Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5211
Peer-review started: December 31, 2020
First decision: March 27, 2021
Revised: April 7, 2021
Accepted: May 7, 2021
Article in press: May 7, 2021
Published online: July 6, 2021
Processing time: 174 Days and 22.5 Hours
This study reports a case of autologous tenon capsule packing to treat the posterior exit wound of penetrating injury.
To treat a 58-year-old male patient with penetrating eyeball injury caused by an iron sheet, we used autologous tenon capsule packing. Two months after removal of the silicone oil, the corrected visual acuity was 0.3, the retina was flat, the tenon capsule graft was in place, the posterior wound closed well, and the intraocular pressure was 15.8 mmHg.
Autologous tenon capsule packing to treat the posterior exit wound of penetrating injury is safe and effective.
Core Tip: Eyeball penetrating injury refers to an open trauma that may allow the exposure of any vulnerant into the eye from one side, and penetrates the entire eyeball and traverses through the other side of the eyeball. Eyeball penetrating injury wounds are divided into entry wound and exit wound. The laceration at the exit wound is often located at the posterior position and is difficult to suture during the first-stage surgery, and any attempt to a reckless suture may cause even greater damage to the eyeball. Thus, our report describes a newly modified technique involving the use of autologous tenon capsule packing to treat the posterior exit wound of penetrating injury.
- Citation: Yi QY, Wang SS, Gui Q, Chen LS, Li WD. Autologous tenon capsule packing to treat posterior exit wound of penetrating injury: A case report. World J Clin Cases 2021; 9(19): 5211-5216
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5211.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5211
Eyeball penetrating injury refers to an open trauma that may allow the exposure of any vulnerant into the eye from one side, and penetrates the entire eyeball and traverses through the other side of the eyeball. Eyeball penetrating injury wounds are divided into entry wound and exit wound. The laceration at the exit wound is often located at the posterior position and is difficult to suture during the first-stage surgery, and any attempt to a reckless suture may cause even greater damage to the eyeball[1]. We report a case of secondary surgery in which a new modified technique was used to treat the exit wound after penetrating ocular injury.
A 58-year-old male patient presented with decreased vision acuity and pain for 5 h in the right eye after being injured by an iron bullet.
The patient was admitted to our emergency department after being injured by an iron bullet.
The patient was healthy.
The patient had a disease-free personal and family history.
Ophthalmological examination of the right eye showed decreased naked vision, correct light projection, intraocular pressure of 3.7 mmHg, slight eyelid swelling, mixed congestion in the bulbar conjunctiva, and subconjunctival hemorrhage. An oblique laceration of about 6 mm long was visible in the bulbar conjunctiva at 5:30 o’clock direction and 4 mm away from the corneosclera margin. The cornea was slightly edematous with a large number of blood cells attached in the posterior cornea, and the depth of the anterior chamber was acceptable. The aqueous humor was bloody turbid. The pupil was round with a diameter of 4 mm and the lens was locally opaque. A large amount of vitreous hemorrhage was noticed and the fundus was unclear.
Blood tests showed no obvious abnormality.
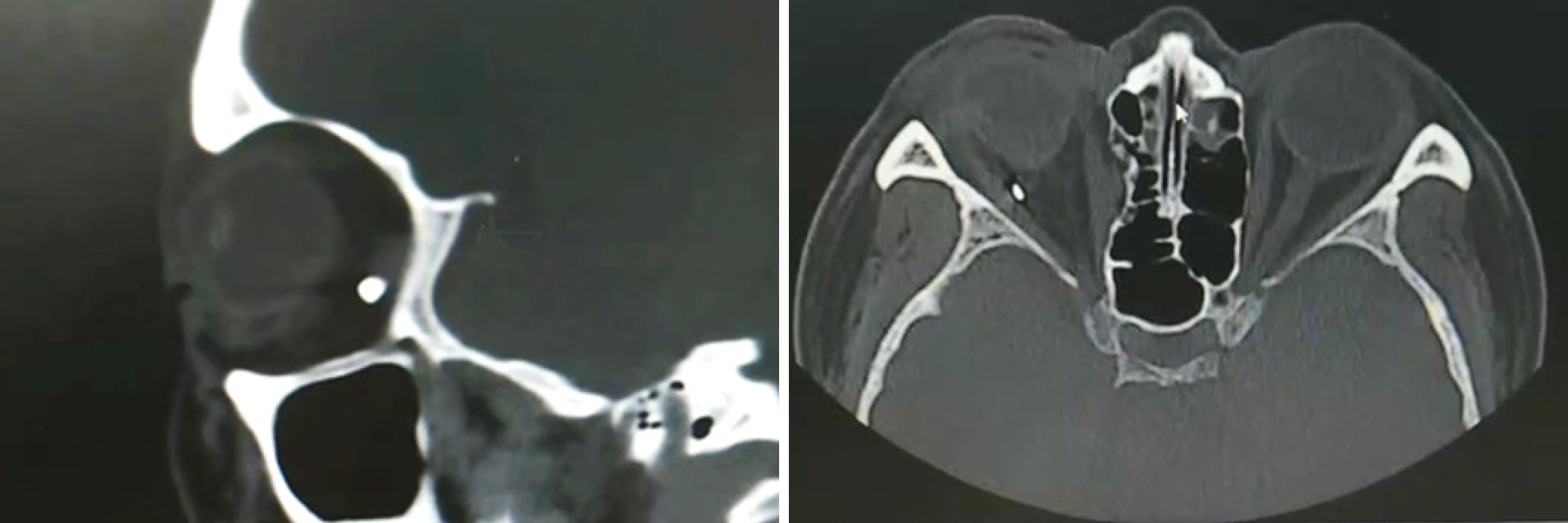
Orbital computed tomography showed an abnormal morphology of the right eyeball, and a foreign body behind the eyeball (Figure 1).
The final diagnosis of the present case was right eye penetrating injury and foreign body in the right eye orbit.
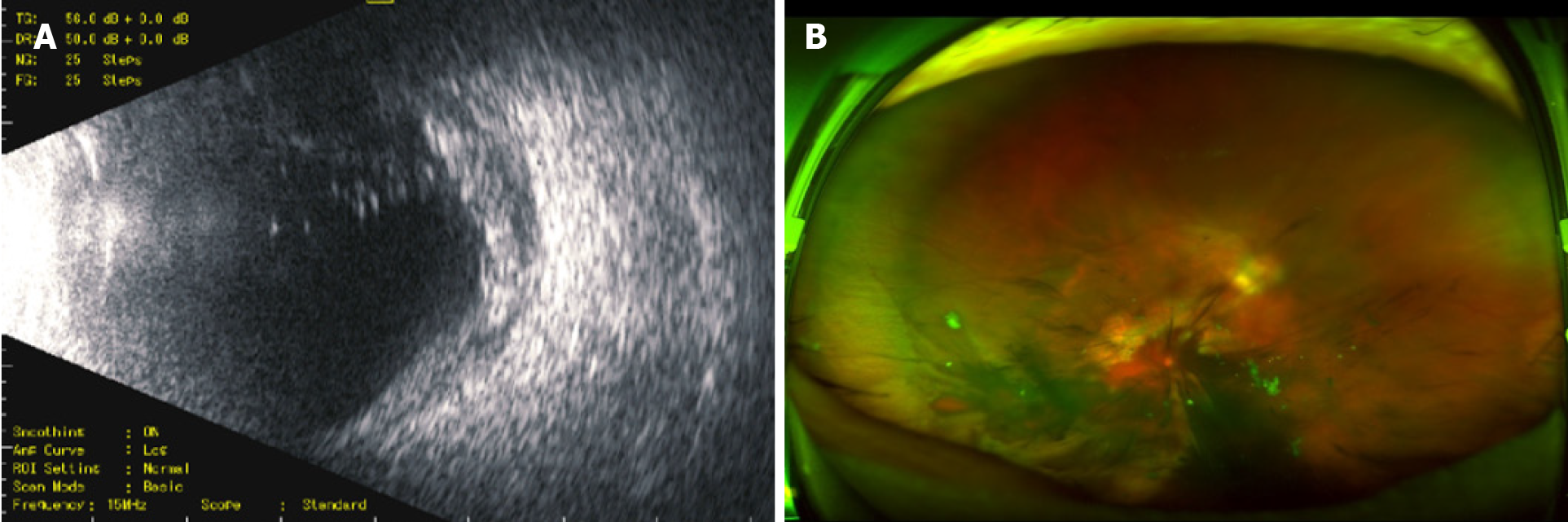
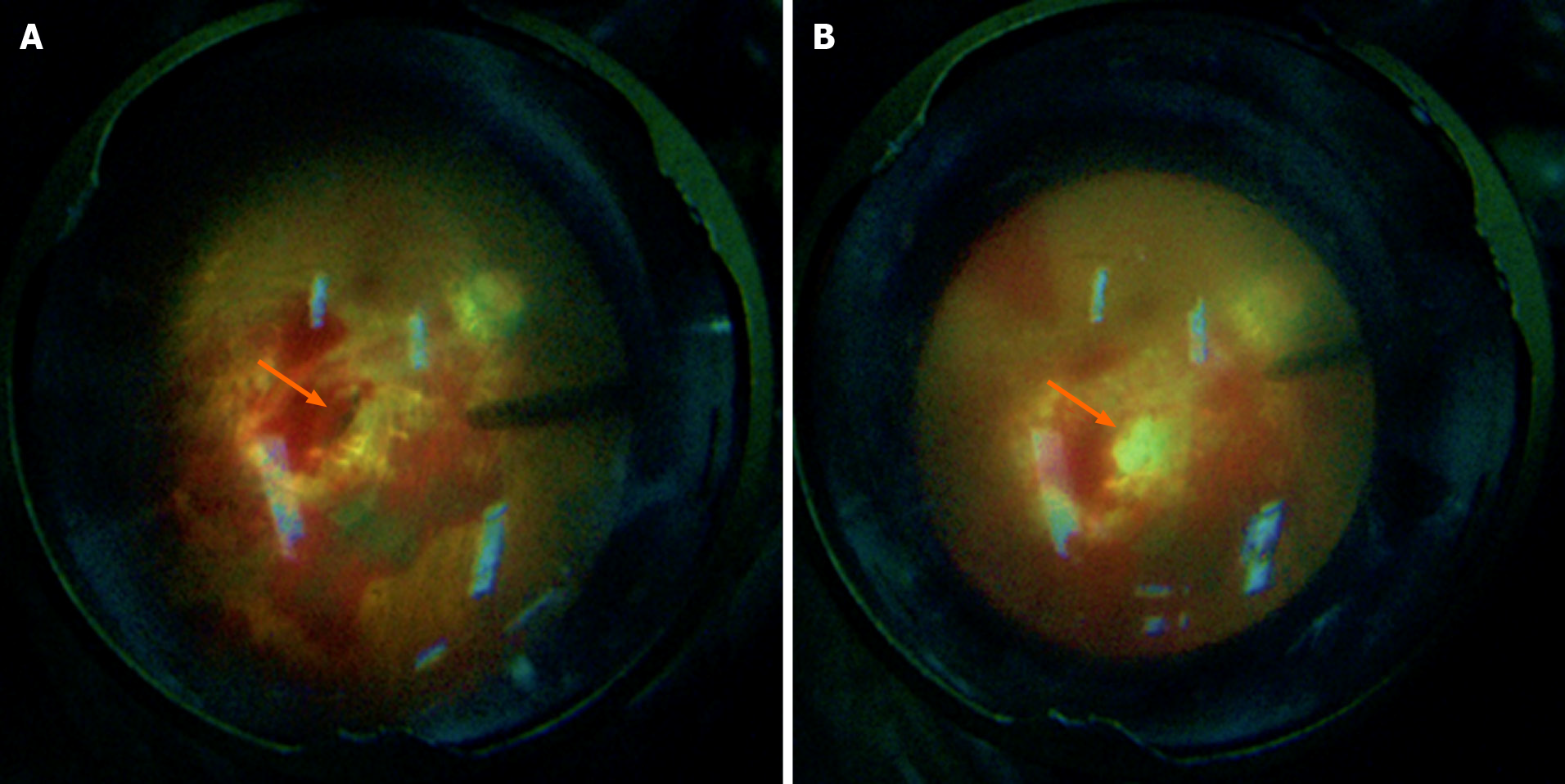
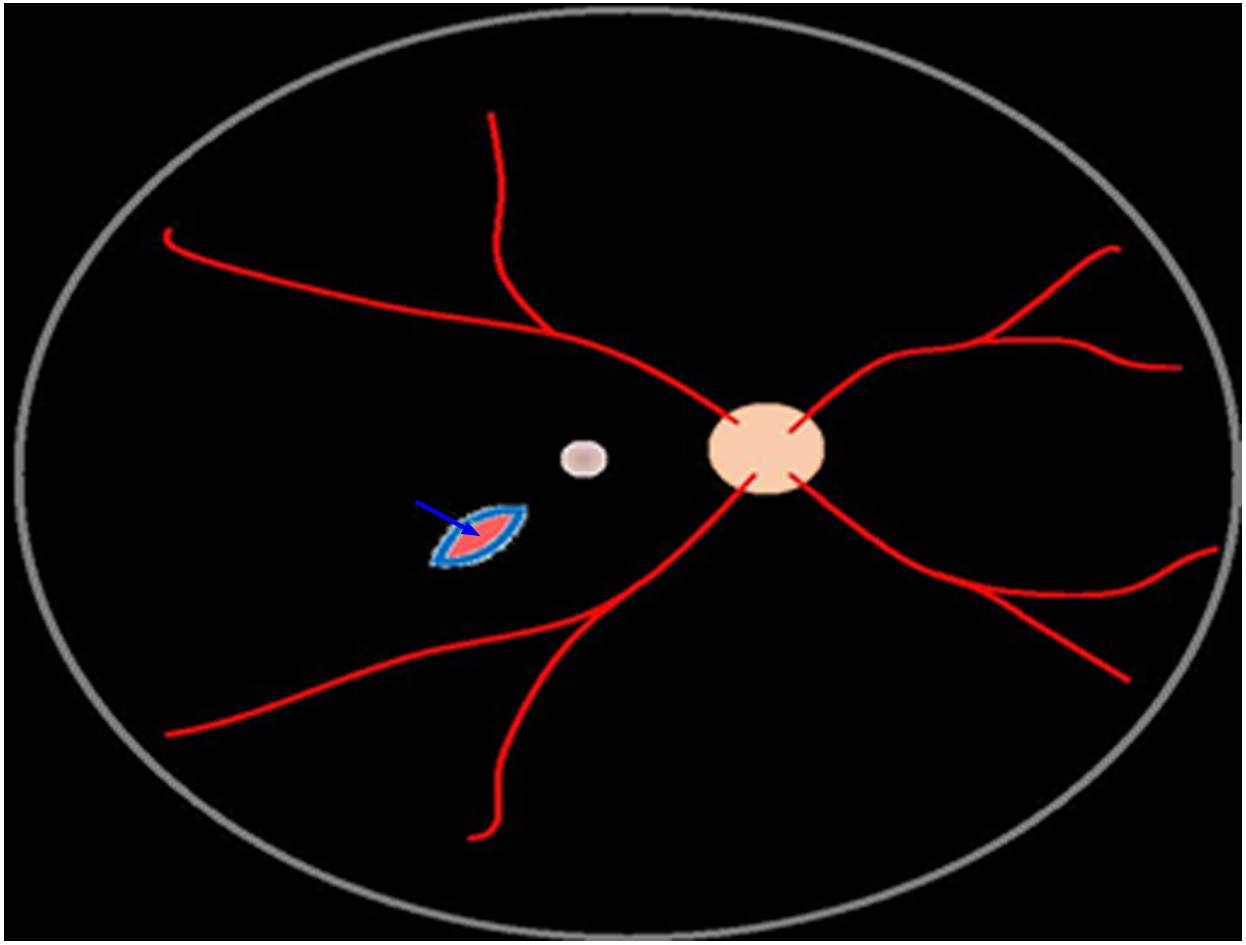
After emergency admission, the patient underwent right eyeball debridement and suturing with scleral exploration under local anesthesia. During surgery, a 6 mm long full-thickness laceration of the sclera was seen under a conjunctival laceration at 5:30 o’clock direction and 4 mm away from the scleral margin. The scleral laceration was closed with two stitches using 8-0 suture. Because the foreign body was located inside the posterior orbit and was stable in nature, the removal of it was not considered for the time being. Postoperatively, the patient was given general and topical antibiotics and hormonal medications, as well as preventive tetanus antitoxin. During 1 wk postoperatively, the patient’s right eye was stable, without intraocular inflammation, elevated intraocular pressure, or intraocular active bleeding (Figure 2). One week later, the patient underwent "23G vitrectomy in the right eye" under local anesthesia to remove the vitreous hemorrhage. First, we performed a conventional 23G three channel incision to remove vitreous hemorrhage. It was found that the posterior exit wound of the penetrating injury was located at two pupillary distances (PD) below the temporal region of the macula in the right eye, and a full-thickness spindle hole with a transverse diameter of about one PD was seen in the wall of the eyeball. The conjunctiva was cut from the upper corneoscleral margin, the conjunctiva and fascia were separated, and a fascial flap with an appropriate size was selected, which was trimmed and filled in the hole at the posterior exit wound of the penetrating injury via the scleral puncture using intraocular forceps after the conjunctival epithelial tissue was removed. Subsequently, gas-liquid exchange in the vitreous cavity and injection of silicone oil were performed (Figure 3). The surgery diagram is shown in Figure 4. Postoperatively, the patient was given antibiotics and hormone eye drops.
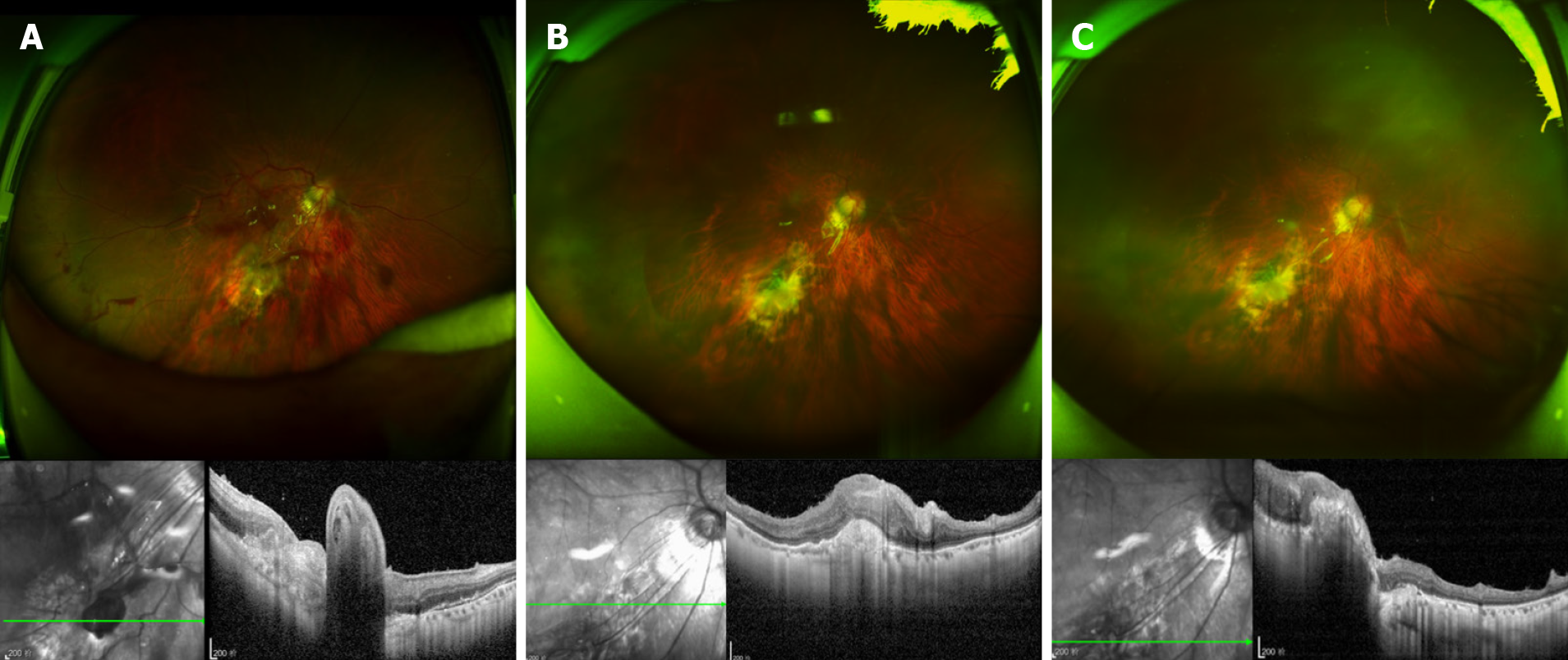
The patient revisited the hospital at 2 wk, 1 mo, and 5 mo after surgery, and 2 mo after removal of the silicone oil. Ophthalmological examination at 2 wk after surgery revealed that the best corrected visual acuity of the right eye was 0.02, there was silicone oil filling in the vitreous cavity of the right eye and a flattened retina, the tenon capsule graft was in place at the hole of the fundus eyeball wall, and the intraocular pressure was 15.3 mmHg. Optical coherence tomography (OCT) examination showed that the stuffing tissue in the hole was protruded in place, and the surrounding retina was flattened. Ophthalmological examination at 5 mo after surgery showed that the best corrected visual acuity was 0.3, there was silicone oil filling in the vitreous cavity of the right eye and a flattened retina, the tenon capsule graft was in place at the hole of the fundus ocular wall, and the intraocular pressure was 16.1 mmHg. OCT examination showed that the stuffing tissue in the hole was in place and continuous with the surrounding tissue, and the surrounding retina was flat. Ophthalmological examination at 2 mo after removal of the silicone oil showed that the best corrected visual acuity was 0.3, there was a flattened retina, and the tenon capsule graft was in place at the hole of the fundus ocular wall. OCT examination showed that the stuffing tissue in the hole was in place and continuous with the surrounding tissue, the surrounding retina was flat, and the intraocular pressure was 15.8 mmHg (Figure 5). No complications occurred during or after the surgery.
Eyeball penetrating injury refers to an open trauma that may allow the exposure of any vulnerant into the eye from one side, and penetrates the entire eyeball and traverses through the other side of the eyeball. Such extensive injuries accompanied by intraocular or orbital foreign bodies often cause serious damages to the eye tissue, and may predispose to secondary infections, retinal detachment, and optic nerve damage, which leads to difficulty in treatment and a poor prognosis[2].
Clinically, eyeball penetrating injury wounds are divided into entry wound and exit wound. The laceration at the exit wound is often located at the posterior position and is difficult to suture during the first-stage surgery, and any attempt to a reckless suture may cause even greater damage to the eyeball. It was reported that some smaller wounds with stable intraocular pressure can heal by themselves within the time window of second-stage surgery. Moreover, during the second-stage vitreoretinal surgery, these small wounds that can heal by themselves can be quickly filled with silicone oil after gas-liquid exchange, so as to control the stable intraocular pressure[3,4]. On the other hand, larger wounds with more extensive damage are managed by filling the posterior exit wound using gelatin sponge. However, studies have shown that gelatin sponge is a synthetic material that may induce an immune response when used as a filler[5,6]. Zhu et al[7] have reported to use amnion transplantation to treat and correct the choroidal holes caused by trauma. Similar to gelatin, amnion as a foreign body filler may also potentially induce an immune response[7-9]. Ma et al[1] have used autologous tenon capsule transplantation to fill posterior exit wounds caused by penetrating injuries. The main component of the tenon capsule is fibrous tissue, which is similar to scleral tissue and conducive to tissue repair and scar healing. To avoid the chances of rejection reactions and to facilitate the healing process, autologous tenon capsules are used to fill such posterior exit wounds[1]. This method provided impressive results and restored the integrity of the wall of the eyeball, and maintained the intraocular pressure and prevented the leakage of silicone oil or inert filling gas in the eye.
In this case, we used autologous tenon capsule packing to treat the posterior exit wound of penetrating injury, which achieved satisfactory effects. For the case, the posterior perforation port was closed well, without immune reaction and silicone oil overflow. The intraocular pressure remained normal. Over time, the stuffing became flat. It healed and had good continuity with the surrounding eyeball wall. This method provides a reference for the treatment of similar cases, but should be subject to validation with more cases and long-term observation.
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yang J S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Ma J, Zhang Y, Moe MC, Zhu TP, Yao K. Transocular removal of a retrobulbar foreign body and internal patch of the posterior exit wound with autologous tenon capsule. Arch Ophthalmol. 2012;130:493-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Savar A, Andreoli MT, Kloek CE, Andreoli CM. Enucleation for open globe injury. Am J Ophthalmol 2009; 147: 595-600. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Kanu LN, Jiang Y, Gonzalez AF, Mieler WF. Visual and Anatomic Outcomes in Perforating Ocular Injuries. J Vitreoretin Dis. 2019;3:428-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Topping TM, Abrams GW, Machemer R. Experimental double-perforating injury of the posterior segment in rabbit eyes: the natural history of intraocular proliferation. Arch Ophthalmol. 1979;97:735-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 88] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Black P. Cerebrospinal fluid leaks following spinal surgery: use of fat grafts for prevention and repair. Technical note. J Neurosurg. 2002;96:250-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Luparello C, Mauro M, Lazzara V, Vazzana M. Collective Locomotion of Human Cells, Wound Healing and Their Control by Extracts and Isolated Compounds from Marine Invertebrates. Molecules. 2020;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Zhu D, Jin X, Zhou J. Transplantation of amniotic membrane for choroidal hole to treat suprachoroidal silicone oil migration. Acta Ophthalmol. 2017;95:e522-e523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Murphy SV, Skardal A, Nelson RA Jr, Sunnon K, Reid T, Clouse C, Kock ND, Jackson J, Soker S, Atala A. Amnion membrane hydrogel and amnion membrane powder accelerate wound healing in a full thickness porcine skin wound model. Stem Cells Transl Med. 2020;9:80-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 9. | Dewey MJ, Johnson EM, Slater ST, Milner DJ, Wheeler MB, Harley BAC. Mineralized collagen scaffolds fabricated with amniotic membrane matrix increase osteogenesis under inflammatory conditions. Regen Biomater. 2020;7:247-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |