Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5197
Peer-review started: December 7, 2020
First decision: March 27, 2021
Revised: April 2, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 6, 2021
Processing time: 199 Days and 5.5 Hours
Peliosis hepatis (PH) is a rare benign lesion of vascular origin with a pathological characteristic of multiple blood-filled cavities in the liver parenchyma. It is commonly misdiagnosed due to its lack of specificity in clinical presentation and laboratory test results. Herein, a case of a patient with PH who was misdiagnosed with hepatic echinococcosis before operation to remove the lesions was analyzed, with an emphasis on the computed tomography and magnetic resonance imaging characteristics of PH.
We outline the case of a 40-year-old Chinese female who was admitted with aggravated abdominal pain with fever for 1 wk. Ultrasound examination at the local hospital indicated hepatic echinococcosis. However, discordance between imaging diagnosis, clinical history and laboratory examinations in our hospital. Subsequently, the patient was pathologically confirmed as having PH-like changes, which recurred 1 year after operation removal of the lesion.
Our objective is to highlight the imaging diagnostic value of PH.
Core Tip: The imaging presentation of peliosis hepatis is complex and diverse, which does not correspond with the clinical history and laboratory examination. In this case, computed tomography and magnetic resonance imaging characteristics of peliosis hepatis were valuable that had been proven.
- Citation: Ren SX, Li PP, Shi HP, Chen JH, Deng ZP, Zhang XE. Imaging presentation and postoperative recurrence of peliosis hepatis: A case report. World J Clin Cases 2021; 9(19): 5197-5202
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5197.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5197
In 1916, Schoenlank[1] described peliosis hepatis (PH) through histopathological biopsy: multiple blood-filled cavities of various sizes in the liver parenchyma. This is a rare disease and usually misdiagnosed due to clinical symptoms and laboratory findings are single with atypical symptoms and liver function abnormalities[2]. However, the imaging findings are diverse and complex with similar lesions, like liver hematoma[3], liver cyst[4], liver hemangioma[5], liver echinococcosis[6], liver metastasis[7], adenoma[8] and abscess. Therefore, imaging diagnosis will be an important challenge for the diagnosis of hepatic purpura. Here, we analyze the computed tomography (CT) and magnetic resonance imaging images in a case of a patient with PH who was misdiagnosed with echinococcosis before an operation to remove the lesion. The patient provided informed consent for publication of the case.
A 40-year-old woman reported persistent total abdominal distension and radiating back pain for 1 mo and aggravated abdominal pain with fever for 1 wk.
The patient had no other symptoms except for progressive abdominal pain with fever for 1 wk.
Her past medical history indicated antral gastritis for 10 years, unknown specific treatment, no underlying disease and no history of living in foci of infection or endemic areas.
She had no personal or family history of other diseases.
On physical examination, the patient presented with abdominal distension and percussion pain in the liver area (+), and she had a blood pressure of 132/78 mmHg with pulse rate of 75 beats per minute.
Laboratory examination indicated the following: total bilirubin, 41.9 mmol/L; direct bilirubin, 17.6 mmol/L; indirect bilirubin, 24.3 mmol/L; gamma-glutamyl transferase, 274 U/L; alkaline phosphatase, 309 U/L; lactate dehydrogenase, 327 U/L; serum 5′-nucleotidase, 28.8 U/L; and serum cholinesterase, 3542 U/L. Urinalysis, coagulation tests, complete blood count, infection marker tests and tumor marker tests did not reveal any obvious abnormalities.
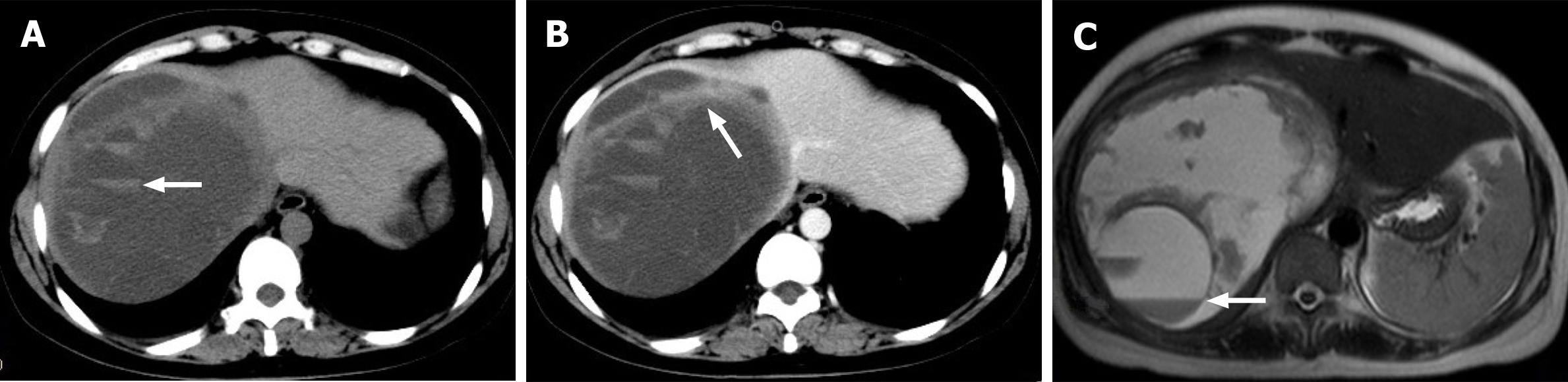
Ultrasound examination at the local hospital indicated hepatic echinococcosis, and the patient was admitted to our hospital for further treatment. CT scanning of the right lobe of the liver revealed a cystic lesion approximately 11.7 cm × 15.2 cm in size and with clear margins. Multiple sacs of various sizes were present inside the cyst, with high-density blood accumulation opacities, and fluid–fluid levels in some of the sacs (Figure 1A). The margin of the lesion was slightly enhanced on enhanced scan (Figure 1B), and the inferior vena cava was compressed and unclear. Magnetic resonance imaging examination revealed a large mixed long T2 signal in the right lobe of the liver, the “capsule-in-capsule” sign, signs of intracapsular stratification (Figure 1C) and compression and stenosis of the inferior vena cava.
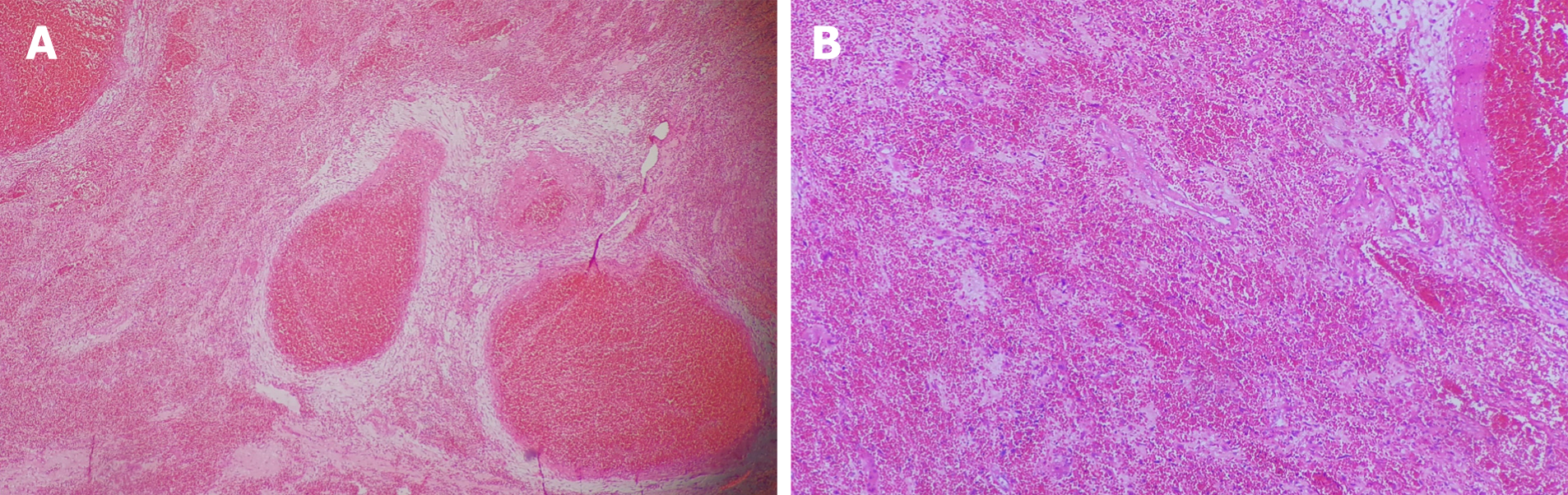
Pathology was consistent with PH-like changes (Figure 2). Microscopy showed multiple blood-filled cysts and liver parenchymal hemorrhage and necrosis in the lesion. The inner wall of the cyst cavity was not lined by endothelial cells.
The lesion was removed by open surgery under general anesthesia.
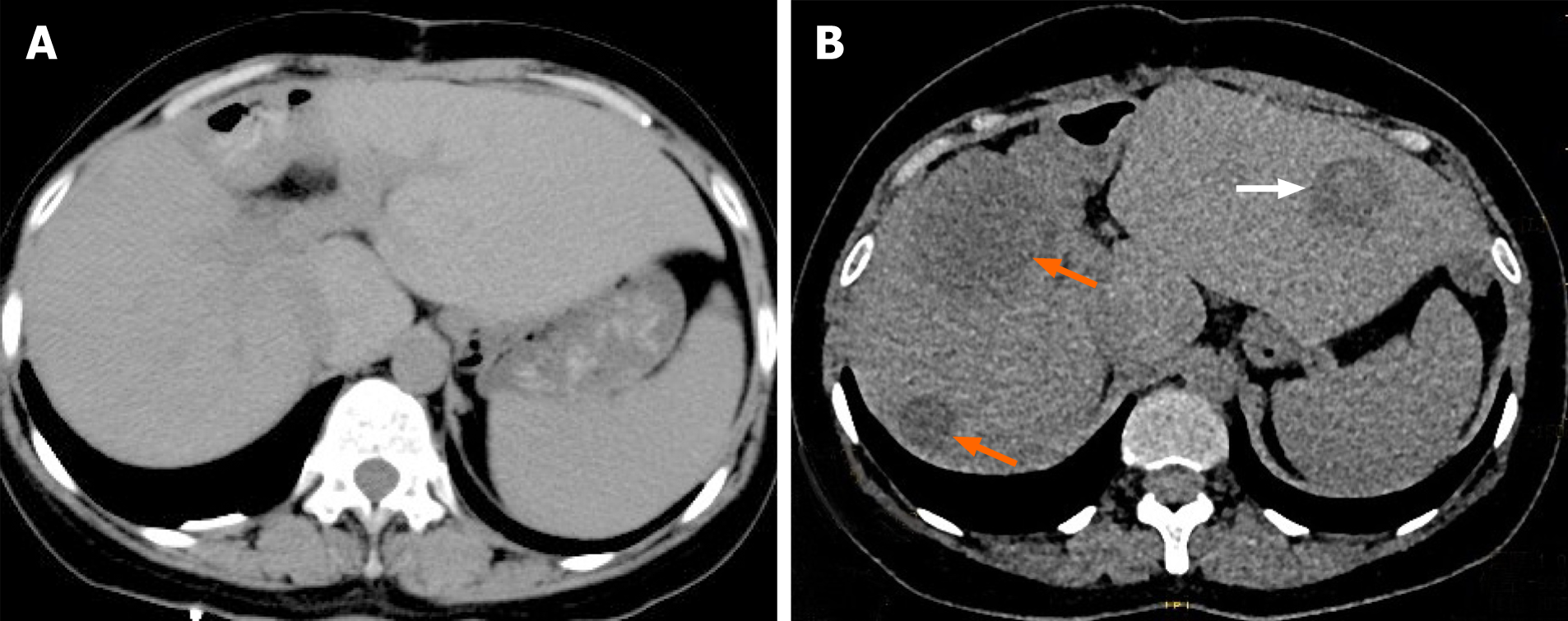
The patient had no signs of recurrence at the 3 mo postoperative re-examination (Figure 3A). On abdominal CT re-examination 1 year after operation, multiple low or slightly low-density patches were detected in the liver parenchyma, and some lesions exhibited high-density opacities with blood-like density (Figure 3B). Recurrence of PH was considered.
The present case has several features. First, the patient presented with PH by operation and pathology. Second, imaging manifestations did not match symptoms and laboratory tests. Third, the lesions relapsed 1 year after the operation.
PH pathologically manifests as multiple blood-filled cysts of various sizes in the liver parenchyma[1,9]. PH mostly occurs in adults, and its incidence between males and females is the same[10]. The causes of PH are unknown, and its development may be associated with factors such as drugs, toxin exposure[5], cancer[11,12], infection, immunodeficiency[13] and organ transplantation[14]. In recent years, some resear
The results of the laboratory examination of patients with PH are generally nonspecific. The main manifestation is impaired liver function. Abnormal elevation of some biochemical indicators may indicate hepatocyte necrosis. The clinical manifestations also differ because of the different sizes of the lesions. When lesions are small, most patients do not present with any clinical symptoms[18]. But when lesions are large, some patients may present with abdominal distension, fatigue, loss of appetite and other symptoms. In addition, lesion rupture and bleeding may present as sudden severe abdominal pain and hemorrhagic shock[2,8,19].
The classic imaging features of PH are as follows: (1) the “capsule-in-capsule” sign, that is, multiple small sacs within a large lesion; and (2) fluid–fluid levels in the cyst (mixed old and new bleeding). The presentation of PH can be diverse depending on whether concomitant bleeding is present and the imaging characteristics of each period of bleeding[9]. Plain CT scan revealed the presence of equal- or high-density changes in low-density opacities. Enhanced scan can reveal the following[20-23]: (1) Persistent weak enhancement: lesions are relatively low- or equal-density in the arterial phase, portal phase and delayed phase. When the lesions are large and combined with hemorrhage and necrosis, they may present with solid margins with partial weak enhancement similar to the present case; (2) Centripetal enhancement: the lesion margin exhibits annular or nodular enhancement in the arterial phase and gradually spread to the center of the lesion in the portal phase and delayed phase; and (3) Persistent and obvious enhancement: significant nodular or patchy enhancement of the lesion is present in the arterial phase; the lesion is relatively dense in the portal phase, and the density gradually decreases in the delayed phase. Plain magnetic resonance imaging scan T1WI showed mostly low signal and T2WI showed mostly high signal. T1WI can show equal- or high-density signal with concomitant bleeding. When the bleeding in the lesion is both new and old, the “liquid–liquid level” sign can be seen. The presentation on enhanced scan is consistent with that on enhanced CT[5,20,21].
Asymptomatic patients with small PH lesions can be followed up for observation. For those with large lesions, lesion rupture and bleeding are usually prevented via surgical resection[5]. The most fundamental treatment for this disease involves eliminating or controlling its pathological factors. Thereafter, the prognosis is good, and recurrence is rare. But the present case experienced recurrence at 1 year after operation, strongly suggesting that hidden pathogenic factors may not have been addressed in this case.
The imaging presentation of PH is complex and diverse. When the imaging diagnosis does not correspond with the clinical history and laboratory examination, the possibility of this disease should be considered. However, pathological examination is required for a final diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karavaş E S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Schoenlank W. Ein fall von peliosis hepatis. Virchows Arch Path Anat 1916;222: 358-364 . [RCA] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Chen CY, Wang YP, Lu CL. An Unusual Hepatic Mass in a Young Man. Gastroenterology. 2019;157:e4-e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Dave YA, Gupta A, Shah MM, Carpizo D. Liver haematoma as a presentation of peliosis hepatis. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Atila K, Coker A, Uçar D, Karademir S, Sağol O, Astarcioğlu H, Astarcioğlu I. A rare clinical entity misdiagnosed as a tumor: peliosis hepatis. Ulus Travma Acil Cerrahi Derg. 2007;13:149-153. [PubMed] |
| 5. | Crocetti D, Palmieri A, Pedullà G, Pasta V, D'Orazi V, Grazi GL. Peliosis hepatis: Personal experience and literature review. World J Gastroenterol. 2015;21:13188-13194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 49] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Liu J, Wang Y, Yin S, Ke N, Liu X. Huge peliosis hepatis mimicking cystic echinococcosis: A case report. Medicine (Baltimore). 2019;98:e18141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Zucchetti BM, Shimada A, Siqueira LT. Peliosis Hepatis Simulates Liver Metastases. J Glob Oncol. 2018;4:1-3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Berkowitz ST, Gannon KM, Carberry CA, Cortes Y. Resolution of spontaneous hemoabdomen secondary to peliosis hepatis following surgery and azithromycin treatment in a Bartonella species infected dog. J Vet Emerg Crit Care (San Antonio). 2016;26:851-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Dai YN, Ren ZZ, Song WY, Huang HJ, Yang DH, Wang MS, Huang YC, Chen MJ, Zhang JJ, Tong YX, Pan HY. Peliosis hepatis: 2 case reports of a rare liver disorder and its differential diagnosis. Medicine (Baltimore). 2017;96:e6471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Tsukamoto Y, Kiyasu J, Utsunomiya H, Nakashima Y, Choi I, Suehiro Y, Aratake Y, Abe Y. Danazol-induced peliosis hepatis accompanied by disseminated intravascular coagulation in a patient with myelodysplastic syndrome transformed from aplastic anemia. Rinsho Ketsueki. 2016;57:1026-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Wannesson L, Chigrinova E, Raditchkova M, Mazzucchelli L, Ghielmini M. Peliosis hepatis in cancer patients mimicking infection and metastases. Onkologie. 2009;32:54-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Slim R, Hachem N, Smayra V, Yaghi C, Daniel F, Boujaoude J, Honein K, Sayegh R, Ghosn M. Education and Imaging. Hepatobiliary and pancreatic: peliosis hepatis associated with multiple myeloma. J Gastroenterol Hepatol. 2014;29:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Sanz-Canalejas L, Gómez-Mampaso E, Cantón-Moreno R, Varona-Crespo C, Fortún J, Dronda F. Peliosis hepatis due to disseminated tuberculosis in a patient with AIDS. Infection. 2014;42:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Yu CY, Chang LC, Chen LW, Lee TS, Chien RN, Hsieh MF, Chiang KC. Peliosis hepatis complicated by portal hypertension following renal transplantation. World J Gastroenterol. 2014;20:2420-2425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Funayama K, Shimizu H, Tanaka H, Kawachi I, Nishino I, Matsui K, Takahashi N, Koyama A, Katsuragi-Go R, Higuchi R, Aoyama T, Watanabe H, Kakita A, Takatsuka H. An autopsy case of peliosis hepatis with X-linked myotubular myopathy. Leg Med (Tokyo). 2019;38:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Butt MO, Luck NH, Hassan SM, Abbas Z, Mubarak M. Peliosis Hepatis Complicating Pregnancy: A Rare Entity. J Transl Int Med. 2017;5:132-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Iwata T, Adachi K, Takahashi M. Peliosis Hepatis Mimicking Malignant Hypervascular Tumors. J Gastrointest Surg. 2017;21:1095-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Tan CHN, Soon GST, Kow WCA. Liver lesions detected in a hepatitis B core total antibody-positive patient masquerading as hepatocellular carcinoma: a rare case of peliosis hepatis and a review of the literature. Ann Hepatobiliary Pancreat Surg. 2017;21:157-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Mascagni P, Melandro F, Larghi Laureiro Z, Mennini G, Rossi M. Spontaneous hepatic rupture in a bodybuilder: a case report and review of the literature. Rev Esp Enferm Dig. 2018;110:254-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Kim SH, Lee JM, Kim WH, Han JK, Lee JY, Choi BI. Focal peliosis hepatis as a mimicker of hepatic tumors: radiological-pathological correlation. J Comput Assist Tomogr. 2007;31:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Ferrozzi F, Tognini G, Zuccoli G, Cademartiri F, Pavone P. Peliosis hepatis with pseudotumoral and hemorrhagic evolution: CT and MR findings. Abdom Imaging. 2001;26:197-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Gouya H, Vignaux O, Legmann P, de Pigneux G, Bonnin A. Peliosis hepatis: triphasic helical CT and dynamic MRI findings. Abdom Imaging. 2001;26:507-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Kim SB, Kim DK, Byun SJ, Park JH, Choi JY, Park YN, Kim DY. Peliosis hepatis presenting with massive hepatomegaly in a patient with idiopathic thrombocytopenic purpura. Clin Mol Hepatol. 2015;21:387-392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |