Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5594
Peer-review started: March 1, 2021
First decision: May 11, 2021
Revised: May 19, 2021
Accepted: May 27, 2021
Article in press: May 27, 2021
Published online: July 16, 2021
Processing time: 127 Days and 23.9 Hours
Spinal dural arteriovenous fistula (SDAVF) is an extremely rare vascular malformation of the central nervous system that is often confused with degenerative spinal disorders due to similar early symptoms and clinical features. Here, we report a case of SDAVF recurrence 8 years after lumbar spine surgery and summarize relevant literature.
A 54-year-old male was admitted to our hospital complaining of lower back pain, numbness in both lower extremities and intermittent claudication. Subsequent imaging identified lumbar spinal stenosis. Following surgical treatment, the patient’s symptoms significantly resolved, and he was able to perform daily activities. However, similar symptoms appeared 8 years later, followed by confirmation of SDAVF diagnosis. The patient underwent neurosurgery 7 mo after symptom onset. The follow-up period lasted 14 mo, and the patient remains with marginal neurological symptoms.
This case highlights the importance of prompt SDAVF diagnosis. Due to its nonspecific clinical presentation, the clinical experience of the surgeon and definitive imaging examination are indispensable. Additionally, timely neuro
Core Tip: Spinal dural arteriovenous fistulas (SDAVFs) are rare disorders because its onset and early symptoms resemble more common disorders, especially spinal degeneration disease. It is therefore often misdiagnosed and misclassified, resulting in ineffective clinical interventions, hence poor prognosis. Here, we report a case of SDAVF that went into remission, but symptoms recurred 8 years later as lumbar spinal stenosis, supporting the idea that SDAVF is an acquired disorder. Currently, imaging is an important way of confirming SDAVF diagnosis. Early, effective treatment may significantly improve SDAVF prognosis.
- Citation: Ouyang Y, Qu Y, Dong RP, Kang MY, Yu T, Cheng XL, Zhao JW. Spinal dural arteriovenous fistula 8 years after lumbar discectomy surgery: A case report and review of literature. World J Clin Cases 2021; 9(20): 5594-5604
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5594.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5594
Spinal dural arteriovenous fistula (SDAVF) is a vascular malformation of the spinal cord, and these malformations are broadly classified as extradural AVF, intradural dorsal AVF, intradural ventral AVF, extradural-intradural spinal arteriovenous malformations (AVM), intramedullary AVM and conus medullaris AVM, based on the specific anatomical and pathophysiological factors[1]. Its incidence ranges between 5-10 persons per million[2] and mainly affects middle-aged and elderly males[3].
An anatomically straightforward cause of this disorder is the direct connection between the spinal cord feeding radicular artery and radicular vein[4]. Abnormal retrograde infusion of arterial blood into the venous plexus causes venous congestion and hypertension, resulting in congestive edema and ultimately spinal cord ischemia. This is the main mechanism of spinal cord injury and may lead to irreversible symptoms[5].
Due to its relative rarity, this disease has an insidious onset and is symptomatically similar to many more common disorders, particularly degenerative disorders of the spine, resulting in significant rates of delayed diagnosis and treatment error, leading to poor prognosis[6]. Early SDAVF diagnosis and treatment can significantly improve patient outcomes. Thus, the differential diagnostic ability of clinicians is crucial[5,7]. Here, we report a case of recurrent SDAVF following lumbar spine surgery and summarize recent related advances in SDAVF research.
First admission: Eight years before, the patient complained of experiencing lower back pain for several years and numbness with pain in both lower extremities for 2 years, which gradually worsened over 1 year.
Second admission: Seven months ago, the patient had no obvious triggers to develop low back pain with numbness in both lower extremities.
First admission: The patient was male and did not have an obvious cause of lumbar intermittent pain with pain numbness in both lower extremities and intermittent claudication for about 10 m, which relieved after rest. The patient underwent conservative treatment, and no remission was seen.
Second admission: The patient presented 7 mo ago with low back pain accompanied by pain and fatigue in both lower extremities, intermittent claudication distance of about 50 m, having recently needed a walking stick. The patient had obvious numbness in the saddle area as well as urinary and fecal dysfunction. No significant mitigating or aggravating factors were found during this period.
First admission: He had no significant medical history.
Second admission: The patient underwent lumbar surgery 8 years ago.
There was no consanguineous marriage or family history of significant disease.
First admission: L5 spinous process and paraspinous process had light tenderness. Muscular strength of the four extremities showed no obvious abnormality. Bilateral lower leg lateral, dorsolateral foot and plantar dysesthesia, heavier on the right side. Saddle region hypoesthesia was evident, abdominal wall reflexes and Achilles tendon reflexes were not elicited, bilateral straight leg raise tests were positive, and pathological reflexes were not elicited.
Second admission: The patient had numbness in the sensory planes, bilaterally from below the groin, with strength grade 4 in the iliopsoas, quadriceps, and bilaterally in the tibialis anterior muscles. A grade 3 strength was noted in the extensor hallucis longus and bilaterally in the gastrocnemius muscles. Knee tendon and Achilles tendon reflexes were reduced bilaterally. Straight leg raise tests and pathological reflexes were negative.
The case did not involve laboratory examinations.
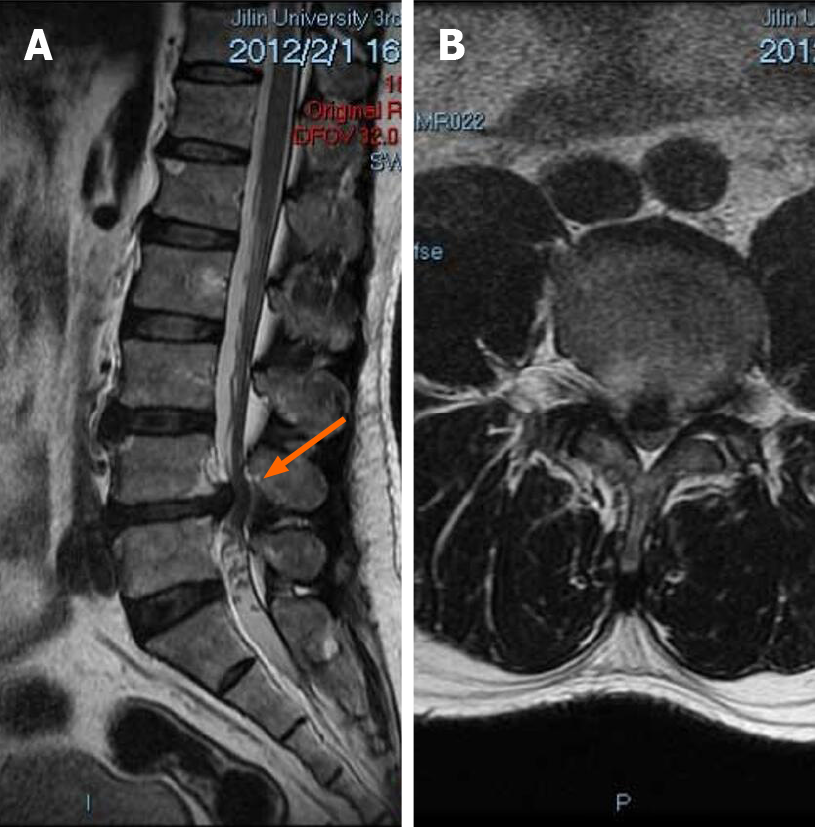
First admission: Using a T2 magnetic resonance imaging (MRI) imaging, the sagittal view of the patient revealed straightening of the physiological curvature of the lumbar spine and a herniated disc at segments L4-L5 (Figure 1A). Axial scanning revealed compression of the dura mater at segments L4-L5 and presence of spinal canal stenosis (Figure 1B).
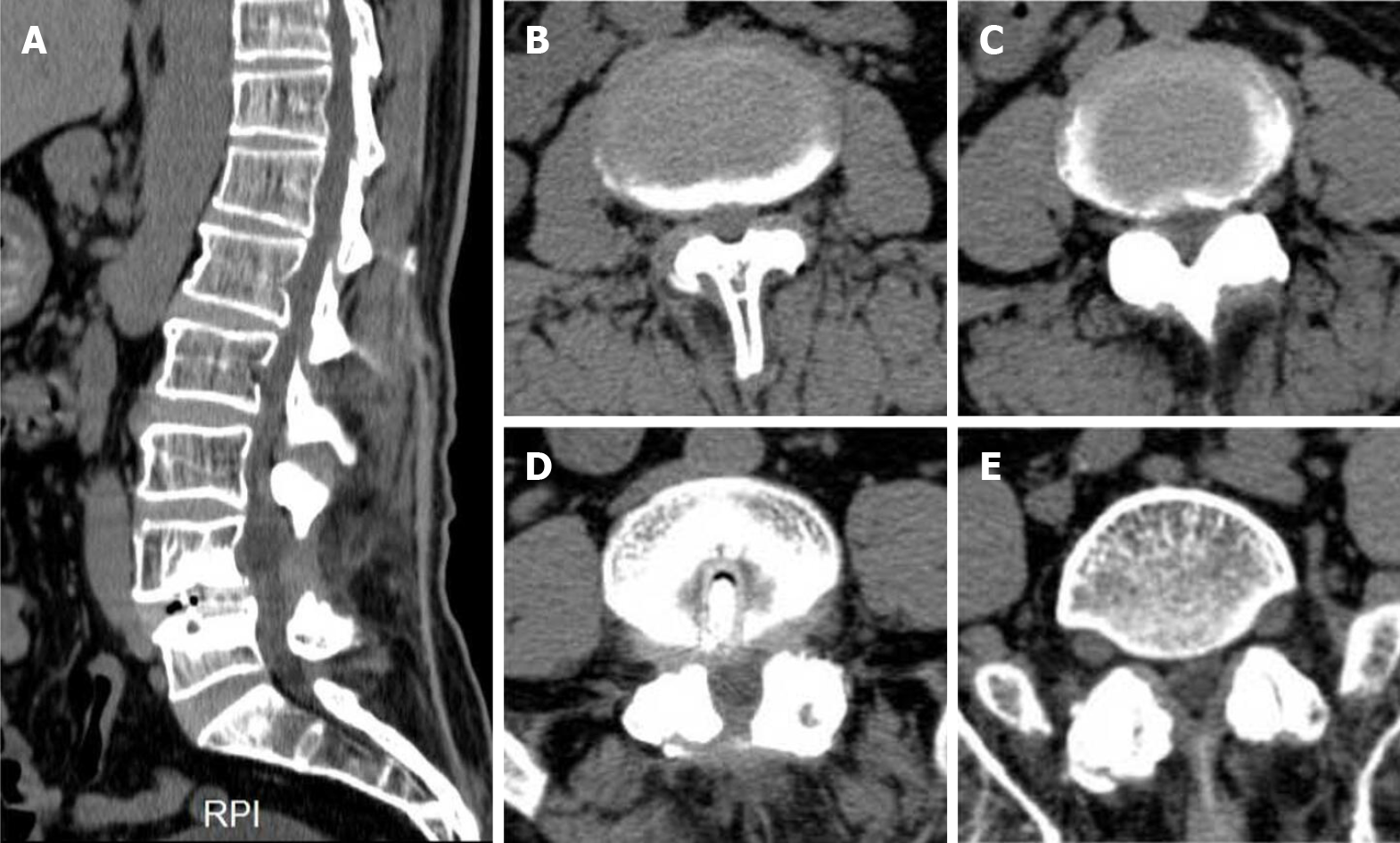
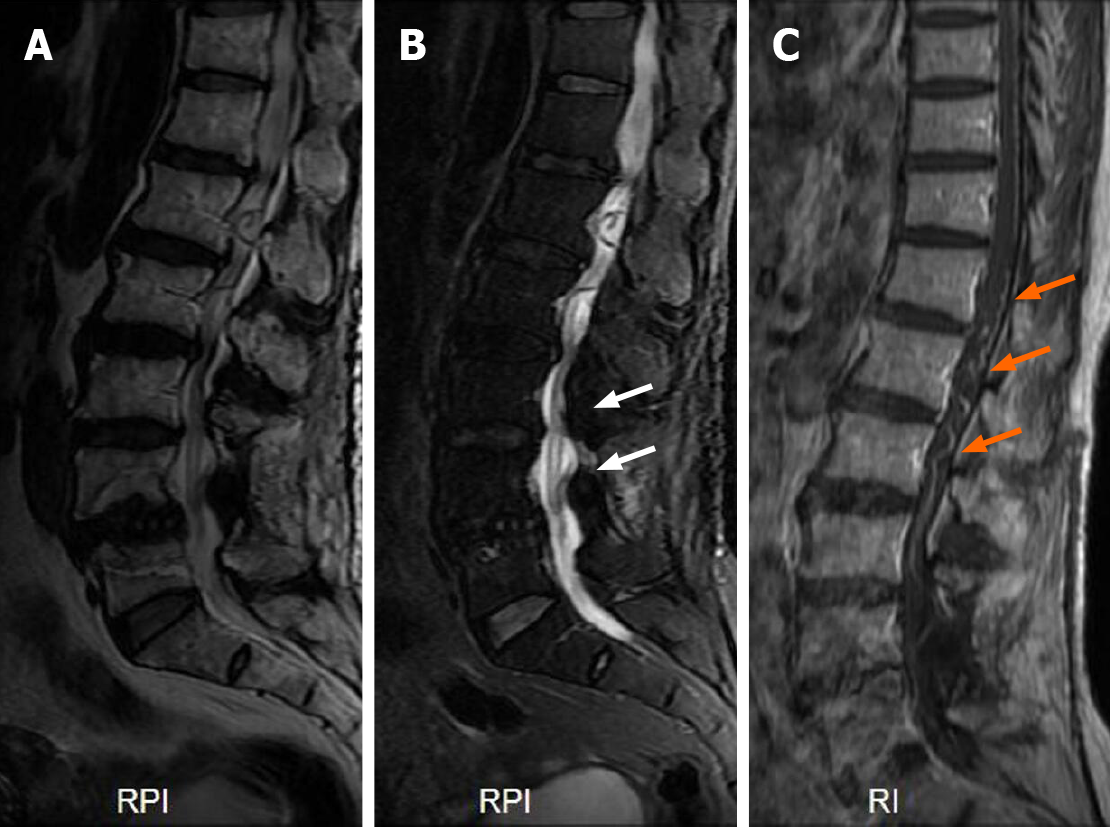
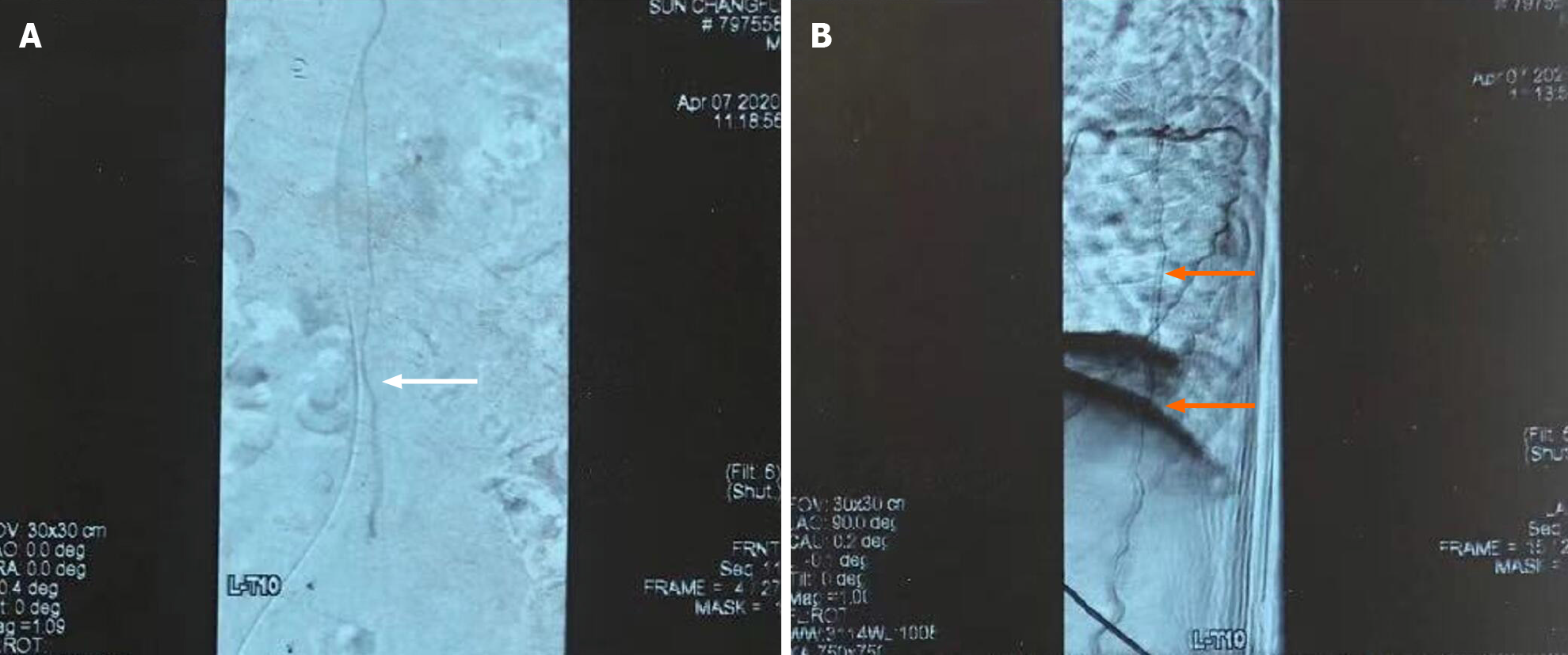
Second admission: Admission computed tomography scan showed that the L4 vertebral body moved forward after lumbar surgery, with lumbar degenerative disease and multiple segment disc herniation (Figure 2). MRI plain scan showed that the changes of the vertebral body were similar to those revealed by computed tomography scan and that there was high signal in the spinal cord on T2 image (Figure 3A and 3B). Contrast-enhanced MRI and spinal angiography revealed abnormal vessels in the dorsal side of the spinal cord (Figures 3C and 4).
Herniated discs at L4-L5 segments; spinal canal stenosis.
SDAVF, L4 spondylolisthesis, L3-L4 disc herniation, Spinal degeneration.
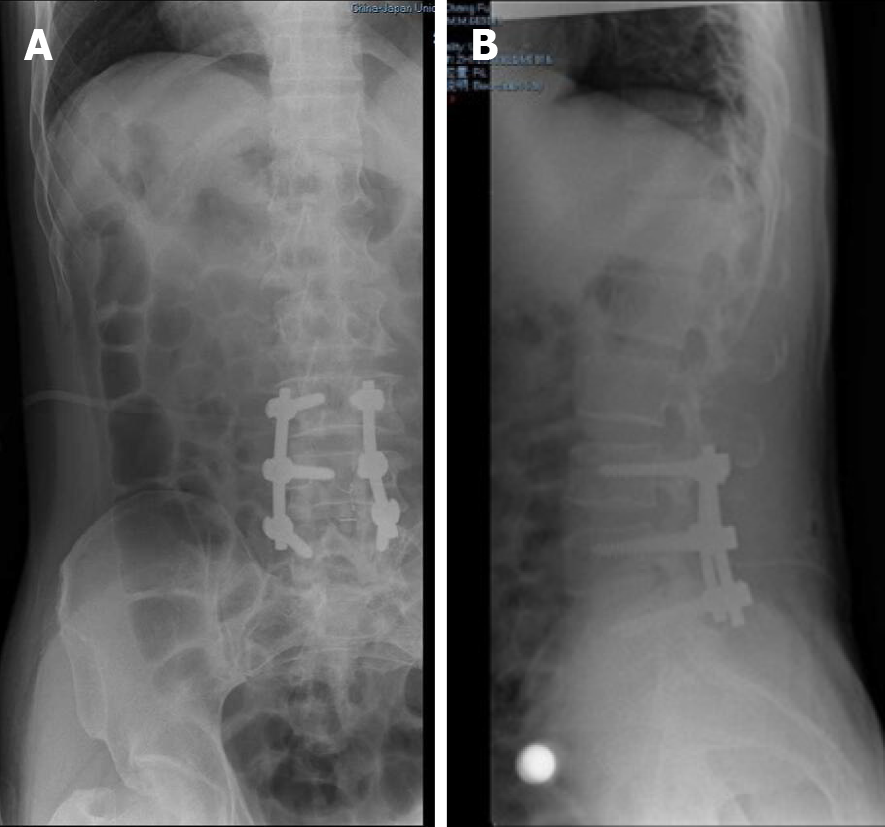
The patient was treated under general anesthesia with lamina decompression, intervertebral disc removal, cage implantation and internal fixation. Postoperative X-ray showed good internal fixation position (Figure 5).
The patient was anesthetized, carefully prone on the operating table, and radiopaque markers were preoperatively administered to facilitate intraoperative positioning. Local anesthetics and epinephrine were injected dermally in the surgical area to reduce bleeding. The skin, superficial fascia and deep fascia were incised stepwise to reveal the lamina. A single laminectomy was performed, and the dura was fully exposed. Intraoperative X-ray reconfirmed the level of surgery. After microscopically incising the dura along the midline while leaving the arachnoid intact and exploring the area of the intravertebral foramen in the subdural space between the dura and the intact arachnoid, the proximal portion of the arterialized vein was seen to emerge from the dura. Thus, temporary aneurysm clips were applied to the arterialized vein, visible as color alterations and bulging of veins distal to the occlusion. The arterialized draining vein was then extracted from the nerve root, coagulated with low-power bipolar and divided. The dura was sutured, and the surgical incision closed layer by layer.
The patient experienced stepwise postoperative pain disappearance in the low back and leg. After half a year, the patient’s saddle region sensation returned to normal, and abdominal wall reflexes and Achilles tendon reflexes returned. The patient experienced hyperesthesia on the lateral calf, dorsolateral foot and plantar foot bilaterally in the first three postoperative weeks, which gradually normalized over the following year. Follow-up continued until the patient removed the internal fixation, about 2 years after surgery, with the patient experiencing significant symptom relief and capable of performing daily activities.
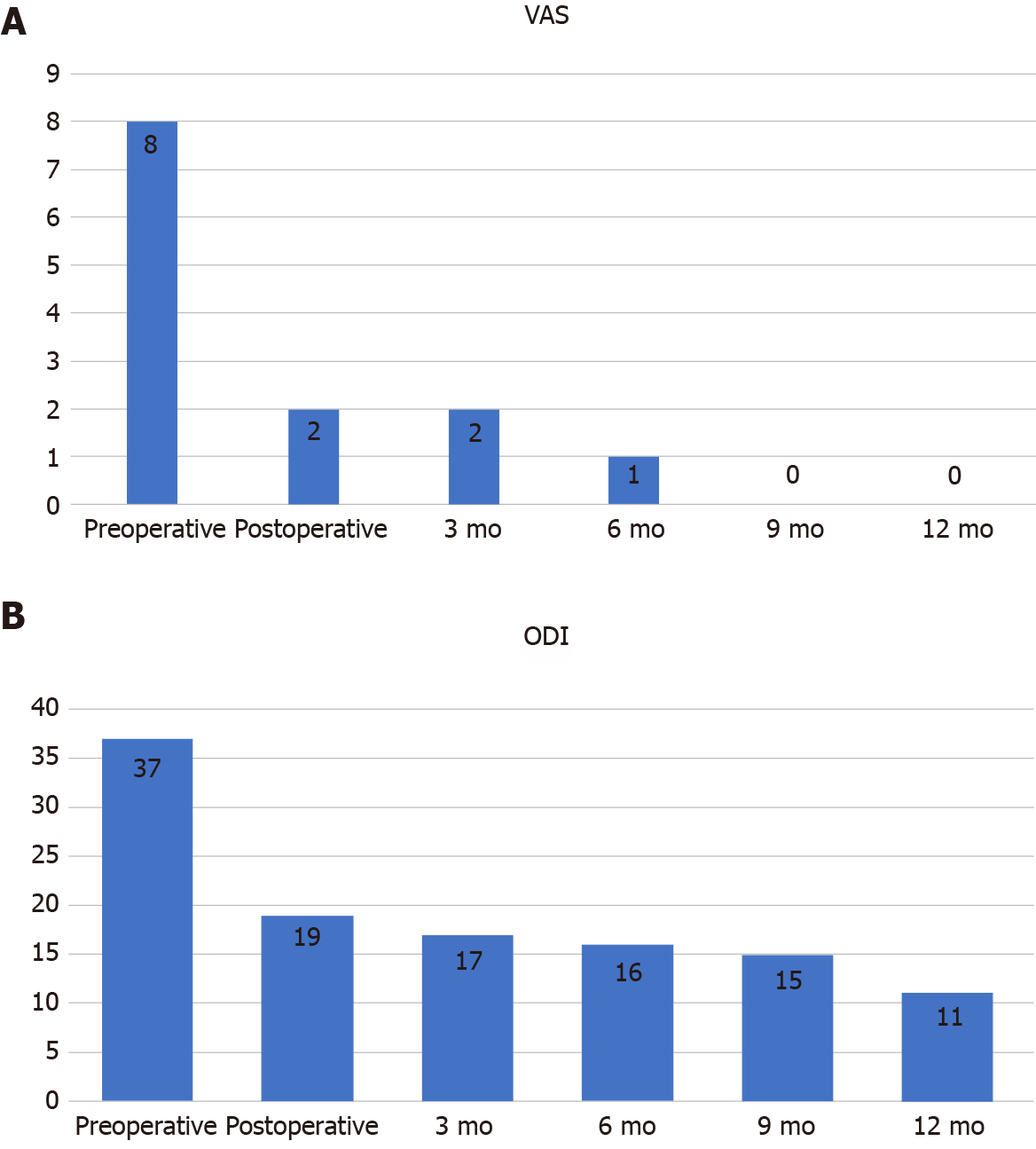
The patient was followed up for 1 year after surgery, during which low back pain as well as numbness and pain in both lower extremities significantly improved, although they still existed. The patient’s lower limb muscle strength recovered significantly, and he tried to walk. Urine and stool function returned to normal. Numbness in the saddle area was not significantly relieved, and the radiation symptoms from the incision to the buttock and saddle area occurred occasionally. According to the Modified Aminoff-Logue scale (Table 1), the patient’s gait improved from grade 3 to 1, while micturition improved from grade 2 to 0. Postoperative changes in visual analogue scale and Oswestry disability index are shown in Figure 6.
| Modified Aminoff-Logue scale | |
| Gait disturbance | Micturition |
| 0 Normal | 0 Normal |
| 1 Leg weakness or abnormal gait; no restricted activity | 1 Hesitance, urgency or frequency |
| 2 Grade 1 with restricted activity | 2 Occasional urinary incontinence or retention |
| 3 Requires cane or similar support for walking | 3 Total urinary incontinence or retention |
| 4 Requires walker or crutches for walking | |
| 5 Unable to stand; confined to bed or wheelchair | |
Here, we report an SDAVF case 8 years after lumbar spinal stenosis surgery. To the best of our knowledge, few cases of SDAVF 8 years after lumbar surgery have been published. Initial SDAVF misdiagnosis rate is 81%, while the erroneous treatment rate is 62% as it exhibits nonspecific clinical manifestation. SDAVF misdiagnosis can lead to selection of the wrong treatment strategy, resulting in neurological dysfunction and even paralysis. Moreover, due to delayed diagnosis, many patients already have severe motor-sensory, sexual and sphincter dysfunction at the time of diagnosis. About 10%-30% of the patients require a wheelchair for ambulatory visits[8,9]. Thus, early and accurate SDAVF diagnosis may significantly improve this disease’s outcome. Here, we described a 54-year-old male who after SDAVF diagnosis, received surgery and had satisfactory clinical outcomes. Moreover, we reviewed SDAVF patients’ features with regards to gender, age, radiology, diagnosis, treatment and prognosis (Table 2).
| Ref. | Age | MRI feature | Symptom | Duration of symptoms | Outcome |
| Derollez et al[27], 2019 | 76 | Hypersignal of the spinal cord from T6 to the terminal cone and flow voids behind the spinal cord | Protopathic hypoesthesia, tactile allodynia, numbness in the soles of his feet and hypopallesthesia in the inferior limbs, especially on the right side | 1 mo | Complete recovery of his motor and sphincterial dysfunctions, the only remaining symptom was paresthesia of his inferior limbs |
| Ren et al[28], 2019 | 61 | T5 to the conus with multiple flow voids posterior to the spinal cord | Motor weakness (grade 4/5) and reduced sensation in both legs | 6 mo | The patient’s symptoms gradually improved |
| Petrin et al[29], 2020 | 87 | Diffuse spinal cord signal change from approximately the T3 to the conus medullaris with vascular patterns at the posterior aspect of the spinal canal | Intermittent loss of sensation in the legs, buckling of his legs with falls and multiple episodes of unexplained new-onset fecal incontinence | 3 mo | The patient made significant functional recovery and return to independent activities of daily living |
| Li et al[30], 2017 | 65 | Dilated tortuous vessels with flow voids extending from C4 to the cauda equina | Decreased muscle strength in both legs (grade 4), hypesthesia occurred below L3 level, defecation difficulty, urinary incontinence and erectile dysfunction | 4 yr | The paresthesia and weakness in both legs and the sphincter dysfunction disappeared completely 1 yr after surgery |
| Gailloud[31], 2018 | 67 | Longitudinally extensive myelopathy with parenchymal enhancement and flow-voids | Progressive lower extremity weakness and pain associated with sphincter dysfunction | Not mentioned | Improvement in his lower extremity pain and was otherwise unchanged |
| Niu et al[32], 2020 | 25 | Multiple tortuous vascular flow voids in the lumbosacral canal from the conus medullaris to the S2 level with prominent edema and swelling of the spinal cord | Intermittent pain of the right lower limb | 1 mo | The patient’s symptoms were completely relieved |
| Prieto et al[33], 2009 | 56 | Total spine showed diffuse intramedullary hyperintensity with peripheral sparing between T8 and the conus medullaris, prominent perimedullary flow voids on the dorsal aspect of the cord | Lower extremity weakness and ascending numbness from his toes to his groin, urinary retention | 9 mo | The patient’s lower extremity muscle strength was normal, and the deep tendon reflexes were bilaterally hyper-reflexic in both legs |
Regarding SDAVF demographic features, it is reported that the time interval from symptom appearance to diagnosis varies from a few days to many years[10], with a mean duration of 12 mo[11]. Many factors, like atypical clinical symptoms, variable course and misleading imaging results[2], contribute to delay or miss SDAVF diagnosis. Here, the duration from disease onset to accurate diagnosis was 7 mo, which was shorter than the mean time in previous studies[11], which is a critical reason for his good prognosis. A retrospective review found that the disease mainly occurs in middle-aged and elderly men and has a chronic progression of symptoms limited to the lower limbs, which are aggravated by activity[12]. In this case the patient was aged 54 at SDAVF diagnosis, which was consistent with previous findings[12].
In various studies, the description of diseases that are easily confused with SDAVF is not identical. However, the main diseases are degenerative spinal disease, myelitis, prostate disease and intramedullary tumor[13]. To differentiate SDAVF from polyneuropathy, the following key points should be considered at clinical presentation: Involvement of the upper limbs (SDAVF is rare), sensory involvement of the sacrum (polyneuropathy is very rare) and upper neuronal signs (polyneuropathy is rare)[14]. Here, the patient had a history of lumber surgery for lumbar disc herniation 8 years before. Recently, the patient experienced a low back radiating pain to both lower extremities, an intermittent claudication distance of about 50 m, numbness in the saddle area and urinary and fecal dysfunction. MRI revealed L3-4 lumbar disc herniation, improving the accuracy of SDAVF diagnosis. However, we found that physical examination is not fully consistent with clinical presentation. Initially, we suspected that he had an intraspinal tumor in the thoracic or lumbar spine, but interestingly enhanced MRI revealed SDAVF. Thus, careful neurological examination is essential to excluding SDAVF.
In clinical practice, many patients undergo unnecessary examinations or treatments, including prostate surgery or biopsy, discectomy and laminectomy or fusion before correct diagnosis is reached[14]. These measures are not only unnecessarily distressful to the patient but also delay optimal treatment[15]. This problem is compounded by factors like a patient’s older age, degenerative spine disease comorbidities, prostatic or vascular insufficiency and the lack of awareness of SDAVF by clinicians[16]. In this case, the patient had mixed symptoms of nerve root compression due to L3-L4 disc herniation and spinal cord compression due to SDAVF. He therefore underwent L3-L4 disc removal and electrocoagulation of the spinal artery. With the rapid development of endovascular techniques, more and more medical centers tend to use endovascular embolization techniques for the treatment of SDAVF[17].But a multicenter study found that only 0.69% of patients in the neurosurgical treatment group had treatment failure and no patients had recurrence, whereas 20% of patients in the endovascular treatment group had treatment failure and 16% had recurrence[13]. Another systematic review also confirmed that the surgical treatment group was superior to the endovascular treatment group in the degree of postoperative neurological recovery, treatment success and recurrence rates[18]. Therefore, our choice of surgical treatment may also be one of the factors for the better prognosis of the patient. In our opinion, the good clinical outcome of this patient was due to early diagnosis upon admission and the choice of an appropriate surgical plan.
SDAVF pathogenesis is unclear. Some studies suggest it is caused by reopening of thrombosed radicular veins[14]. Radicular vein occlusion/thrombosis has also been identified as part of the disease[19]. Unlike AVM, which is often regarded as congenital, SDAVF is common in middle-aged and elderly men. Thus, some studies suggest it is an acquired disorder[20]. Consistent with past studies, due to the long remission after the first operation, the etiology of the second operation may be closely related to reopening of the radicular vein.
With regards to clinical symptoms, unlike poly (radicular) neuropathy, the distribution of its sensory or motor deficits is often asymmetric. Myelitis may be related to “congestive” veins in MRI examination, which can simulate the findings in SDAVF. However, bladder incontinence and dysuria are common in SDAVF and enlarged prostates.
With regards to SDAVF radiological features, it is mainly diagnosed using MRI, which shows: (1) the presence of abnormal vessels or vascular flow voids; (2) increased T2 signal within the spinal cord; and (3) spinal cord dilatation[10]. In terms of hyperintensity on T2 images within the spinal cord, in contrast to anterior spinal artery infarcts, myelitis, and spinal cord tumors, spinal cord edema due to spinal vascular malformations is usually homogeneous, with tapering margins extending to 5-7 vertebrae[21]. Severe spinal stenosis can also demonstrate venous congestion and tortuosity but usually spans only 1-2 vertebral bodies, with a cluster of redundant nerves and blood vessels seen at the stenosis on magnetic resonance myelography. The presence of cord edema or serpentine flow voids on the dorsal surface of the spinal cord on T2 images may minimize confusion with SDAVF[22].
Here, MRI showed hyperintense shadowing of multiple segments of the spinal cord in T2 weighted images. Enhanced MRI revealed tortuously dilated vascular shadow of the dorsal spinal cord, which is consistent with past studies[22]. Here, computed tomography with MRI only revealed spinal degenerative lesions. However, image findings did not correspond to the patient’s severe clinical symptoms. Subsequently, contrast-enhanced MRI confirmation was performed. Moreover, spinal angiography, the gold standard for SDAVF diagnosis, was done preoperatively on this patient. Spinal angiography can determine the location of fistula and the state of the supplying artery and draining vein. Additionally, it can determine the presence of multiple fistulas and guide surgical or interventional treatment[23]. Although the development of MRI imaging techniques, especially the advent of contrast-enhanced, time resolved MR angiography, has improved the accurate rate of diagnosing SDAVFs, these imaging techniques still suffer from a missed diagnosis rate of approximately 10.5%[24]. Considering the severe adverse prognosis after underdiagnosis, spinal angiography should be recommended for all suspected patients. Finally, the patient was diagnosed with SDAVF.
Although this study has achieved a good clinical effect, there are still many limitations. First, the case number in this study was relatively small. Thus, a multicenter large-sample study is needed to summarize the radiological imaging features of SDAVF. Secondly, although the patient was diagnosed and operated successfully after hospitalization, he had slight residual low back pain, leg pain and numbness in the saddle after the operation, probably due to the late treatment. For patients with delayed diagnosis, about 60% of patients show improvement in movement disorders after treatment, but only about 30% of patients show im
Although SDAVF pathogenesis is ill-defined, it is considered an acquired condition. Because SDAVF symptoms are not specific, imaging findings are critical for its diagnosis. This case and past studies have shown that surgery is an effective treatment and that early, effective treatment significantly improves prognosis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sarica FB S-Editor: Gao CC L-Editor: Filipodia P-Editor: Liu JH
| 1. | Kim LJ, Spetzler RF. Classification and surgical management of spinal arteriovenous lesions: arteriovenous fistulae and arteriovenous malformations. Neurosurgery. 2006;59:S195-201; discussion S3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 88] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Krings T, Geibprasert S. Spinal dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2009;30:639-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 285] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 3. | Maimon S, Luckman Y, Strauss I. Spinal Dural Arteriovenous Fistula: A Review. Adv Tech Stand Neurosurg. 2016;111-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Chibbaro S, Gory B, Marsella M, Tigan L, Herbrecht A, Orabi M, Bresson D, Baumann F, Saint-Maurice JP, George B, Kehrli P, Houdart E, Manisor M, Pop R. Surgical management of spinal dural arteriovenous fistulas. J Clin Neurosci. 2015;22:180-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Wojciechowski J, Kunert P, Nowak A, Dziedzic T, Czernicki T, Wójtowicz K, Leśniewski K, Marchel A. Surgical treatment for spinal dural arteriovenous fistulas: Outcome, complications and prognostic factors. Neurol Neurochir Pol. 2017;51:446-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Jellema K, Tijssen CC, Sluzewski M, van Asbeck FW, Koudstaal PJ, van Gijn J. Spinal dural arteriovenous fistulas--an underdiagnosed disease. A review of patients admitted to the spinal unit of a rehabilitation center. J Neurol. 2006;253:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ronald AA, Yao B, Winkelman RD, Piraino D, Masaryk TJ, Krishnaney AA. Spinal Dural Arteriovenous Fistula: Diagnosis, Outcomes, and Prognostic Factors. World Neurosurg. 2020;144:e306-e315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Jellema K, Canta LR, Tijssen CC, van Rooij WJ, Koudstaal PJ, van Gijn J. Spinal dural arteriovenous fistulas: clinical features in 80 patients. J Neurol Neurosurg Psychiatry. 2003;74:1438-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 130] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 9. | Donghai W, Ning Y, Peng Z, Shuo X, Xueen L, Bin H, Xingang L. The diagnosis of spinal dural arteriovenous fistulas. Spine (Phila Pa 1976). 2013;38:E546-E553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Hunt R, Roberts RM, Mortimer AM. Spinal dural arteriovenous fistula: delay to radiological diagnosis and sources of radiological error. Clin Radiol 2018; 73: 835.e11-835. e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Narvid J, Hetts SW, Larsen D, Neuhaus J, Singh TP, McSwain H, Lawton MT, Dowd CF, Higashida RT, Halbach VV. Spinal dural arteriovenous fistulae: clinical features and long-term results. Neurosurgery. 2008;62:159-66; discussion 166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 12. | Murphy OC, Hedjoudje A, Salazar-Camelo A, Pardo CA, Gailloud P. Clinical characteristics, misdiagnosis and outcomes of patients with low-flow spinal arteriovenous fistulas. J Neurol Sci. 2020;413:116863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Takai K, Endo T, Yasuhara T, Seki T, Watanabe K, Tanaka Y, Kurokawa R, Kanaya H, Honda F, Itabashi T, Ishikawa O, Murata H, Tanaka T, Nishimura Y, Eguchi K, Takami T, Watanabe Y, Nishida T, Hiramatsu M, Ohtonari T, Yamaguchi S, Mitsuhara T, Matsui S, Uchikado H, Hattori G, Yamahata H, Taniguchi M. Neurosurgical vs endovascular treatment of spinal dural arteriovenous fistulas: a multicenter study of 195 patients. J Neurosurg Spine. 2020;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Jellema K, Tijssen CC, van Gijn J. Spinal dural arteriovenous fistulas: a congestive myelopathy that initially mimics a peripheral nerve disorder. Brain. 2006;129:3150-3164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 199] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 15. | Medel R, Crowley RW, Dumont AS. Endovascular management of spinal vascular malformations: history and literature review. Neurosurg Focus. 2009;26:E7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Saladino A, Atkinson JL, Rabinstein AA, Piepgras DG, Marsh WR, Krauss WE, Kaufmann TJ, Lanzino G. Surgical treatment of spinal dural arteriovenous fistulae: a consecutive series of 154 patients. Neurosurgery. 2010;67:1350-1357; discussion 1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Lad SP, Santarelli JG, Patil CG, Steinberg GK, Boakye M. National trends in spinal arteriovenous malformations. Neurosurg Focus. 2009;26:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Goyal A, Cesare J, Lu VM, Alvi MA, Kerezoudis P, Brinjikji W, Nasr D, Lanzino G, Bydon M. Outcomes following surgical vs endovascular treatment of spinal dural arteriovenous fistula: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2019;90:1139-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 19. | Merland JJ, Riche MC, Chiras J. Intraspinal extramedullary arteriovenous fistulae draining into the medullary veins. J Neuroradiol. 1980;7:271-320. [PubMed] |
| 20. | Koch C. Spinal dural arteriovenous fistula. Curr Opin Neurol. 2006;19:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Hurst RW, Grossman RI. Peripheral spinal cord hypointensity on T2-weighted MR images: a reliable imaging sign of venous hypertensive myelopathy. AJNR Am J Neuroradiol. 2000;21:781-786. [PubMed] |
| 22. | Jeng Y, Chen DY, Hsu HL, Huang YL, Chen CJ, Tseng YC. Spinal Dural Arteriovenous Fistula: Imaging Features and Its Mimics. Korean J Radiol. 2015;16:1119-1131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 23. | Kralik SF, Murph D, Mehta P, O'Neill DP. Diagnosis of spinal dural arteriovenous fistula using 3D T2-weighted imaging. Neuroradiology. 2017;59:997-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Grossberg JA, Howard BM, Saindane AM. The use of contrast-enhanced, time-resolved magnetic resonance angiography in cerebrovascular pathology. Neurosurg Focus. 2019;47:E3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 25. | Jablawi F, Schubert GA, Dafotakis M, Pons-Kühnemann J, Hans FJ, Mull M. Long-Term Outcome of Patients with Spinal Dural Arteriovenous Fistula: The Dilemma of Delayed Diagnosis. AJNR Am J Neuroradiol. 2020;41:357-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Jellema K, Sluzewski M, van Rooij WJ, Tijssen CC, Beute GN. Embolization of spinal dural arteriovenous fistulas: importance of occlusion of the draining vein. J Neurosurg Spine. 2005;2:580-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Derollez C, Tard C, Kazémi A, Vermersch P, Pruvo JP. A Rare and Treatable Cause of Medullar Claudication: Spinal Dural Arteriovenous Fistula. Ochsner J. 2019;19:397-400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Ren Y, Liu H, Chen TY, Li J. True metachronous multiple spinal dural arteriovenous fistulas: case report and review of the literature. Br J Neurosurg. 2019;1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Petrin Z, Marino RJ, Oleson CV, Simon JI, McCormick ZL. Paralysis After Lumbar Interlaminar Epidural Steroid Injection in the Absence of Hematoma: A Case of Congestive Myelopathy Due to Spinal Dural Arteriovenous Fistula and a Review of the Literature. Am J Phys Med Rehabil. 2020;99:e107-e110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Li J, Li G, Bian L, Hong T, Yu J, Zhang H, Ling F. Concomitant Lumbosacral Perimedullary Arteriovenous Fistula and Spinal Dural Arteriovenous Fistula. World Neurosurg 2017; 105: 1041.e7-1041. e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Gailloud P. Spinal dural arteriovenous fistula (SDAVF) variant with dual perimedullary and epidural drainage. Eur Spine J. 2018;27:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Niu X, Ren Y, Li J. Concomitant Sacral Dural Arteriovenous Fistula and Conus Medullaris Arteriovenous Malformation with Respective Drainage Veins: Case Report and Literature Review. World Neurosurg. 2020;141:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Prieto R, Pascual JM, Gutiérrez R, Santos E. Recovery from paraplegia after the treatment of spinal dural arteriovenous fistula: case report and review of the literature. Acta Neurochir (Wien). 2009;151:1385-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |