Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5631
Peer-review started: February 18, 2021
First decision: April 24, 2021
Revised: May 2, 2021
Accepted: June 1, 2021
Article in press: June 1, 2021
Published online: July 16, 2021
Processing time: 139 Days and 3.8 Hours
Cytomegalovirus (CMV) colitis is usually seen in immunocompromised patients with risk factors such as human immunodeficiency virus infection, solid organ transplant, inflammatory bowel disease, or malignancy. Therefore, many clinicians usually do not consider the possibility of CMV colitis in immunocompetent patients. We reported a rare case of segmental colonic hypoganglionosis associated with CMV colitis in an immunocompetent patient.
A 48-year-old woman with no underlying disease was admitted to our hospital for severe abdominal pain and constipation. Computed tomography of the abdomen showed diffuse dilatation of the small intestine and the entire colon. Initial sigmoidoscopic findings and result of polymerase chain reaction (PCR) for CMV revealed the compatible findings of CMV colitis, the patient was treated with intravenous ganciclovir. After treatment, sigmoidoscopic findings and CMV PCR results improved. However the patient continued to suffered from constipation. Eight months after the initial admission, patient visited the emergency department with severe abdominal pain and imaging revealed aggravation of fecal impaction and bowel dilatation. We performed subtotal colectomy to control patient’s symptom. Histological examination of the resected specimen showed significantly reduced number of mature ganglion cells in the sigmoid colon compared to that in the proximal colon.
Our case demonstrates that CMV colitis can develop even in patients with no other underlying disease, and that CMV colitis can be one of the causes for developing colonic hypoganglionosis.
Core Tip: Cytomegalovirus (CMV) colitis is usually seen in immunocompromised patients such as those with human immunodeficiency virus infection, solid organ transplant, inflammatory bowel disease, or malignancy. In this paper, we report a rare case of CMV colitis induced segmental colonic hypoganglionosis in an immunocompetent patient. This case highlights the importance of clinical suspicion of CMV infection in immunocompetent patients with colonic ulcers and atypical symptoms to ensure its early diagnosis and favorable outcomes.
- Citation: Kim BS, Park SY, Kim DH, Kim NI, Yoon JH, Ju JK, Park CH, Kim HS, Choi SK. Cytomegalovirus colitis induced segmental colonic hypoganglionosis in an immunocompetent patient: A case report. World J Clin Cases 2021; 9(20): 5631-5636
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5631.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5631
Cytomegalovirus (CMV) colitis is a common manifestation of CMV tissue-invasive end-organ disease, usually seen in immunocompromised patients with risk factors such as human immunodeficiency virus infection, solid organ transplant, inflammatory bowel disease, or malignancy[1-4]. Recent studies have reported CMV colitis in immunocompetent patients, but there were risk factors such as old age, blood transfusion, and recent steroid use in most patients. Therefore, many clinicians usually do not consider the possibility of CMV colitis in immunocompetent patients[5].
Hypoganglionosis is characterized by a decreased in the number of ganglion cells in the submucosa and myenteric plexuses of the colon. While hypoganglionosis is usually congenital and occurs at infancy or early childhood, acquired hypoganglionosis (adult-onset form) is extremely uncommon and cause intractable constipation or pseudo-obstruction.
Here, we presented a case of segmental colonic hypoganglionosis associated with CMV colitis in an immunocompetent patient.
Severe abdominal pain and constipation.
A 48-year-old woman with unremarkable medical history other than intermittent constipation, was presented to the emergency department (ED) complaining of severe abdominal pain and absence of spontaneous bowel movements.
The patients had no remarkable history of any underlying disease or prior surgery.
Physical examination revealed abdominal distension with hyperactive bowel sounds and diffuse abdominal tenderness.
Routine laboratory evaluation was normal, including complete blood cell count, urine analysis, biochemical tests and thyroid function test.
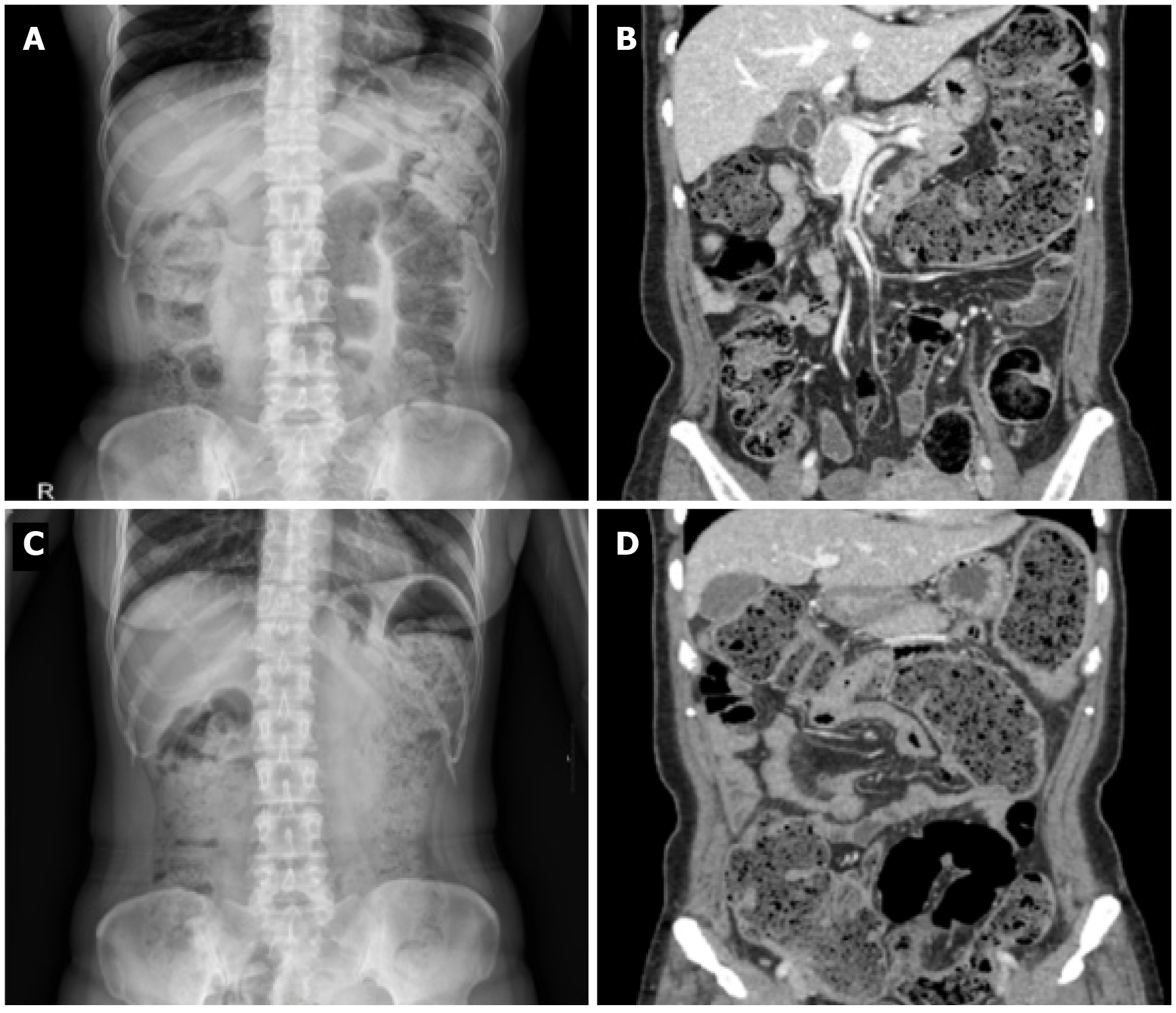
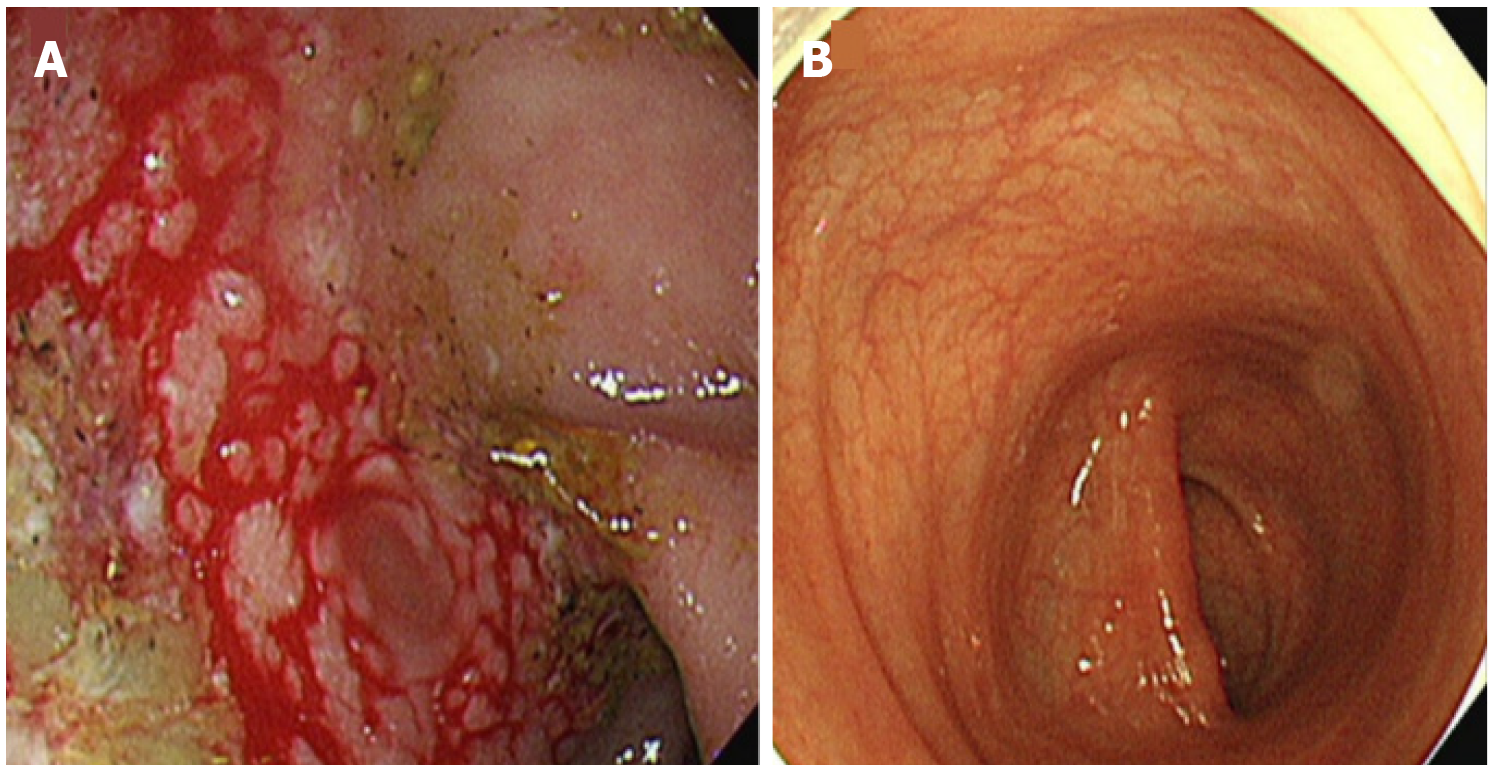
Abdominal X-ray and computed tomography (CT) scan showed diffuse dilation of the small intestine and the entire colon without any definite obstructive lesion (Figure 1A and B). Sigmoidoscopy showed multiple geographic friable ulcerative lesions in the sigmoid colon (Figure 2A).
Pathologic findings showed necro-inflammatory mucosal change with positive CMV immunohistochemical stain. CMV polymerase chain reaction (PCR) for colonic mucosa (1.7 × 105 copies/mL) and blood (4.5 × 102 copied/mL) were also positive.
CMV colitis induced segmental hypoganglionosis.
Based on the Sigmoidoscopic imaging, pathologic findings and positive CMV PCR result, this patient was diagnosed with CMV colitis, despite of the patient had no underlying disease.
Partial improvement of clinical symptoms was achieved with intravenous (IV) ganciclovir (5 mg/kg, every 12 h for 2 wk) and oral laxatives. Follow-up colonoscopy after 3 mo showed improvement of previous ulcerative lesions (Figure 2B) and blood CMV PCR results turned negative, even though the patient was still suffering from constipation.
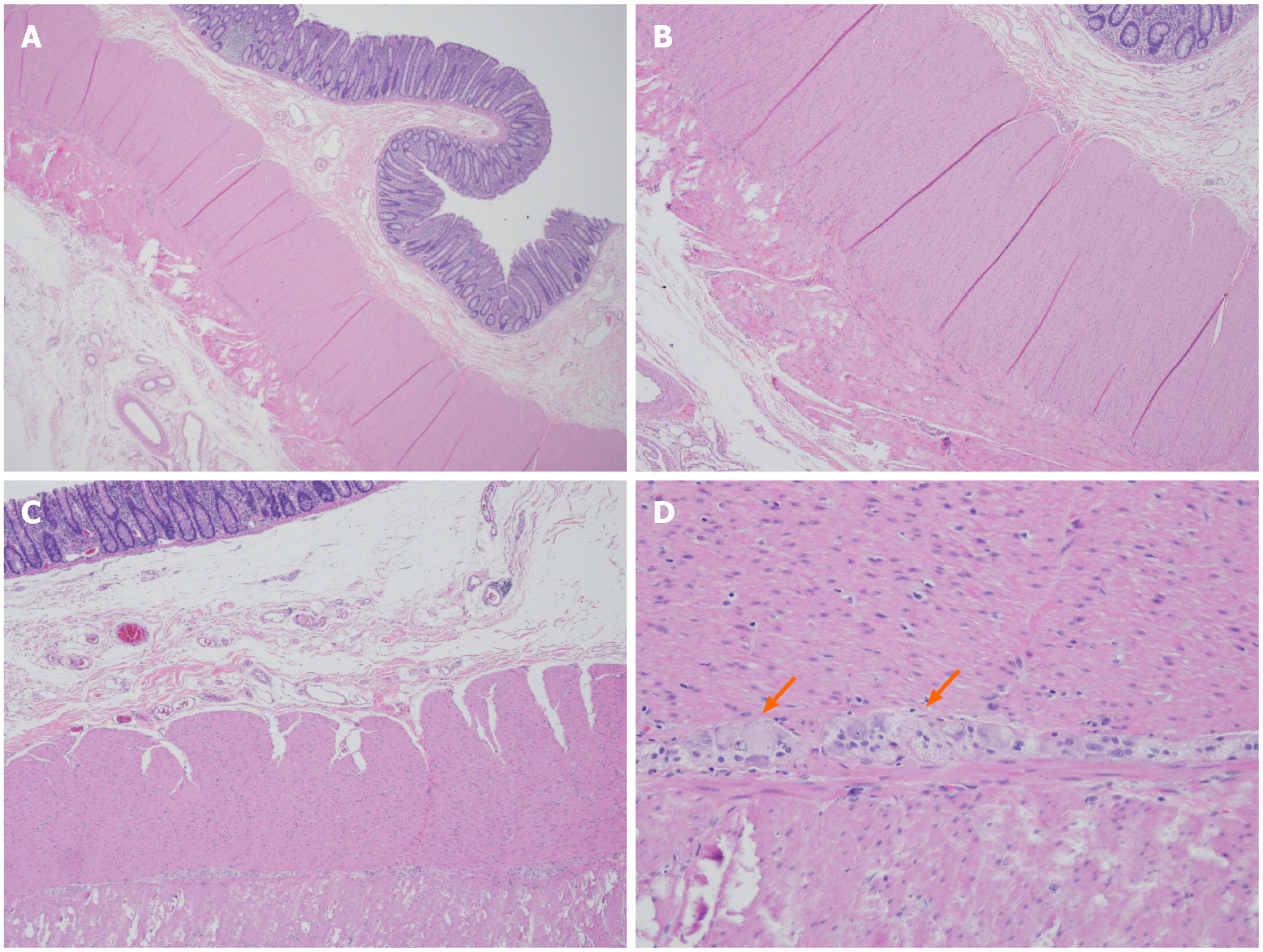
Eight months after initial admission, she visited the ED again due to severe constipation with abdominal pain. CT scan revealed aggravation of fecal impaction and bowel dilatation from the ascending to the descending colon with edematous colonic wall thickening in the sigmoid colon (Figure 1C and D). As she had suffered from recurrent symptoms of colonic pseudo-obstruction, we decided to perform surgery to relieve her symptoms. Histological examination of the resected specimen showed normal feature of mucosa and submucosal vascular congestion. However, the myenteric plexus contained a significantly reduced number of mature ganglion cells in the sigmoid colon compared to that in the proximal colon (Figure 3).
The patient was followed-up for 1 year after operation with improvement in her bowel habits after colectomy.
Even though CMV colitis has been known to occur in immunocompromised hosts[6], recent studies suggested an increasing trend of CMV colitis in immunocompetent patients, especially with risk factors such as old age, renal failure, recent use of steroid or a recent history of blood transfusion[1,2]. However, in the current case, risk factors that may have affected the immune system such as underlying disease or a recent history of using immunosuppressant medication were not present.
Symptoms of CMV colitis are variable and include diarrhea, fever, abdominal pain, hemorrhage, colonic pseudo-obstruction or perforation[3-5].
Even though spontaneous remission without antiviral therapy might occur in immunocompetent patients[6], the treatment of choice for CMV colitis is antiviral therapy with ganciclovir or foscarnet. Previous reports showed no treatment failure in immunocompetent patients diagnosed with CMV colitis who were treated with IV ganciclovir[1]. In this case, the clinical symptoms such as abdominal pain and stool passage partially improved and follow-up colonoscopy revealed resolution of prior colonic mucosal ulcers. However, despite complete healing of mucosal ulceration, histopathological examination of the resected specimen showed a decreased number of ganglion cells in the myenteric plexus, which may suggest irreversible nerve damage of the colonic wall. This finding was in line with those of previous studies, which showed that a viral infection might result in degeneration and loss of ganglion cells in patients with colonic pseudo-obstruction[7-9].
Since the patient had intermittent constipation, the possibility of the exacerbation of preexisting colonic hypoganglionosis caused by CMV colitis cannot be excluded. However, according to previous report, the mean duration of constipation in acquired hypoganglionosis was 7 years, whereas in this case patient, the duration of consti
This case suggested the importance of clinical suspicion of CMV infection in immunocompetent patients presenting with colonic ulcer and atypical symptoms to ensure early diagnosis and favorable outcomes.
We report a rare case of CMV colitis induced segmental hypoganglionosis in immunocompetent patient. This case highlights that CMV colitis can develop even in patients with no other underlying disease, and that CMV colitis can be one of the causes of colonic hypoganglionosis
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jin B S-Editor: Fan JR L-Editor: A P-Editor: Wang LYT
| 1. | Ko JH, Peck KR, Lee WJ, Lee JY, Cho SY, Ha YE, Kang CI, Chung DR, Kim YH, Lee NY, Kim KM, Song JH. Clinical presentation and risk factors for cytomegalovirus colitis in immunocompetent adult patients. Clin Infect Dis. 2015;60:e20-e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Cho JH, Choi JH. Cytomegalovirus ileo-pancolitis presenting as toxic megacolon in an immunocompetent patient: A case report. World J Clin Cases. 2020;8:552-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Yerushalmy-Feler A, Padlipsky J, Cohen S. Diagnosis and Management of CMV Colitis. Curr Infect Dis Rep. 2019;21:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Orloff JJ, Saito R, Lasky S, Dave H. Toxic megacolon in cytomegalovirus colitis. Am J Gastroenterol. 1989;84:794-797. [PubMed] |
| 5. | Shimada Y, Iiai T, Okamoto H, Suda T, Hatakeyama K, Honma T, Ajioka Y. Toxic megacolon associated with cytomegalovirus infection in ulcerative colitis. J Gastroenterol. 2003;38:1107-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Galiatsatos P, Shrier I, Lamoureux E, Szilagyi A. Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts. Dig Dis Sci. 2005;50:609-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Holland-Cunz S, Göppl M, Rauch U, Bär C, Klotz M, Schäfer KH. Acquired intestinal aganglionosis after a lytic infection with varicella-zoster virus. J Pediatr Surg. 2006;41:e29-e31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Taguchi T, Masumoto K, Ieiri S, Nakatsuji T, Akiyoshi J. New classification of hypoganglionosis: congenital and acquired hypoganglionosis. J Pediatr Surg. 2006;41:2046-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Song EM, Kim JW, Lee SH, Chang K, Hwang SW, Park SH, Yang DH, Jung KW, Ye BD, Byeon JS, Yang SK, Lee HJ, Yu CS, Kim CW, Kim J, Myung SJ. Colonic Pseudo-obstruction With Transition Zone: A Peculiar Eastern Severe Dysmotility. J Neurogastroenterol Motil. 2019;25:137-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Do MY, Myung SJ, Park HJ, Chung JW, Kim IW, Lee SM, Yu CS, Lee HK, Lee JK, Park YS, Jang SJ, Kim HJ, Ye BD, Byeon JS, Yang SK, Kim JH. Novel classification and pathogenetic analysis of hypoganglionosis and adult-onset Hirschsprung's disease. Dig Dis Sci. 2011;56:1818-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |