Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5683
Peer-review started: March 4, 2021
First decision: April 29, 2021
Revised: May 5, 2021
Accepted: May 26, 2021
Article in press: May 26, 2021
Published online: July 16, 2021
Processing time: 124 Days and 20.4 Hours
Submucosal hematoma (SH) is one of the rare causes of upper gastrointestinal bleeding. As a rare and critical disease in clinical practice, it should be paid more attention to by clinicians to avoid missed diagnosis and misdiagnosis. Most of the esophageal submucosal hematomas have clear causes, including retrosternal pain, dysphagia, etc. Here, we report a rare case of SH extending from the hypopharynx to the lower esophagus caused by oral administration of hirudin and panax notoginseng powder, with atypical clinical manifestation. Such a long submucosal hematoma has rarely been reported.
The patient was a 60-year-old male with a history of gastritis, hypertension, coronary heart disease, and coronary stent implantation. The patient developed chest tiredness and heartburn after taking 10 capsules of a homemade mixture of hirudin and notoginseng powder in the previous 2 d. He did not have hematemesis or black stool. Gastroscopy and chest computed tomography confirmed the diagnosis of SH, which ranged from the pharynx to the lower esophagus and was 35-40 cm in length. After the diagnosis was confirmed, we performed active conservative treatment on the patient, and the patient recovered well and remained asymptomatic during the 26-mo follow-up.
SH is rare, and cases with atypical clinical symptoms may lead to misdiagnosis and missed diagnosis. Ignorance of this disease can lead to serious clinical consequences. Conservative therapy is effective and the prognosis is good.
Core Tip: Esophageal submucosal hematoma is a rare cause of upper gastrointestinal bleeding. As an acute and critical disease rarely seen in clinic, it needs to be known to clinicians. At present, submucosal hematoma caused by oral mixture of hirudin and notoginseng powder has not been reported at home and abroad. The patient was a 60-year-old male who had taken 10 capsules of hirudin and notoginseng powder mixture made by himself 2 d ago and developed atypical clinical manifestations such as chest tiredness and heartburn. Endoscopy shows that the hematoma extended from the pharynx to the lower esophagus, and the length was 35-40 cm. Such a long submucosal hematoma is also rare.
- Citation: Liu L, Shen XJ, Xue LJ, Yao SK, Zhu JY. Submucosal hematoma with a wide range of lesions, severe condition and atypical clinical symptoms: A case report. World J Clin Cases 2021; 9(20): 5683-5688
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5683.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5683
Submucosal hematoma (SH) of the digestive tract is an uncommon clinical condition, which can occur spontaneously or be caused by trauma such as during endoscopic surgery[1,2]. Characteristic clinical manifestations of SH comprises dysphagia or odynophagia, acute chest pain, and hematemesis[3]. Typical cases of SH have been reported by several authors[1,2,4]. However, no cases of the SH extending from the hypopharynx to the lower esophagus caused by oral administration of hirudin and panax notoginseng powder have been reported, especially cases with atypical clinical manifestations. We here report such a rare case.
A 60-year-old man was admitted to the Emergency Department of our hospital with chest tightness and heartburn for 2 d.
The patient had taken 10 capsules (containing hirudin and panax notoginseng powder) 2 d prior before and subsequently developed chest tightness and heartburn. Capsules were prepared by the patient himself. It is considered that the oral dose of the capsule was too large. The patient had a short period of shock, and we considered hemorrhagic shock.
The patient had a history of gastritis, hypertension, and coronary heart disease for more than 5 years. The patient's blood pressure was well controlled with oral antihypertensive drugs. Coronary artery stent implantation was performed for coronary heart disease 2 years ago. After coronary stenting, the patient self-administered aspirin and plavix for a relatively short period of time. He is not currently taking any antiplatelet drugs.
He denies any personal and family history.
Physical examination showed tenderness in subxiphoid, blood pressure of 80/42 mmHg (normal range: 90-140/60-90 mmHg), pulse rate of 122/min (normal range: 60-90/min), and respiratory rate of 22/min (normal range: 16-20/min). The patient had two episodes of transient loss of consciousness.
Blood tests revealed abnormal results: A red blood cell count of 1.3 × 1012/L (4.3-5.8 × 1012/L), a platelet count of 12 × 109/L (125-360 × 109/L), a hemoglobin count of 42 g/L (130-175 g/L), and a D-dimer count of 1.65 mg/L (0-0.55 mg/L).
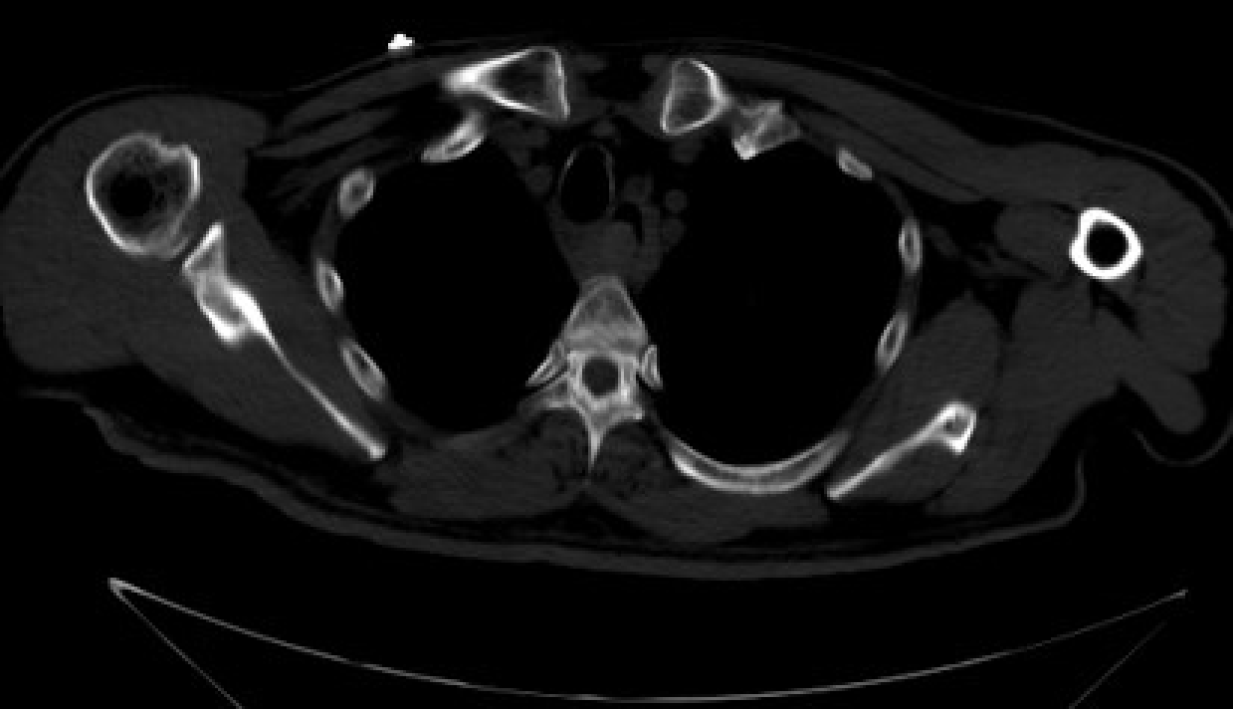
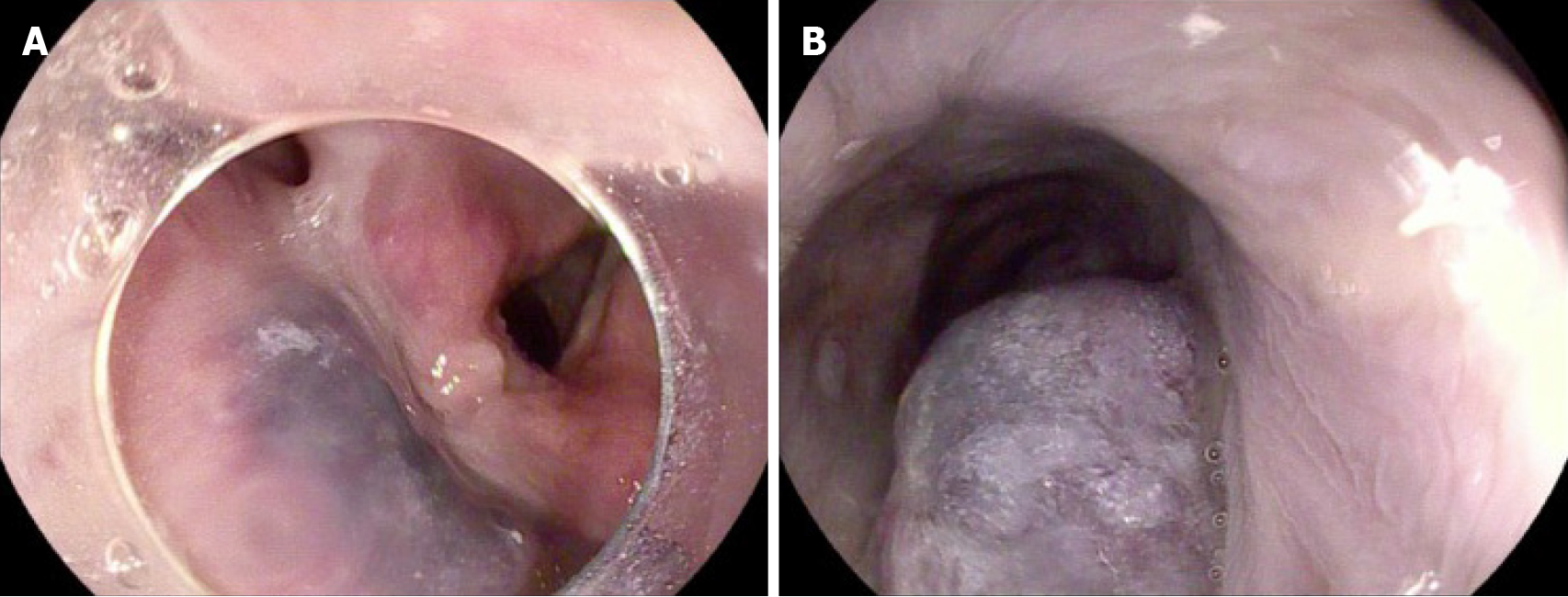
Chest computed tomography (CT) revealed marked narrowing of the entire esophageal lumen (Figure 1). Emergency endoscopy found a large SH extending from the hypopharynx to the lower esophagus. The lesion was a coarse mucosal protuberant lesion parallel to the longitudinal axis of the esophagus, with a length of 35-40 cm (Figure 2A and B).
We considered the patient to be in hemorrhagic shock. Due to excessive blood loss and reduced effective circulating blood volume, the shock type was hypovolemic shock. Based on the CT and emergency endoscopy findings, the final diagnosis was SH extending from the hypopharynx to the lower esophagus.
The patient was successfully managed with conservative therapy. During the period, the patient was given intravenous fluid infusion, intermittent infusion of red blood cells and fibrinogen, intravenous infusion of esomeprazole, oral thrombin, and general conservative treatments.
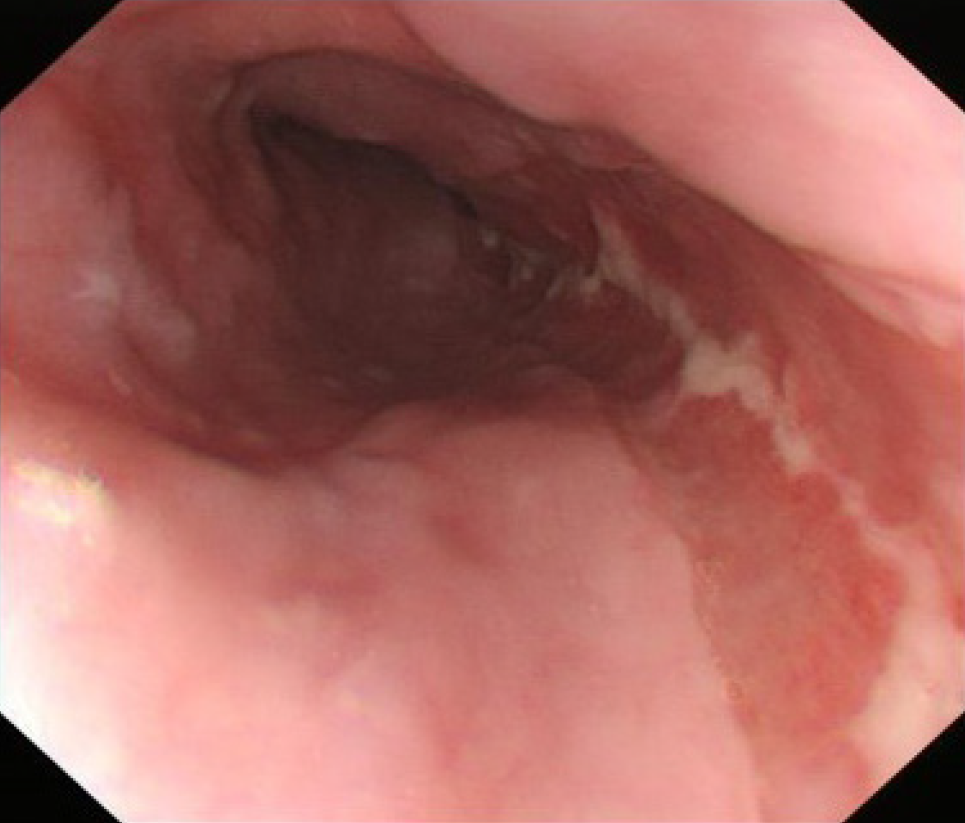
By timely fluid replacement, component blood transfusion, the patient soon regained consciousness, the condition did not continue to deteriorate. After 15 d, the gastroscopy showed the absorption of the submucosal hematoma of the esophagus (Figure 3). The patient's general condition improved well. The patient remained asymptomatic during a 26-mo follow-up.
SH of digestive tract is rare, and it primarily occurs in the esophagus or duodenum[5]. In the present case, SH was found extending from the hypopharynx to the lower esophagus. The patient had no bleeding of the skin and mucosa. To the best of our knowledge, no such cases had been reported in the literature. The patient was informed from someone else that hirudin and notoginseng powder have the therapeutic effect of promoting blood circulation and removing blood stasis, so he took 10 self-made capsules containing hirudin and panax notoginseng powder 2 d prior, which is a unique feature of this case. The hirudin is a direct inhibitor of thrombin and it can affect blood coagulation and promote fibrinolysis in many ways[6]. In addition, the hirudin has a strong efficacy in anti-thrombus and inhibition of platelet aggregation[6]. The effective component of panax notoginseng is the total saponin of panax notoginseng, which can shorten bleeding and clotting time[7]. It also has a pharmacodynamics effect in anti-platelet aggregation and thrombolysis[8]. In this case, the patient had a history of hypertension, coronary heart disease, and coronary stent implantation, we therefore speculate that pathophysiological changes may have occurred in the blood vessels of in many organs of the body. These potential changes together with the use of capsules containing hirudin and panax notoginseng powder eventually resulted in SH. After oral administration of the mixture of hirudin and panax notoginseng capsule, blood coagulation function in the body was impaired, as lowering platelets aggravates tendency of bleeding. At the same time, hirudin can directly act on the body cavity mucosa. According to the CT findings, we initially diagnosed a SH in this patient. The patient had a short period of shock, and we considered hemorrhagic shock. By timely fluid replacement, component blood transfusion, the patient soon regained consciousness, and the condition did not continue to deteriorate. Gastroscopy is the gold standard for defining SH. The patient was in a compositional transfusion, his shock had improved and he was conscious, so we did an emergency gastroscope. Emergency endoscopy confirmed the diagnosis of a SH. The patient's condition improved after 6 d in the intensive care unit, and he was transferred to the general digestive ward for 9 d of conservative treatments.
Clinical manifestations of the patient were not typical, and it was difficult to make a correct diagnosis quickly. The patient's bleeding was in the submucosa and did not enter the gastrointestinal tract, so there was no evidence of hematemesis or bloody stool. Chief complaints of the patient were chest tightness and heartburn, which need to be distinguished from ischemic heart disease, pulmonary embolism, and reflux esophagitis. In this case, the absence of significant abnormalities in troponin T and electrocardiogram results can rule out myocardial infarction. Detailed and accurate acquisition of clinical data of patients, comprehensive physical examination combined with endoscopy, and CT are useful for accurate diagnosis. Risk factors for SH include female sex, hypertension, increased esophageal pressure, coagulopathy, and use of an anticoagulant[2,4]. It has been reported that elderly patients who are taking anticoagulant or antiplatelet medication are at higher risk for SH[4]. This case report has confirmed these findings. The esophageal submucosal hematoma was one of the rare causes of upper gastrointestinal bleeding. As a rare and critical disease in clinic, it should be paid more attention to by the clinicians, especially the doctors in the emergency department, in order to avoid misdiagnosis. The necessary condition for the onset of this disease is the sudden increase of pressure in the esophageal lumen, most of which have clear causes. Esophageal submucosal hematoma generally does not involve the muscular layer, so the treatment is mainly conservative medical treatment. Treatment methods include water fasting, acid suppression, hemostasis, esophagus and gastric mucosa protection, and symptomatic supportive treatment. Hematoma usually absorbs itself within 2 to 3 wk and has a good prognosis.
SH of digestive tract is an uncommon condition. Our case shows that the SH extending from the hypopharynx to the lower esophagus can occur due to ingestion of hirudin and panax notoginseng powder. Conservative therapy is effective, and prognosis is excellent. Clinical symptoms of atypical cases can mimic cardiothoracic emergencies, and ignorance of the disease may cause serious clinical consequences. Physicians should be aware of this rare condition even when clinical symptoms are atypical.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta A S-Editor: Wang JL L-Editor: Filipodia P-Editor: Liu JH
| 1. | Wang Q, Juan YH, Zhong X. Intramural haematoma of the esophagus: multimodality imaging findings and clinical triad. Acta Clin Belg. 2014;69:395-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Sharma K, Wang Y. Submucosal esophageal hematoma precipitated by chronic idiopathic thrombocytopenic purpura. Radiol Case Rep. 2017;12:278-280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Jeong ES, Kim MJ, Yoo SH, Kim DH, Jung JS, Koo NH, Chang SH. Intramural hematoma of the esophagus after endoscopic pinch biopsy. Clin Endosc. 2012;45:417-420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Trip J, Hamer P, Flint R. Intramural oesophageal haematoma-a rare complication of dabigatran. N Z Med J. 2017;130:80-82. [PubMed] |
| 5. | Lee CC, Ravindranathan S, Choksi V, Pudussery Kattalan J, Shankar U, Kaplan S. Intraoperative Gastric Intramural Hematoma: A Rare Complication of Percutaneous Endoscopic Gastrostomy. Am J Case Rep. 2016;17:963-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Zhang J, Lan N. Hirudin variants production by genetic engineered microbial factory. Biotechnol Genet Eng Rev. 2018;34:261-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Zhang S, Chen C, Lu W, Wei L. Phytochemistry, pharmacology, and clinical use of Panax notoginseng flowers buds. Phytother Res. 2018;32:2155-2163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Duan L, Xiong X, Hu J, Liu Y, Li J, Wang J. Panax notoginseng Saponins for Treating Coronary Artery Disease: A Functional and Mechanistic Overview. Front Pharmacol. 2017;8:702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |