Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5226
Peer-review started: February 9, 2021
First decision: February 28, 2021
Revised: March 8, 2021
Accepted: April 12, 2021
Article in press: April 12, 2021
Published online: July 6, 2021
Processing time: 134 Days and 23.4 Hours
Congenital muscular dystrophy (CMD) is a clinically and genetically heterogeneous group of inherited muscle disorders. Mutations in the CRPPA gene (encoding CDPLribitol pyrophosphorylase A) are recognized as causative factors of dystroglycanopathies, a subtype of CMD with defects in glycosylation.
The present study examined a Chinese family, whose proband presented mainly with muscle weakness in both lower limbs but without brain and eye symptoms. In this family, a homozygous deletion, c. 1114-1116del (p.V372del), was identified in exon 8 of CRPPA in the proband, while a heterozygous deletion was identified in the proband’s father and mother, who lacked symptoms. A mild dystroglycanopathy of CMD was diagnosed.
The findings of this study expanded the clinical and mutational spectrum of patients with CMD associated with CRPPA mutations.
Core Tip: A homozygous deletion, c. 1114-1116del (p.V372del), was identified in the exon 8 of the CRPPA gene in a Chinese family, which was diagnosed as congenital muscular dystrophy. Mutations in the CRPPA gene are recognized as causative factors of dystroglycanopathies, a subtype of congenital muscular dystrophy with defects in glycosylation. Findings in this study expanded the clinical and mutational spectrum of congenital muscular dystrophy patients with the CRPPA gene.
- Citation: Yang M, Xing RX. Homozygous deletion, c. 1114-1116del, in exon 8 of the CRPPA gene causes congenital muscular dystrophy in Chinese family: A case report. World J Clin Cases 2021; 9(19): 5226-5231
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5226.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5226
Congenital muscular dystrophy (CMD) is a clinically and genetically heterogeneous group of inherited muscle disorders, with muscle weakness often apparent at birth or in infancy. CMD is subtyped mainly by the causative pathogenic variants of multiple genes[1]. Currently, there are no complete or satisfactory classification systems. Classification by phenotype has shortcomings because the same phenotype can be caused by pathogenic variants in different genes, while one gene can result in a spectrum of clinical phenotypes. CMD is often subtyped according to the gene and its encoded protein in which the pathogenic variants occur, for example, defects in structural proteins (Laminin alpha-2 deficiency; collagen VI-deficient CMD), defects in glycosylation (dystroglycanopathies), defects of endoplasmic reticulum proteins (SEPN1-related CMD), and defects of nuclear envelope proteins (LMNA-related CMD)[2,3]. More than 19 gene mutations in POMT1, LARGE1, POMT2, FKRP, POMGNT1, FKTN, and Isoprenoid synthase domain-containing (ISPD, also called CRPPA) genes have been identified in dystroglycanopathies[4,5].
The CRPPA gene encodes CDP-L-ribitol pyrophosphorylase A, a protein involved in glycosylation. CRPPA helps to produce ribitol 5-phosphate, which is an important component of α-dystroglycan. The α-dystroglycan protein helps to anchor the cytoskeleton to the lattice of proteins and other molecules in the extracellular matrix. In skeletal muscles, glycosylated α-dystroglycan helps to stabilize and protect muscle fibers[6]. CRPPA mutations can cause deficiency of functional α-dystroglycan and damaged muscle fibers, which affects the development, structure, and function of skeletal muscles[7]. Besides causing dystroglycanopathies, CRPPA mutations have been identified in Walker–Warburg syndrome, muscle-eye-brain disease, and limbgirdle muscular dystrophy[5,8].
Most of the reported CMDs are inherited in an autosomal recessive manner and often affect one individual in non-consanguineous, small families. In contrast, most individuals with LMNA-related CMD and collagen VI-deficient CMD have a de novo pathogenic variant following an autosomal dominant manner. In the present study, we examined a family with CMD inherited in an autosomal recessive manner and identified a deletion, c. 1114-1116del, in the CRPPA gene as the cause.
A 26-year-old male presented with a 20-year history of elevated creatine kinase levels, and he had been diagnosed with fatigue in both lower limbs 4 years ago.
The patient visited the local hospital due to poor performance in his physical education class and was found to have an increase in creatine kinase levels (12270 U/L) 20 years ago when he was 6-years-old). At that time, there were no obvious symptoms of physical weakness in ordinary life, only the poor performance in physical education. No deletion of the DMD gene (encoding dystrophin) was detected using 25 pairs of primers. The patient accepted treatment with Chinese herbal medicine; however, the level of creatine kinase did not decrease significantly. Four years ago (at 22-years-old), the patient began to experience weakness in both lower extremities, manifested as strenuous standing up from a squatting position and strenuous stepping up the stairs, which gradually worsened to the point that standing up from squatting required hand support on the knees.
The patient was healthy before.
The patient denied consanguineous marriage and any special medical history and personal history. The parents had no symptoms of muscle weakness and had a normal creatine kinase level.
Physical examinations showed a 4/5 muscle strength when lying down while holding the head up; 5/5 muscle strength for the double upper extremity deltoid muscles, triceps, flexor and extensor carpal muscles, and short flexor extensor; 4/5 muscle strength for the biceps; 3/5 muscle strength for the double lower limb iliac muscles, gluteus maximus, and quadriceps; 1/5 muscle strength for the thigh adductor; 4/5 muscle strength for the gluteal middle muscle and hamstring muscle; and 5/5 muscle strength for tibialis anterior muscle and gastrocnemius muscle. The muscle tone was normal, and the upper tendon reflex and ankle reflex were normal. However, there was no reflex of both knees. Bilateral Babinski sign was negative.
Enzyme tests showed creatine kinase of 11082 U/L and creatine kinase myocardial band of 126 U/L.
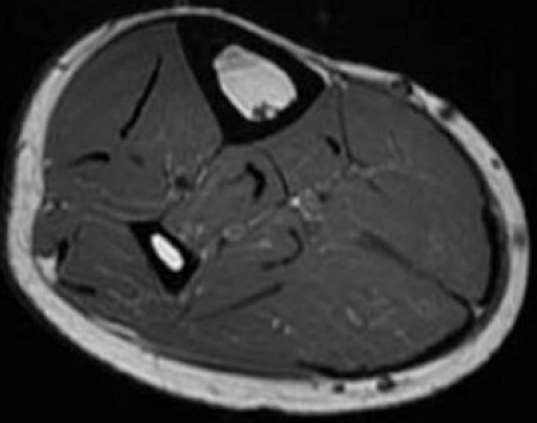
A routine electrocardiogram showed sinus arrhythmia and left ventricular high voltage. Pulmonary function test showed nonspecific ventilation dysfunction. Chest computed tomography showed left interlobar pleura and local pleura nodular thickening, suggesting an inflammation. Heart Doppler ultrasound and liver, gallbladder, pancreas, spleen, and urinary tract ultrasound showed no obvious abnormalities. Neuromyography showed no obvious abnormalities in motor nerve and sensory nerve conduction velocity. Quantitative electromyography measurement showed some myogenic changes in the right medial femoral muscle, gastrocnemius muscle, and tibialis anterior muscle. Magnetic resonance imaging of the right calf showed that the gastrocnemius muscle and soleus muscle were experiencing atrophy to different degrees, mainly in the medial head of the gastrocnemius muscle (Figure 1).
The proband and his parents were enrolled after providing informed written consent. Genomic DNA was extracted from white blood cells using a Genomic DNA extraction kit (Qiagen, Hilden, Germany). All exons of the CRPPA gene were sequenced using whole exome sequencing (Yulong Biomedical Group, Shanghai, China).
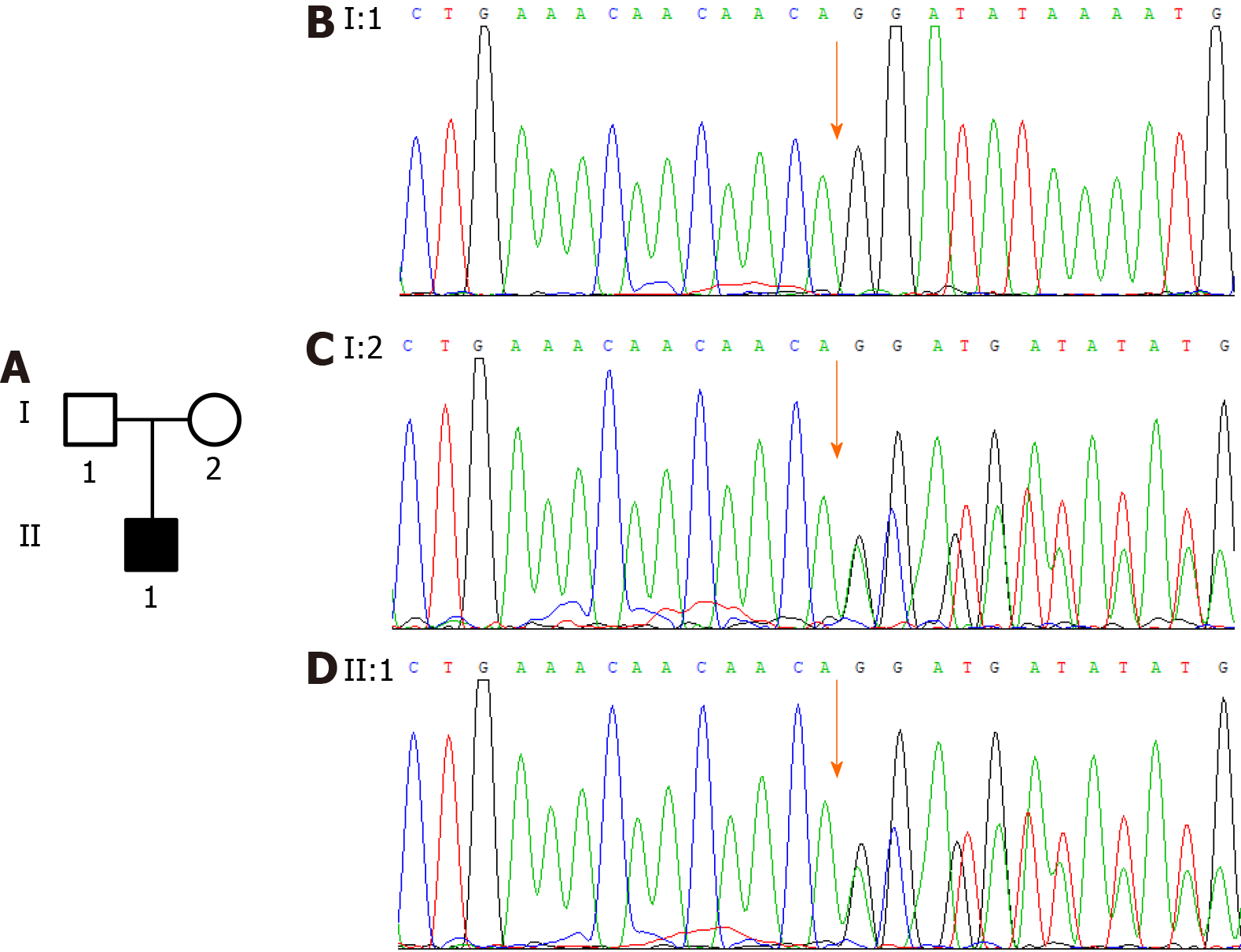
A homozygous deletion, c. 1114-1116del (p.V372del), was identified in exon 8 of the CRPPA gene (NM_001101426.3) in the proband (Figure 2B), while a heterozygous deletion was identified in the proband’s father and mother (Figure 2C and 2D). This variant was not included in the 1000 Genomes Project database or the ESP6500 data set of the National Heart, Lung, and Blood Institute exome sequencing project.
A mild dystroglycanopathy of CMD was diagnosed.
The patient was treated with vitamin B2 (5 mg three times a day) and coenzyme Q10 (10 mg three times a day).
During a follow-up period of 3 mo, the symptoms remained the same.
The pedigree presented in this study suggested a recessively inherited muscle disorder with progressive muscle weakness. Although there were no obvious symptoms of physical weakness in ordinary life in the proband at 6-years-old, his creatine kinase level was elevated and his performance in physical education was poor. This suggested mild muscle damage. Thus, the proband was diagnosed with congenital muscular dystrophy.
Muscular dystrophy is a disorder often caused by mutations in genes involved in muscle structure and function, which leads to muscle weakness and progressive disability[9]. Patients with muscular dystrophy often have an elevated level of creatine kinase caused by muscle damage[10]. Mostly, muscular dystrophy runs in families and can be a recessive, dominant, or X-linked inherited disorder[9]. In this study, gene mutation detection found a homozygous mutation, c. 1114-1116del, in CRPPA in the proband; however, his mother and father have a heterozygous deletion. The heterozygous mutation did not cause obvious muscle weakness in the patient’s parents, suggesting that only the homozygous mutation is pathogenic. We therefore propose that CMD caused by mutation of c. 1114-1116del of the CRPPA gene operates in a recessively inherited manner in this family.
Dystroglycanopathies are a group of CMDs caused by defects in glycosylation and are extremely variable in phenotypic severity. Severe dystroglycanopathies can result in structural brain, eye, and muscle abnormalities, while less severe forms of the disease group often have an adult onset without brain or eye abnormalities[11]. In this study, the symptoms of physical weakness occurred in the proband at 22-years-old, and no brain or eye abnormalities were found. This suggested mild dystroglycanopathy. Thus, CMD with c. 1114-1116del in the CRPPA gene progressed slowly. The proband was diagnosed with a mild dystroglycanopathy of CMD.
To date, mutations in 18 genes, including those encoding proteins involved in αdystroglycan glycosylation (FKTN, FKRP, ISPD, and TMEM5) have been identified in patients with the dystroglycanopathy subtype of CMD, and all these mutations demonstrate autosomal recessive inheritance[12]. The CRPPA gene has over ten other names, including ISPD[5]. ISPD mutations were identified in several dystroglycanopathy variants including CMD, Walker–Warburg syndrome, limbgirdle muscular dystrophy, and cobblestone lissencephaly[13]. In our pedigree, no mutation of the DMD gene was detected. DMD is the largest known human gene that is involved in the production of dystrophin, which functions in muscle movement. In contrast, the CRPPA gene produces a protein that regulates α-dystroglycan in glycosylation, which subsequently stabilizes and protects muscle fibers.
In conclusion, this study reported a pedigree in which the proband had mild dystroglycanopathy of CMD caused by a homozygous mutation, c. 1114-1116del, of the CRPPA gene.
We are thankful to the patient who agreed to participate in this study.
Manuscript source: Unsolicited manuscript
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chisthi MM S-Editor: Zhang L L-Editor: Filipodia P-Editor: Wang LL
| 1. | Wang CH, Bonnemann CG, Rutkowski A, Sejersen T, Bellini J, Battista V, Florence JM, Schara U, Schuler PM, Wahbi K, Aloysius A, Bash RO, Béroud C, Bertini E, Bushby K, Cohn RD, Connolly AM, Deconinck N, Desguerre I, Eagle M, Estournet-Mathiaud B, Ferreiro A, Fujak A, Goemans N, Iannaccone ST, Jouinot P, Main M, Melacini P, Mueller-Felber W, Muntoni F, Nelson LL, Rahbek J, Quijano-Roy S, Sewry C, Storhaug K, Simonds A, Tseng B, Vajsar J, Vianello A, Zeller R; International Standard of Care Committee for Congenital Muscular Dystrophy. Consensus statement on standard of care for congenital muscular dystrophies. J Child Neurol. 2010;25:1559-1581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 134] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 2. | Fichna JP, Macias A, Piechota M, Korostyński M, Potulska-Chromik A, Redowicz MJ, Zekanowski C. Whole-exome sequencing identifies novel pathogenic mutations and putative phenotype-influencing variants in Polish limb-girdle muscular dystrophy patients. Hum Genomics. 2018;12:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Sparks SE, Quijano-Roy S, Harper A, Rutkowski A, Gordon E, Hoffman EP, Pegoraro E, Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mirzaa G, Amemiya A. Congenital Muscular Dystrophy Overview – RETIRED CHAPTER, FOR HISTORICAL REFERENCE ONLY 1993. [PubMed] |
| 4. | Saito K, Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mirzaa G, Amemiya A. Fukuyama Congenital Muscular Dystrophy 1993. [PubMed] |
| 5. | Gençpınar P, Uyanık G, Haspolat Ş, Oygür N, Duman Ö. Clinical and Molecular Manifestations of Congenital Muscular Alpha-Dystroglycanopathy due to an ISPD Gene Mutation. Neurophysiology. 2019;51:373-378. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | United States National Library of Medicine. CRPPA gene. CDP-L-ribitol pyrophosphorylase A. In: MedilinePlus [cited 3 March 2021]. Available from: https://ghr.nlm.nih.gov/gene/CRPPA. |
| 7. | Barton ER, Pacak CA, Stoppel WL, Kang PB. The ties that bind: functional clusters in limb-girdle muscular dystrophy. Skelet Muscle. 2020;10:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Song D, Fu X, Ge L, Chang X, Wei C, Liu J, Yang H, Qu S, Bao X, Toda T, Wu X, Xiong H. A splice site mutation c.1251G>A of ISPD gene is a common cause of congenital muscular dystrophy in Chinese patients. Clin Genet. 2020;97:789-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | National Health Service. Muscular dystrophy-Causes. [cited 3 March 2021]. Available from: https://www.nhs.uk/conditions/muscular-dystrophy/causes/. |
| 10. | Mayo Clinic. Muscular dystrophy-Diagnosis. [cited 3 March 2021]. Available from: https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/diagnosis-treatment/diagnosis/dxc-20375389. |
| 11. | Johnson K, Bertoli M, Phillips L, Töpf A, Van den Bergh P, Vissing J, Witting N, Nafissi S, Jamal-Omidi S, Łusakowska A, Kostera-Pruszczyk A, Potulska-Chromik A, Deconinck N, Wallgren-Pettersson C, Strang-Karlsson S, Colomer J, Claeys KG, De Ridder W, Baets J, von der Hagen M, Fernández-Torrón R, Zulaica Ijurco M, Espinal Valencia JB, Hahn A, Durmus H, Willis T, Xu L, Valkanas E, Mullen TE, Lek M, MacArthur DG, Straub V. Detection of variants in dystroglycanopathy-associated genes through the application of targeted whole-exome sequencing analysis to a large cohort of patients with unexplained limb-girdle muscle weakness. Skelet Muscle. 2018;8:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Bouchet-Séraphin C, Vuillaumier-Barrot S, Seta N. Dystroglycanopathies: About Numerous Genes Involved in Glycosylation of One Single Glycoprotein. J Neuromuscul Dis. 2015;2:27-38. [PubMed] |
| 13. | Magri F, Colombo I, Del Bo R, Previtali S, Brusa R, Ciscato P, Scarlato M, Ronchi D, D'Angelo MG, Corti S, Moggio M, Bresolin N, Comi GP. ISPD mutations account for a small proportion of Italian Limb Girdle Muscular Dystrophy cases. BMC Neurol. 2015;15:172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |