Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5073
Peer-review started: February 25, 2021
First decision: April 4, 2021
Revised: April 19, 2021
Accepted: April 26, 2021
Article in press: April 26, 2021
Published online: July 6, 2021
Processing time: 118 Days and 22.1 Hours
Total arterial revascularization is associated with increased patency and long-term efficacy and decreased perioperative morbidity and mortality and incidence of cardiac-related events and sternal wound infection compared with conventional coronary artery bypass surgery (CABG), in which the left internal mammary artery (LIMA) is typically grafted to the left anterior descending artery with additional saphenous vein grafts often used. This study determined whether these favorable clinical results could be realized at the authors’ institute.
To summarize the early efficacy and clinical experience of individualized total arterial coronary artery bypass grafting surgery.
CABG was performed on 35 patients with non-single-vessel coronary artery disease by adopting total arterial grafts at Fourth Affiliated Hospital of Harbin Medical University between April 2016 and December 2019. LIMA was used in 35 patients, radial artery (RA) was used in 35 patients, and right gastroepiploic artery (RGEA) was used in 9 patients. Perioperative complications were observed, short-term graft patency rate was followed-up, and quality of life was assessed.
All patients underwent off-pump coronary artery bypass and the surgeries were successful. All of them were discharged without any complications or deaths. During the follow-up, it was found that patients’ angina symptoms were relieved and New York Heart Association classification for cardiac function was class I to class II. A total of 90 vessels were grafted with no occlusion for internal mammary artery, three occlusions for RA, and one occlusion for RGEA.
The individualized total arterial strategy based on the vessels targeting individual anatomic characteristics can achieve complete revascularization with satisfactory short-term grafting patency rate.
Core Tip: To determine whether total arterial revascularization is superior to conventional coronary artery bypass surgery (CABG), we observed the efficacy and clinical outcomes in patients receiving three major arterial grafts during arterial revascularization surgery. All patients were discharged without occurrence of death. Over a follow-up of 3 mo to 1 year, the number of anastomoses was high, the graft occlusion rate was low, and no severe complications occurred. The use of arterial conduits generally provides significantly better late survival especially in patients with multi-vessel coronary disease, cardiac event-free survival and improved health-related quality of life compared to conventional CABG.
- Citation: Chen WG, Wang BC, Jiang YR, Wang YY, Lou Y. Clinical application of individualized total arterial coronary artery bypass grafting in coronary artery surgery. World J Clin Cases 2021; 9(19): 5073-5081
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5073.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5073
Coronary heart disease (CHD), a common clinical heart disease, is one of the diseases with the highest mortality rate worldwide[1]. Despite the continuous development of interventional techniques, coronary artery bypass grafting is still the ideal and standard treatment for multi-vessel coronary artery disease[2]. The long-term patency rate after coronary artery bypass surgery (CABG) is an important factor influencing the prognosis of patients. At present, an internal mammary artery and one or more great saphenous veins grafts (SVGs) are commonly used as conduit for transmyo
Thirty-five patients with CHD undergoing total arterial CABG at Fourth Affiliated Hospital of Harbin Medical University (Harbin, China) between April 2016 and December 2019 were selected as the study subjects (Table 1). There were 26 males and 9 females with an average age of 56 ± 8.75 years (range: 33 to 73 years), of whom 2 were over 70-years-old, 12 were diagnosed with diabetes mellitus, 6 underwent left main coronary artery surgery, 29 were diagnosed with multi-vessel disease, and 8 patients were diagnosed with acute myocardial infarction. Specifically, 35 patients received left internal mammary artery (LIMA) grafts and 35 received radial artery (RA) grafts including 12 who received bilateral RA grafts and 9 who received right gastroepiploic artery (RGEA) grafts during the CABG surgery.
| Clinical data | n (%) |
| Age (yr) | 56.5 ± 6.5 |
| Gender | |
| Male | 26 (74.3) |
| Female | 9 (25.7) |
| Hypertension | 22 (62.9) |
| Hyperlipemia | 7 (20.0) |
| Diabetes | 11 (31.4) |
| Myocardial infarction | 6 (17.1) |
| History of PCI | 0 (0) |
| Cerebrovascular accident | 4 (11.4) |
| Renal insufficiency | 2 (5.7) |
| Family history of coronary heart disease | 2 (5.7) |
| Smoking history | 15 (42.9) |
| Drinking history | 6 (17.1) |
| Cardiac functional grading | |
| Class II | 5 (20.0) |
| Class III | 30 (80.0) |
| History of atrial fibrillation | 1 (2.9) |
| Ejection fraction | 61.1 ± 5.5 |
Routine preoperative testing was carried out via coronary angiography, echocardiography, computed tomography (CT) chest scan, CT head scan, arterial blood gas analysis, and blood test to comprehensively assess the basic preoperative situations of patients. For patients with myocardial infarction or complicated with mitral regur
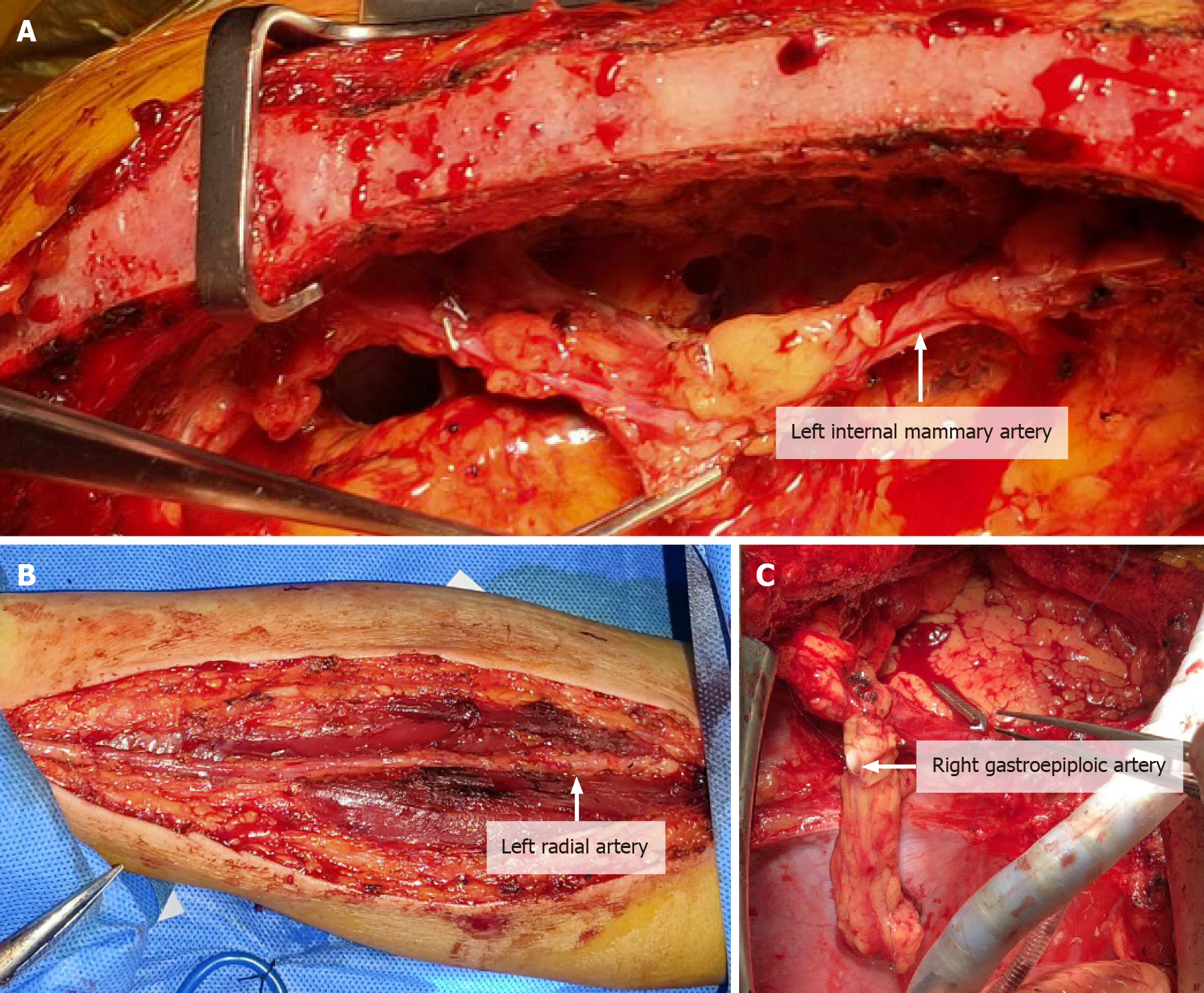
LIMA harvest: Median sternotomy was performed. The LIMA was separated from the branches to the first intercostal artery to the bifurcation of the internal mammary artery and the superior abdominal wall artery while branches along the way were clamped using titanium clips (Figure 1A).
RA harvest: RA incision extended from 2 cm to the elbow joint to transverse 2–3 cm incision in the wrist flexor fold. Arc incision was made along the RA pulse and around the medial to the edge of flexor carpi radialis. Always be mindful of preservation of the superficial branches to radial nerve and lateral cutaneous nerve of forearm. RA and its two accompanying satellite veins should be exposed and should be divided together using the “non-touch technique.” The branches should be treated with titanium clips to avoid spasticity. It is also suggested that papaverine saline should be used to spray, soak and wash and preserve branches (Figure 1B).
RGEA harvest: To harvest a GEA graft, the median sternotomy incision should be extended to 3–5 cm below the xiphoid process and entered the abdominal cavity. The RGEA was separated along the middle of the greater curvature of the stomach to the margin of pylorus. The branch vessels should be clamped using titanium clips and the branches on the side of the greater curvature of the stomach should be cut off. In addition, papaverine hydrochloride solution should be sprayed locally for standby use (Figure 1C).
Schemes were formulated for individualized total arterial revascularization CABG by comprehensively considering factors such as preoperative coronary angiography, distribution and calcification of target vessels during operation, heart size and the length of grafted vessel. A variety of conduits could be used for the surgery such as Y or T grafting configuration. If the length of LIMA was not long enough to be anastomosed with the anterior descending branch, or the flow rate was slightly poor, its diagonal branch could be selected to realize anastomosis. Actually, RA should be used to be anastomosed with the anterior descending branch. The median sternal incision was adopted and systemic heparin (1.5 mg/kg) was given to main the activated clotting time for more than 300 s. The ascending aorta was clamped with lateral forceps and the proximal end graft anastomoses should be managed firstly. Distal anastomosis and off pump coronary artery bypass (OPCAB) surgery was performed with anterior descending branch, diagonal branch, circumflex branch, right coronary artery or posterior descending branch and posterior branch of left ventricle selected as graft sequence. When RGEA was used, an incision was made on the diaphragm at the anastomotic position within the coronary artery, and then the artery was fixed on epicardium. At last, neutralization, hemostasis and sternal closure were performed.
After surgery, stable hemodynamic level and internal environment should be maintained. Myocardial markers were monitored regularly to ensure adequate volume and avoid using large dose of alpha receptor agonists. Considering the characteristics of spasticity for vessel grafts, apart from the no-touch technique used during the operation, continuous intravenous pumping of diltiazem (0.5 to 1 μg/kg per min) should also be administered during the operation and within 48 h after the operation. Moreover, oral diltiazem should be given to patients up to 1 year after surgery. If drainage decreased after the surgery, low molecular weight heparin could be injected subcutaneously on the first postoperative day or in the morning on the next day twice a day for 5 to 7 d. In addition, antiplatelet agents such as Bayaspirin and clopido
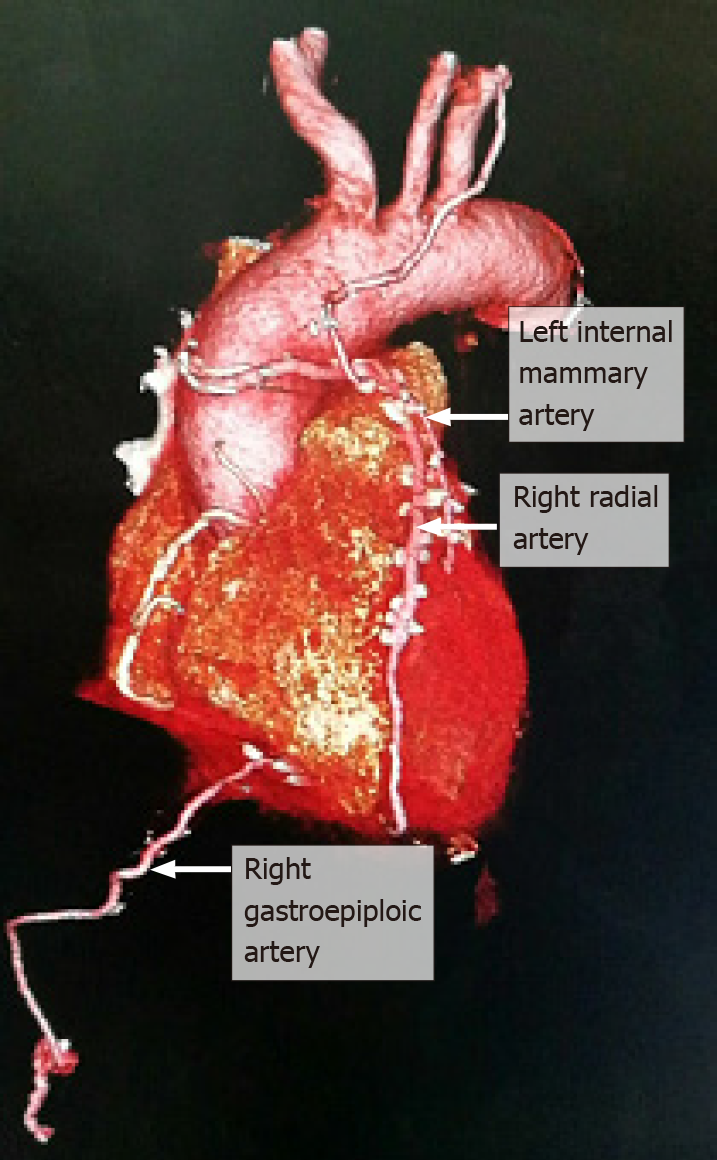
All 35 patients in the study underwent OPCAB. The surgeries were successful and all of them recovered and were discharged with no deaths reported. During the follow-up, all the symptoms of angina were relieved and the cardiac function class was between class I and class II. In general, a total of 90 vessels were grafted with an average of 2.6 vessels per person. LIMA was chosen in 35 patients, RA was chosen in 35 patients including bilateral harvesting of RA in 12 patients and RGEA in 9 patients. During a 3-mo to 1-year follow-up, no occlusion was discovered for LIMA graft and RA graft occlusion occurred in 3 patients with graft occlusion rate of 6.5% and occlusion of RGEA occurred in 1 patient with graft occlusion rate of 11.1%. Graft occlusion rate was 6.2% in patients with diabetics. No graft occlusion was observed in patients over 70 years old. Two patients had mild numbness in left forearm and left thumb and returned to normal at 1 wk after surgeries, with no other complications of forearm and hand and no abdominal complications such as gastrointestinal complications (Figure 2).
In 1967, Favaloro and Johnson succeeded in using greater saphenous vein (GSV) as a bypass conduit for the grafting procedure between the aorta and a coronary artery. Since then, the said method has been introduced and popularized rapidly because of its definite curative effect. Subsequently, it has become the main surgical treatment for CHD. However, after years of follow-up and observation, it was found that the GSV was prone to intimal hyperplasia and sclerosis, and the long-term patency rate was low with a 10-year patency rate of merely 50%[4]. As far as conduit materials are concerned, artery graft showed superior long term potency to SVG. In the literature, studies have confirmed that use of more than two artery conduits is associated with decreased mortality or improved long-term survival[5]. Benefits due to the use of conduit was not only limited to its excellent long-term patency but was also involved its protection of coronary circulation[6]. It is the development tendency of CABG to preferably use arterial conduits to take the place of SVG and gradually achieve multi-arterial and even total arterial revascularization.
LIMA, the gold standard choice as an arterial conduit for CABG, has a sound long-term patency rate. As space is limited, the detailed advantages of LIMA will not be elaborated upon here. However, it is impossible to achieve revascularization for all target vessels due to the limited length. The clinical application of other arterial conduits is a good supplement to LIMA such as RIMA, RA, right gastroepiploic artery, inferior epigastric artery, and descending branch of lateral circumflex femoral artery. In view of the fact that the use of bilateral LIMA grafts may aggravate postoperative pain, reduce sternum perfusion, as well as increase the probability of non-healing sternum and incision and the probability of sternal wound infection and deep infection[7], the authors’ department has not adopted it extensively. Regarding inferior epigastric artery and descending branch of lateral circumflex femoral artery, they have been rarely used in clinical practice because of issues such as subsidiary injury and poor long-term patency.
Attention is raised to RA because of the advantages such as easy access to easy to anatomy harvest, suitable caliber, all-round use, manageability, less complications, and less influence on forearm blood flow. A total of 46 RA grafts were used in 35 patients in the authors’ department and 3 of them were occluded in short-term period with an occlusion rate of 6.5%. There was no significant difference when compared with the occlusion rate of 6.7% reported by Cao et al[8]. Nevertheless, it was slightly lower when compared with the 1-year occlusion rate of 8.2% for coronary angiography reported in a study by Desai et al[9]. The author believes that two of the occlusions were associated with the use of right RA which underwent coronary angiography before operation. Besides, time interval between the operation and angiography was only 1 or 2 d. Although preoperative vascular ultrasound confirmed that the blood flow was unobstructed and occlusion 2 cm from the puncture was removed during the operation, the occlusion rate was still high. Zacharias et al[10] believe that preoperative angiography of right RA may cause damages to the integrity and function of the endothelium of RA. Moreover, the damages cannot be completely recovered even at 15 d after the operation. Gaudino et al[11] even believe that the damages may extend to 30 d. In addition, of the three occluded radial arteries, two were anastomosed with the diagonal branch, which is thought to be associated with the competitive flow after recanalization of LIMA and anterior descending artery. It is worth mentioning that the existence of competitive flow may lead to the decrease of blood flow and accelerate its occlusion. Therefore, in the CABG guidelines jointly formulated by the American College of Cardiology Foundation and the American Heart Association in 2011, RA grafting was recommended (class IIb) in left coronary artery (coronary artery stenosis > 70%) or right coronary artery (coronary artery stenosis ≥ 90%) bypass grafting surgeries[12]. In this study, the graft occlusion rate was 6.2% in diabetic patients and no graft occlusion was observed in patients over 70-years-old, which was not significantly different from the reports made by Habib et al[13] and Hoffman et al[14]. It showed that diabetes and age over 70-years-old were not contraindications to RA harvesting. By contrast, the use of RA graft can be beneficial to their survival. The long-term patency rate of RA grafting is better than that of SVG grafting or even close to LIMA grafting, which will definitely play a key role in total arterial CABG. Although the utilization rate of RA grafting in CABG is not as high as expected, it still has bright prospects in the future.
RGEA grafting will not cause artery ischemia injury when it is used for grafting due to its ideal length and appropriate caliber, the same histological structure as LIMA and being independent of external nutrient vessels for nutrition. Moreover, atherosclerosis rarely occurs in RGEA grafting. Its anatomical position is close to diaphragm surface of the heart, which makes it particularly suitable for the revascularization of right coronary artery and multiple coronary arteries on the diaphragmatic surface of heart[15]. In this study, nine right gastroepiploic arteries were anastomosed with the right coronary artery (posterior descending branch and left ventricular posterior branch). The short-term follow-up CTA examination showed that one vessel was occluded, with an occlusion rate of 11.1%. Its patency rate was slightly lower than the recent patency rate of 92.4% reported by Ali et al[16] after an analysis and summary of the literature concerning RGEA grafting vessels published from 2000 to 2007, which may be associated with vasospasm caused during the early stage of operation. Kamohara et al[17] thought that RGEA graft could be safely used for CABG if its average diameter was more than 2 mm. Lee et al[18] believed that RGEA might not be suitable for CABG if its average diameter was less than 1.4 mm. Considering its characteristics of small diameter tube and being prone to spasm, the operation has been further improved, calcium antagonists have been used, and alpha receptor agonists have been less used in the later stage. To date, no graft occlusion has occurred. In addition, competitive flow is still a factor that shall not be ignored. In the occlusion cases in this study, investigators used RGEA to anastomose with the posterior descending branch with 70% to 90% stenosis. However, Ryu et al[19] thought that when a vessel is used as a target vessel for right gastroepiploic artery, its stenosis rate should be over 90% to obtain a better effect. Therefore, the selection of target vessel is very vital in RGEA surgery. No abdominal complications such as gastrointestinal complications occurred during the study period. Therefore, for young patients without gastric diseases who prepared to undergo upper abdominal surgery, especially for patients whose ascending aortas are unsuitable for anastomosis because of calcification, it is a good choice to have their right gastroepiploic arteries anastomosed with severely stenosed right coronary artery.
This study demonstrated that the individualized total arterial CABG does not increase surgical trauma, perioperative complications, and mortality. By contrast, it has sound surgical safety and short-term clinical efficacy. Although artery graft has a tendency to develop spasm, it has high patency rate, which can significantly reduce the adverse cardiovascular events to avoid reoperation and improve quality of life of patients. Therefore, for coronary heart disease patients who have reasonable life expectancy, individualized total arterial CABG is recommended to enhance the potential benefits of patients and society. In this study, the sample size of RA and RGEA grafting is small and the duration of follow-up is not long, which will have a certain impact on the statistical results. It is necessary to further expand the sample size and make a long-term follow-up of the total arterial grafts to observe its long-term clinical effect.
Total arterial revascularization is characterized by better long-term patency results and outcomes such as fewer incidence of myocardial infarctions and angina, lower incidence of reintervention, lower associated mortality rates and longer late survival and better quality of life than the traditional coronary artery bypass grafting (CABG).
Considering the participants were young at enrollment, and most of them were in a good physical state without severe history of diseases, total arterial revascularization was performed to maximize the efficacy of CABG procedures and reduce the adverse effects caused by using one or more great saphenous veins grafts.
The study reported here the efficacy and outcomes of total arterial coronary artery bypass grafting in 35 patients with non-single-vessel coronary artery diseases.
There are a variety of grafting techniques for arterial revascularization. The study selected three major strategies: left internal mammary artery (LIMA), radial artery (RA) and right gastroepiploic artery (RGEA) grafting. Thirty-five patients with non-single-vessel coronary artery diseases underwent CABG operation receiving the three kinds of grafts based on their physical conditions. Specifically, a total 90 vessels were grafted with an average of 2.6 vessels per person. Thirty-five patients received LIMA grafts, 35 patients received RA grafts and 9 patients received RGEA grafts. Perioperative complications and patency were observed, and quality of life was followed-up.
Patients undergoing total arterial revascularization resulted in improved clinical outcomes. All the patients were discharged from hospitals without occurrence of deaths. Over the follow-up, no occlusion was discovered for LIMA graft and occlusion of RA and RGEA grafts was low without severe postoperative complications.
In spite of technical difficulty associated with the harvest of LIMA, RA and RGEA, total arterial revascularization provided favorable results especially in the aspect of anastomoses and patency compared with commonly used veins as grafts, which are more likely than artery grafts to develop plaque and become blocked over time.
The usage of total arterial revascularization is restricted by several factors such patient age and general health, history of other diseases and conditions. For instance, it should be avoided in patients with insulin-dependent diabetics, or in patients with severe chronic obstructive pulmonary disease because they are at a high risk of developing sternal wound infections and the availability of conduits was constrained. More real-world studies should be conducted to determine the individuated revascularization strategies in this population.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Snyder J S-Editor: Wang JL L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Song YY, Xu XH, Lu XH, Wang XW. Clinical application of individuated total arterial coronary artery bypass grafting. Nanjing Yike Daxue Xuebao. 2019;39:899-902. |
| 2. | Khan AR, Golwala H, Tripathi A, Riaz H, Kumar A, Flaherty MP, Bhatt DL. Meta-analysis of Percutaneous Coronary Intervention Versus Coronary Artery Bypass Grafting in Left Main Coronary Artery Disease. Am J Cardiol. 2017;119:1949-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Mohite PN, Thingnam SK, Saxena AK. Radial artery compression in incomplete palmar arch for radial artery harvesting. Asian Cardiovasc Thorac Ann. 2014;22:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, Gott JP, Herrmann HC, Marlow RA, Nugent WC, O'Connor GT, Orszulak TA, Rieselbach RE, Winters WL, Yusuf S, Gibbons RJ, Alpert JS, Eagle KA, Garson A Jr, Gregoratos G, Russell RO, Smith SC Jr. ACC/AHA Guidelines for Coronary Artery Bypass Graft Surgery: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1991 Guidelines for Coronary Artery Bypass Graft Surgery). American College of Cardiology/American Heart Association. J Am Coll Cardiol. 1999;34:1262-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 291] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 5. | Pick AW, Orszulak TA, Anderson BJ, Schaff HV. Single vs bilateral internal mammary artery grafts: 10-year outcome analysis. Ann Thorac Surg. 1997;64:599-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 218] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 6. | Dimitrova KR, Hoffman DM, Geller CM, Dincheva G, Ko W, Tranbaugh RF. Arterial grafts protect the native coronary vessels from atherosclerotic disease progression. Ann Thorac Surg. 2012;94:475-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Benedetto U, Altman DG, Gerry S, Gray A, Lees B, Pawlaczyk R, Flather M, Taggart DP; Arterial Revascularization Trial investigators. Pedicled and skeletonized single and bilateral internal thoracic artery grafts and the incidence of sternal wound complications: Insights from the Arterial Revascularization Trial. J Thorac Cardiovasc Surg. 2016;152:270-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 133] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Cao C, Ang SC, Wolak K, Peeceeyen S, Bannon P, Yan TD. A meta-analysis of randomized controlled trials on mid-term angiographic outcomes for radial artery vs saphenous vein in coronary artery bypass graft surgery. Ann Cardiothorac Surg. 2013;2:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 9. | Desai ND, Cohen EA, Naylor CD, Fremes SE; Radial Artery Patency Study Investigators. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med. 2004;351:2302-2309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 368] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 10. | Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Late results of conventional vs all-arterial revascularization based on internal thoracic and radial artery grafting. Ann Thorac Surg. 2009;87:19-26.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Gaudino M, Leone A, Lupascu A, Toesca A, Mazza A, Ponziani FR, Flore R, Tondi P, Massetti M. Morphological and functional consequences of transradial coronary angiography on the radial artery: implications for its use as a bypass conduit. Eur J Cardiothorac Surg. 2015;48:370-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM Jr, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:2610-2642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 346] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 13. | Habib RH, Schwann TA, Engoren M. Late effects of radial artery vs saphenous vein grafting in patients aged 70 years or older. Ann Thorac Surg. 2012;94:1478-1484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Hoffman DM, Dimitrova KR, Decastro H, Friedmann P, Geller CM, Ko W, Tranbaugh RF. Improving long term outcome for diabetic patients undergoing surgical revascularization by use of the radial artery conduit: a propensity matched study. J Cardiothorac Surg. 2013;8:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Huang FJ, Yang JF, Lai YQ, Xu CL, Wu Q. Right gastroepiploic artery as a coronary bypass graft in coronary artery bypass graft surgery: an experience of 32 cases. Zhonhua Waike Zazhi. 2005;43:98-99. |
| 16. | Ali E, Saso S, Ashrafian H, Athanasiou T. Does a skeletonized or pedicled right gastro-epiploic artery improve patency when used as a conduit in coronary artery bypass graft surgery? Interact Cardiovasc Thorac Surg. 2010;10:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Kamohara K, Minato N, Minematsu N, Yunoki J, Hakuba T, Satoh H, Morokuma H, Takao Y. Preoperative evaluation of the right gastroepiploic artery on multidetector computed tomography in coronary artery bypass graft surgery. Ann Thorac Surg. 2008;86:1444-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Lee DH, Lee W, Kim KB, Cho KR, Park EA, Chung JW, Park JH. Availability of the right gastroepiploic artery for coronary artery bypass grafting: preoperative multidetector CT evaluation. Int J Cardiovasc Imaging. 2010;26:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Ryu SW, Ahn BH, Choo SJ, Na KJ, Ahn YK, Jeong MH, Kim SH. Skeletonized gastroepiploic artery as a composite graft for total arterial revascularization. Ann Thorac Surg. 2005;80:118-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |