Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5332
Peer-review started: February 28, 2021
First decision: April 14, 2021
Revised: April 22, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 6, 2021
Processing time: 116 Days and 3 Hours
Ectopic opening of the common bile duct is a condition with low incidence. Patients with an ectopic common bile duct opening have a high incidence of common bile duct stones and acute cholangitis. Patients with atypical symptoms and imaging findings are easily misdiagnosed; moreover, it is difficult to retrieve stones by endoscopic retrograde cholangiopancreatography, and common bile duct stones are prone to postsurgical recurrence.
A 45-year-old male patient presented with “intermittent upper abdominal pain and elevated liver enzymes for 1 wk”. Transabdominal ultrasound indicated dilation of the common bile duct and the presence of stones. Magnetic resonance imaging showed that the common bile duct was dilated with stones and that its opening was ectopic. Endoscopic retrograde cholangiopancreatography revealed an abnormal opening of the common bile duct into the duodenal bulb and the presence of common bile duct stones. Laparoscopic extrahepatic choledochectomy and hepatoenteric anastomosis were performed. After surgery, the patient recovered well and was discharged. The patient has been followed up for 2 years since the operation. He has not experienced stone recurrence, and his liver function and quality of life are good.
Improved understanding of ectopic opening of the common bile duct is needed for clinicians to provide patients with appropriate treatment.
Core Tip: Ectopic opening of the common bile duct into the duodenal bulb is very rare. Patients with an ectopic common bile duct opening have a high incidence of common bile duct stones and acute cholangitis. Furthermore, patients with atypical symptoms and imaging findings are easily misdiagnosed. This report describes a case of ectopic opening of the common bile duct into the duodenal bulb with recurrent choledocholithiasis. This report is expected to provide experience for the diagnosis and treatment of this condition by describing the clinical data of this patient with an ectopic opening of the common bile duct into the duodenal bulb.
- Citation: Xu H, Li X, Zhu KX, Zhou WC. Ectopic opening of the common bile duct into the duodenal bulb with recurrent choledocholithiasis: A case report. World J Clin Cases 2021; 9(19): 5332-5338
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5332.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5332
The ends of the normal pancreatic duct and the common bile duct open together through the duodenal papilla into the dorsal medial wall of the middle descending part of the duodenum, and an opening into the middle portion of the nondescending segment is considered an ectopic opening. Studies have shown that the incidence of ectopic bile duct opening is 2%-23%, including openings into the stomach, pyloric duct, and duodenum; openings into the duodenum are more common in the lower corner or horizontal part of the duodenum. An opening in the duodenal bulb is a very rare location[1-6]. Due to the lack of specificity of the clinical manifestations of ectopic opening of the common bile duct into the duodenal bulb, lack of understanding by clinicians, and drawbacks of imaging examinations such as computed tomography, missed diagnosis or misdiagnosis of ectopic opening of the common bile duct often occurs[3,4]. Cases of ectopic opening of the common bile duct into the duodenal bulb are often found incidentally when patients undergo endoscopic retrograde cholangiopancreatography (ERCP) due to common bile duct stones or stenosis of the end of the common bile duct[2-6]. Here, we report a case of ectopic opening of the common bile duct into the duodenal bulb with recurrent choledocholithiasis. This report is expected to provide experience for the diagnosis and treatment of this disease through the clinical data of a patient with ectopic opening of the common bile duct into the duodenal bulb. The patient provided informed consent for publication of this case.
A 45-year-old man was admitted to the hospital with a chief complaint of intermittent upper abdominal pain and elevated liver enzymes for 1 wk.
Four years prior, the patient underwent cholecystectomy along with common bile duct exploration and stone removal at a local hospital for the treatment of gallbladder stones and common bile duct stones. One week prior, the patient had intermittent upper abdominal pain and discomfort. The local hospital found abnormal liver enzyme levels.
The patient denied a previous history of diseases such as hypertension or diabetes.
The patient denied a history of smoking, tuberculosis, or alcohol or drug use. No family members had similar diseases.
There was no overall yellowing of the skin and sclera. Mild tenderness was observed on deep palpation of the right upper abdomen. There was no rebound pain or muscle tension throughout the abdomen.
Laboratory examinations conducted after this admission showed the following: Alanine aminotransferase: 543 IU/L (normal: < 49 IU/L); aspartate aminotransferase: 213 IU/L (normal: < 49 IU/L); alkaline phosphatase: 194.9 IU/L (normal: < 125 IU/L); gamma glutamyl transpeptidase: 511.6 IU/L (normal: < 69 IU/L); direct bilirubin: 7.1 µmol/L (normal: < 6.8 µmol/L); indirect bilirubin: 19.3 µmol/L (normal: < 19 µmol/L); and carbohydrate antigen 19-9: 42.4 U/mL (normal: < 27 U/mL). Other laboratory tests were normal.
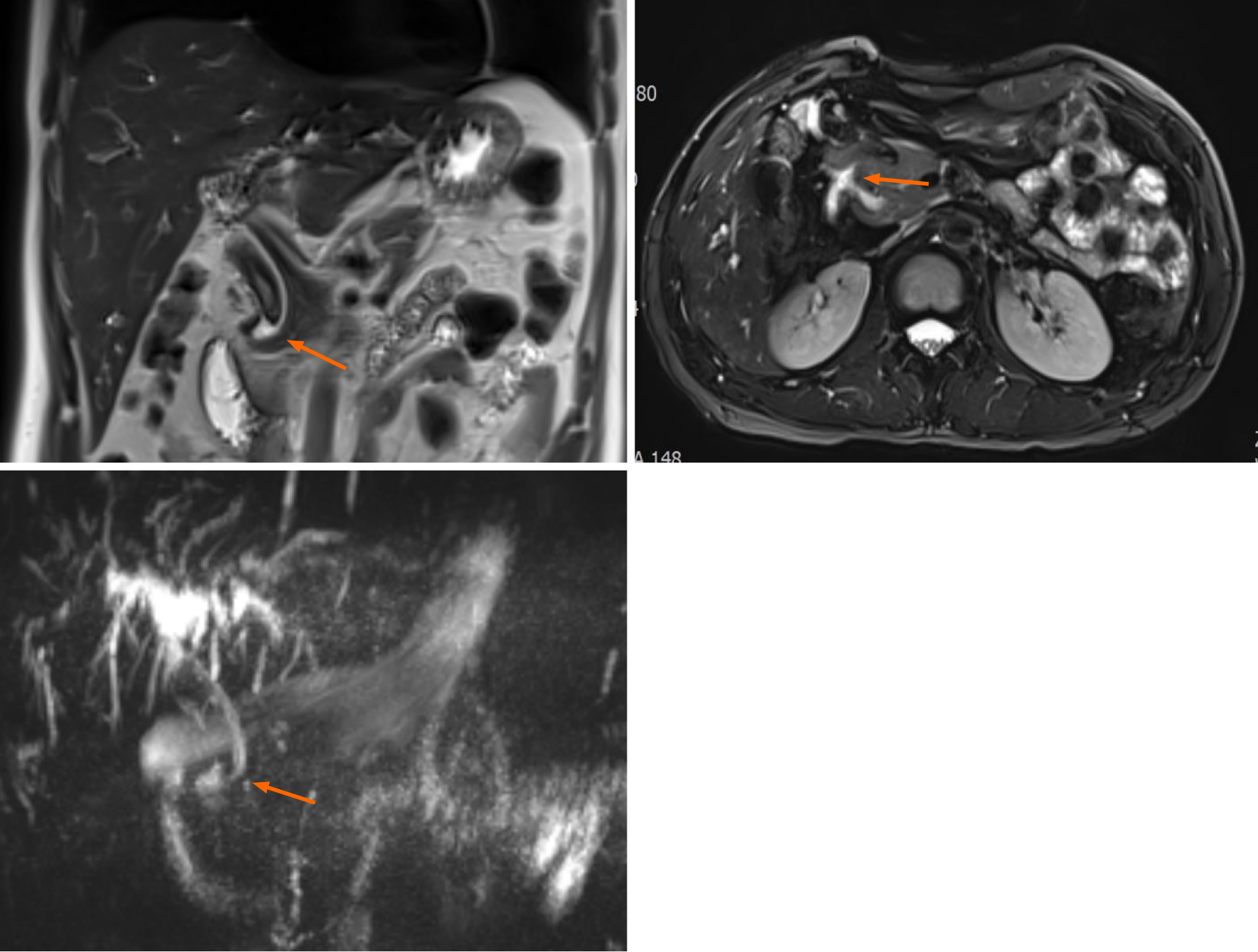
Transabdominal ultrasound indicated dilation of the common bile duct and the presence of stones. Magnetic resonance imaging showed that the common bile duct was dilated with stones, was severely angled, and did not merge normally with the pancreatic duct (Figure 1). ERCP revealed an abnormal opening of the common bile duct into the duodenal bulb and the presence of common bile duct stones (Figure 2).
Following the imaging and laboratory examinations, the diagnoses were common bile duct stones along with ectopic opening of the common bile duct and acute cholangitis.
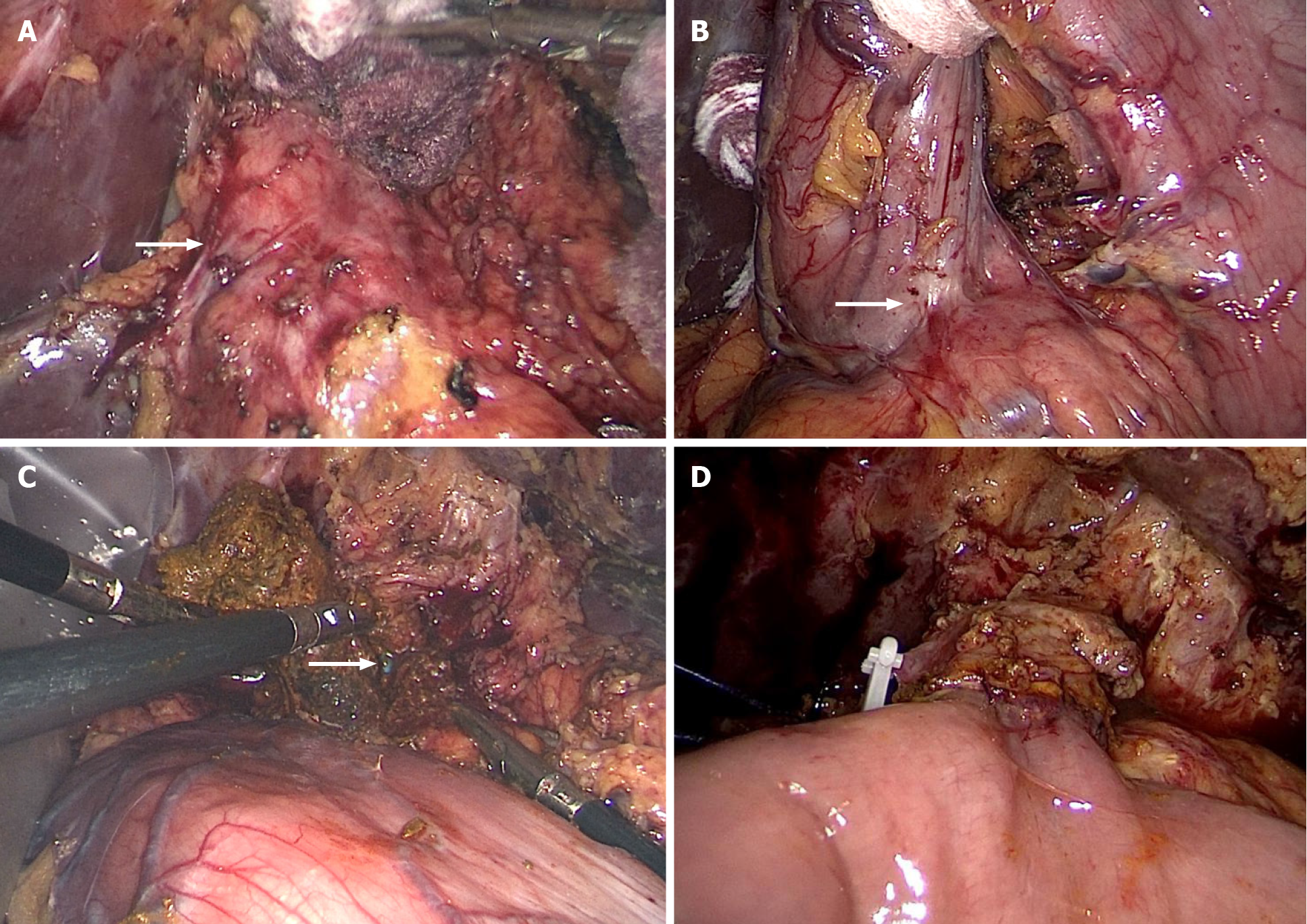
Considering the patient’s repeated episodes of common bile duct stones along with the ectopic opening of the common bile duct, recurrent abdominal pain and acute cholangitis, the common bile duct stones could not be completely resolved with ERCP. After communicating with the patient and family members, laparoscopic extrahepatic common bile duct resection and hepatoenteric anastomosis were performed (Figure 3).
After the operation, the patient recovered well and was discharged. The patient has been followed up for 2 years since the operation. He has not experienced stone recurrence, and his liver function and quality of life are good.
An ectopic opening of the common bile duct is more commonly located in the distal end of the descending duodenum and is rarely present in the duodenal bulb. The duodenal papilla is mostly located in the middle 1/3 of the descending segment of the duodenum (accounting for approximately 66% of cases), with 27% of cases in the lower 1/3 of the descending segment, and approximately 3% of cases in the upper 1/3 of the descending segment. Only 4% of cases are near the horizontal segment of the duodenum[7]. Sezgin et al[3] reported 11 cases of ectopic opening, of which 3 cases opened into the third segment of the duodenum. There is no consensus on the cause of ectopic opening of the common bile duct. Li et al[8] proposed that an ectopic distal hepatic diverticulum in the early embryonic stage can lead to abnormal fusion.
The clinical manifestations of an ectopic common bile duct opening are nonspecific and easily missed[8]. In recent years, magnetic resonance cholangiopancreatography has been used to identify a portion of the duodenal papilla and abnormal bile duct confluence. The advantages of this technique are noninvasiveness, a simple and safe operation, the absence of complications, and lack of pain in patients. It is not necessary to use contrast agents, but cases of missed diagnoses and misdiagnoses can occur. Ordinary gastroscopy, especially duodenoscopy, carefully conducted under endosco
ERCP treatment can be attempted for patients with an ectopic common bile duct opening and common bile duct stones. However, when the ectopic opening is in the duodenal bulb, local deformation and stenosis often occur, which are prone to cause bleeding and perforation. In addition, when ERCP examination or Oddi sphincterotomy is performed, because the opening is located at the level of the duodenum, it is difficult to locate the large papilla of the duodenum and perform intubation, which leads to failure of the operation[13,14].
At present, the problem of recurrent common bile duct stones after surgery has not been resolved. The recurrence of stones seriously affects the quality of life of patients, and elderly individuals experience more harm due to physical frailty and weakened immunity[15]. Some scholars[16] have shown that a common bile duct diameter ≥ 15 mm is a risk factor for stone recurrence after endoscopic stone removal. Bile duct dilatation can promote cholestasis and bacterial infection, which are potential risk factors for the recurrence of stones[15-17]. If chronic inflammation and fibrosis of the bile duct are present, the elasticity of the tube wall is lost, and even if the stone is removed, bile duct dilation will continue to exist. Bile duct stenosis can directly lead to cholestasis and easily formed stones. Under normal circumstances, the extrahepatic bile duct is only slightly curved and is similar to a straight line. Factors such as a history of biliary surgery can cause the bile duct to bend or even form an angle. An angle in the common bile duct can cause cholestasis and bile duct dilation. A smaller angle results in slower flow of bile, a longer bile-emptying time, and a higher concentration of bile. This in turn increases the cholesterol saturation in the bile, and the contraction of the bile duct decreases, making it impossible to exclude supersaturated bile, which easily causes stone recurrence[17-19]. Ectopic opening of the common bile duct will change the angulation of the common bile duct, which will increase the recurrence rate of bile duct stones and the incidence of acute cholangitis after surgery[20-22]. If the bile duct path is too long or too short and bile duct confluence abnormalities or congenital bile duct cysts are present, altered angulation of the bile duct may be related to a combined functional abnormality of the sphincter of Oddi.
Due to the existence of the duodenal papillary sphincter and the relative negative pressure in the duodenal cavity, it is difficult for digestive juice to flow back into the common bile duct under normal circumstances, and thus, the incidence of common bile duct stones and cholangitis is very low. In patients with an ectopic common bile duct, due to the lack of sphincter function and absence of negative pressure in the cavity, especially in the case of ectopic opening of the common bile duct into the duodenal bulb or near the gastric pylorus, high pressure in the stomach after eating can cause digestive juice and food residue to easily flow back into the common bile duct. This can cause recurrent cholangitis and the recurrence of common bile duct stones, resulting in uncomfortable symptoms. In the present case, cholangitis and common bile duct stones recurred. Laboratory tests showed abnormal liver enzyme and bilirubin levels. During ERCP, the common bile duct was incidentally found to have an ectopic opening into the duodenal bulb. The patient had undergone cholecystectomy and common bile duct exploration in the past, and common bile duct stones and acute cholangitis occurred again 4 years later, which was considered. In view of the anatomical variation associated with this condition, the fundamental solution is to perform extrahepatic bile duct resection and cholangioenterostomy to eliminate the structural basis of common bile duct stones.
Ectopic opening of the common bile duct is relatively rare in clinical practice; clinicians have insufficient experience in diagnosing and treating this anomaly, and it is easy to miss or misdiagnose. Therefore, it is necessary to raise awareness of this condition in clinical work. At the same time, for patients with difficult stone retrieval by ERCP, postoperative stone recurrence and recurrence of acute cholangitis, attention should be given to etiological treatment, such as controlling biliary tract infection, improving biliary motility, and removing biliary obstruction while removing stones. Treating both symptoms and root causes can effectively solve the problem of recurrence of stones after surgery.
We sincerely thank the ERCP Diagnosis and Treatment Center and the Department of Radiology in our hospital for providing information.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Cocca S, Contini S, Karakus OZ, Villarejo-Campos P S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Peng YC, Chow WK. Ectopic papilla of Vater in duodenum bulb: A hospital-based study. Medicine (Baltimore). 2019;98:e14642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Disibeyaz S, Parlak E, Cicek B, Cengiz C, Kuran SO, Oguz D, Güzel H, Sahin B. Anomalous opening of the common bile duct into the duodenal bulb: endoscopic treatment. BMC Gastroenterol. 2007;7:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Sezgin O, Altintaş E, Uçbilek E. Ectopic opening of the common bile duct into various sites of the upper digestive tract: a case series. Gastrointest Endosc. 2010;72:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Saritas U, Senol A, Ustundag Y. The clinical presentations of ectopic biliary drainage into duodenal bulbus and stomach with a thorough review of the current literature. BMC Gastroenterol. 2010;10:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Parlak E, Dişibeyaz S, Cengiz C, Ciçek B, Ozin Y, Kacar S, Saşmaz N, Sahin B. Ectopic opening of the common bile duct and duodenal stenosis: an overlooked association. BMC Gastroenterol. 2010;10:142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Hekimoglu K, Ustundag Y, Saritas U. Ectopic openings of the bilio-pancreatic ducts in the stomach in an elderly case presenting with choledocholithiasis and acute cholangitis. J Gastrointestin Liver Dis. 2008;17:238-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Han X, Li Z, Zhang W. The relative analysis between duodenal papilla ectope and pancreaticobiliary maljunction. Linchuang Fangshexue Zazhi. 2008;27:1050-1052. |
| 8. | Li L, Yamataka A, Wang YX, Wang DY, Wang K, Li ZX, Shimizu T, Yamashiro Y, Zhang JZ, Lane GJ, Miyano T. Anomalous pancreatic duct anatomy, ectopic distal location of the papilla of Vater and congenital biliary dilatation: a new developmental triad? Pediatr Surg Int. 2003;19:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Lu QL, Lin F, Duan HQ, Liu H. Clinical effects of endoscopic retrograde cholangiopancreatography on the treatment of acute biliary pancreatitis. Xiandai Yiyuan Zazhi. 2014;14:90-92. |
| 10. | Amano Y, Takahashi M, Oishi T, Kumazaki T. MR cholangiopancreatography of double common bile duct with ectopic drainage into stomach. J Comput Assist Tomogr. 2002;26:141-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Krstic M, Stimec B, Krstic R, Ugljesic M, Knezevic S, Jovanovic I. EUS diagnosis of ectopic opening of the common bile duct in the duodenal bulb: a case report. World J Gastroenterol. 2005;11:5068-5071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Muhammedoğlu B. Ectopic Opening of the Common Bile Duct into the Duodenal Bulb: Diagnosis and Therapeutic Management and Considerations for Timing of Surgery and Duration of Follow-up After Initial Endoscopic Retrograde Cholangiopancreatography. Surg Laparosc Endosc Percutan Tech. 2019;29:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Takikawa T, Kanno A, Masamune A, Hongo S, Yoshida N, Nakano E, Miura S, Hamada S, Kume K, Kikuta K, Hirota M, Shimosegawa T. Ectopic Opening of the Common Bile Duct Accompanied by Choledochocele and Pancreas Divisum. Intern Med. 2016;55:1097-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Hong J, Pan W, Zuo W, Wang A, Zhu L, Zhou X, Li G, Liu Z, Liu P, Zhen H, Zhu Y, Ma J, Yuan J, Shu X, Lu N, Chen Y. Efficacy and safety of therapeutic ERCP in patients with ectopic papilla of Vater. Medicine (Baltimore). 2020;99:e18536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Cheon YK, Lehman GA. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006;18:461-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Song ME, Chung MJ, Lee DJ, Oh TG, Park JY, Bang S, Park SW, Song SY, Chung JB. Cholecystectomy for Prevention of Recurrence after Endoscopic Clearance of Bile Duct Stones in Korea. Yonsei Med J. 2016;57:132-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Seo DB, Bang BW, Jeong S, Lee DH, Park SG, Jeon YS, Lee JI, Lee JW. Does the bile duct angulation affect recurrence of choledocholithiasis? World J Gastroenterol. 2011;17:4118-4123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Wu LY, Wang SH, Jia GF, Zhu LS, Ling MD, Wang XX, Shan H. Risk factors for recurrent common bile duct stones after endoscopic sphincterotomy. Zhonghua Xiaohuabing Yu Yingxiang Zazhi. 2015;5:5-9. |
| 19. | Strnad P, von Figura G, Gruss R, Jareis KM, Stiehl A, Kulaksiz H. Oblique bile duct predisposes to the recurrence of bile duct stones. PLoS One. 2013;8:e54601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Zeng AX, Liu BY, Zeng DH. Relationship between duodenal papilla ectopic and recurrent bile duct stones postoperative. Xiandai Yiyuan Zazhi. 2015;32-33. |
| 21. | Lee SS, Kim MH, Lee SK, Kim KP, Kim HJ, Bae JS, Seo DW, Ha HK, Kim JS, Kim CD, Chung JP, Min YI. Ectopic opening of the common bile duct in the duodenal bulb: clinical implications. Gastrointest Endosc. 2003;57:679-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Taş A, Kara B, Ölmez S, Yalçın MS, Öztürk NA, Saritas B. Retrospective analysis of cases with an ectopic opening of the common bile duct into duodenal bulb. Adv Clin Exp Med. 2018;27:1361-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |