Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5179
Peer-review started: February 13, 2021
First decision: March 14, 2021
Revised: March 21, 2021
Accepted: April 25, 2021
Article in press: April 25, 2021
Published online: July 6, 2021
Processing time: 130 Days and 15.9 Hours
Portal vein thrombosis (PVT) was previously a contraindication for trans-jugular intrahepatic portosystemic shunt (TIPS).
To perform a systematic review and meta-analysis of the current available studies investigating outcomes of TIPS for cirrhotic patient with PVT.
Multiple databases were systematically searched to identify studies investigating the outcomes of TIPS for cirrhotic patients with PVT. The quality of studies was assessed by Cochrane Collaboration method and Methodological Index for Non-Randomized Studies. The demographic data, outcomes, combined treatment, and anticoagulation strategy were extracted.
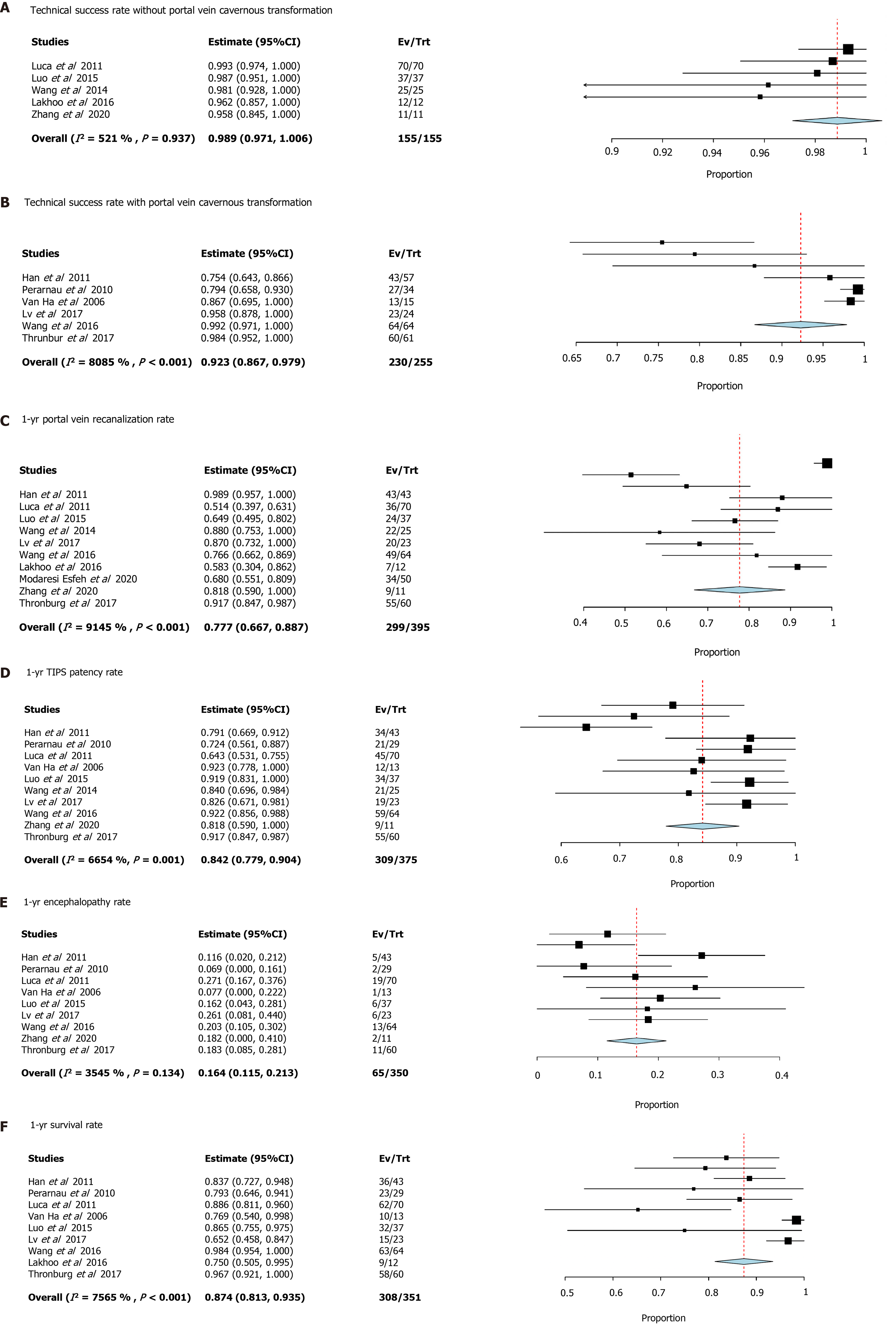
Twelve studies were identified with 460 patients enrolled in the analysis. The technical success rate was 98.9% in patients without portal vein cavernous transformation and 92.3% in patients with portal vein cavernous transformation. One-year portal vein recanalization rate was 77.7%, and TIPS patency rate was 84.2%. The cumulative encephalopathy rate was 16.4%. One-year overall survival was 87.4%.
TIPS is indicated for portal hypertension related complications and the restoration of pre-transplantation portal vein patency in cirrhotic patients with PVT. Cavernous transfor
Core Tip: Trans-jugular intrahepatic portosystemic shunt (TIPS) is indicated for portal hypertension related complications and the restoration of pre-transplantation portal vein patency in cirrhotic patients with portal vein thrombosis. Cavernous transformation is an indicator for technical failure. Post-TIPS anticoagulation seems not mandatory. Simultaneous TIPS and percutaneous mechanical thrombectomy device could achieve accelerated portal vein recanalization and decreased thrombolysis-associated complications, but further investigation is still needed.
- Citation: Zhang JB, Chen J, Zhou J, Wang XM, Chen S, Chu JG, Liu P, Ye ZD. Systematic review and meta-analysis of trans-jugular intrahepatic portosystemic shunt for cirrhotic patients with portal vein thrombosis. World J Clin Cases 2021; 9(19): 5179-5190
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5179.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5179
Portal vein thrombosis (PVT) refers to thrombosis within the portal vein, including main trunk, splenic, or mesenteric vein. The prevalence of PVT in cirrhotic patients can reach to 36%, depending on the severity of liver disease and diagnostic method[1,2]. Trans-jugular intrahepatic portosystemic shunt (TIPS) is indicated for cirrhotic patients with refractory ascites and variceal bleeding not controlled with medical or endoscopic therapy[3,4].
In cirrhotic patients with PVT, increased portal hypertension, decreased liver perfusion, and worsened liver function may occur[5]. Initially, PVT was regarded as contraindication for TIPS because of the technical difficulties, especially in patients with portal vein cavernous transformation[6]. However, some investigator attempted to carry out TIPS in cirrhotic patients with PVT and achieved good results[7]. The theoretical basis is that TIPS can increase portal blood velocity, resulting in clot resorption and portal vein recanalization.
However, most of the relevant studies were anecdote-based, and the sample sizes were relatively small. At present, only limited data are available for TIPS in cirrhotic patients with PVT. Therefore, we wanted to review systematically the published data of TIPS for cirrhotic patients with PVT.
MEDLINE, CNKI, Google Scholar, EMBASE, and Cochrane database were systematically searched for all relevant published studies evaluating outcomes following TIPS in cirrhotic patients with PVT. Several combinations of search terms were used, including “trans-jugular intrahepatic portosystemic shunt,” “portal vein thrombosis,” “cavernous transformation,” “liver cirrhosis,” “variceal bleeding,” and “early TIPS.” Moreover, some journals in interventional radiology, gastroenterology, and vascular surgery were reviewed manually for relative articles.
Titles and abstracts of the papers were screened first. Only studies evaluating outcomes following TIPS in cirrhotic patients with PVT were included. Case reports and review articles were excluded.
Quality of randomized controlled trials were assessed using Cochrane Collaboration method. Quality of non-randomized studies were assessed using Methodological Index for Non-Randomized Studies scale[8].
Demographics and outcome data were extracted for each eligible paper. Demographic data included: (1) etiology of liver cirrhosis, (2) symptom and comorbidity, (3) thrombosis characteristics, (4) technical details, and (5) periprocedural anticoagulative strategies. Outcome data included: (1) technical success rate, (2) portal vein recanalization rate, (3) TIPS patency, (4) hepatic encephalopathy rate, and (5) survival.
Intraclass correlation coefficient was calculated for evaluating the level of agreement between investigators assessing the study quality. means ± SD of both Methodological Index for Non-Randomized Studies score and Cochrane Collaboration method score were calculated.
Funnel plot was used for assessing publication bias. Study heterogeneity was tested using Q statistic, with P < 0.1 indicating significance. SPSS 22 (SPSS Inc., Armonk, NY, United States) and Open Meta-Analyst software (http://www.cebm.brown.edu/openmeta/download.html) were used for data analysis.
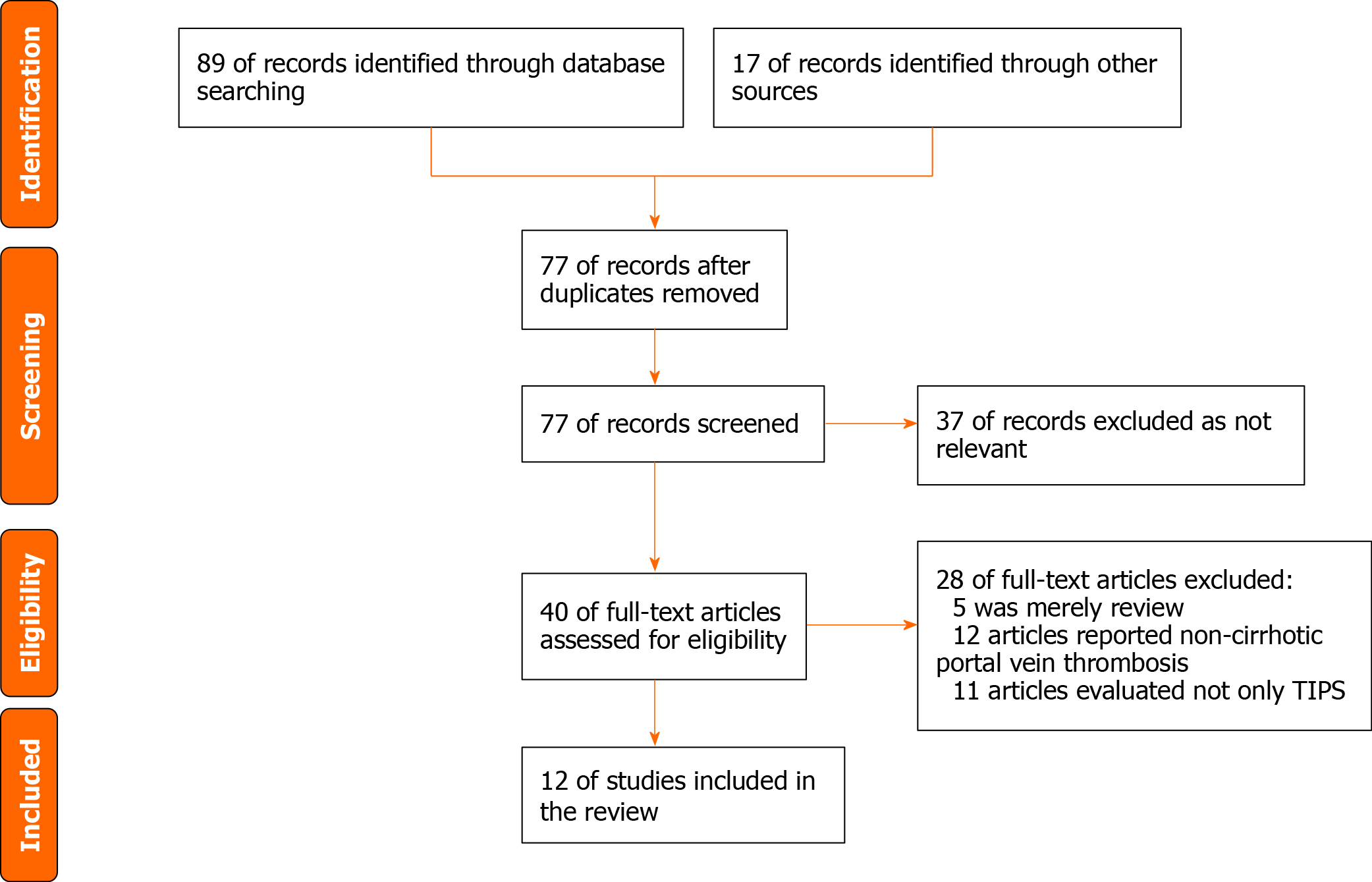
Twelve papers published over the past 15 years, reporting a total of 460 patients, were included in the study[1,2,4,9-17] (Figure 1). The included study characteristics are shown in Table 1. Of these studies, nine were retrospective and three were rando
| Ref. | Time period | Publication year | Country | Design | Inclusion criteria | Exclusion criteria | End point |
| Han et al[9] | December 2001-September 2008 | 2011 | China | Retrospective | Definite diagnosis of PVT; concomitant decompensated cirrhosis; absence of malignancy; absence of previous primary thrombosis of the hepatic vessels; absence of pancreatitis, appendicitis, and splenectomy by trauma | Patients with thrombosis, in other segments of the portal system rather than the main portal vein (MPV) or with MPV stenosis < 50% within MPV | Technical success and portal vein recanalization; procedure-related complications; shunt dysfunction and revision; hepatic encephalopathy; overall survival |
| Perarnau et al[10] | 1990-2004 | 2010 | France | Retrospective | Patient received TIPS with complete portal thrombosis | Lack of cirrhosis (Chiari syndrome, noncirrhotic portal hypertension, metastatic breast cancer); TIPS performed in transplanted liver; hepatocellular carcinoma; unfulfilled medical records | Technical success; early complications; long-term patency; hepatic encephalopathy; survival |
| Luca et al[11] | January 2003-February 2010 | 2011 | Italy | Retrospective | Patient have associated portal vein thrombosis prior to TIPS | Non-cirrhotic patient; Thrombosis limited to right and/or left portal branch; hepatocellular carcinoma; did not undergo imaging study prior or after TIPS | Technical success; recanalization of portal vein; complications and survival |
| Van Ha et al[4] | December 1995-December 2003 | 2006 | United States | Retrospective | Liver cirrhotic patient with portal vein thrombosis received TIPS | N/A | Technical success; TIPS patency; hepatic encephalopathy; survival |
| Luo et al[1] | January 2010-December 2012 | 2015 | China | RCT | Patients with cirrhosis and PVT, aged 18-70 yr, previous episodes of variceal bleeding, and a Child-Pugh score of 7-13 | PVT of 25% or less within the vessel lumen; limited thrombosis in the intrahepatic portal branch; portal cavernoma; gastric varices; hepatocellular carcinoma; previous endoscopic treatment of varices within 3 mo; and contradictions to TIPS, EBL, or propranolol | The primary end point was the incidence of recurrent variceal bleeding. The secondary end points were incidence of TIPS dysfunction, recanalization of the portal venous system, occurrence of hepatic encephalopathy, or death for any reason |
| Wang et al[2] | January 2010-September 2010 | 2014 | China | Retrospective | Patients with cirrhosis and concomitant PVT who underwent successful TIPS creation | N/A | Rebleeding events; changes in PVT; survival |
| Lv et al[12] | May 2011-January 2014 | 2017 | China | RCT | Liver cirrhosis (diagnosed by clinical presentations, laboratory tests, images or liver biopsies), age between 18 and 75 yr, PVT > 50% of the portal vein trunk and a history of endoscopy-proven variceal bleeding in the past 6 wk | Uncontrolled active variceal bleeding; technical impracticality of TIPS; previous EBL + NSBB, TIPS placement or shunt surgery; concomitant renal insufficiency; severe cardiopulmonary diseases; uncontrolled systemic infection or sepsis; hepatocellular carcinoma or other extrahepatic malignancy; and contraindications for propranolol, anticoagulation or TIPS | The primary endpoint was variceal rebleeding; The secondary endpoints included survival, overt hepatic encephalopathy, portal vein recanalization and re-thrombosis, other complications of portal hypertension and adverse effects |
| Wang et al[13] | October 2012-February 2014 | 2016 | China | RCT | Patients with cirrhosis and PVT who were undergoing TIPS placement | Technical failure of TIPS; a thrombus limited to the intrahepatic portal branches; diffuse PVT involving the entire portal venous system; a contraindication to anticoagulation therapy; already undergoing anticoagulation or antiplatelet aggregation therapy; platelet count of less than 20000/mm3 or international normalized ratio greater than 2; a malignancy or myeloproliferative disorder; refusal to participate or enroll in another prospective study | The primary outcome measure was a change in portal vein patency status; secondary outcomes were gastrointestinal bleeding, shunt dysfunction, hepatic encephalopathy, and survival |
| Lakhoo and Gaba[14] | December 2008-March 2014 | 2016 | United States | Retrospective | Patient underwent TIPS for PVT | Patients who lacked cross-sectional imaging follow-up after TIPS | The primary endpoint was post-TIPS spleno-mesenteric-portal venous patency; Secondary endpoint included durability of patency, patient transplant free survival, liver transplant rate, and post-TIPS variceal bleeding incidence |
| Modaresi Esfeh and Ansari-Gilani[15] | January 2020-December 2018 | 2020 | United States | Retrospective | Patient with PVT before TIPS placement | N/A | Primary endpoint was recanalization of the portal vein within the first year following TIPS placement |
| Zhang et al[16] | March 2018-April 2019 | 2020 | China | Retrospective | Clearly diagnosed cirrhotic patient with portal vein thrombosis (≤ 2 wk), with visceral bleeding or ascites; thrombosis involved at least 2 branches of superior mesenteric vein, splenic vein and inferior mesenteric vein; contraindication for catheter-directed thrombosis | Merely mural portal thrombosis or the thrombosis is regional; sub-acute or chronic PVT; patient without cirrhosis and portal hypertension; above Child-Pugh C category or coagulation disorders | Portal vein recanalization; TIPS patency; peri-operative complications; encephalopathy |
| Thornburg et al[17] | 2009-2015 | 2017 | United States | Retrospective | Medical need for transplantation and presence of chronic PVT on pre-operative imaging | The inability to be listed for transplantation for reasons other than the presence of PVT and complete, chronic portomesenteric thrombosis precluding catheterization of the portal vein or splenic vein | Portal vein and TIPS patency before and after transplantation; clinical and laboratory adverse events; survival |
Except for one that did not report indication[13], the main indication for TIPS was to treat complications of portal hypertension. Treating gastrointestinal variceal bleeding or preventing re-bleeding was reported in 77.01% of patients, and treating refractory ascites or pleural effusion was reported in 15.82% of patients. In one study[17], TIPS was utilized for the restoration of portal vein patency.
Demographics and results of the included studies are shown in Table 2.
| Ref. | No. | Male, n | Age in yr | TIPS success rate, % | Cavernoma, n | 1-yr portal vein recanalization rate, % | 2-yr portal vein recanalization rate, % | 1-yr TIPS patency, % | Encephalopathy rate, % | Survival rate, % | Combined treatment | Follow-up time |
| Han et al[9] | 57 | 20 | 50.9 ± 1.6 | 75 | 30 | 100 | 68.2 | 79.3 | 1-yr 25; 2-yr 27 | 1-yr 86.1; 5-yr 76.7 | Anti-coagulation, heparin-warfarin-aspirin | 5 yr |
| Perarnau et al[10] | 34 | 18 | 58 ± 11 | 79 | 19 | N/A | N/A | 72 | 6.9 | 1-yr 80; 4-yr 55 | Heparin for 10 d, prolong to 20 d in patients with thrombocytopenia | 4 yr |
| Luca et al[11] | 70 | 47 | 55 ± 8 | 100 | 0 | 51 | 81 | 64.3 | 1-yr 27; 2-yr 32 | 1-yr 89; 2-yr 81 | N/A | 4 yr |
| Van Ha et al[4] | 15 | 13 | 53 | 86.7 | 4 | N/A | N/A | 92.3 | 7.7 | 76.9 | Heparin-warfarin in 2 cases, heparin in 2 cases | Mean 17 mo |
| Luo et al[1] | 37 | 19 | 50.78 ± 13.61 | 100 | 0 | 64.9 | 71.3 | 91.7 | 1-yr 16.2; 2-yr 38.5 | 1-yr 86.5; 2-yr 72.9 | Low molecular weight heparin for 3 d, bridge to warfarin for at least 6 mo | 2 yr |
| Wang et al[2] | 25 | 14 | 47.28 ± 12.36 | 100 | 0 | N/A | 87 | N/A | 1-yr 96; 3-yr 39.3 | Long-term warfarin | 3 yr | |
| Lv et al[12] | 24 | 13 | 49 (46-62) | 96 | 11 | 87 | 80 | 82.6 | 26.1 | 1-yr 83.5; 2-yr 73 | Thrombolysis in 5 cases, anti-coagulation in 22 cases | 2 yr |
| Wang et al[13] | 64 | 38 | 54.76 | 100 | 4 | 76.6 | N/A | 92.2 | 1-yr 20.3 | 1-yr 98.4 | Anti-coagulation in 31 cases | 1 yr |
| Lakhoo and Gaba[14] | 12 | 5 | 63 | 100 | 0 | 58.3 | N/A | 92 | N/A | 75% | Anti-coagulation in 3 cases | Median 109 d |
| Modaresi Esfeh and Ansari-Gilani[15] | 50 | 34 | 55.3 ± 11 | 100 | N/A | 68 | N/A | N/A | N/A | N/A | N/A | N/A |
| Zhang et al[16] | 11 | 6 | 46 ± 9 | 100 | 0 | 81.8 | N/A | 81.8 | 18.2 | N/A | AngioJet and anti-coagulation | 1 yr |
| Thornburg et al[17] | 61 | 37 | 58 (median) | 98 | 29 | 92 | N/A | 92 | 18 | 5-yr 82 | N/A | 5 yr |
The overall technical success rate for TIPS was 94.6% (435/460) for all the included studies. In patients with portal vein cavernous transformation, the lowest technical success rate was 53.33%, as reported by Han et al[9]. The cumulative technical success rate was 98.9% in patients without portal vein cavernous transformation and 92.3% in patients with portal vein cavernous transformation[1,2,11,14,16]. Most of the TIPS was achieved through a traditional trans-jugular approach; trans-hepatic and trans-splenic approach was employed to facilitate portal recanalization or to target the punctured vessel.
One-year portal vein recanalization rate was 77.7%, and TIPS patency rate was 84.2%. TIPS combined with AngioJet thrombectomy device was reported by Zhang et al[16], and the portal vein recanalization rate was reported to be 81.8%. Luca et al[11] reported that independent predictors for portal vein recanalization were thrombosis of a single vein, PVT severity of grade I, de novo diagnosis of PVT, and absence of gastro-esophageal varices.
Nine studies[1,4,9-13,16,17] reported hepatic encephalopathy rate. The highest 1-year hepatic encephalopathy rate was 27%, reported by Luca et al[11]. The overall 1-year encephalopathy rate was 16.4%. The highest 2-year encephalopathy rate was 38.5%, reported by Luo et al[1].
Most of the studies reported 1-year survival rates, and they ranged from 75% to 98.4%. The overall 1-year survival was 87.4%. Two studies[9,17] reported a 5-year survival rates of 82% and 76.7%, respectively. Han et al[9] reported that both technical success and survival were closely associated with the degree of main portal vein occlusion.
Most studies did not have unified standard for anticoagulation strategy. Only one study[13] evaluated whether post-TIPS anticoagulation was necessary. The result showed that anticoagulation therapy may not be necessary in certain patients with PVT because TIPS placement alone can achieve a high persistent recanalization rate.
The primary etiology of PVT is decompensated cirrhosis, especially those with splenectomy. Patients with prior splenectomy have a higher incidence of PVT, which can influence the technical success and patency rate of TIPS[18]. We suggest that patients with portal hypertension should avoid splenectomy if they plan to receive TIPS treatment.
PVT in cirrhotic patients is most often asymptomatic and detected incidentally on routine ultrasound[19]. Spontaneous resolution occurs in approximately 40% of PVT[20]. Symptoms may vary from asymptomatic to life-threatening conditions related to portal hypertension and hepatic decompensation[21]. The treatment strategy for PVT includes anti-coagulation, thrombolysis, and thrombectomy. TIPS is an effective adjunctive therapy to recanalize the portal vein and reduce portal hypertension. For PVT patients with obvious portal hypertensive symptoms, such as recurrent gastrointestinal bleeding or refractory ascites, TIPS is the only way to improve hepatopetal flow and offers a low-resistance outflow channel.
TIPS placement is challenging in advanced occlusive PVT thrombosis and portal vein cavernous transformation. As the current study reported, the lowest technical success rate was reported to be 53.33% in portal vein cavernous transformation[9]. Some investigators regarded portal cavernous transformation as a contraindication for TIPS because the original portal vein has been obliterated or has become a fibrotic cord[22]. It has come a long way from being a contraindication to an indication because of technical difficulties and frequent procedure related complications. Combined trans-jugular/trans-hepatic or trans-jugular/trans-splenic approach could improve technical success rate[23].
The successful employment of percutaneous mechanical thrombectomy device in PVT has been reported[24,25]. It is more suitable for acute or subacute PVT with accelerated portal vein recanalization and decreased thrombolysis-associated complications. Simultaneous creation of TIPS could reconstruct portal outflow and further improve therapeutic effect. But most of the associated studies were case reports or small case series. Larger patient cohorts should be evaluated for further analysis.
PVT was thought to have a negative impact on liver cirrhosis progression and patient survival because it further increased portal hypertension, which may lead to life-threating complications and worsening liver function[21]. A meta-analysis including 2436 cirrhotic patients suggested that PVT appears to increase mortality and ascites[26]. In the current study, TIPS could not improve the survival of cirrhotic patients with PVT but could alleviate the portal hypertension related complications and improve quality of life, without an increase in hepatic encephalopathy.
Another indication of TIPS for cirrhotic patients with PVT was to maintain pre-transplantation portal vein patency. Portal vein recanalization-TIPS is a concept aimed at achieving portal vein recanalization in chronic PVT[27]. In these patients, the stent should be implanted in the main portal vein as short as possible to reserve sufficient non-stented PV for end-to-end anastomosis during liver transplantation.
Wang et al[13] suggested that increased portal blood velocity after TIPS may offset the hypercoagulable state and result in portal recanalization even without anticoagulation. In addition, the safety of anticoagulation drugs is also a problem, especially in cirrhotic patients. The study, however, did not included PVT in the entire portal venous system because TIPS procedure in those patients is quite difficult. Thus, the value of post-TIPS anticoagulation should be further investigated in patients with diffuse PVT.
Limitations may exist in our study. First, the pooled analysis was based on study-level data (Figure 2). Second, only three of the included studies were random controlled trials, and the others were retrospective cohort studies. Therefore, heterogeneity may exist among the studies.
In conclusion, TIPS is indicated for portal hypertension related complications and the restoration of pre-transplantation portal vein patency in cirrhotic patients with PVT. Cavernous transformation is an indicator for technical failure. Post-TIPS anticoagulation seems not mandatory. Simultaneous TIPS and percutaneous mechanical thrombectomy device could achieve accelerated portal vein recanalization and decreased thrombolysis-associated complications, but further investigation is still needed.
In clinical practice, portal vein thrombosis (PVT) was previously a contraindication for trans-jugular intrahepatic portosystemic shunt (TIPS).
Evaluating TIPS utility in the management of cirrhotic patients with PVT.
To review systematically the current evidence of TIPS in the management of cirrhotic patients with PVT.
Search and evaluate the relevant published paper and then extract and analyze the key data.
TIPS can be safely carried out using a different approach in cirrhotic patient with PVT. However, in patients with cavernous transformation, it is relatively difficult.
TIPS is indicated for portal hypertension related complications and the restoration of pre-transplantation portal vein patency in cirrhotic patients with PVT. Cavernous transformation is an indicator for technical failure.
TIPS could be carried out in most of cirrhotic patients with PVT. We plan to carry out a similar study with a prospective design to evaluate TIPS utility for patients with PVT.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Garbuzenko DV S-Editor: Gao CC L-Editor: Filipodia P-Editor: Wang LL
| 1. | Luo X, Wang Z, Tsauo J, Zhou B, Zhang H, Li X. Advanced Cirrhosis Combined with Portal Vein Thrombosis: A Randomized Trial of TIPS vs Endoscopic Band Ligation Plus Propranolol for the Prevention of Recurrent Esophageal Variceal Bleeding. Radiology. 2015;276:286-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 2. | Wang Z, Zhao H, Wang X, Zhang H, Jiang M, Tsauo J, Luo X, Yang L, Li X. Clinical outcome comparison between TIPS and EBL in patients with cirrhosis and portal vein thrombosis. Abdom Imaging. 2015;40:1813-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | García-Pagán JC, Caca K, Bureau C, Laleman W, Appenrodt B, Luca A, Abraldes JG, Nevens F, Vinel JP, Mössner J, Bosch J; Early TIPS (Transjugular Intrahepatic Portosystemic Shunt) Cooperative Study Group. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-2379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 826] [Cited by in RCA: 842] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 4. | Van Ha TG, Hodge J, Funaki B, Lorenz J, Rosenblum J, Straus C, Leef J. Transjugular intrahepatic portosystemic shunt placement in patients with cirrhosis and concomitant portal vein thrombosis. Cardiovasc Intervent Radiol. 2006;29:785-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Englesbe MJ, Kubus J, Muhammad W, Sonnenday CJ, Welling T, Punch JD, Lynch RJ, Marrero JA, Pelletier SJ. Portal vein thrombosis and survival in patients with cirrhosis. Liver Transpl. 2010;16:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 185] [Article Influence: 12.3] [Reference Citation Analysis (2)] |
| 6. | Copelan A, Kapoor B, Sands M. Transjugular intrahepatic portosystemic shunt: indications, contraindications, and patient work-up. Semin Intervent Radiol. 2014;31:235-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 7. | Senzolo M, Tibbals J, Cholongitas E, Triantos CK, Burroughs AK, Patch D. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with and without cavernous transformation. Aliment Pharmacol Ther. 2006;23:767-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3743] [Cited by in RCA: 5641] [Article Influence: 256.4] [Reference Citation Analysis (0)] |
| 9. | Han G, Qi X, He C, Yin Z, Wang J, Xia J, Yang Z, Bai M, Meng X, Niu J, Wu K, Fan D. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol. 2011;54:78-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 187] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 10. | Perarnau JM, Baju A, D'alteroche L, Viguier J, Ayoub J. Feasibility and long-term evolution of TIPS in cirrhotic patients with portal thrombosis. Eur J Gastroenterol Hepatol. 2010;22:1093-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Luca A, Miraglia R, Caruso S, Milazzo M, Sapere C, Maruzzelli L, Vizzini G, Tuzzolino F, Gridelli B, Bosch J. Short- and long-term effects of the transjugular intrahepatic portosystemic shunt on portal vein thrombosis in patients with cirrhosis. Gut. 2011;60:846-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 197] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 12. | Lv Y, Qi X, He C, Wang Z, Yin Z, Niu J, Guo W, Bai W, Zhang H, Xie H, Yao L, Wang J, Li T, Wang Q, Chen H, Liu H, Wang E, Xia D, Luo B, Li X, Yuan J, Han N, Zhu Y, Xia J, Cai H, Yang Z, Wu K, Fan D, Han G; PVT-TIPS Study Group. Covered TIPS vs endoscopic band ligation plus propranolol for the prevention of variceal rebleeding in cirrhotic patients with portal vein thrombosis: a randomised controlled trial. Gut. 2018;67:2156-2168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 140] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 13. | Wang Z, Jiang MS, Zhang HL, Weng NN, Luo XF, Li X, Yang L. Is Post-TIPS Anticoagulation Therapy Necessary in Patients with Cirrhosis and Portal Vein Thrombosis? Radiology. 2016;279:943-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 14. | Lakhoo J, Gaba RC. Outcomes of transjugular intrahepatic portosystemic shunt creation for flow-enabled dissolution of spleno-mesenterico-portal venous thrombosis. Diagn Interv Imaging. 2016;97:1085-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Modaresi Esfeh J, Ansari-Gilani K. Transjugular intrahepatic portosystemic shunt in cirrhotic patients with portal vein thrombosis. Eur J Gastroenterol Hepatol. 2020;32:762-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Zhang WW, Ren JZ, Han XW, Chen PF, Li FZ, Kuang DL, Zhou PL, Ding PX, Bi YH. [Clinical application and efficacy of TIPS combined with AngioJet mechanical thrombectomy for liver cirrhosis with extensive portal vein thrombosis]. Zhonghua Yi Xue Za Zhi. 2020;100:533-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Thornburg B, Desai K, Hickey R, Hohlastos E, Kulik L, Ganger D, Baker T, Abecassis M, Caicedo JC, Ladner D, Fryer J, Riaz A, Lewandowski RJ, Salem R. Pretransplantation Portal Vein Recanalization and Transjugular Intrahepatic Portosystemic Shunt Creation for Chronic Portal Vein Thrombosis: Final Analysis of a 61-Patient Cohort. J Vasc Interv Radiol 2017; 28: 1714-1721. e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 18. | Dong F, Luo SH, Zheng LJ, Chu JG, Huang H, Zhang XQ, Yao KC. Incidence of portal vein thrombosis after splenectomy and its influence on transjugular intrahepatic portosystemic shunt stent patency. World J Clin Cases. 2019;7:2450-2462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 19. | Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, Development, and Treatment of Portal Vein Thrombosis in Patients With and Without Cirrhosis. Gastroenterology 2019; 156: 1582-1599. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 249] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 20. | Qi X, Guo X, Yoshida EM, Méndez-Sánchez N, De Stefano V, Tacke F, Mancuso A, Sugawara Y, Yang SS, Teschke R, Arora A, Valla DC. Transient portal vein thrombosis in liver cirrhosis. BMC Med. 2018;16:83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 21. | Faccia M, Ainora ME, Ponziani FR, Riccardi L, Garcovich M, Gasbarrini A, Pompili M, Zocco MA. Portal vein thrombosis in cirrhosis: Why a well-known complication is still matter of debate. World J Gastroenterol. 2019;25:4437-4451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 44] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 22. | Jiang ZB, Shan H, Shen XY, Huang MS, Li ZR, Zhu KS, Guan SH. Transjugular intrahepatic portosystemic shunt for palliative treatment of portal hypertension secondary to portal vein tumor thrombosis. World J Gastroenterol. 2004;10:1881-1884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Li ZP, Wang SS, Wang GC, Huang GJ, Cao JQ, Zhang CQ. Transjugular intrahepatic portosystemic shunt for the prevention of recurrent esophageal variceal bleeding in patients with cavernous transformation of portal vein. Hepatobiliary Pancreat Dis Int. 2018;17:517-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Sze DY, O'Sullivan GJ, Johnson DL, Dake MD. Mesenteric and portal venous thrombosis treated by transjugular mechanical thrombolysis. AJR Am J Roentgenol. 2000;175:732-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Wolter K, Decker G, Kuetting D, Trebicka J, Manekeller S, Meyer C, Schild H, Thomas D. Interventional Treatment of Acute Portal Vein Thrombosis. Rofo. 2018;190:740-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Stine JG, Shah PM, Cornella SL, Rudnick SR, Ghabril MS, Stukenborg GJ, Northup PG. Portal vein thrombosis, mortality and hepatic decompensation in patients with cirrhosis: A meta-analysis. World J Hepatol. 2015;7:2774-2780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 27. | Salem R, Vouche M, Baker T, Herrero JI, Caicedo JC, Fryer J, Hickey R, Habib A, Abecassis M, Koller F, Vogelzang R, Desai K, Thornburg B, Hohlastos E, Resnick S, Lewandowski RJ, Sato K, Ryu RK, Ganger D, Kulik L. Pretransplant Portal Vein Recanalization-Transjugular Intrahepatic Portosystemic Shunt in Patients With Complete Obliterative Portal Vein Thrombosis. Transplantation. 2015;99:2347-2355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 113] [Article Influence: 12.6] [Reference Citation Analysis (0)] |