Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5453
Peer-review started: March 12, 2021
First decision: April 24, 2021
Revised: April 26, 2021
Accepted: May 7, 2021
Article in press: May 7, 2021
Published online: July 16, 2021
Processing time: 117 Days and 20.8 Hours
Coronary artery disease (CAD) is one of the leading causes of death and disease burden in China and worldwide. A practical and reliable prediction scoring system for CAD risk and severity evaluation is urgently needed for primary prevention.
To examine whether the prediction for atherosclerotic cardiovascular disease risk in China (China-PAR) scoring system could be used for this purpose.
A total of 6813 consecutive patients who underwent diagnostic coronary angiography were enrolled. The China-PAR score was calculated for each patient and CAD severity was assessed by the Gensini score (GS).
Correlation analysis demonstrated a significant relationship between China-PAR and GS (r = 0.266, P < 0.001). In receiver operating characteristic curve analysis, the cut-off values of China-PAR for predicting the presence and the severity of CAD were 7.55% with a sensitivity of 55.8% and specificity of 71.8% [area under the curve (AUC) = 0.693, 95% confidence interval: 0.681 to 0.706, P < 0.001], and 7.45% with a sensitivity of 58.8% and specificity of 67.2% (AUC = 0.680, 95% confidence interval: 0.665 to 0.694, P < 0.001), respectively.
The China-PAR scoring system may be useful in predicting the presence and severity of CAD.
Core Tip: Very few researchers have focused on the validity of risk score models in predicting the severity of coronary artery disease. In our study, a total of 6813 consecutive patients who underwent diagnostic coronary angiography were enrolled. The prediction for atherosclerotic cardiovascular disease risk in China (China-PAR) score was calculated for each patient and coronary artery disease severity was assessed by the Gensini score. Finally, the China-PAR scoring system was discovered to be applicable in the estimation of both the presence and severity of coronary artery disease in addition to their role in predicting cardiovascular events.
- Citation: Hong XL, Chen H, Li Y, Teeroovengadum HD, Fu GS, Zhang WB. Prediction of presence and severity of coronary artery disease using prediction for atherosclerotic cardiovascular disease risk in China scoring system. World J Clin Cases 2021; 9(20): 5453-5461
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5453.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5453
Coronary artery disease (CAD) is a leading cause of death and disease burden in China and worldwide[1-3]. The cost of hospitalization for acute myocardial infarction (MI) in China is substantially high, contributing to the major challenge of primary care in China[3]. Therefore, it is of great significance to develop equations for CAD risk and severity evaluation before the clinical signs or cardiovascular events of CAD occur.
Several prediction models for CAD risk evaluation have been built and applied in public health and clinical practice. Well-known equations are the Framingham risk score (FRS) developed in1976[4], the Systematic Coronary Risk Evaluation (SCORE) in Europe[5], QRESEARCH cardiovascular risk (QRISK1 and QRISK2) algorithms in the United Kingdom[6], Pooled Cohort Equations (PCEs) reported in the American College of Cardiology/American Heart Association guideline[7], and the most recently published prediction for atherosclerotic cardiovascular disease risk in China (China-PAR) scoring system[8].
Many investigators have evaluated the performance of two or more risk prediction models in different populations. However, very few researchers have focused on the validity of the risk score models in predicting the severity of CAD. Thus, we conducted this study to evaluate the utility of the China-PAR score in assessing the severity of CAD in the Chinese population.
This was a retrospective study in which a total of 6813 consecutive patients who were admitted for diagnostic coronary angiography (CAG) were enrolled. Our study complied with the Declaration of Helsinki and was approved by the hospital ethics review board (Sir Run Run Shaw Hospital, Zhejiang Province, China). All study patients were referred for CAG according to the results of their electrocardiograms, abnormal noninvasive stress tests, and/or symptoms suggestive of CAD. Patients who had acute coronary syndrome, chronic or acute heart failure, severe chronic renal disease, previous myocardial infarction or percutaneous coronary intervention, and previous coronary artery bypass surgery were excluded. Initially, two experienced interventional cardiologists evaluated all patients’ angiograms and assessed the Gensini score (GS). Thereafter, four medical students without knowledge of patients’ CAD status calculated the China-PAR score through a mobile automatic calculator (http://www.cvdrisk.com.cn/ASCVD/Eval).
Detailed clinical and demographic characteristics were obtained from all patients. Overnight fasting venous blood samples were taken on the same day of the procedure. The left ventricular ejection fraction was evaluated by echocardiograph before angiography. Waist circumference (WC) was measured at 1 cm above the navel at minimal respiration. Cigarette smoking was defined as ever-smoked 100 cigarettes or currently smoking. Hypertension was defined as repeated blood pressure measurements of systolic blood pressure ≥ 140 mmHg, diastolic ≥ 90 mmHg, or currently taking antihypertensive drugs. Type 2 diabetes mellitus (DM) was defined as a previous diagnosis and/or fasting blood glucose of 126 mg/dL or under current treatment of antidiabetic medications. Family history of atherosclerotic cardiovascular disease (ASCVD) was defined as at least one first-degree relative with MI or stroke. The China-PAR scoring system predicts the risk for development of CAD by taking into account age, sex, geographic region, urbanization, WC, total cholesterol, high-density lipoprotein cholesterol (HDL-C), blood pressure, DM, current smoking, and family history of ASCVD.
Selective coronary angiography was performed via the Judkins technique. Significant CAD was diagnosed if there was ≥ 50% diameter stenosis in at least one major epicardial coronary artery. The severity of CAD was calculated with the GS system by assigning a severity score to each coronary stenosis as 1 for 1% to 25% narrowing, 2 for 26% to 50%, 4 for 51% to 75%, 8 for 76% to 90%, 16 for 91% to 99%, and 32 for a completely occluded artery. A multiplier was then assigned according to the importance of the coronary artery: 5 for the left main coronary artery, 2.5 for the proximal segment of the left anterior descending (LAD) coronary artery, 2.5 for the proximal segment of the circumflex artery, 1.5 for the mid-segment of the LAD, 1.0 for the distal segment of the LAD, mid-distal region of the circumflex artery, the obtuse marginal artery, the right coronary artery, and the posterolateral artery, and 0.5 for any other branch[9].
Statistical analyses were carried out using the SPSS statistical package, version 18.0 (SPSS Inc, Chicago, IL, United States). Continuous values are expressed as the mean ± SD or median (minimum to maximum). Differences between the means were compared by t test when the variables showed a normal distribution, or by the Mann-Whitney U test when they did not. ANOVA or Kruskal–Wallis test was used to compare variables among three groups. Categorical variables are presented as counts and percentages and were compared by the chi-square test. Correlations were evaluated via Spearman’s rank test. Receiver operating characteristic (ROC) curve analysis was conducted to determine the value of China-PAR score for predicting the severity of coronary. A two-sided P value < 0.05 was considered significant.
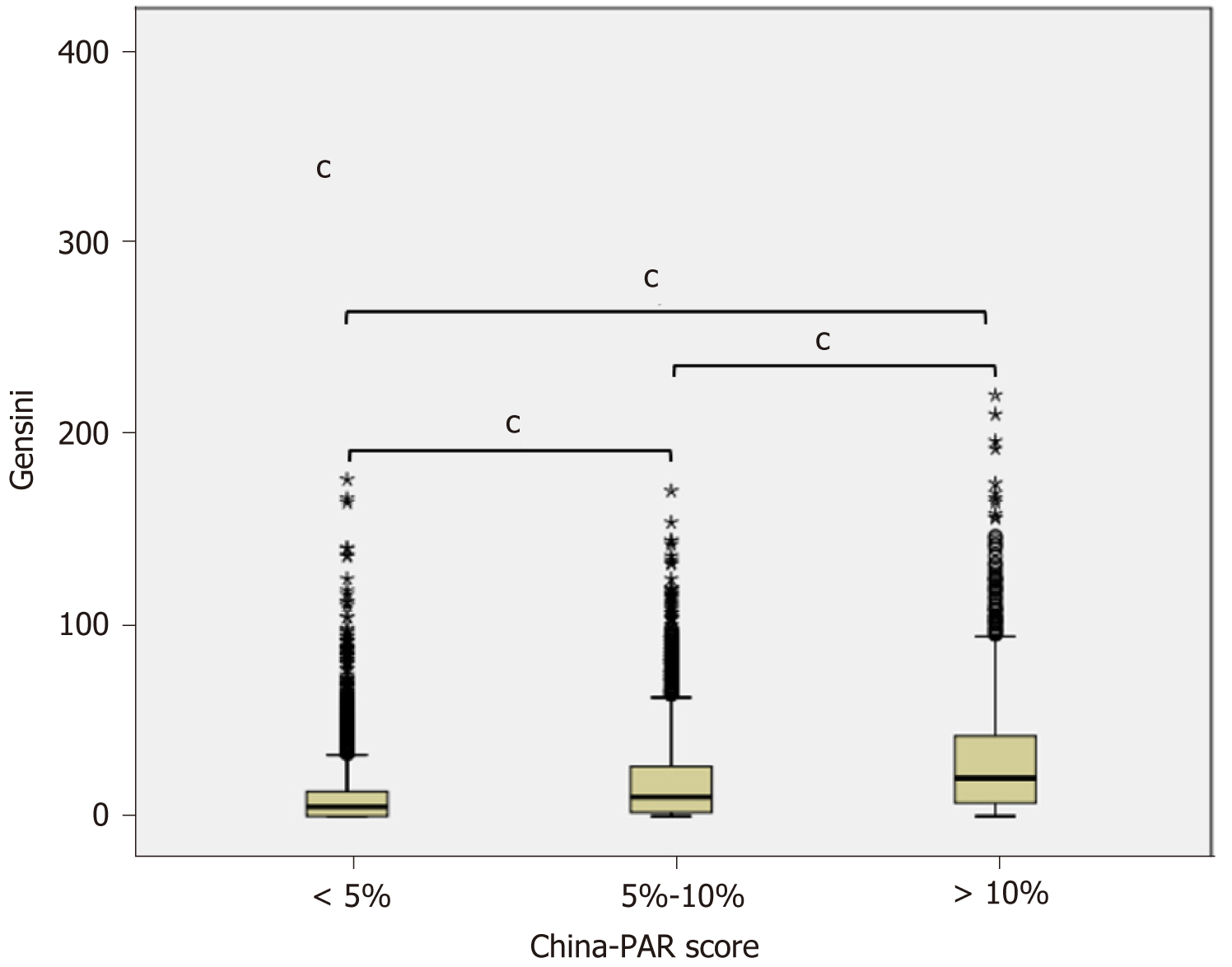
A comparison of clinical and demographical characteristics of the GS = 0, low GS [7 (4, 11)], and high-GS [34 (24, 52)] groups is presented in Table 1. There was a statistically significant difference among the three groups in terms of the related risk factors (P < 0.001 or P < 0.05). The mean age, WC, percentage of males, hypertension, DM, smoking, and family history of ASCVD were the highest in the high-GS group (P < 0.001), whereas HDL-C levels and epidermal growth factor receptor were the lowest in the high-GS group (P < 0.001). When each group was classified by China-PAR risk stratification, the high-GS group presented a higher proportion of patients with China-PAR > 10%, and lower proportion of patients with China-PAR < 5% (P < 0.001). In addition, the higher China-PAR score group tended to have a higher GS (P < 0.001) (Figure 1).
| Gensini score = 0 | Low-Gensini score | High-Gensini score | P value1 | P value | P value | P value | |
| 0 | 7 (4, 11) | 34 (24, 52) | (Group 1-2) | (Group 1-3) | (Group 2-3) | ||
| Number of patients | 1601 | 2628 | 2584 | ||||
| Age (yr) | 62 (55, 69) | 64 (57, 69) | 67 (61, 73) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Male, n (%) | 826 (51.6) | 1474 (56.1) | 1790 (69.3) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Waist circumference | 82 (80, 87) | 82 (80, 87) | 82 (80, 87) | < 0.001 | 0.693 | 0.002 | 0.002 |
| BMI, kg/m2 | 24.4 (22.1, 26.8) | 24.3 (22.2, 26.6) | 24.2 (22.2, 26.3) | 0.028 | 0.282 | 0.047 | 0.284 |
| Hypertension, n (%) | 756 (47.2) | 1441 (54.8) | 1724 (66.7) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| DM, n (%) | 194 (12.1) | 406 (15.4) | 658 (25.5) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Smoking, n (%) | 228 (14.2) | 427 (16.2) | 514 (19.9) | < 0.001 | 0.08 | < 0.001 | 0.001 |
| Family history of ASCVD | 4 (0.2) | 35 (1.3) | 110 (4.3) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| EF, % | 55.65 (38, 65.09) | 68 (62.9, 72.7) | 66.8 (61.3, 72) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Glucose, mmol/L | 5.45 (4.92, 6.39) | 5.53 (4.95, 6.60) | 5.76 (5.07, 7.15) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| eGFR | 93.3 (80.9, 102.1) | 91.5 (80, 100) | 88 (74, 97.9) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| NT-ProBNP | 95 (45, 320) | 79 (40, 209.75) | 131 (59, 377.75) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Triglyceride | 4.34 (3.64, 5.059) | 4.19 (3.45, 5.03) | 4.099 (3.45, 4.97) | 0.026 | 0.885 | 0.029 | 0.019 |
| TC | 1.39 (0.99, 1.99) | 1.38 (1, 1.9775) | 1.45 (1.03, 2.04) | 0.012 | 0.001 | < 0.001 | 0.189 |
| LDL-C | 2.33 (1.74, 2.88) | 2.19 (1.62, 2.87) | 2.16 (1.64, 2.83) | 0.03 | < 0.001 | < 0.001 | 0.687 |
| HDL-C | 0.94 (0, 1.11) | 0.9325 (0, 1.1) | 0.88 (0, 1.03) | < 0.001 | 0.092 | < 0.001 | < 0.001 |
| China-PAR | 5.3 (3.1, 7.9) | 6 (3.8, 8.9) | 8.5 (5.8, 12.2) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| < 5%, n (%) | 744 (46.5) | 1009 (38.4) | 454 (17.6) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| 5%-10%, n (%) | 616 (38.5) | 1115 (42.4) | 1150 (44.5) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| > 10%, n (%) | 241 (15.1) | 504 (19.2) | 980 (37.9) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Table 2 displays the characteristics of patients divided by the presence of CAD or not. China-PAR score was significantly higher in the CAD group than in the non-CAD group (P < 0.001). The CAD group also revealed a higher proportion of patients with China-PAR > 10%, and lower proportion of patients with China-PAR < 5% (P < 0.001).
| Non-CAD | CAD | P value1 | |
| Number of patients | 3365 | 3448 | |
| Age (yr) | 62 (56, 69) | 67 (60, 73) | < 0.001 |
| Male, n (%) | 1778 (52.8) | 2312 (67.1) | < 0.001 |
| Waist circumference | 82 (80, 87) | 82 (80, 87) | 0.026 |
| BMI, kg/m2 | 24.4 (22.3, 26.7) | 24.2 (22.2, 26.3) | < 0.001 |
| Hypertension, n (%) | 1660 (49.3) | 2261 (65.6) | < 0.001 |
| DM, n (%) | 417 (12.4) | 841 (24.4) | < 0.001 |
| Smoking, n (%) | 501 (14.9) | 668 (19.4) | < 0.001 |
| Family history of ASCVD | 21 (0.6) | 128 (3.7) | < 0.001 |
| EF, n (%) | 67.3 (62, 72.2) | 67 (61.8, 72.09) | 0.071 |
| Glucose, mmol/L | 5.46 (4.92, 6.44) | 5.72 (5.059, 7.05) | < 0.001 |
| eGFR | 93 (81.3, 101.3) | 88.34 (74.7, 97.98) | < 0.001 |
| NT-ProBNP | 83 (41, 249) | 116 (54, 328) | < 0.001 |
| Triglyceride | 1.38 (0.99, 1.98) | 1.44 (1.03, 2.03) | 0.009 |
| TC | 4.28 (3.55, 5.06) | 4.12 (3.44, 4.98) | < 0.001 |
| LDL-C | 2.27 (1.69, 2.88) | 2.15 (1.63, 2.83) | 0.323 |
| HDL-C | 1.11 (0.94, 1.31) | 1.05 (0.89, 1.24) | < 0.001 |
| China-PAR | 5.4 (3.4, 8.0) | 8.2 (5.4, 12.0) | < 0.001 |
| < 5%, n (%) | 1497 (44.5) | 710 (20.6) | < 0.001 |
| 5%-10%, n (%) | 1380 (41.0) | 1501 (43.5) | < 0.001 |
| > 10%, n (%) | 488 (14.5) | 1237 (35.9) | < 0.001 |
| Gensini score | 2 (0, 5) | 26 (16, 45) | < 0.001 |
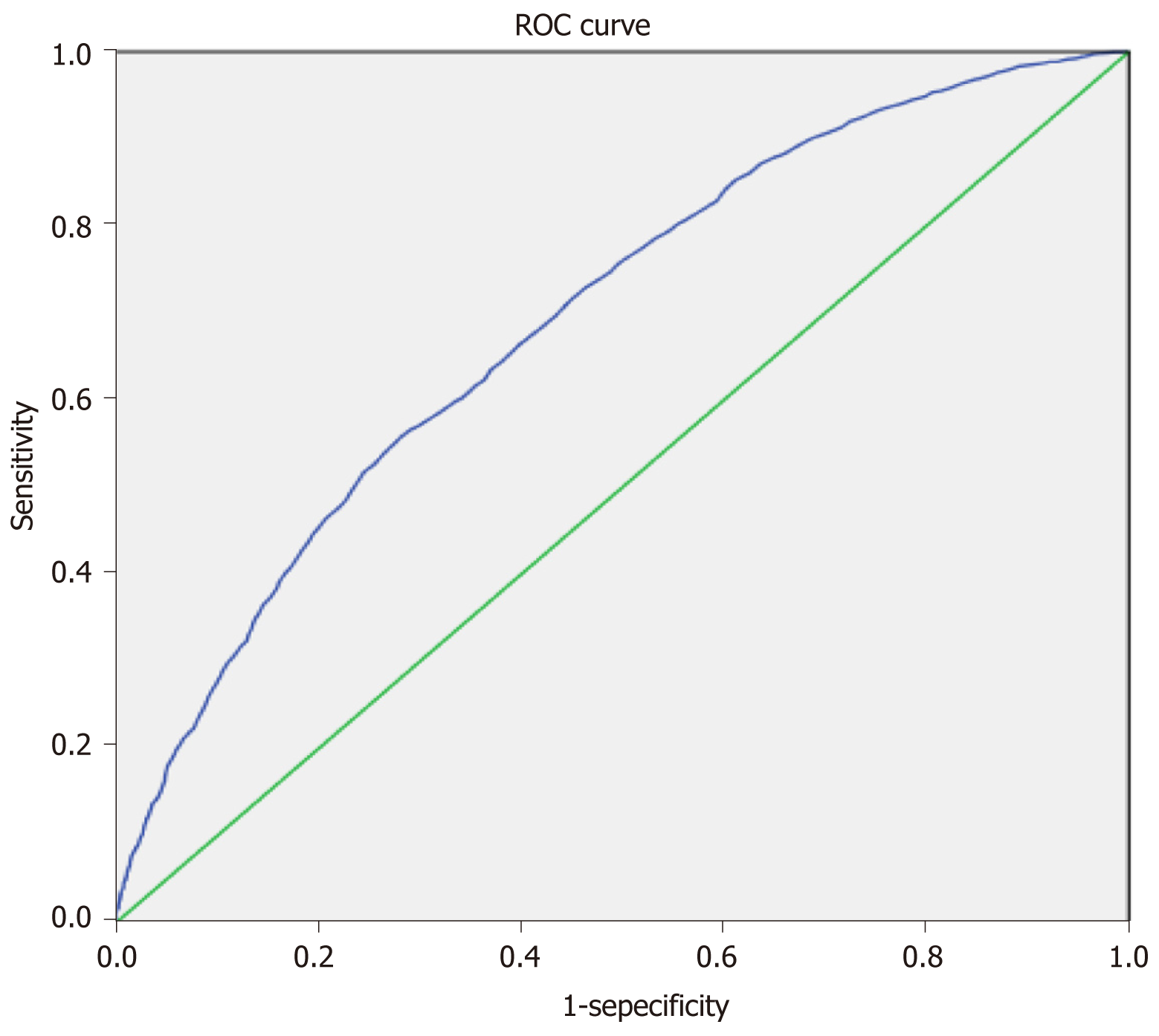
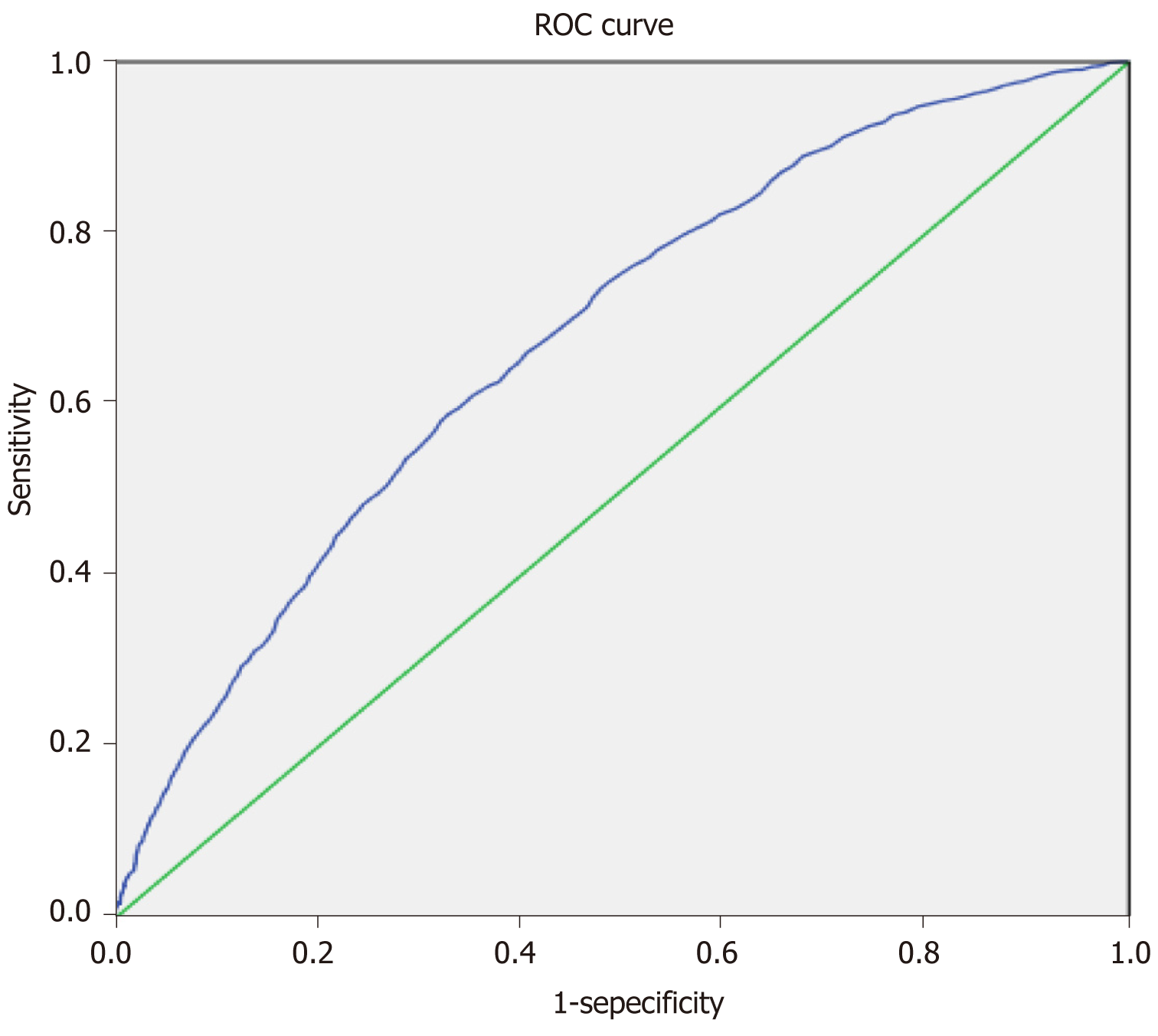
The relationship between China-PAR and GS was evaluated using correlation and regression analyses in the whole group. Correlation analysis showed that China-PAR was significantly correlated with GS (r = 0.266, P < 0.001). Logistic or linear regression analysis further confirmed that China-PAR score was correlated with the presence and severity of CAD (β = 0.072, P < 0.001; β = 0.081, P < 0.001, respectively). ROC curve analysis was performed subsequently. The cut-off value of China-PAR for predicting the presence of CAD was 7.55% with a sensitivity of 55.8% and specificity of 71.8% [area under the curve (AUC) = 0.693, 95% confidence interval: 0.681 to 0.706, P < 0.001] (Figure 2). For prediction of severe CAD, the CAD group was classified into two groups by GS, and the cut-off value was 7.45%, with a sensitivity of 58.8% and specificity of 67.2% (AUC = 0.680, 95% confidence interval: 0.665 to 0.694, P < 0.001) (Figure 3).
The major finding of the present study was that the China-PAR risk stratification scoring system may predict both the presence and severity of CAD.
During the past decades, ischemic heart disease has become the major cause of death in China[3]. The development and progression of CAD are often insidious and slow under the influence of multiple risk factors. More than 90% of the patients developing CAD have at least one cardiovascular risk factor[10], and some risk factors can be modified by lifestyle changes and medical treatment. Therefore, assessing the risk of developing CAD is of great importance in terms of primary prevention. Numerous risk prediction tools have been developed to assess the individual risk of developing CAD[11]. However, most of them are derived primarily from Western populations and might not be suitable for direct application in the Chinese population. The China-PAR project is the first study to develop and validate 10-year risk prediction equations for ASCVD using data from four contemporary Chinese cohorts[8]. It has been preliminarily confirmed that China-PAR outperformed the PCEs in 5-year ASCVD risk prediction in the Chinese population[12].
Despite the availability of many validated risk prediction models, to date, insufficient date is available regarding the best method to predict the CAD presence and severity. In a study including 1296 patients with stable chest pain who underwent cardiac computed tomographic angiography (CTA), Versteylen et al[13] found that the ability of the FRS and SCORE risk scoring systems to predict CAD was similar but superior to that of Prospective Cardiovascular Münster and the Diamond Forrester risk classification system[13]. Another CTA study assessing risk scores in patients with rheumatoid arthritis demonstrated that patients with coronary calcification trend to have a higher FRS compared to those without[14]. Additionally, in a small Turkish population who underwent CAG, Sayin et al[15] also found that the FRS could be used for prediction of CAD severity[15]. Another documented study suggested that the CHADS2, CHA2DS2-VASc, and especially CHA2DS2-VASc-HS scores could be considered predictive of the risk of severe CAD[16].
China-PAR equations incorporated multiple major risk factors based on the Chinese population. We believed that they could also be used to predict CAD severity. Our study verified the hypothesis in some degree, providing a cost-effective method in CAD identification. However, the predictive power of China-PAR scoring system may need to be improved by integrating other variables in the future research. Since the burden of cardiovascular morbidity and mortality is disproportionately higher in China compared to developed countries, misclassification of a high-risk patient at the crucial stage may cause unacceptable consequences.
There are several limitations in our study. First, this study is based on patients who were admitted for diagnostic CAG and most patients were from a southern Chinese city. Thus, it would not reflect the general Chinese population. Second, the GS system has its own limitation, and it could not reflect the actual clinical severity of the coronary artery lesion. Furthermore, this is a single-center cross-sectional design study, and our results need a multicenter study to confirm.
China-PAR scoring system was discovered to be applicable in the estimation of both the presence and severity of CAD in addition to their role in predicting cardiovascular events.
A practical and reliable prediction scoring system for coronary artery disease (CAD) risk and severity evaluation is lacking.
Very few researchers have focused on the validity of the risk score models in predicting the severity of CAD.
To evaluate the utility of the prediction for atherosclerotic cardiovascular disease risk in China (China-PAR) scoring system in assessing the severity of CAD in the Chinese population.
The China-PAR score and Gensini score (GS) were calculated for each enrolled patient. Thereafter, correlation analysis and receiver operating characteristic curve analysis were performed.
The China-PAR score was positively associated with the GS.
The China-PAR scoring system is applicable in the estimation of both the presence and severity of coronary artery disease.
A multicenter prospective study should be performed to further confirm the utility of the China-PAR score in assessing the severity of CAD in the Chinese population.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Schoenhagen P, Ueda H S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5495] [Cited by in RCA: 5223] [Article Influence: 522.3] [Reference Citation Analysis (0)] |
| 2. | Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, Li Y, Liu Y, Yin P, Liu J, Yu S, Tan F, Barber RM, Coates MM, Dicker D, Fraser M, González-Medina D, Hamavid H, Hao Y, Hu G, Jiang G, Kan H, Lopez AD, Phillips MR, She J, Vos T, Wan X, Xu G, Yan LL, Yu C, Zhao Y, Zheng Y, Zou X, Naghavi M, Wang Y, Murray CJ, Yang G, Liang X. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 875] [Cited by in RCA: 1015] [Article Influence: 112.8] [Reference Citation Analysis (0)] |
| 3. | Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, Wan X, Yu S, Jiang Y, Naghavi M, Vos T, Wang H, Lopez AD, Murray CJ. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987-2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1375] [Cited by in RCA: 1433] [Article Influence: 119.4] [Reference Citation Analysis (0)] |
| 4. | D'Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4272] [Cited by in RCA: 5233] [Article Influence: 307.8] [Reference Citation Analysis (0)] |
| 5. | Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, Njølstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM; SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3471] [Cited by in RCA: 3580] [Article Influence: 162.7] [Reference Citation Analysis (0)] |
| 6. | Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ. 2007;335:136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 626] [Cited by in RCA: 657] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 7. | Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1958] [Cited by in RCA: 2582] [Article Influence: 234.7] [Reference Citation Analysis (0)] |
| 8. | Yang X, Li J, Hu D, Chen J, Li Y, Huang J, Liu X, Liu F, Cao J, Shen C, Yu L, Lu F, Wu X, Zhao L, Gu D. Predicting the 10-Year Risks of Atherosclerotic Cardiovascular Disease in Chinese Population: The China-PAR Project (Prediction for ASCVD Risk in China). Circulation. 2016;134:1430-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 421] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 9. | Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1273] [Cited by in RCA: 1499] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 10. | Ford ES, Giles WH, Mokdad AH. The distribution of 10-Year risk for coronary heart disease among US adults: findings from the National Health and Nutrition Examination Survey III. J Am Coll Cardiol. 2004;43:1791-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 235] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 11. | Zhao D, Liu J, Xie W, Qi Y. Cardiovascular risk assessment: a global perspective. Nat Rev Cardiol. 2015;12:301-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 12. | Tang X, Zhang D, He L, Wu N, Si Y, Cao Y, Huang S, Li N, Li J, Dou H, Gao P, Hu Y. Performance of atherosclerotic cardiovascular risk prediction models in a rural Northern Chinese population: Results from the Fangshan Cohort Study. Am Heart J. 2019;211:34-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Versteylen MO, Joosen IA, Shaw LJ, Narula J, Hofstra L. Comparison of Framingham, PROCAM, SCORE, and Diamond Forrester to predict coronary atherosclerosis and cardiovascular events. J Nucl Cardiol. 2011;18:904-911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Chung CP, Oeser A, Avalos I, Gebretsadik T, Shintani A, Raggi P, Sokka T, Pincus T, Stein CM. Utility of the Framingham risk score to predict the presence of coronary atherosclerosis in patients with rheumatoid arthritis. Arthritis Res Ther. 2006;8:R186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Sayin MR, Cetiner MA, Karabag T, Akpinar I, Sayin E, Kurcer MA, Dogan SM, Aydin M. Framingham risk score and severity of coronary artery disease. Herz. 2014;39:638-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Cetin M, Cakici M, Zencir C, Tasolar H, Baysal E, Balli M, Akturk E. Prediction of coronary artery disease severity using CHADS2 and CHA2DS2-VASc scores and a newly defined CHA2DS2-VASc-HS score. Am J Cardiol. 2014;113:950-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |