Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5339
Peer-review started: March 8, 2021
First decision: March 25, 2021
Revised: March 29, 2021
Accepted: April 25, 2021
Article in press: April 25, 2021
Published online: July 6, 2021
Processing time: 108 Days and 1.4 Hours
Secondary jejunal tumor from renal cell carcinoma (RCC) is extremely rare in clinical practice and is easily missed and misdiagnosed because of the low incidence and atypical symptoms.
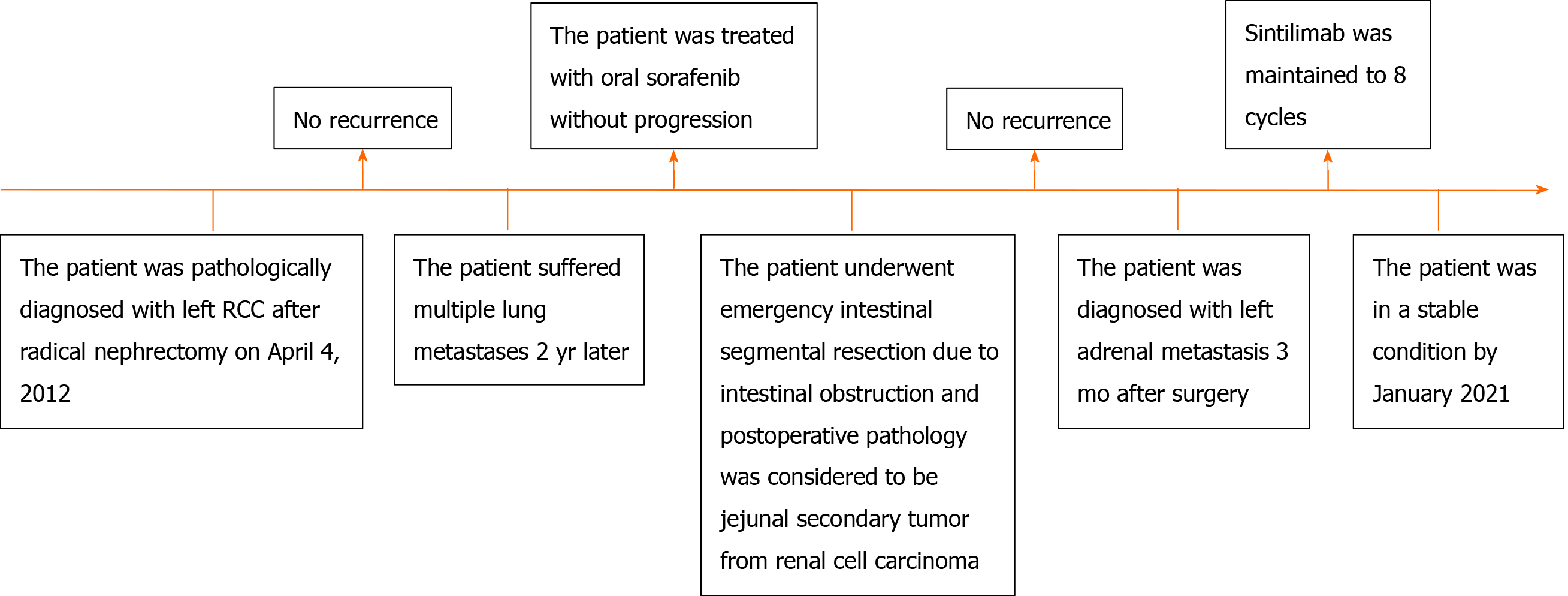
A 38-year-old male patient was diagnosed pathologically with left RCC after radical nephrectomy in 2012. The patient then suffered multiple lung metastases 2 years later and was treated with oral sorafenib without progression for 6 years. In 2020, an emergency intestinal segmental resection due to intestinal obstruction was required, and postoperative pathology confirmed a jejunal secondary tumor from RCC. The patient had a smooth recovery following surgery. Three months after surgery, the patient was diagnosed with left adrenal metastasis, and subsequent sintilimab therapy has stabilized his condition.
This report is written to remind urologists and pathologists of the potential for small intestinal secondary tumors when a patient with a history of RCC seeks treatment for digestive symptoms. Enteroscopy and abdominal contrast-enhanced computed tomography are essential means of examination, but severe cases require immediate surgical intervention despite the lack of a preoperative examination to distinguish tumor attributes.
Core Tip: Jejunal secondary tumor from renal cell carcinoma (RCC) is extremely rare. Herein, we present a case of small bowel obstruction caused by a jejunal secondary tumor from RCC. A male patient who underwent a left radical nephrectomy for RCC before visited the hospital with intestinal obstruction symptoms. Emergency intestinal segmental resection was performed, and postoperative pathology confirmed a jejunal secondary tumor from RCC. This report is written to remind urologists and patho
- Citation: Bai GC, Mi Y, Song Y, Hao JR, He ZS, Jin J. Small bowel obstruction caused by secondary jejunal tumor from renal cell carcinoma: A case report. World J Clin Cases 2021; 9(19): 5339-5344
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5339.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5339
Renal tumors are one of the most common tumors of the urinary system. Approximately 85% of renal tumors are renal cell carcinoma (RCC), and approximately 70% are clear cell histology[1]. Although the diagnosis and treatment of RCC are progressing rapidly, approximately 15% of RCC patients were diagnosed with metastases at the first visit[2], and approximately 20%-30% with localized RCC will experience recurrence after radical or partial nephrectomy[3]. Small intestinal secon
On March 8, 2020, a 38-year-old male patient presented to the emergency department with a 20-d history of reduced aerofluxus and defecation, accompanied by intermittent vomiting and abdominal colic.
The patient visited the hospital on July 30, 2012, presenting with a left renal tumor found via abdominal ultrasonography and computed tomography (CT). Laparoscopic radical nephrectomy was performed on August 4, 2012, and the postoperative pathology suggested a renal clear cell carcinoma measuring 6.0 cm × 6.0 cm × 5.5 cm (PT1b). The patient was diagnosed with pulmonary metastasis 2 years later through positron emission tomography-CT (PET-CT) and subsequently treated with oral sorafenib for 6 years without metastatic progression.
The patient had no special personal and family history.
Physical examination revealed a surgical scar on the left waist, abdominal distension, and severe abdominal tenderness around the umbilicus with mild rebound tenderness. The liver and spleen were impalpable.
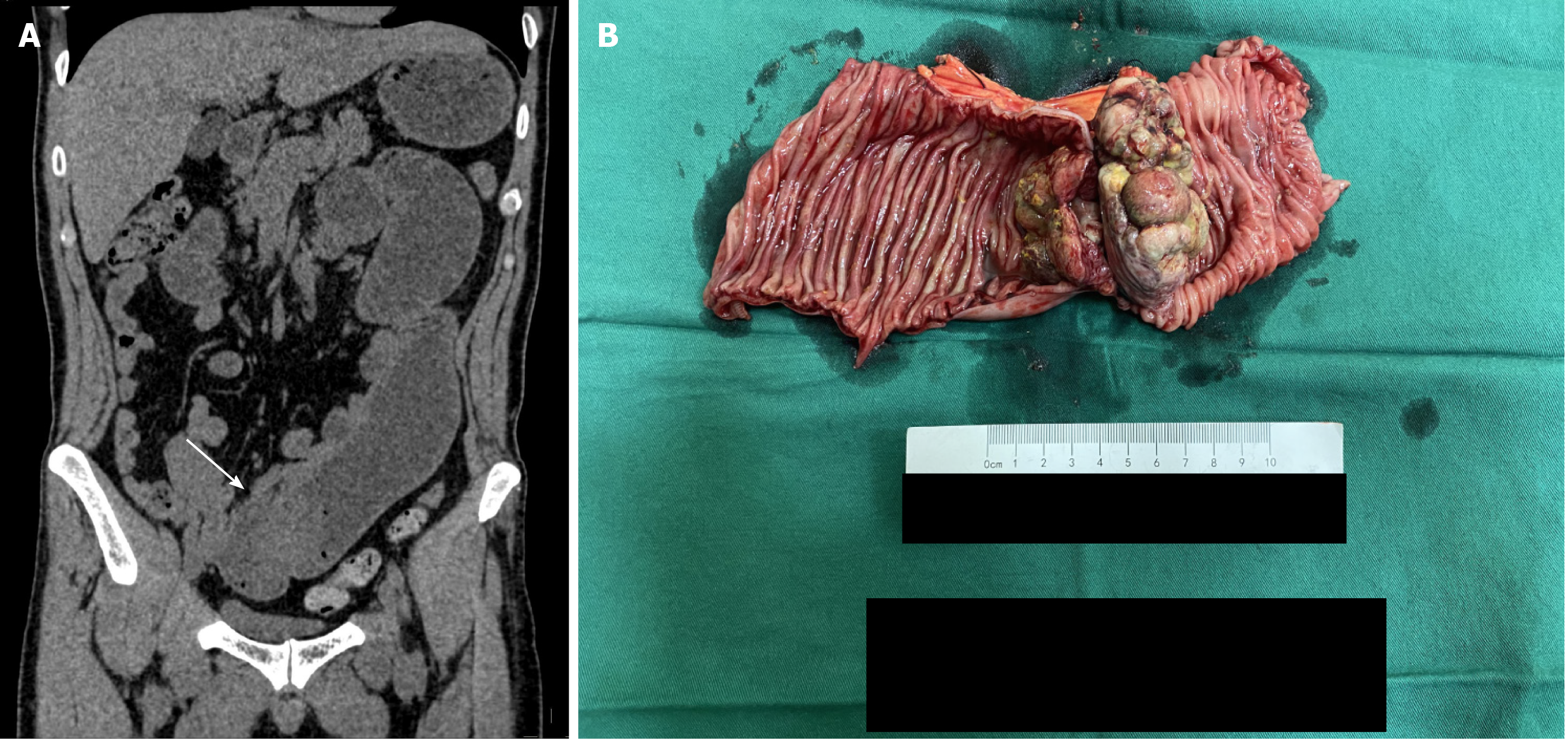
Abdominal CT revealed small intestinal obstruction caused by a large irregular mass in the jejunum lumen (Figure 1A). There was no time for further examinations such as enteroscopy and abdominal contrast-enhanced CT.
The diagnosis was confirmed as small bowel obstruction due to a jejunal secondary tumor from RCC.
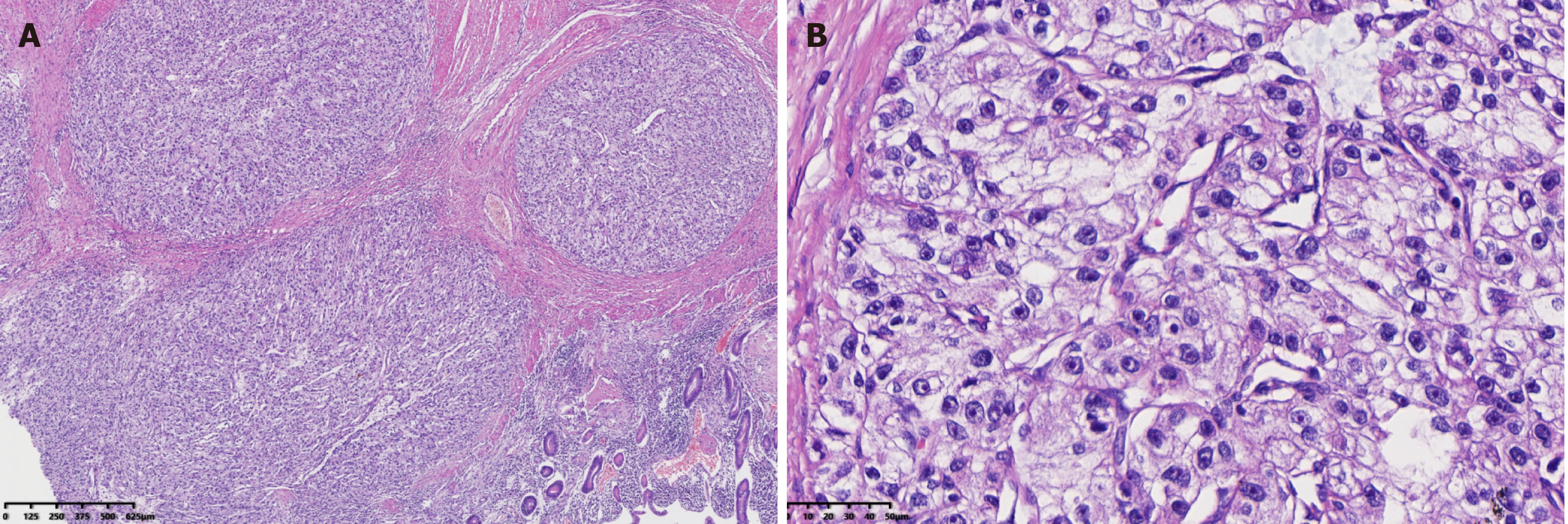
Emergency segmental resection and end-to-end anastomosis of the small intestine were performed. The postoperative specimen was a cauliflower-like broad-based crunchy lesion measuring 6.5 cm × 5 cm × 5 cm (Figure 1B). The results of the histologic examination were consistent with metastatic renal clear cell carcinoma. The lesion presented as masses of clear tumor cells with small nuclei and abundant cytoplasm surrounded by a net-like fibrovascular stroma (Figure 2A and B). The patient had a smooth recovery following surgery.
Three months after the small intestine surgery, PET-CT showed left adrenal metastasis from RCC (Figure 3). Then sintilimab (200 mg, every 21 d) was given to control the disease progression. The therapy was continued for eight cycles, and the patient was in a stable condition by January 2021.
Metachronous metastasis of RCC to the small intestine is a distinctly rare occurrence and is complicated by concomitant lung metastases and subsequent adrenal metastasis[5]. In a retrospective analysis of 44 small intestinal secondary tumors, colon cancer was the most common primary tumor (43.2%), followed by pancreatic and ovarian cancer (11.4% each). RCC accounted for only two in the study (4.5%)[6]. Furthermore, an autopsy report showed that in all 687 cases confirmed as RCC by histology, only two cases were found to have small intestinal metastases, accounting for 0.5% of the 392 metastatic cases[7].
In 15 patients with small intestinal metastases secondary to renal cancer, as summarized by Mueller et al[8], 5 patients presented with gastrointestinal bleeding, 5 with intussusception, 2 with small bowel obstruction, 1 with biliary obstruction, and 1 with both gastrointestinal bleeding and bowel obstruction. Therefore, for patients with a history of renal cancer, the possibility of small intestinal secondary tumors should be considered if the above symptoms are present. Either misdiagnosis or delayed treatment may endanger the health of the patients.
When seeing a patient with similar symptoms and a history of cancer, the disease's vital signs and severity should be assessed initially to determine the appropriate examination and treatment planning. Routine blood tests, liver function tests, bilirubin tests, stool occult blood tests, abdominal X-ray, especially enteroscopy, and abdominal contrast-enhanced CT are practical accessory examinations of diagnosing small bowel tumors and evaluating accompanying symptoms. Serum creatinine tests and other renal function evaluations are also indispensable for the operation history of primary renal tumor[9]. If the situation permits, a full-body imaging examination should be performed to exclude other possible metastatic lesions. In this case, preoperative diagnosis, which is essential for small bowel tumors, was not complete due to difficulty in applying enteroscopy and abdominal contrast-enhanced CT under emergency conditions.
Metastatic small bowel tumors should be differentiated from other malignant lesions such as adenocarcinoma, carcinoid, and lymphoma, the three most common cancers in the small intestine[10]. Valuable information for differential diagnosis can be obtained by examining the morphological features of the lesion via imaging. Small intestinal adenocarcinoma classically presents with a short annular stricture. Carcinoid tends to infiltrate the mesentery, causing angulation, kinking, rigidity, and separation of small bowel loops. Lymphoma always presents as a non-obstructive lesion with wall thickening combined with lymphadenopathy and systematic symptoms[11,12]. Metastatic cancers in the small bowel are usually large[13] and should be considered when the patient has a history of malignancy.
Since renal carcinoma is insensitive to chemotherapy and radiotherapy, resection of metastatic lesions is feasible and effective in patients with a previous nephr
This case study has been presented to remind urologists and pathologists of the possibility of small intestinal secondary tumors when a patient with a history of RCC presents with digestive symptoms. Enteroscopy and abdominal contrast-enhanced CT are essential means of examination, but severe cases require immediate surgical intervention despite the lack of a preoperative examination to distinguish tumor attributes.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Balducci G, Yang RM S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Motzer RJ, Jonasch E, Michaelson MD, Nandagopal L, Gore JL, George S, Alva A, Haas N, Harrison MR, Plimack ER, Sosman J, Agarwal N, Bhayani S, Choueiri TK, Costello BA, Derweesh IH, Gallagher TH, Hancock SL, Kyriakopoulos C, LaGrange C, Lam ET, Lau C, Lewis B, Manley B, McCreery B, McDonald A, Mortazavi A, Pierorazio PM, Ponsky L, Redman BG, Somer B, Wile G, Dwyer MA; CGC; Hammond LJ, Zuccarino-Catania G. NCCN Guidelines Insights: Kidney Cancer, Version 2.2020. J Natl Compr Canc Netw. 2019;17:1278-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 171] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 2. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13300] [Cited by in RCA: 15475] [Article Influence: 2579.2] [Reference Citation Analysis (2)] |
| 3. | Williamson TJ, Pearson JR, Ischia J, Bolton DM, Lawrentschuk N. Guideline of guidelines: follow-up after nephrectomy for renal cell carcinoma. BJU Int. 2016;117:555-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Smith SJ, Carlson HC, Gisvold JJ. Secondary neoplasms of the small bowel. Radiology. 1977;125:29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Nozawa H, Tsuchiya M, Kobayashi T, Morita H, Kobayashi I, Sakaguchi M, Mizutani T, Tajima A, Kishida Y, Yakumaru K, Kagami H, Sekikawa T. Small intestinal metastasis from renal cell carcinoma exhibiting rare findings. Int J Clin Pract. 2003;57:329-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Minardi AJ Jr, Zibari GB, Aultman DF, McMillan RW, McDonald JC. Small-bowel tumors. J Am Coll Surg. 1998;186:664-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 73] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Weiss L, Harlos JP, Torhorst J, Gunthard B, Hartveit F, Svendsen E, Huang WL, Grundmann E, Eder M, Zwicknagl M. Metastatic patterns of renal carcinoma: an analysis of 687 necropsies. J Cancer Res Clin Oncol. 1988;114:605-612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 86] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Mueller JL, Guyer RA, Adler JT, Mullen JT. Metastatic renal cell carcinoma to the small bowel: three cases of GI bleeding and a literature review. CEN Case Rep. 2018;7:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Wang Z, Wang G, Xia Q, Shang Z, Yu X, Wang M, Jin X. Partial nephrectomy vs. radical nephrectomy for renal tumors: A meta-analysis of renal function and cardiovascular outcomes. Urol Oncol 2016; 34: 533.e11-533. e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Hatzaras I, Palesty JA, Abir F, Sullivan P, Kozol RA, Dudrick SJ, Longo WE. Small-bowel tumors: epidemiologic and clinical characteristics of 1260 cases from the connecticut tumor registry. Arch Surg. 2007;142:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 141] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 11. | Yang CB, Yu N, Jian YJ, Yu Y, Duan HF, Zhang XR, Ma GM, Guo Y, Duan X. Spectral CT Imaging in the Differential Diagnosis of Small Bowel Adenocarcinoma From Primary Small Intestinal Lymphoma. Acad Radiol. 2019;26:878-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Laurent F, Drouillard J, Lecesne R, Bruneton JN. CT of small-bowel neoplasms. Semin Ultrasound CT MR. 1995;16:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | STARR A, MILLER GM. Solitary jejunal metastasis twenty years after removal of a renal-cell carcinoma; report of a case. N Engl J Med. 1952;246:250-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Barata PC, Rini BI. Treatment of renal cell carcinoma: Current status and future directions. CA Cancer J Clin. 2017;67:507-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 607] [Article Influence: 75.9] [Reference Citation Analysis (0)] |
| 15. | Alt AL, Boorjian SA, Lohse CM, Costello BA, Leibovich BC, Blute ML. Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer. 2011;117:2873-2882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 308] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 16. | Azagury D, Liu RC, Morgan A, Spain DA. Small bowel obstruction: A practical step-by-step evidence-based approach to evaluation, decision making, and management. J Trauma Acute Care Surg. 2015;79:661-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Urbano J, Manuel Cabrera J, Franco A, Alonso-Burgos A. Selective arterial embolization with ethylene-vinyl alcohol copolymer for control of massive lower gastrointestinal bleeding: feasibility and initial experience. J Vasc Interv Radiol. 2014;25:839-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Ljungberg B, Albiges L, Abu-Ghanem Y, Bensalah K, Dabestani S, Fernández-Pello S, Giles RH, Hofmann F, Hora M, Kuczyk MA, Kuusk T, Lam TB, Marconi L, Merseburger AS, Powles T, Staehler M, Tahbaz R, Volpe A, Bex A. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2019 Update. Eur Urol. 2019;75:799-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 934] [Article Influence: 155.7] [Reference Citation Analysis (0)] |