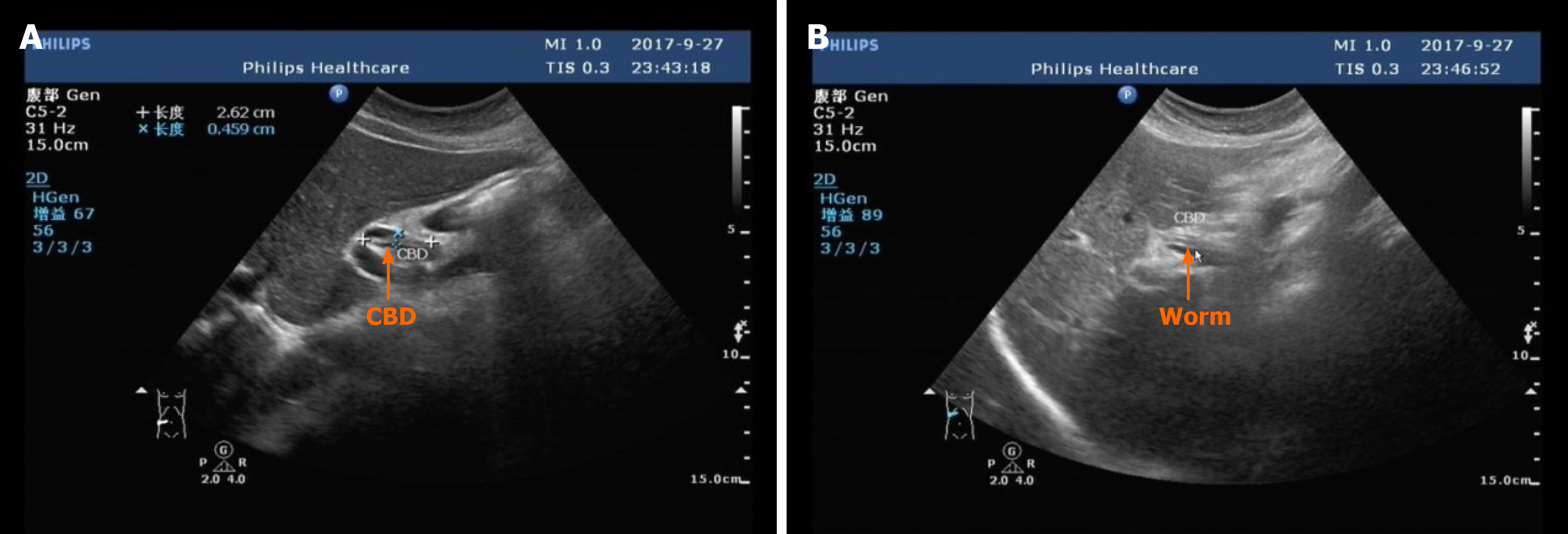
Abdominal ultrasound revealed that the gallbladder was normal in size and shape; the upper segment of the common bile duct was about 28 mm long and 4 mm wide, slightly dilated and parallel to the tubular structure, without obvious peristalsis (Figure 1). A preliminary diagnosis of biliary ascariasis was made. No abnormalities were found in the liver, pancreas, spleen and kidneys. Cholangitis due to biliary ascaris was suspected.
A diagnosis of ascaris worm was made by microbiological analysis.
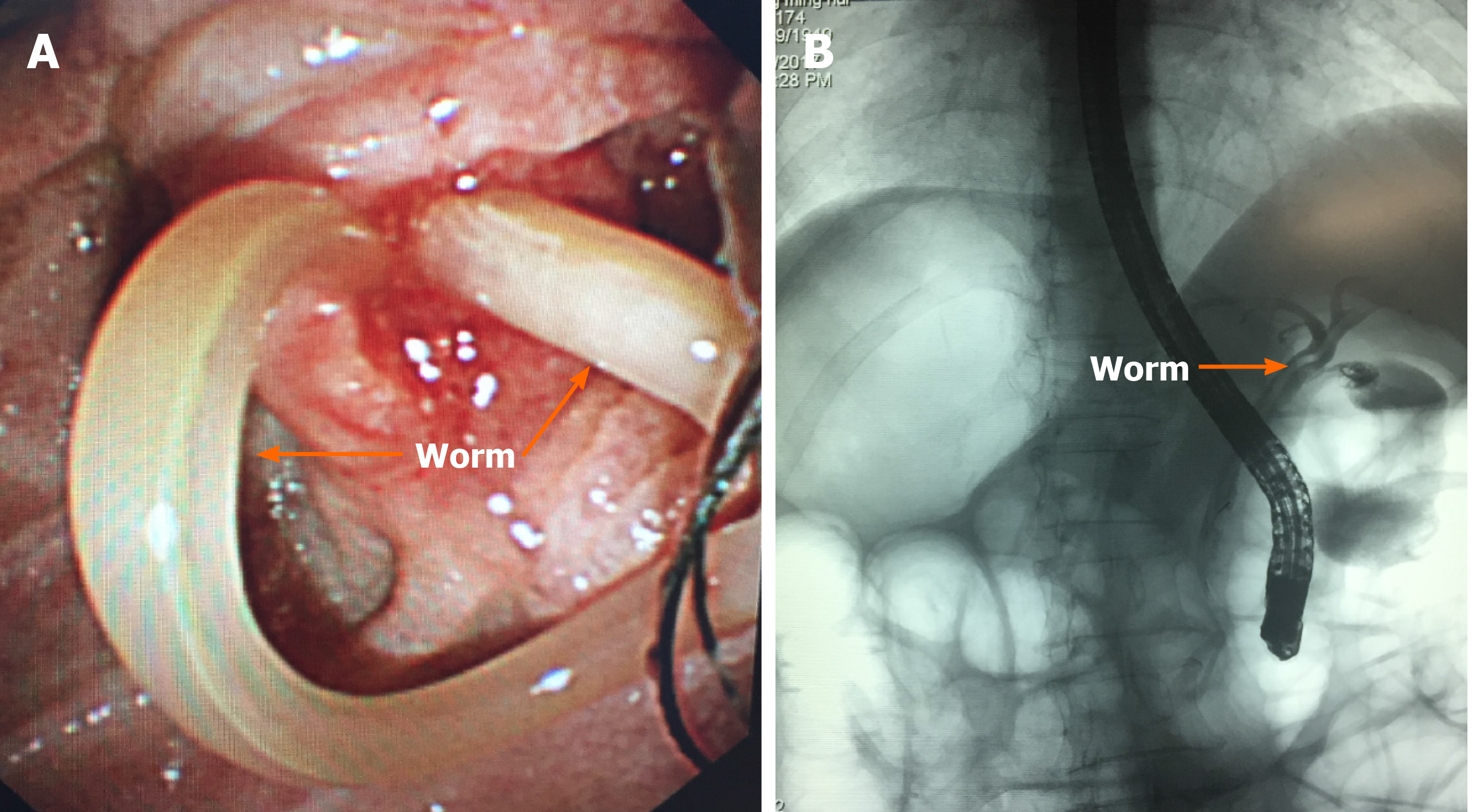
Therefore, the patient was referred for endoscopic retrograde cholangiopancreatography (ERCP) (Figure 2). No dilatation of intrahepatic bile ducts was detected, and an active worm shadow was seen from the common bile duct to the right hepatic duct. The worm was extracted from the bile duct using a stone net. Subsequently, the contrast agent was re-injected and there was no worm residue in the common bile duct cavity. The lower end of the common bile duct was unblocked, and a large amount of contrast agent was found in the intestinal tract. An endoscopic nasobiliary drainage tube was placed.
The patient's pain rapidly eased after the worm was extracted and the anthelminthic drug albendazole was administered. The endoscopic nasobiliary drainage tube was removed on the third day when bile drainage had ceased, and the patient was discharged without any complications. She was advised to take rest and maintain dietary hygiene to improve nutrition. The patient was doing well at a follow-up visit 1 year after discharge, and no recurrence of biliary ascariasis was found during ongoing surveillance.
With the development of the health industry, improvement of people's living standards and enhancement of health awareness worldwide, the incidence of ascariasis has been steadily decreasing. However, in some remote rural areas, its incidence remains relatively high[1,2]. In China, ascariasis is very common among rural residents[3].
Ascaris lumbricoides worm rarely enters the biliary system. However, in case of duodenal papillary muscle dysfunction or changes in the intestinal parasitic environment, the Ascaris lumbricoides worm may move to the duodenum and enter the biliary tract through the opening of the papillary muscle, causing spasms in the sphincter of Oddi and bile duct, and paroxysmal abdominal cramps. Its typical feature is paroxysmal colic on the right side of the xiphoid process, which may be accompanied by nausea, vomiting, jaundice, etc.[4]. If the patient is not referred to the hospital in time, severe dehydration and toxic shock will occur, known as biliary ascariasis, which will endanger the life and health of the patient. Biliary ascaris worm can be located anywhere in the biliary tract, but is more commonly found in the bile duct and rarely in the gallbladder. This is because the angle between the gallbladder tube and bile duct is larger, so the ascaris worm cannot easily enter the gallbladder[5,6].
Biliary ascariasis cannot be definitively diagnosed solely based on clinical manifestations and fecal egg examination. With the development of modern imaging diagnostic techniques, the diagnosis of biliary tract diseases has greatly progressed. At present, there are many imaging diagnostic methods for biliary tract diseases, such as B-ultrasound, computed tomography, magnetic resonance imaging, etc., which enable direct and vivid diagnosis of biliary obstruction[7,8]. Ultrasonic diagnosis of biliary ascariasis is non-invasive and easy, with high sensitivity, strong specificity and safety, and is often used as the first choice. It shows the shape of ascaris worm and can reveal the characteristic movement of the worm in the biliary tree. The typical B-ultrasound image of ascaris worm shows tubular echo structure without shadow[9].
The treatment of biliary ascariasis involves the following three clinical modalities: "non-surgical treatment with integrated traditional Chinese and Western medicine"; "surgical treatment"; and, "endoscopic treatment"[3]. Non-surgical treatment of biliary ascariasis includes antispasmodic, analgesic, antibacterial and choleretic agents, which shows slow progress with uncertain therapeutic effect[10,11]. Moreover, it may lead to death of ascaris worm in the biliary tract, causing gallstones and other complications[12].
For patients with poor medical treatment or with severe hepatobiliary infection, surgical treatment may be considered[13-15]. When there are no complications of biliary ascariasis, choledocholithotomy and T-tube drainage can be used. However, the worms often move out of the biliary tract when the biliary tract is explored. There are also cases where ascaris worms reenter the biliary tract after surgery and relapse. Moreover, choledocholithotomy and T-tube drainage involve major trauma, slow recovery and long recovery time[16].
With the development of endoscopic diagnosis and treatment, removal or deworming of Ascaris lumbricoides worms by endoscopy has achieved great success[17]. ERCP is a confirmatory test to determine the presence of Ascaris lumbricoides worms in the biliary system, and can be simultaneously used to visualize and treat ascariasis, which is both diagnostic and therapeutic method. During ERCP in the present case, it was found that the Ascaris lumbricoides worm did not completely enter the common bile duct and was incarcerated in the duodenal papilla. Hence, it could be extracted by placing a stone net through a fiber duodenoscope. In case of complete entry of worm into the biliary tract, duodenal papillary sphincter incision can be performed through the fiberoptic duodenoscope to remove the worm, which can also be used for examination purposes, local irrigation and medication[18-20]. ERCP can be simultaneously used for the treatment of biliary ascariasis at the time of diagnosis. The operation is performed through the normal physiological channels, which not only reduces the damage to the body but also treats the common bile duct-associated diseases while eliminating the etiology, thus reducing the risk of surgery and the occurrence of complications. It is a safe and effective method for the treatment of biliary ascariasis[21,22].
A clear diagnosis upon admission is extremely important. The main symptom of biliary ascariasis is abdominal pain, which can be easily misdiagnosed as other hepatobiliary diseases that cause abdominal pain, such cholecystitis, gallstone, liver cancer, various hepatitis and other diseases[23]. Therefore, the medical history should be inquired in detail, physical examination should be carefully performed, necessary laboratory and instrument examinations should be conducted in a timely manner, such as ultrasound, and attention should be paid to differential diagnosis. Endoscopic treatment and postoperative anti-ascariasis therapy can achieve better efficacy for biliary ascariasis[24,25]. Given the high incidence of biliary ascariasis in rural areas in China, strengthening information and education is an important measure to prevent this disease. Hence, health knowledge should be widely publicized, so that the people living in rural areas develop good hygiene habits, wash hands before meals, do not eat unwashed fruits and vegetables, do not drink dirty water, etc.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Marusic M S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
| 1. | Khuroo MS, Rather AA, Khuroo NS, Khuroo MS. Hepatobiliary and pancreatic ascariasis. World J Gastroenterol. 2016;22:7507-7517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 86] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (2)] |
| 2. | Ramzan Z, Anzengruber F. A case of biliary ascariasis. Isr Med Assoc J. 2014;16:324-325. [PubMed] |
| 3. | Wang Y, Liu J. Biliary ascariasis: particular cause of biliary tract infection. Hepatobiliary Surg Nutr. 2020;9:119-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Mansilla-Vivar R, Sainza Caballero E, Saldaña Dueñas C, Casanova Ortiz L, Fernandez-Urien I, Vila Costas JJ. Biliary ascariasis as etiology of recurrent abdominal pain. Endoscopy. 2016;48 Suppl 1:E196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Choi JH, Seo M. A Case of Biliary Ascariasis in Korea. Korean J Parasitol. 2017;55:659-660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Thandassery RB, Jha AK, Goenka MK. Biliary ascariasis: an uncommon cause for recurrent biliary colic after biliary sphincterotomy and common bile duct stone removal. Trop Doct. 2014;44:108-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Villa-Gómez Roig G, Mahler MA, Manazzoni D, Villa-Gomez M, Vidales G, Marcolongo M. Spectrum of biliary parasites affecting the biliary tree (Fasciola hepatica, Echinococcus granulosus, and Ascaris lumbricoides). Endoscopy. 2018;50:E224-E226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Stojanov D, Slavkovic A, Bukvić N. Biliary ascariasis in a 6-month old child. Hippokratia. 2015;19:288. [PubMed] |
| 9. | Darlington CD MBBS, MS, Anitha GFS MBBS, MD. Ascaridial Volvulus: An Uncommon Cause of Ileal Perforation. Iran J Med Sci. 2018;43:432-435. [PubMed] |
| 10. | Azhar M, Sheikh AS, Khan A, Mustafa S, Shah IA, Hameed B. Hepatobiliary ascaeiasis complicated by pancreatitis. J Ayub Med Coll Abbottabad. 2015;27:479-481. [PubMed] |
| 11. | Das AK. Hepatic and biliary ascariasis. J Glob Infect Dis. 2014;6:65-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Balasubramanian G. An unusual cause of biliary colic. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Keshvala C, Naidu L. Not everything in the gallbladder is gallstones: an unusual case of biliary ascariasis. BJR Case Rep. 2019;5:20180123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Sharma M, Somani P, Prasad R, Jindal S, Pathak A. Biliary ascariasis: mimicker of biliary stent. VideoGIE. 2017;2:179-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Sharma M, Shoukat A, Kirnake V, Bennett A. Idiopathic Acute Pancreatitis: Role of EUS With Reference to Biliary and Pancreatic Ascariasis. Am J Gastroenterol. 2015;110:1367-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Sharma M, Showkat A, Somani P. An Unusual Cause of Biliary Colic. Gastroenterology. 2017;153:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lohala N, Gurung RB, Bhattarai R, Lama A. An Unwanted Guest in the Biliary Tract: A Case Report. JNMA J Nepal Med Assoc. 2019;57:371-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Sharma A, Jariwala P, Kaur N. Biliary ascariasis presenting with gangrenous perforation of the gall bladder: report of a case and brief review of literature. Trop Doct. 2018;48:242-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Somani P, Sharma M, Jindal S. Endoscopic ultrasound appearance of dead Ascaris lumbricoides in the biliary tract. Endoscopy. 2017;49:E275-E276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Kong F, Xi H, Bai Y, Li Z. Ascaris infestation of biliary tree mimicking gallbladder cancer. Dig Liver Dis. 2015;47:e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | de Almeida BL, Silva DV, do Rosário MS, Gonçalves BSD, Nunes MG, Ney ALCM, Silvany C, de Siqueira IC. Biliary ascariasis and severe bacterial outcomes: Report of three cases from a paediatric hospital in Brazil. Int J Infect Dis. 2020;95:115-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Bundela V, Gupta P, Mandavdhare HS, Dutta U, Sharma V. Gastrointestinal: An unusual cause of biliary colic: Biliary ascariasis. J Gastroenterol Hepatol. 2018;33:975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Mohd Noor NA, Goh SN, Tan CH. Biliary Ascariasis: An Unusual Case of Obstructive Jaundice. Clin Gastroenterol Hepatol. 2020;18:A16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Sundriyal D, Mittal G, Kumar S, Manjunath S, Sharma N, Gupta M. Biliary Ascariasis Mimicking Colonic Tumor Infiltration of the Biliary System. Indian J Surg Oncol. 2015;6:280-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Lynser D, Handique A, Daniala C, Phukan P, Marbaniang E. Sonographic images of hepato-pancreatico-biliary and intestinal ascariasis: A pictorial review. Insights Imaging. 2015;6:641-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |