Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5259
Peer-review started: February 8, 2021
First decision: March 28, 2021
Revised: April 9, 2021
Accepted: May 8, 2021
Article in press: May 8, 2021
Published online: July 6, 2021
Processing time: 135 Days and 8.5 Hours
Gastrointestinal xanthomas are asymptomatic and infrequent non-neoplastic lesions that commonly occur in the stomach with Helicobacter pylori-associated gastritis and rarely in the esophagus. To date, there have been no reports of esophageal xanthoma combined with esophageal cancer. Herein, we present the first case in the literature of a diffuse xanthoma complicated with early esoph
A 68-year-old man visited our department with a 2-mo history of epigastric discomfort. He underwent surgery for gastric cancer 6 years ago. Esophagogastroduodenoscopy showed a semi-circumferential irregular yellowish-colored and granular lesion in the esophagus (30-35 cm from the incisors). Using magnifying endoscopy with narrow band imaging, aggregated minute and yellowish-colored spots with tortuous microvessels on the surface were observed, and background coloration was clearly seen in the lesion. As endoscopic biopsy suggested a histologically high-grade dysplasia; the lesion was completely resected en bloc by endoscopic submucosal dissection (ESD). The resected specimen was confirmed to be a squamous cell carcinoma in situ with extensive foamy cells in the superficial mucosal layer. Immunohistochemically, the observed foamy cells were strongly positive for CD68, which is characteristic of xanthoma. The clinical course was favorable, and no recurrence was observed 2 years and 7 mo after ESD.
Diffuse xanthoma concurrent with early esophageal cancer is extremely rare. The characteristic endoscopic features may assist endoscopists in diagnosing similar lesions.
Core Tip: Esophageal xanthomas are uncommon, non-neoplastic lesions characterized by the accumulation of foamy histiocytes. Herein, we present the first case of early esophageal cancer covered by xanthomas, diffusely and superficially treated by endoscopic submucosal dissection. Knowing these characteristic endoscopic features can help endoscopists reach a correct diagnosis for appropriate treatment.
- Citation: Yang XY, Fu KI, Chen YP, Chen ZW, Ding J. Diffuse xanthoma in early esophageal cancer: A case report. World J Clin Cases 2021; 9(19): 5259-5265
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5259.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5259
Xanthomas are considered to be asymptomatic, non-neoplastic lesions that can be found anywhere along the gastrointestinal tract, commonly in the stomach and colon, and rarely in the esophagus. Endoscopically, they are small (1-2 mm in size), single or multiple, yellow, orange, or white well-demarcated sessile macules with irregular outlines that rarely exceed 5 mm[1,2]. Diffuse xanthoma complicated by early esophageal cancer has never been reported in the literature. We herein present the first case treated by endoscopic submucosal dissection (ESD).
A 68-year-old man was admitted with a 2-mo history of epigastric discomfort.
The patient presented with a complaint of intermittent, dull, and non-radiating epigastric pain. No associated nausea, vomiting, melena, or loss of body mass was observed.
The patient underwent distal gastrectomy for gastric cancer 6 years ago. Histological analysis revealed a moderately poorly differentiated adenocarcinoma, staged at pT4aN2M0 IIIB. The patient recovered well after adjuvant chemotherapy, and he was followed regularly. No evidence of local recurrence or distant metastasis was identified 6 years after surgery. His history included hypertension and type 2 diabetes mellitus controlled with medications for more than 10 years.
The patient reported consuming alcohol daily and smoking one pack of cigarettes per day for 42 years until he was 60 years old. His family history was negative for cancers.
The patient’s temperature was 36.5 °C, heart rate was 63 bpm, respiratory rate was 18 breaths per minute, and blood pressure was 141/93 mmHg. The physical examination was unremarkable.
The laboratory work-up showed that the levels of the tumor markers CA19-9, CA-125, carcinoembryonic antigen, squamous cell carcinoma antigen, and alpha-fetoprotein were in the normal range. Other biochemistry test results were also within normal limits.
Abdominal computed tomography revealed postoperative changes. Chest computed tomography and cardiac ultrasound were normal. No nodal involvement or distant metastasis was identified.
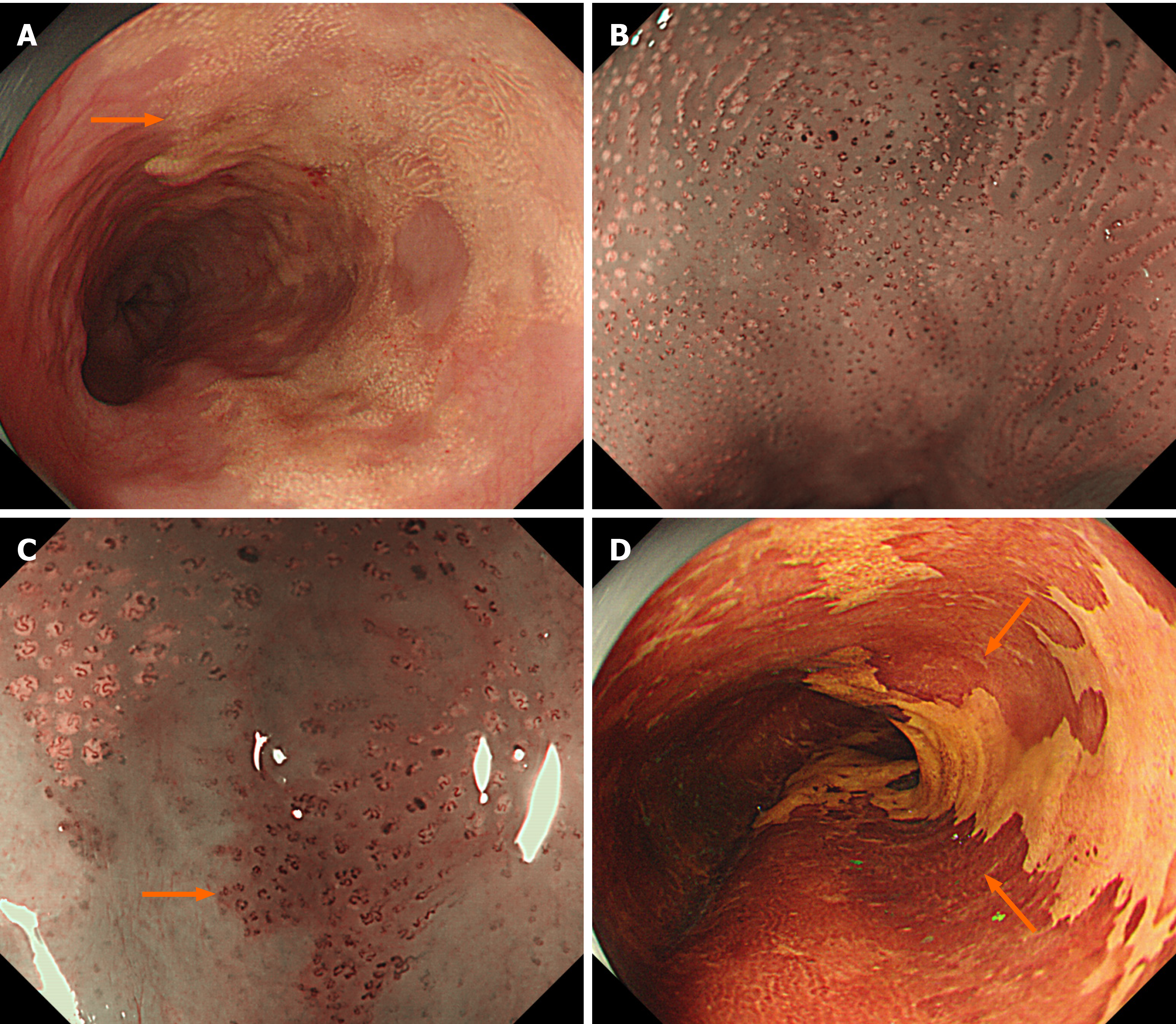
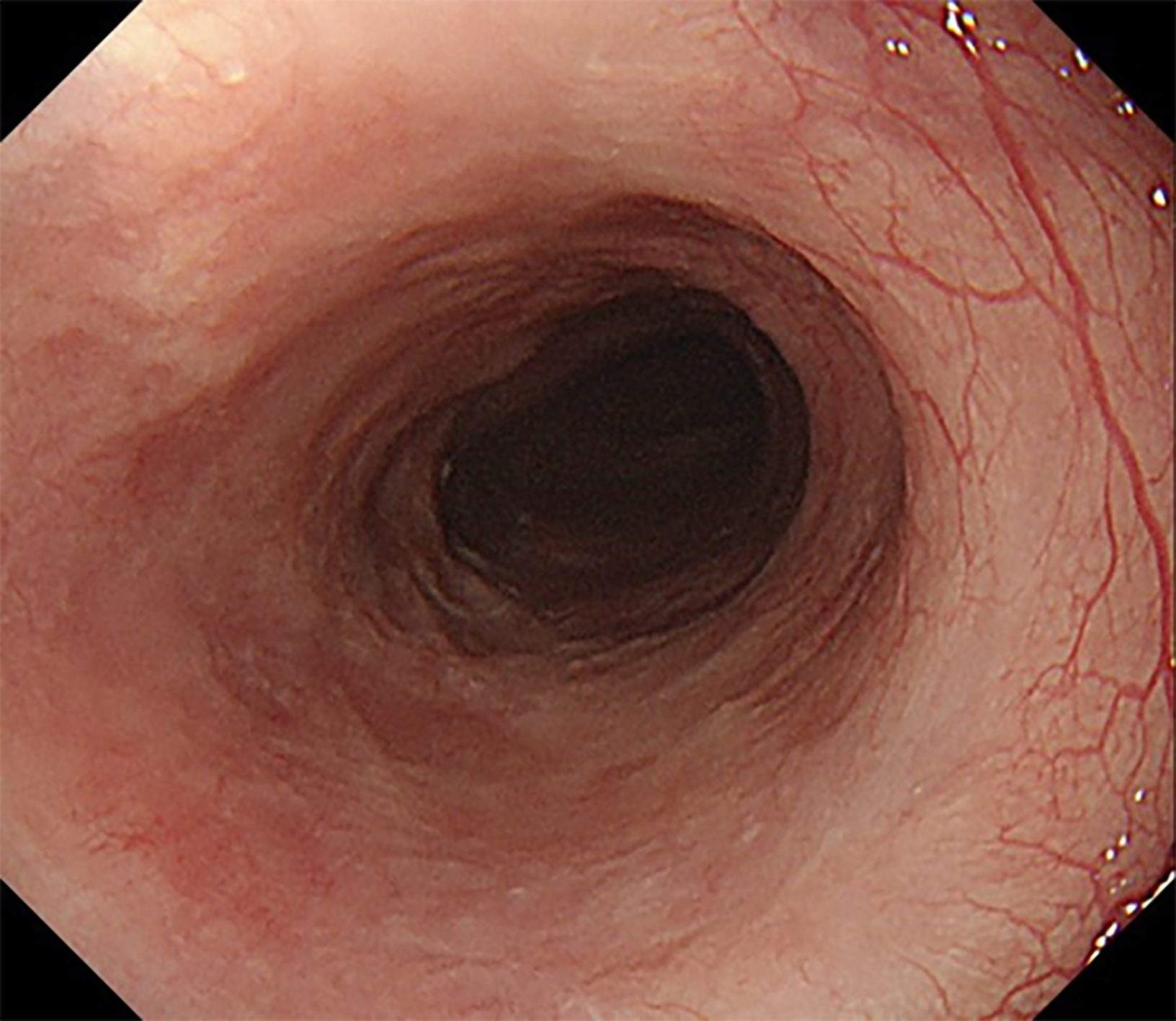
Esophagogastroduodenoscopy showed a semi-circumferential, irregular, yellowish-colored and granular lesion in the esophagus (30-35 cm from the incisors) (Figure 1A). Magnifying endoscopy with narrow band imaging (NBI) revealed aggregated minute yellowish spots with tortuous microvessels inside (Figure 1B). Moreover, type B1 intrapapillary capillary loops (IPCLs) and intervascular background coloration were observed around the yellow spots (Figure 1C). Lugo's iodine staining (1%) demons
The final preoperative diagnosis was diffuse esophageal xanthoma complicated with early esophageal cancer.
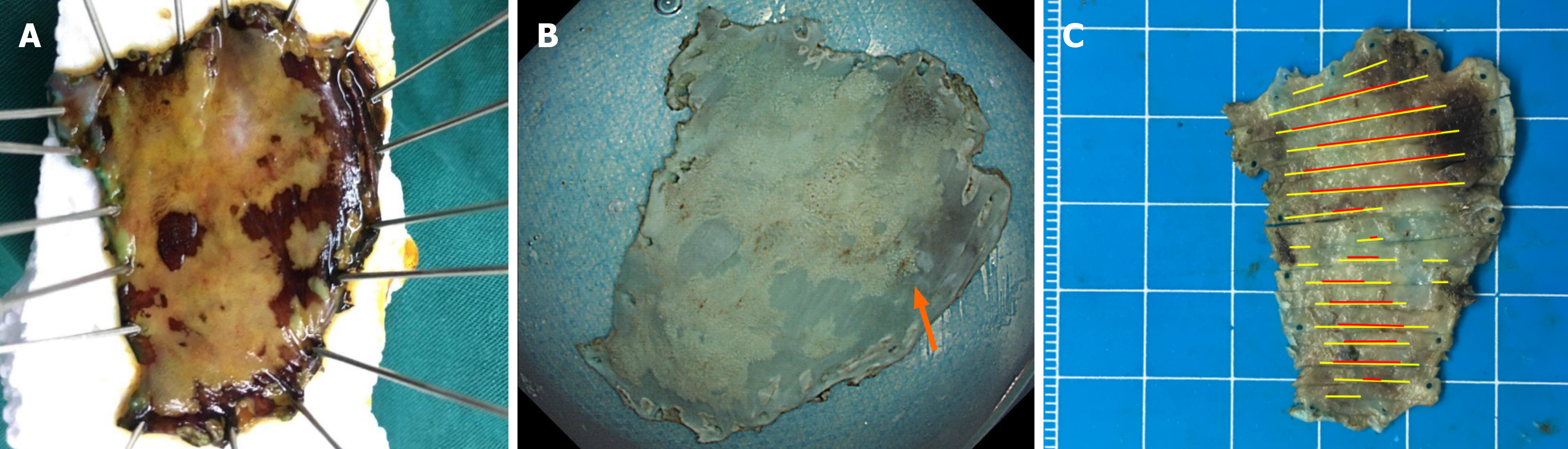
The lesion was completely resected en bloc by ESD (Figure 2). Oral prednisolone was administered at a dose of 30 mg/d on the third day after ESD. The dose was then gradually tapered in decrements of 5 mg/d every 2 wk for 1 mo followed by decrements of 5 mg/d every week for the next 4 wk. Steroids were discontinued after 8 wk.
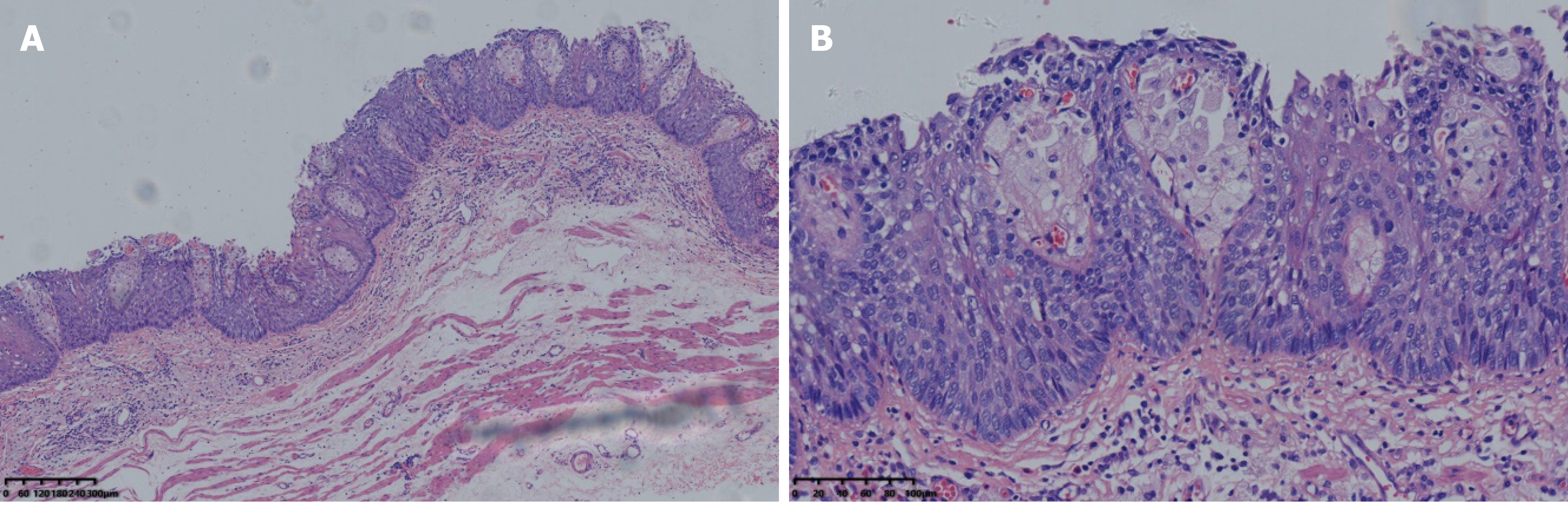
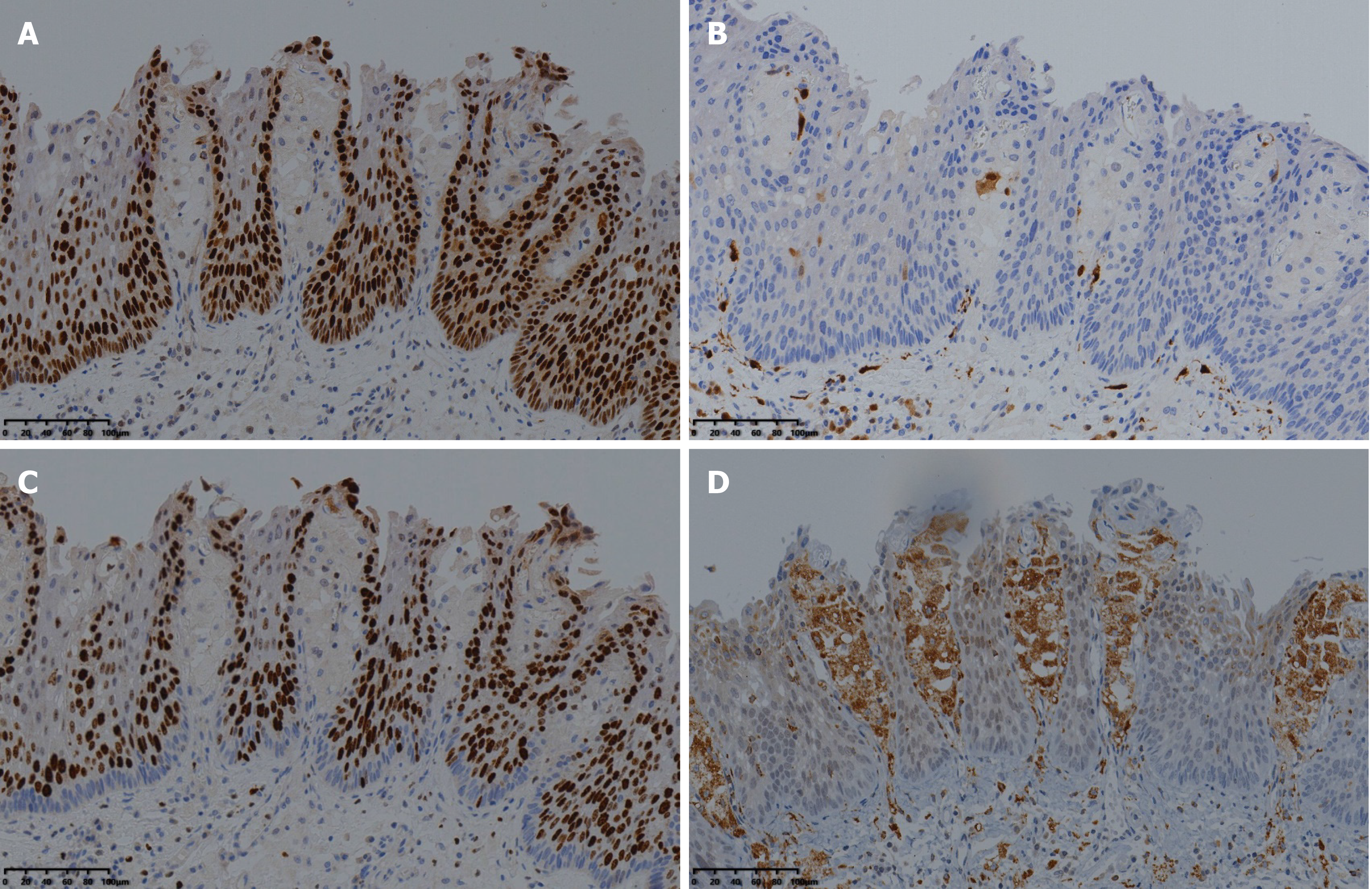
Histologically, the resected specimen was confirmed to be a squamous cell carcinoma in situ in which extensive foam cells were seen in the superficial mucosal layer (Figure 3). Immunohistochemical staining showed that the lesion was positive for P53 and negative for P16 (Figure 4A and B). The Ki-67 index was 90% (Figure 4C). The observed foamy cells were strongly positive for CD68, identical to a histiocytic cell origin, which is characteristic of xanthoma (Figure 4D). Postoperatively, the patient recovered well and was discharged from the hospital on day 5. There were no complaints of dysphagia following ESD. On follow-up endoscopy, which was scheduled at 3, 6, 12 and 24 mo after ESD, there was no postprocedural esophageal stricture, and neither recurrent nor metachronous lesions were found (Figure 5).
Gastrointestinal xanthomas are asymptomatic and infrequent non-neoplastic lesions characterized by the accumulation of foamy cells in the lamina propria[3]. They occur more frequently in the stomach with Helicobacter pylori-associated gastritis, and are rarely seen in the intestine or esophagus. The endoscopic findings of esophageal xanthomas have been reported as yellowish granular spots, yellowish elevated lesions, yellow-white colored plaques, or yellow verruciform lesions, measuring from 2 to 20 mm (usually ≤ 5 mm)[4-8]. Diffuse and extensive esophageal xanthoma in a patient is extremely rare. Gastrointestinal xanthoma is considered benign without clinical significance. However, it can be missed unless proven by a negative biopsy[2]. Therefore, endoscopic biopsy is recommended for such yellowish elevated lesions to distinguish ectopic sebaceous glands, carcinoid tumors, granular cell tumors, malignant lymphomas, or papillomas[1,3,9,10]. Histologically, the accumulation of foamy histiocytes of xanthoma could be a clue for differential diagnosis. Positive immunohistochemical staining for CD68, which indicates a histiocytic origin, is another characteristic finding of xanthoma[1].
Although the etiology of esophageal xanthoma remains unknown, it was reported to be derived from focal mucosal damage, in which lipids from damaged cell membranes are captured by interstitial histiocytes[11]. This may explain why they occur less frequently in the esophagus than in the stomach because the esophageal mucosa can better tolerate mucosal injury[12]. Xanthoma may also be associated with conditions such as history of radiotherapy or chemotherapy, infection, and biliary reflux[3,4,10]. To date, no apparent relationship between esophageal xanthoma and hyperlipidemia has been reported[13]. To the best of our knowledge, there have been no reports of esophageal xanthoma combined with esophageal malignancy. A history of subtotal gastrectomy and adjuvant chemotherapy may be related to the occurrence of diffuse xanthoma of the esophagus in our patient. Furthermore, the patient's long-term history of smoking together with heavy alcohol consumption could be a risk factor for concurrent esophageal cancer.
Changes in IPCLs, seen in magnifying NBI with the endoscopic classification of the Japan Esophageal Society, have been demonstrated to be simple and useful for differentiating whether identified lesions are neoplastic, and the prediction of the depth of invasion of superficial esophageal squamous cell carcinoma (SESCC) was also available[14]. Type A, lacking severe irregularity, corresponds to non-cancerous lesions; type B exhibits severe irregularity, identical to neoplastic lesions. Type B IPCLs were sub-classified into B1, B2, and B3 for T1a-EP or T1a-LPM, T1a-MM or T1b-SM1, and T1b-SM2 tumors, respectively[14]. In previous reports, magnifying endoscopy revealed esophageal xanthoma lesions as areas with aggregated minute yellowish spots with tortuous micro-vessels inside[15,16]. In addition to these reported characteristics, type B1 IPCLs and intervascular background coloration were also observed in our case. Intervascular background coloration has been reported to be useful for predicting the histology of high-grade intraepithelial neoplasia and invasive SESCC[17,18]. Type B1 tumors consist of abnormal IPCLs with a conserved loop-like formation, which is considered to correspond to T1a-EP or T1a-LPM[14]. These endoscopic findings correspond well with the histological findings in this case. As mentioned above, despite the fact that esophageal xanthomas are usually considered to be uncommon non-neoplastic lesions, determination of these lesions is imperative since they might be concurrent with malignancy. In addition, the characteristic endoscopic findings of our case may assist endoscopists in diagnosing similar lesions.
We report the first case of diffuse xanthoma complicated with early esophageal cancer. The characteristic endoscopic findings of xanthomas and esophageal cancer seen in image-enhanced endoscopy can help endoscopists to reach the correct diagnosis for appropriate treatment if this rare combination of disease is kept in mind.
The authors thank Dr. Qian LJ at Department of Pathology, The Affiliated Jinhua Hospital, Zhejiang University School of Medicine for providing some of the immunohistochemical findings from the resected specimen.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Endo S, Kinami S S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Hirokawa M, Takenaka R, Takahashi A, Sugihara K, Wada H, Tashiro T, Horiguchi H, Wakatsuki S, Sano T. Esophageal xanthoma: report of two cases and a review of the literature. J Gastroenterol Hepatol. 2003;18:1105-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Dirweesh A, Khan M, Bukhari S, Rimmer C, Shmuts R. Nodular Esophageal Xanthoma: A Case Report and Review of the Literature. Case Rep Gastrointest Med. 2017;2017:1503967. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Vimala R, Ananthalakshmi V, Murthy M, Shankar TR, Jayanthi V. Xanthelasma of esophagus and stomach. Indian J Gastroenterol. 2000;19:135. [PubMed] |
| 4. | Salamanca J, Alemany I, Sosa G, Pinedo F, Hernando S, Martín-Acosta P. Esophageal verruciform xanthoma following radiotherapy. Gastroenterol Hepatol. 2012;35:317-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Hamada K, Yamasaki Y, Kubota JI, Okada H. Yellowish lesions in the oesophagus. Gut. 2019;68:39-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Licci S, Campo SM, Ventura P. Verruciform xanthoma of the esophagus: an uncommon entity in an unusual site. Endoscopy. 2010;42 Suppl 2:E330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Becheanu G, Dumbrava M, Arbanas T, Diculescu M, Hoyeau-Idrissi N, Fléjou JF. Esophageal xanthoma--report of two new cases and review of the literature. J Gastrointestin Liver Dis. 2011;20:431-433. [PubMed] |
| 8. | Bang CS, Kim YS, Baik GH, Han SH. Xanthoma of the esophagus. Clin Endosc. 2014;47:358-361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Tsai SJ, Lin CC, Chang CW, Hung CY, Shieh TY, Wang HY, Shih SC, Chen MJ. Benign esophageal lesions: endoscopic and pathologic features. World J Gastroenterol. 2015;21:1091-1098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 68] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 10. | Herrera-Goepfert R, Lizano-Soberón M, García-Perales M. Verruciform xanthoma of the esophagus. Hum Pathol. 2003;34:814-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Odze R, Antonioli D, Shocket D, Noble-Topham S, Goldman H, Upton M. Esophageal squamous papillomas. A clinicopathologic study of 38 lesions and analysis for human papillomavirus by the polymerase chain reaction. Am J Surg Pathol. 1993;17:803-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Gencosmanoglu R, Sen-Oran E, Kurtkaya-Yapicier O, Tozun N. Xanthelasmas of the upper gastrointestinal tract. J Gastroenterol. 2004;39:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Díaz Del Arco C, Álvarez Sánchez Á, Fernández Aceñero MJ. Non-gastric Gastrointestinal Xanthomas: Case Series and Literature Review. J Gastrointestin Liver Dis. 2016;25:389-394. [PubMed] |
| 14. | Oyama T, Inoue H, Arima M, Momma K, Omori T, Ishihara R, Hirasawa D, Takeuchi M, Tomori A, Goda K. Prediction of the invasion depth of superficial squamous cell carcinoma based on microvessel morphology: magnifying endoscopic classification of the Japan Esophageal Society. Esophagus. 2017;14:105-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 224] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 15. | Hamada K, Uedo N, Kubo C, Tomita Y, Ishihara R, Yamasaki Y, Omori M, Arao M, Suzuki S, Iwatsubo T, Kato M, Tonai Y, Shichijo S, Matsuura N, Nakahira H, Kanesaka T, Yamamoto S, Akasaka T, Hanaoka N, Takeuchi Y, Higashino K, Okada H, Iishi H. Endoscopic appearance of esophageal xanthoma. Endosc Int Open. 2019;7:E1214-E1220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Mori H, Kato M, Uraoka T. A Case of Esophageal Xanthoma with Epithelial Reactive Inflammation with a Characteristic Finding of Narrow-Band Imaging Magnifying Endoscopy. Dig Dis. 2020;38:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Minami H, Inoue H, Ikeda H, Satodate H, Hamatani S, Nakao K, Kudo SE. Usefulness of Background Coloration in Detection of Esophago-Pharyngeal Lesions Using NBI Magnification. Gastroenterol Res Pract. 2012;2012:529782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Kanzaki H, Ishihara R, Ishiguro S, Nagai K, Matsui F, Yamashina T, Ohta T, Yamamoto S, Hanaoka N, Hanafusa M, Takeuchi Y, Higashino K, Uedo N, Iishi H, Tomita Y. Histological features responsible for brownish epithelium in squamous neoplasia of the esophagus by narrow band imaging. J Gastroenterol Hepatol. 2013;28:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |