Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5479
Peer-review started: March 16, 2021
First decision: May 1, 2021
Revised: May 7, 2021
Accepted: May 19, 2021
Article in press: May 19, 2021
Published online: July 16, 2021
Processing time: 113 Days and 3.3 Hours
Hypoxemia is a common complication in obese patients during gastroscopy with sedation. The Wei nasal jet tube (WNJT) is a new special nasopharyngeal airway with the ability to provide supraglottic jet ventilation and oxygen insufflation via its built-in wall channels. The aim of this study was to compare the efficacy and safety of the WNJT vs a nasal cannula for supplemental oxygen during gastro
To compare the efficacy and safety of the WNJT vs a nasal cannula for supplemental oxygen during gastroscopy with propofol mono-sedation in obese patients.
A total of 103 obese patients with a body mass index of 30 kg/m2 or more undergoing elective gastroscopy under propofol mono-sedation were randomly assigned to receive supplemental oxygen at 5 L/min through either a WNJT (WNJT group, n = 51) or a nasal cannula (nasal cannula group, n = 52). The lowest pulse oxygen saturation (SpO2) and mild and severe hypoxemia during gastro
The lowest SpO2 during gastroscopy with propofol mono-sedation was significantly increased in the WNJT group compared with the nasal cannula group. The incidence of mild hypoxemia and total incidence of hypoxemia were significantly lower in the WNJT group than in the nasal cannula group. Other than a higher incidence of epistaxis in the WNJT group, the occurrence of adverse events was similar between the devices. While neither device demonstrated a statistically significant difference in satisfaction among patients, the WNJT did result in improved satisfaction among anesthetists and physicians.
During gastroscopy with propofol mono-sedation in obese patients, the WNJT, when compared with a nasal cannula for supplemental oxygen, can significantly reduce the occurrence of hypoxemia and improve both arterial oxygenation and satisfaction among anesthetists and physicians. The use of the WNJT may, however, lead to epistaxis in a few patients. In view of this clinically acceptable risk-benefit ratio, the WNJT may be recommended as an alternative tool for supplemental oxygen for the prevention of hypoxemia during gastroscopy with propofol mono-sedation in obese patients.
Core Tip: This study is a prospective, randomized controlled trial aimed to compare the efficacy and safety of Wei nasal jet tube (WNJT) and nasal prongs for supplemental oxygen during gastroscopy with propofol monosedation in obese patients when a moderate oxygen flow is used. Our results show that the WNJT compared with the nasal prongs for supplemental oxygen is more effective for prevention of hypoxemia during gastroscopy with propofol mono-sedation, though it may result in a potential risk of epistaxis in few patients.
-
Citation: Shao LJZ, Hong FX, Liu FK, Wan L, Xue FS. Prospective, randomized comparison of two supplemental oxygen methods during gastro
scopy with propofol mono-sedation in obese patients. World J Clin Cases 2021; 9(20): 5479-5489 - URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5479.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5479
The use of sedation can relieve patients’ discomfort during upper gastrointestinal (UGI) endoscopy and improve patient satisfaction and the efficiency of endoscopic procedures[1]; however, hypoxemia by respiratory inhibition and airway obstruction during UGI endoscopy with sedation is a major concern[2]. The available evidence indicates that supplemental oxygen can reduce the incidence of hypoxemia during UGI endoscopy with sedation[1,3]. A nasal cannula is a convenient tool to administer supplemental oxygen, although it may be inadequate for patients at increased risk of respiratory inhibition and airway obstruction, such as patients with obesity, sleep apnea syndrome, or cardiopulmonary insufficiency[2,4]. For these patients, the placement of a nasopharyngeal airway to administer supplemental oxygen may be a good solution, as it can ensure an open airway and does not interfere with endoscopic procedures.
The Wei nasal jet tube (WNJT, Well Lead Medical Co. Ltd., Guangzhou, China) is a new special nasopharyngeal airway made of soft material with many functions, such as airway opening, supraglottic jet oxygenation and ventilation, and carbon dioxide monitoring[5]. Our previous work in patients with a normal body mass index (BMI) showed that the WNJT, when compared with a nasal cannula for supplemental oxygen at 5 L/min, was more effective at preventing hypoxemia during gastroscopy with propofol mono-sedation[6]. For obese patients at increased risk of hypoxemia during UGI endoscopy with sedation, however, it remains unclear whether the WNJT is an effective and safe tool for administering supplemental oxygen. Thus, this single-center, prospective, randomized controlled trial (RCT) was designed to compare the efficacy and safety of the WNJT vs a nasal cannula for supplemental oxygen during gastro
This study was approved by the Ethics Committee of Beijing Friendship Hospital, China (Ethics Committee number: 2017-P2-009-02). The trial protocol has been registered with the Chinese Clinical Trial Registry (registration number: ChiCTR-IOR-17013089) and published[7]. This prospective RCT was conducted in the Endoscopy Center of Beijing Friendship Hospital, Capital Medical University.
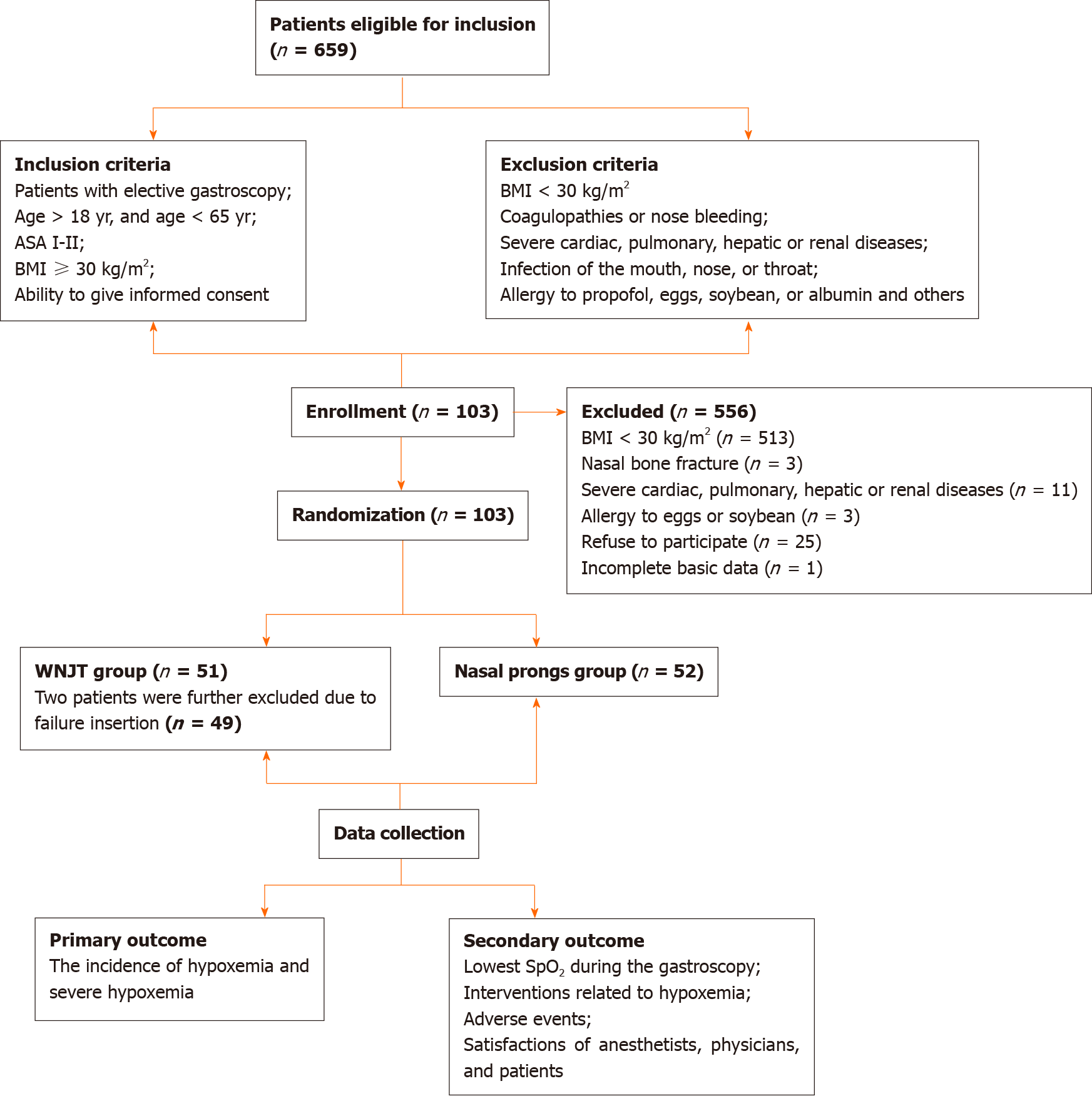
Adult patients scheduled for gastroscopy with propofol mono-sedation between November 2017 and December 2018 were recruited. The inclusion criteria were male or female obese patients; ages 18 to 65 years; a BMI of 30 kg/m2 or more; American Society of Anesthesiologists (ASA) physical status classifications 1-2; and the ability to give informed consent. The exclusion criteria included patients with a BMI of less than 30 kg/m2; a history of coagulopathy or nose bleeding; severe cardiac, pulmonary, hepatic or renal disease; an infection of the mouth, nose, or throat; or an allergy to propofol, eggs, soybean, or albumin.
All included patients provided written informed consent. Based on a random number table generated by a computer, patients were randomly assigned to the WNJT or nasal cannula group. After patients entered the examination room, topical anesthesia of the upper airway was administered by gargling a 2% lidocaine gel, and routine monitoring, including blood pressure, heart rate, and pulse oxygen saturation (SpO2) was performed.
Patients were placed in the lateral position and were asked to take deep breaths with 100% oxygen for pre-oxygenation until an end-tidal oxygen concentration of 88%-90% was reached. Then, sedation was induced with slow intravenous injection of propofol. The sedation depth was evaluated according to the modified Observer’s Assessment of Alertness/Sedation (MOAA/S) score[8]. According to our routine practice, deep sedation with a MOAA/S score of 1 was first obtained to ensure successful insertion of the gastroscope tube and decrease adverse responses to the insertion of the gastroscope tube into the upper airway. During gastroscopy, moderate sedation with a MOAA/S score of 2 or 3 was maintained with additional propofol of 20-30 mg as necessary.
Before sedation, two sprays of ephedrine were applied to each nostril for all patients. The selected naris for the placement of the WNJT was the naris that the patient reported to be more patent. After adequate depth of sedation was obtained and before gastroscopy was initiated, either a WNJT or a nasal cannula was placed for supplemental oxygen. After inserting the WNJT, its position in the upper airway was re-examined by gastroscopy and adjusted as appropriate, if necessary. If the insertion of the WNJT was difficult via the selected nasal passage, insertion in the contralateral side was attempted. If still unsuccessful after three attempts, the insertion of the WNJT was deemed a failure. During gastroscopy, 5 L/min oxygen was continuously delivered through the built-in channel of the WNJT and nasal cannula in the two groups. After gastroscopy, both the WNJT and nasal cannula were removed before full recovery from sedation.
The lowest SpO2 during gastroscopy was noted. Throughout gastroscopy, if hypoxemia (SpO2 < 90%) occurred, treatment measures included (1) no additional drug; (2) audio or painful stimulation; (3) an increase in the oxygen flow from 5 to 8 L/min; (4) airway opening with the jaw thrust maneuver; (5) the removal of the gastroscope tube and the use of facemask ventilation; or (6) endotracheal intubation for artificial ventilation if the above measures were unsuccessful[1,3,9].
The main study endpoint was the incidence of hypoxemia, including mild (SpO2 = 75%-89% for < 60 s) and severe hypoxemia (SpO2 < 90% for > 60 s or < 75% at any time)[5]. The secondary endpoints included (1) the lowest SpO2 during gastroscopy; (2) interventions to manage hypoxemia, including jaw thrust, facemask ventilation, and/or endotracheal intubation, as described above; (3) adverse events, such as epistaxis, body movement and cough during gastroscopy, and postoperative sore throat; and (4) satisfaction among anesthetists, physicians and patients. Epistaxis was assessed by gastroscopy using a subjective scale: 0, no bleeding; 1, minimal bleeding not requiring suctioning; 2, moderate bleeding requiring suctioning but not hampering visualization; and 3, severe bleeding requiring suctioning and hampering visualization[10]. Postoperative sore throat was assessed at the time of consciousness recovery and 30 min later. At 30 min after the procedure, satisfaction among anesthetists, physicians and patients was evaluated using a 10-point scale and classified as follows: Poor, 1-4; fair, 5-7; and good, 8-10[11].
Computer-generated randomization sequences were used for group assignment in our study. The randomization sequence was generated by a research assistant who was independent of the study and did not have contact with the study participants. Randomization was performed using opaque sealed envelopes before sedation induction.
The sample size was calculated with Pass software (version 11.0, NCSS, LLC, Kaysville, UT, United States). The two independent proportions procedure was used. According to our preliminary experimental results, the incidence of hypoxemia in obese patients during gastroscopy with propofol mono-sedation was 22%; thus, 22% of patients in the nasal cannula group were expected to develop hypoxemia. P1 and P2 were calculated based on the assumption that the WNJT would achieve a reduction in the incidence of hypoxemia from 22% to 11%. Given an α = 0.05 and a power of 80%, it was estimated that 140 patients per group would be required for our study. Assuming a dropout rate of 10%, a total of 308 patients (154 in each group) would be required.
Our study data were managed by statisticians from the Clinical Research Institute of Beijing Friendship Hospital. An interim analysis was performed by the Data and Safety Monitoring Board of our hospital when data from 103 patients were obtained. The results of the interim data analysis suggested that the study could be terminated, as the primary endpoint and secondary endpoints had been reached. Thus, we decided to halt the participation of any additional individuals, even though the initial estimation of sample size had been assumed to be approximately 308 patients.
Statistical analysis of data was performed using SPSS (version 23.0) by a blinded statistician from the Clinical Research Institute of Beijing Friendship Hospital. Data were summarized as means ± SD or medians (25th and 75th percentiles) for continuous data and as frequencies and percentages for categorical data. For continuous data, the characteristics and outcomes of the two groups were compared using the Student's t-test or Wilcoxon-Mann-Whitney test based on the viability of the normality assump
The flow chart of the included and excluded patients in this study is shown in Figure 1. A total of 659 subjects were enrolled, and 556 were excluded. Thus, 103 patients were included in the study and randomly assigned. After randomization, however, 2 patients were further excluded because of a failed insertion of the WNJT. Ultimately, 49 patients in the WNJT group and 52 in the nasal cannula group were used for data analysis. The baseline characteristics of the study subjects were not significantly different between groups. However, the total propofol dosage was significantly lower in the nasal cannula group than in the WNJT group (Table 1).
| Characteristic | WNJT group, n = 49 | Nasal cannula group, n = 52 | P value |
| Age (yr) | 37.89 ± 13.7 | 37.5 ± 12.5 | 0.892 |
| Height (m) | 1.7 ± 0.1 | 1.7 ± 0.1 | 0.293 |
| Weight (kg) | 100.7 ± 17.0 | 96.4 ± 18.2 | 0.217 |
| Sex (M/F) | 19/30 | 16/36 | 0.398 |
| Body mass index (kg/m2) | 35.6 ± 4.8 | 34.7 ± 4.1 | 0.316 |
| Baseline SpO2 (%) | 97.1 ± 1.5 | 97.1 ± 1.6 | 0.982 |
| ASA physical status grade (I/II) | 22/27 | 23/29 | 0.946 |
| Procedure times (min) | 4.6 ± 0.9 | 4.8 ± 0.4 | 0.065 |
| Total propofol dosages (mg) | 229.4 ± 41.7 | 210.2 ± 45.4 | 0.030 |
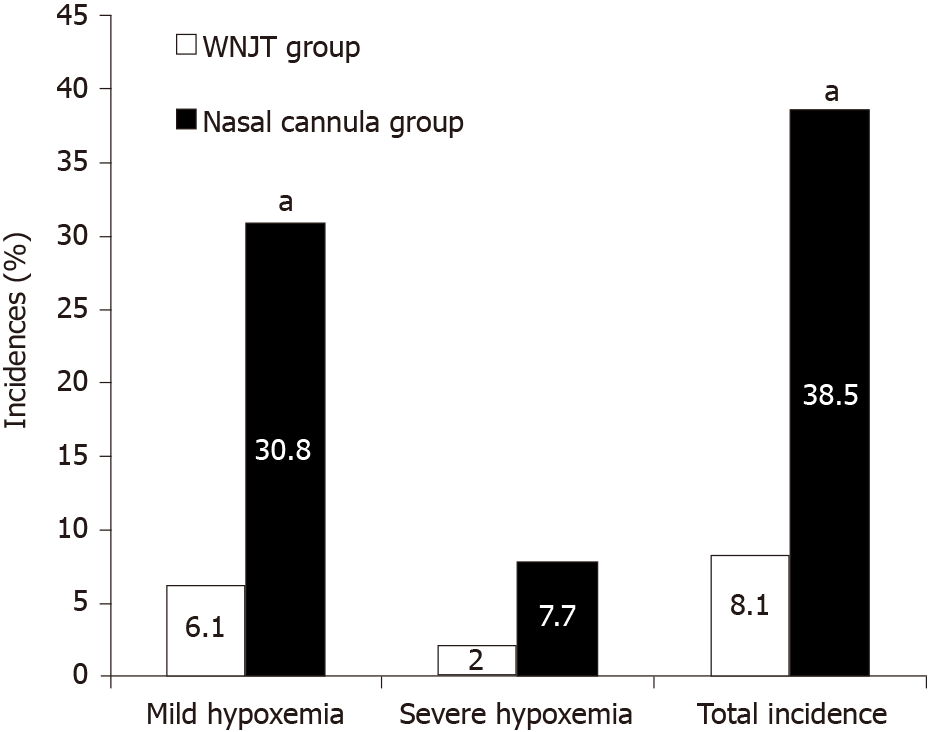
The occurrence of mild and severe hypoxemia during gastroscopy is shown in Figure 2, and the lowest SpO2 and the occurrence of adverse events and interventions related to hypoxemia during gastroscopy are listed in Table 2. The incidence of severe hypoxemia during gastroscopy (2% vs 7.7%) was comparable between groups, but the incidence of mild hypoxemia (6.1% vs 30.8%) and total incidence of hypoxemia (8.1% vs 38.5%) during gastroscopy were significantly decreased in the WNJT group compared with the nasal cannula group. The lowest SpO2 during gastroscopy was significantly higher in the WNJT group than in the nasal cannula groups. Furthermore, the use of airway opening maneuvers to correct hypoxemia during gastroscopy was significantly less common in the WNJT group than in the nasal cannula group. In the WNJT group, minimal to moderate epistaxis was noticed by gastroscopy in three patients. In the nasal cannula group, no patients had epistaxis, but four patients required an interruption of the endoscopic procedure for facemask ventilation to correct hypoxemia. In addition to a significantly higher incidence of epistaxis in the WNJT group, the two groups were comparable with respect to other adverse events. The satisfaction of patients was not significantly different between groups, but satisfaction among both anesthetists and physicians was significantly higher in the WNJT group (Table 3).
| WNJT group, n = 49 | Nasal cannula group, n = 52 | P value | |
| Lowest SpO2 during gastroscopy | 95.5 ± 4.3 | 90.0 ± 7.0 | 0.000 |
| Airway opening maneuvers | 7 (14.3) | 36 (69.2) | 0.000 |
| Facemask ventilation | 0 (0) | 4 (7.7) | 0.118 |
| Body movement | 7 (14.3) | 5 (9.6) | 0.468 |
| Cough | 5 (10.2) | 4 (7.7) | 0.926 |
| Epistaxis (0/1/2/3) | 0/2/1/0 (6.1) | 0/0/0/0 (0) | 0.111 |
| Sore throat | 2 (4.1) | 1 (1.9) | 0.610 |
| WNJT group, n = 49 | Nasal cannula group, n = 52 | P values | |||||
| Good | Fair | Poor | Good | Fair | Poor | ||
| Physicians | 49 (100) | 0 (0) | 0 (0) | 46 (88.5) | 5 (9.6) | 1 (1.9) | 0.015 |
| Anesthetists | 46 (93.9) | 2 (4.1) | 1(2.0) | 38 (73.1) | 12 (23.1) | 2 (3.8) | 0.006 |
| Patients | 49 (100) | 0 (0) | 0(0) | 52 (100) | 0 (0) | 0 (0) | 1.000 |
As obese patients have altered anatomy of the airway, reduced functional residual volume of the lungs and decreased compliance of the chest wall, hypoxemia caused by transient respiratory depression and airway obstruction is very common during painless UGI endoscopy with sedation or anesthesia[12,13]. In fact, obesity has been identified as an independent risk factor for sedation-related adverse events, including hypoxemia during UGI endoscopy with sedation[4,14,15]. By comparing the efficacy and safety of the WNJT to a conventional nasal cannula for supplemental oxygen during gastroscopy under propofol mono-sedation in obese patients with a BMI of 30 kg/m2 or more, the main findings of this study were as follows: (1) with 5 L/min supplemental oxygen, the use of the WNJT compared with conventional nasal cannula significantly increased SpO2 levels and decreased the occurrence of hypoxemia and the use of airway opening maneuvers during gastroscopy; (2) other than a significantly higher incidence of minimal to moderate epistaxis in patients using the WNJT, the occurrence of other adverse events was similar between the devices; and (3) the two devices produced comparable satisfaction among patients, but the WNJT provided greater satisfaction among anesthetists and physicians. These results suggest that the WNJT may be a useful tool with a clinically acceptable risk-benefit ratio for the prevention of hypoxemia during gastroscopy with propofol mono-sedation in obese patients.
Our results showed that the use of the WNJT compared to a conventional nasal cannula for supplemental oxygen can significantly improve oxygenation and decrease the occurrence of hypoxemia in obese patients undergoing gastroscopy with propofol mono-sedation. This finding is consistent with the previous findings in Xiao’s study comparing a conventional nasopharyngeal airway to a nasal cannula for supplemental oxygen in obese patients undergoing UGI endoscopy with propofol sedation[12]. These results at least indicate that the WNJT is as effective as the conventional nasopharyngeal airway for the maintenance of ventilation and the prevention of hypoxemia during UGI endoscopy with propofol sedation in obese patients.
Given that inserting a conventional nasopharyngeal airway is an invasive procedure, the risk of nasal passage injury is always a concern. It has been reported that the incidence of epistaxis when using a conventional nasopharyngeal airway is approximately 5%-12.5%[16-19]. In our present study, epistaxis was observed in only 3 obese patients using the WNJT, with a 6.1% incidence of epistaxis (3/49). Our previous work in patients with a normal BMI showed that the incidence of epistaxis by WNJT insertion was 4.9% (7/144)[6]. This indicates that the WNJT does not significantly increase the occurrence of epistaxis in obese patients compared to patients with a normal BMI. However, Qin et al[5] reported a low incidence of epistaxis of 0.7% (4/596) in patients receiving supplemental oxygen with the WNJT during UGI endoscopy with propofol sedation and 2% (12/592) in patients receiving supraglottic jet oxygenation and ventilation with the WNJT, respectively[5]. In contrast, when supraglottic jet oxygenation and ventilation were carried out with the WNJT, an incidence of epistaxis as high as 16% was reported by Zha et al[20] in sedated patients undergoing flexible bronchoscopy (16/137) and by Wu et al[21] in anesthetized patients receiving intubation with fiber optic bronchoscopy (4/25). As the details of the assessment criteria for epistaxis in other studies are not provided, the exact reasons for these different findings remain unclear. Taking into consideration a comprehensive analysis of data obtained from our study and from other studies[5,6,20,21], the mean incidence of epistaxis with the WNJT, which is approximately 3% (46/1543), seems lower than that seen with a conventional nasopharyngeal airway as reported in previous studies[16-19].
In our study, gastroscopic procedure time was not significantly different between groups, indicating that the insertion of the WNJT compared with the placement of a conventional nasal cannula does not significantly prolong gastroscopic procedure time. This may be mainly because the insertion of the WNJT is a simple procedure that operators can easily master. However, the total propofol dosage was significantly decreased in the nasal cannula group compared with the WNJT group. This may be because the insertion of the WNJT can produce stronger stimulation to the nasal passage and the upper airway. Regardless, the difference in median propofol dosages between groups was only 30 mg. For most obese patients, this small difference in median propofol dosages would not be clinically significant.
Our study showed that the two devices produced comparable satisfaction among patients, but the WNJT provided improved satisfaction among anesthetists and physicians. These findings may be related to the following factors. (1) The use of the WNJT involves an invasive procedure, although it is inserted after adequate sedation and removed before full recovery of sedation. Furthermore, epistaxis occurred in only a few patients in whom the WNJT was used, and the incidence of postoperative sore throat was same with the two devices. These findings may account for the similar satisfaction of patients with the two devices; and (2) The occurrence of adverse events and the need for the use of interventions to address adverse events during UGI endoscopy with sedation are the main determinants of satisfaction among anesthetists and physicians[22]. The higher incidence of hypoxemia and more frequent need for conventional airway opening maneuvers during gastroscopy in patients in whom a nasal cannula was used may explain why both anesthetists and physicians were more satisfied with the WNJT.
There are some limitations in our study design that deserve special attention. First, the insertion of the WNJT after sedation and the removal of the WNJT before full recovery of sedation make patients blind to group assignment, but investigators are not similarly blinded to which devices are used. Therefore, the present study is a single-blinded trial with potential biases of outcome assessment. Second, the duration of gastroscopy in our study was relatively short, commonly approximately 5 min. Consequently, our results should not be extrapolated to other settings with a longer duration of UGI endoscopic procedures, such as endoscopic retrograde cholangiopancreatography. Third, propofol mono-sedation was used in this study. As various sedation regimens may result in different effects on respiratory function during UGI endoscopy[23,24], our results are not representative of patients undergoing UGI endoscopy using propofol combined with other sedatives, including midazolam or opioids. Fourth, the subjects in our study were obese patients ages 18-65 years, with ASA physical status classifications 1-2. The available evidence indicates that age can significantly affect the pharmacokinetics and pharmacodynamics of propofol[25]. Furthermore, the occurrence of adverse events during UGI endoscopy with propofol sedation has been significantly associated with increased age and ASA physical status classifications greater than 2[26,27]. Thus, our results can also not be extrapolated to elderly obese patients and obese patients with multiple comorbidities. Consequently, further clinical trials to address the above issues are needed.
In summary, this single-center, prospective RCT demonstrates that with 5 L/min supplemental oxygen, the WNJT, compared with a conventional nasal cannula, can significantly reduce the occurrence of hypoxemia and provide increased satisfaction among anesthetists and physicians, although its use may lead to mild epistaxis in a few patients. In view of a better risk-benefit ratio, the WNJT should be recommended as an alternative tool to provide supplemental oxygen for the prevention of hypoxemia during gastroscopy with propofol mono-sedation in obese patients.
Hypoxemia by respiratory depression and airway obstruction during upper gastrointestinal endoscopy with sedation is a common concern, especially in obese patients. The nasal cannula is one of the most convenient tools for supplemental oxygen, but it cannot overcome upper airway obstruction. Compared with a nasal cannula (prongs), a conventional nasopharyngeal airway can provide improved efficiency of supplemental oxygen during upper gastrointestinal endoscopy with sedation, but the insertion of the nasopharyngeal airway is an invasive procedure with a potential risk of airway injury.
In view of the significant limitations of available supplemental oxygen methods, it is necessary to find new effective measures for administering supplemental oxygen during upper gastrointestinal endoscopy with sedation. The Wei nasal jet tube (WNJT) is a new special nasopharyngeal airway made of soft material. Our previous work in patients with normal body mass index (BMI) demonstrated that the WNJT compared with a nasal cannula for supplemental oxygen at 5 L/min is more effective for the prevention of hypoxemia during gastroscopy with propofol mono-sedation. For obese patients with an increased risk of hypoxemia during gastroscopy with sedation, however, it remains unclear whether the WNJT is an effective and safe tool for supplemental oxygen.
In this study, we aimed to determine whether the WNJT performs better than a nasal cannula (prongs) for the prevention of hypoxemia during gastroscopy with propofol mono-sedation in obese patients when moderate oxygen flow is provided.
To address the question of whether the WNJT performs better than nasal cannula (prongs) for the prevention of hypoxemia during gastroscopy with propofol mono-sedation when moderate oxygen flow is provided in obese patients, we designed this study as a prospective, randomized controlled trial in which patients with a BMI of 30 kg/m2 or greater, undergoing elective gastroscopy with propofol mono-sedation, were randomized into the two groups to receive either the WNJT or a nasal cannula for supplemental oxygen at a 5 L/min flow rate. The primary endpoint was the incidence of hypoxemia and of severe hypoxemia during gastroscopy.
A total of 103 obese patients were randomized into the two groups, but 49 patients in the WNJT group and 52 patients in the nasal cannula group were used for data analysis, because two patients in the WNJT group were excluded. The total incidence of hypoxemia and of severe hypoxemia during gastroscopy was significantly decreased in the WNJT group compared with the nasal cannula group. Epistaxis by device insertion in the WNJT group occurred in three patients. Other than epistaxis, the occurrence of adverse events was similar between the devices. The two devices did not produce a statistically significant difference in patient satisfaction, but the WNJT did provide increased satisfaction among anesthetists and physicians.
During gastroscopy with propofol mono-sedation in obese patients, the WNJT, compared with a nasal cannula for supplemental oxygen, can significantly reduce the occurrence of hypoxemia and improve satisfaction among anesthetists and physicians, although its use may lead to epistaxis in a few patients.
With a moderate oxygen flow of 5 L/min, the WNJT performs better than a nasal cannula (prongs) for the prevention of hypoxemia during gastroscopy with propofol mono-sedation in obese patients. Thus, in view of a clinically acceptable risk-benefit ratio, the WNJT should be recommended as an alternative tool for supplemental oxygen for the prevention of hypoxemia during gastroscopy with propofol mono-sedation in obese patients.
We thank Dr. Na Zeng from the Department of Methodology Platform, Institute of Clinical Medicine, Beijing Friendship Hospital, for her help with statistical analysis of the data.
Manuscript source: Unsolicited manuscript
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Protopapas AA S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Liu JH
| 1. | Dumonceau JM, Riphaus A, Aparicio JR, Beilenhoff U, Knape JT, Ortmann M, Paspatis G, Ponsioen CY, Racz I, Schreiber F, Vilmann P, Wehrmann T, Wientjes C, Walder B; NAAP Task Force Members. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology Guideline: Non-anesthesiologist administration of propofol for GI endoscopy. Endoscopy. 2010;42:960-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 133] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 2. | Beitz A, Riphaus A, Meining A, Kronshage T, Geist C, Wagenpfeil S, Weber A, Jung A, Bajbouj M, Pox C, Schneider G, Schmid RM, Wehrmann T, von Delius S. Capnographic monitoring reduces the incidence of arterial oxygen desaturation and hypoxemia during propofol sedation for colonoscopy: a randomized, controlled study (ColoCap Study). Am J Gastroenterol. 2012;107:1205-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Cohen LB, Wecsler JS, Gaetano JN, Benson AA, Miller KM, Durkalski V, Aisenberg J. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol. 2006;101:967-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 356] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 4. | Wani S, Azar R, Hovis CE, Hovis RM, Cote GA, Hall M, Waldbaum L, Kushnir V, Early D, Mullady DK, Murad F, Edmundowicz SA, Jonnalagadda SS. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011;74:1238-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Qin Y, Li LZ, Zhang XQ, Wei Y, Wang YL, Wei HF, Wang XR, Yu WF, Su DS. Supraglottic jet oxygenation and ventilation enhances oxygenation during upper gastrointestinal endoscopy in patients sedated with propofol: a randomized multicentre clinical trial. Br J Anaesth. 2017;119:158-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Shao LJ, Zou Y, Liu FK, Wan L, Liu SH, Hong FX, Xue FS. Comparison of two supplemental oxygen methods during gastroscopy with propofol mono-sedation in patients with a normal body mass index. World J Gastroenterol. 2020;26:6867-6879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Shao LJ, Liu SH, Liu FK, Zou Y, Hou HJ, Tian M, Xue FS. Comparison of two supplement oxygen methods during gastroscopy with intravenous propofol anesthesia in obese patients: study protocol for a randomized controlled trial. Trials. 2018;19:602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, Schwam EM, Siegel JL. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244-251. [PubMed] |
| 9. | Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: Nonanesthesiologist administration of propofol for GI endoscopy. Hepatology. 2009;50:1683-1689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Vadhanan P, Tripaty DK. Effect of Bougie-Guided Nasal Intubations upon Bleeding: A Randomised Controlled Trial. Turk J Anaesthesiol Reanim. 2018;46:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Ibáñez M, Parra-Blanco A, Zaballa P, Jiménez A, Fernández-Velázquez R, Fernández-Sordo JO, González-Bernardo O, Rodrigo L. Usefulness of an intensive bowel cleansing strategy for repeat colonoscopy after preparation failure. Dis Colon Rectum. 2011;54:1578-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Xiao Q, Yang Y, Zhou Y, Guo Y, Ao X, Han R, Hu J, Chen D, Lan C. Comparison of Nasopharyngeal Airway Device and Nasal Oxygen Tube in Obese Patients Undergoing Intravenous Anesthesia for Gastroscopy: A Prospective and Randomized Study. Gastroenterol Res Pract. 2016;2016:2641257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Siampalioti A, Karavias D, Zotou A, Kalfarentzos F, Filos K. Anesthesia management for the super obese: is sevoflurane superior to propofol as a sole anesthetic agent? Eur Rev Med Pharmacol Sci. 2015;19:2493-2500. [PubMed] |
| 14. | Berzin TM, Sanaka S, Barnett SR, Sundar E, Sepe PS, Jakubowski M, Pleskow DK, Chuttani R, Sawhney MS. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73:710-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Coté GA, Hovis RM, Ansstas MA, Waldbaum L, Azar RR, Early DS, Edmundowicz SA, Mullady DK, Jonnalagadda SS. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 196] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 16. | Gallagher WJ, Pearce AC, Power SJ. Assessment of a new nasopharyngeal airway. Br J Anaesth. 1988;60:112-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Stoneham MD. The nasopharyngeal airway. Assessment of position by fibreoptic laryngoscopy. Anaesthesia. 1993;48:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Feldman SA, Fauvel NJ, Ooi R. The cuffed pharyngeal airway. Eur J Anaesthesiol. 1991;8:291-295. [PubMed] |
| 19. | Liang H, Hou Y, Sun L, Li Q, Wei H, Feng Y. Supraglottic jet oxygenation and ventilation for obese patients under intravenous anesthesia during hysteroscopy: a randomized controlled clinical trial. BMC Anesthesiol. 2019;19:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Zha B, Wu Z, Xie P, Xiong H, Xu L, Wei H. Supraglottic jet oxygenation and ventilation reduces desaturation during bronchoscopy under moderate to deep sedation with propofol and remifentanil: A randomised controlled clinical trial. Eur J Anaesthesiol. 2021;38:294-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Wu C, Wei J, Cen Q, Sha X, Cai Q, Ma W, Cao Y. Supraglottic jet oxygenation and ventilation-assisted fibre-optic bronchoscope intubation in patients with difficult airways. Intern Emerg Med. 2017;12:667-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Zhang H, Liu CM. Target-controlled intravenous analgesia with remifentanil on hypoxemia in obese patients with painless gastroscopy (In Chinese). Yixue Yanjiu Zazhi. 2017;46:154-156. [DOI] [Full Text] |
| 23. | Behrens A, Kreuzmayr A, Manner H, Koop H, Lorenz A, Schaefer C, Plauth M, Jetschmann JU, von Tirpitz C, Ewald M, Sackmann M, Renner W, Krüger M, Schwab D, Hoffmann W, Engelke O, Pech O, Kullmann F, Pampuch S, Lenfers B, Weickert U, Schilling D, Boehm S, Beckebaum S, Cicinnati V, Erckenbrecht JF, Dumoulin FL, Benz C, Rabenstein T, Haltern G, Balsliemke M, de Mas C, Kleber G, Pehl C, Vogt C, Kiesslich R, Fischbach W, Koop I, Kuehne J, Breidert M, Sass NL, May A, Friedrich C, Veitt R, Porschen R, Ellrichmann M, Arlt A, Schmitt W, Dollhopf M, Schmidbaur W, Dignass A, Schmitz V, Labenz J, Kaiser G, Krannich A, Barteska N, Ell C. Acute sedation-associated complications in GI endoscopy (ProSed 2 Study): results from the prospective multicentre electronic registry of sedation-associated complications. Gut. 2019;68:445-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 24. | Frieling T, Heise J, Kreysel C, Kuhlen R, Schepke M. Sedation-associated complications in endoscopy--prospective multicentre survey of 191142 patients. Z Gastroenterol. 2013;51:568-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Sahinovic MM, Struys MMRF, Absalom AR. Clinical Pharmacokinetics and Pharmacodynamics of Propofol. Clin Pharmacokinet. 2018;57:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 354] [Cited by in RCA: 355] [Article Influence: 50.7] [Reference Citation Analysis (0)] |
| 26. | Leslie K, Allen ML, Hessian EC, Peyton PJ, Kasza J, Courtney A, Dhar PA, Briedis J, Lee S, Beeton AR, Sayakkarage D, Palanivel S, Taylor JK, Haughton AJ, O'Kane CX. Safety of sedation for gastrointestinal endoscopy in a group of university-affiliated hospitals: a prospective cohort study. Br J Anaesth. 2017;118:90-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 27. | Friedrich-Rust M, Welte M, Welte C, Albert J, Meckbach Y, Herrmann E, Kannengiesser M, Trojan J, Filmann N, Schroeter H, Zeuzem S, Bojunga J. Capnographic monitoring of propofol-based sedation during colonoscopy. Endoscopy. 2014;46:236-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |