Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4810
Peer-review started: January 25, 2021
First decision: March 25, 2021
Revised: April 2, 2021
Accepted: April 23, 2021
Article in press: April 23, 2021
Published online: June 26, 2021
Processing time: 137 Days and 5.1 Hours
Hematuria is one of the most common clinical symptoms for urologists and is typically observed in urinary system tumors, prostate hyperplasia, and urinary stone disease. Hematuria due to vesical varices is very rare, and only a few cases have been reported since 1989. We report the first case of vesical varices due to portal hypertension with aberrant development and functioning of the geni
This patient was a 53-year-old man with a history of aberrant development of the genitourinary system and hepatitis B-associated cirrhosis. He was admitted to the emergency department with severe hematuria and bladder clot tamponade. Many abnormally dilated blood vessels were found surrounding the bladder in the pelvis by color Doppler ultrasound, contrast-enhanced computed tomography, and three-dimensional visualization technology. It was difficult to perform transurethral cystoscopy and hemostasis in this patient, so we performed open surgical bladder exploration for hemostasis and surgical devascularization around the bladder.
Urologists should improve the understanding of the pathophysiology, clinical manifestations, diagnosis, and treatment of vesical varices. This case may be presented as a reference for the diagnosis and management of severe hematuria due to vesical varices.
Core Tip: Hematuria due to vesical varices is very rare. Here, we report a case of vesical varices due to portal hypertension with aberrant development and functioning of the genitourinary system, review the literature, and discuss its pathophysiology, clinical manifestations, diagnosis, and treatment.
- Citation: Wei ZJ, Zhu X, Yu HT, Liang ZJ, Gou X, Chen Y. Severe hematuria due to vesical varices in a patient with portal hypertension: A case report. World J Clin Cases 2021; 9(18): 4810-4816
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4810.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4810
Esophageal and gastric fundic varices are common complications of portal hyper
A 53-year-old man was referred to the Emergency Department of our hospital with severe hematuria and a massive bladder clot.
The patient had a history of bilateral cryptorchidism since childhood and was untreated and had hepatitis B-associated cirrhosis for 16 years. He underwent splenectomy with devascularization surgery of the lower esophagus and proximal stomach 10 years ago due to hematemesis and melena.
The physical examination revealed uplift of the suprapubic region and dullness percussion. His pubic hair was sparsely distributed, the penis and scrotum were underdeveloped, and the testis was impalpable in the scrotum (Figure 1).
Blood analysis revealed an abnormal hemogram, including 3.09 × 109/L red blood cells (normal range: 3.5-5.5 × 109/L) with 9.0 g/dL hemoglobin (normal range: 12.0-15.5 g/dL) and normal leukocytic and platelet counts. Prothrombin and partial throm
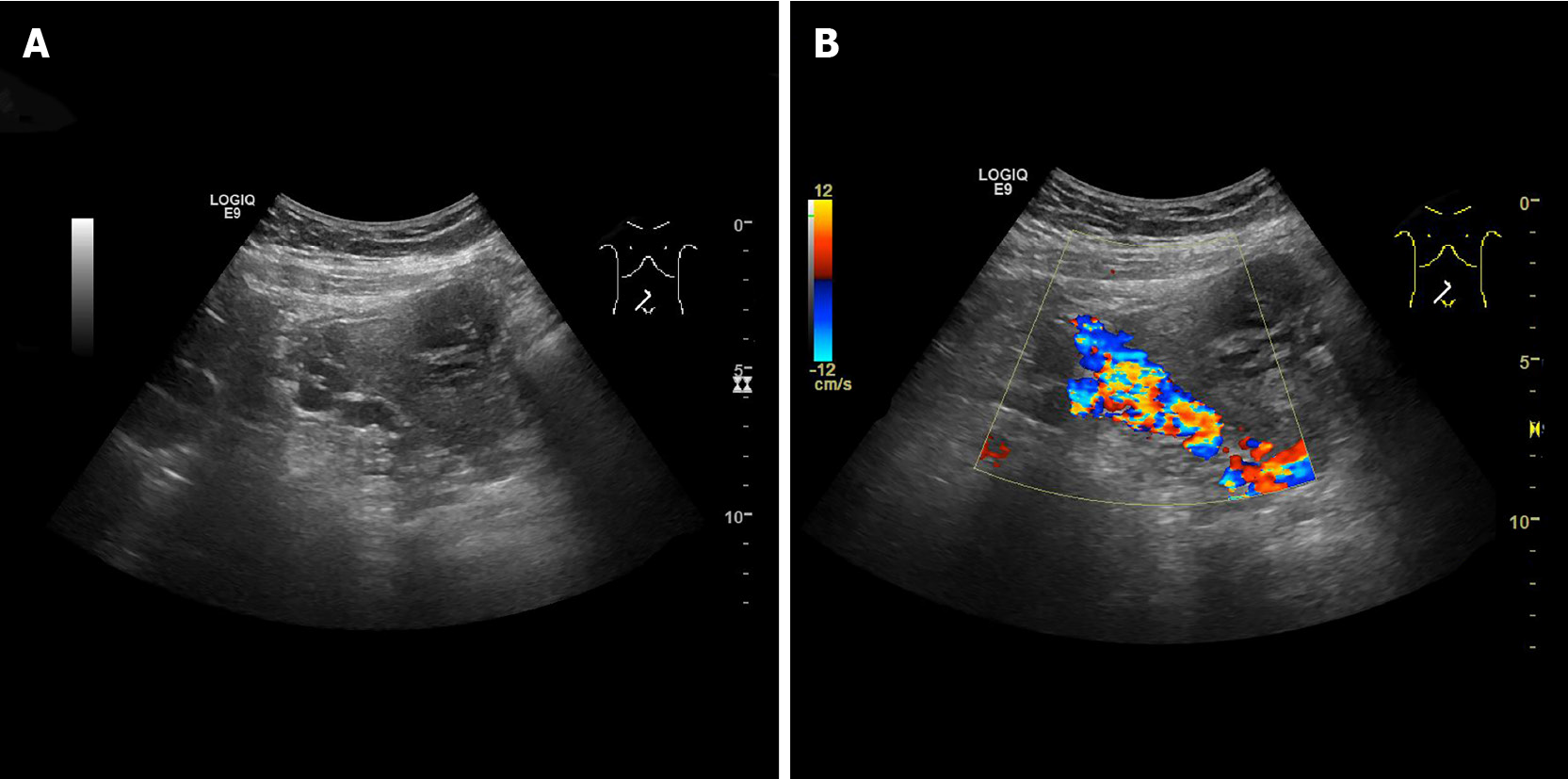
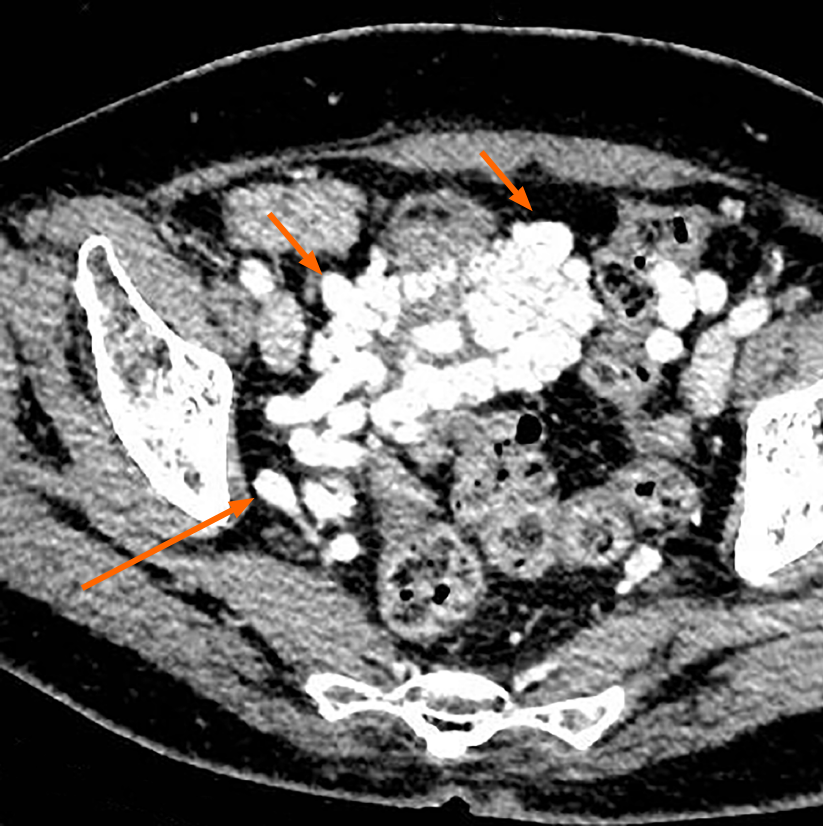
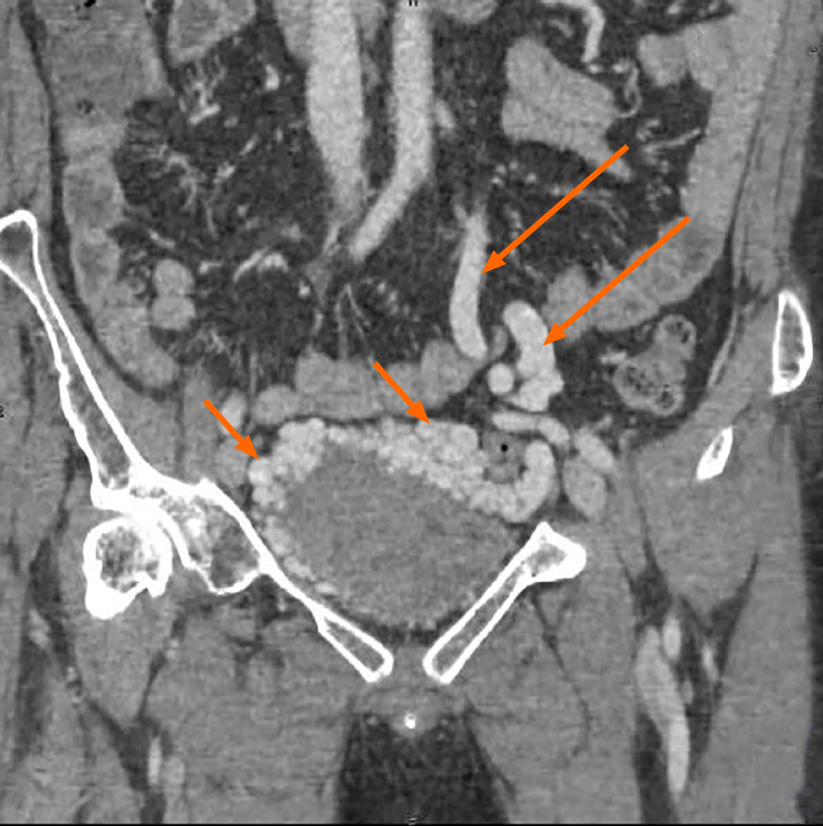
Color Doppler ultrasound demonstrated the enlargement of the portal vein with a main trunk diameter of approximately 14.8 mm and many twisted tube-like echoes around the bladder, which were connected to the bilateral iliac veins. Color Doppler flow imaging showed a color flow signal inside the tube-like echoes (Figure 2). Computed tomography (CT) revealed multiple tortuous and thickened veins on the anterior and both sidewalls of the bladder and enlargement of the inferior mesenteric veins (Figures 3 and 4). Three-dimensional (3D) visualization technology clearly revealed many abnormally dilated blood vessels surrounding the bladder in the pelvis. In this patient, the dilated vesical varices on the right side drained into the internal iliac vein, and those on the left side were connected with the inferior mesenteric vein and finally entered the splenic vein (Figure 5).
The final diagnosis of the presented case was vesical varices.
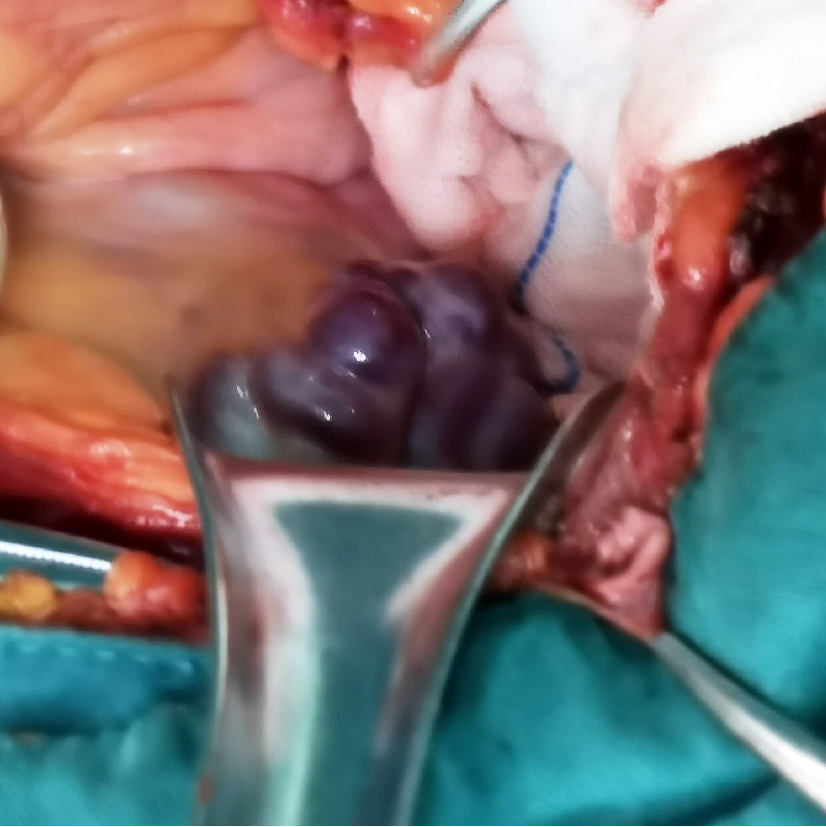
After entering the hospital, the patient underwent indwelling catheterization and continuous bladder irrigation to prevent bladder clot tamping. In the process of continuous bladder irrigation, a large number of blood clots were flushed out. He was given symptomatic treatment, including hemostasis drugs (hemocoagulase atrox and carbazochrome sodium sulfonate) and fluid replacement, but the patient’s hemoglobin continued to decrease. Considering the patient’s continuous bladder bleeding, an open bladder exploration operation was performed imminently. During the operation, a large number of tortuous and swollen veins were observed in the posterior and top walls of the urinary bladder, twisting each other into a mass (Figure 6). The vesical varices on the left side continued with the inferior mesenteric vein. On the right side, the vesical varices drained into the right iliac vessels. After clamping the left side of vesical varices with hemostat, the tension of the venous wall was reduced. After incising the less vascularized area of the anterior wall of the bladder with an ultrasonic knife and clearing the blood clot, venous swelling in the urinary bladder trigone was observed, and a globular raised tortuous vein was observed at the inner side of the right ureteral opening with a 4 mm rupture at the top. The bleeding vein was sewn to stop the bleeding. We separated the vesical varices on both sides of the bladder and ligated and disrupted the large veins.
The operation went smoothly. The patient was followed 3 mo later, and hematuria did not occur again.
Esophageal and gastric fundic varices are common complications of portal hyper
The causes of bladder varicose veins can be divided into secondary and primary causes. Secondary vesical varices are related to portal hypertension[4-7], schistoso
The present patient had a history of portal hypertension due to hepatitis B-associated cirrhosis. With the help of CT examination and 3D visualization technology, it was clearly noted that the vesical varices communicated with the splenic vein and portal vein through the inferior mesenteric vein from the left side and the systemic circulation through the internal iliac vein on the right side. In this patient, long-term liver cirrhosis led to obstruction of portal venous return, which led to increased portal venous pressure and enlargement of the portal vein and upper and lower mesenteric veins. Since the patient had a history of splenectomy with devascularization surgery, the usual collateral veins that communicate the portal vein and the superior vena cava have been disrupted, and the vesical venous plexus became the communicating branch between the portal vein and the inferior vena cava. The increased portal venous pressure can only be conducted through the splenic vein and the inferior mesenteric vein to the bladder vein and then communicate with the inferior vena cava, resulting in tortuosity and dilation of the vesical venous plexus.
The current diagnostic methods for vesical varices are color Doppler and CT; however, 3D visualization technology shows an advantage in displaying the overall situation of dilated veins. As a noninvasive examination, color Doppler has been adopted in the early diagnosis of vesical varices[17], but it cannot reflect the overall blood flow pattern of dilated veins. Conventional CT examination requires the doctor to make subjective assumptions about the 3D models of anatomical parts based on two-dimensional images, which have certain limitations. 3D visualization technology is a 3D digital model reconstructed based on imaging data that has been widely used in urologic disease. It can accurately display the anatomical characteristics of dilated veins and provide more accurate data and positioning for the formulation of surgical plans. To date, cystoscopy has been considered the gold standard for the diagnosis of vesical varices, and we can clearly see tortuous blood vessel masses in the bladder wall through cystoscopy. However, the patient reported here has not been treated for bilateral cryptorchidism since childhood, resulting in aberrant development and functioning of the genitourinary system. Thus, it is difficult to perform cystoscopy. Percutaneous transhepatic portography is also an important method for diagnosing vesical varices, but it is usually not recommended as the first-choice examination due to its invasive nature.
Currently, no uniform opinions on the treatment of vesical varices are available. Lim et al[14] used balloon-occluded percutaneous transhepatic obliteration to treat dilated veins of the bladder and achieved good results given that cystoscopy and CT showed the disappearance of vesical varices after 6 wk. In addition, Sivalingam et al[18] and Parmar et al[19] introduced a treatment modality in treatment of bleeding vesical varices using endoscopic injection of N-butyl cyanoacrylate and achieved satisfactory results. However, Herden et al[6] believed that in symptomatic vesical varices, surgical devascularization around the bladder, laser sclerosis, and coagulation are usually only temporarily effective. Successful long-term treatment involves surgical decompression of portal hypertension by complete or selective portocaval shunts, transjugular intrahepatic portosystemic shunts, or liver transplantation. The bleeding site of symptomatic vesical varices is usually located in the bladder trigone, and it is often clinically manifested as a large amount of gross hematuria, which cannot stop on its own and easily leads to hemorrhagic shock. Drugs and surgery are the main treatment methods. It was difficult to perform transurethral cystoscopy and hemostasis in this patient. Finally, we performed open surgical bladder exploration for hemostasis and surgical devascularization around the bladder.
Hematuria is a common disease in urology, but hematuria caused by varicose veins of the bladder is relatively rare. Urologists should improve the understanding of the pathophysiology, clinical manifestations, diagnosis, and treatment of vesical varices. For patients with massive hematuria, the possibility of this disease should be considered, especially in patients with portal hypertension who have undergone interventions altering portal pressure dynamics and flow patterns. CT and 3D visualization technology can clarify the blood flow direction of dilated veins and provide a reference for the treatment of patients.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arguelles E, Garbuzenko DV, Xiol X S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Yuan YY
| 1. | Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362:823-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 639] [Cited by in RCA: 638] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 2. | Helmy A, Al Kahtani K, Al Fadda M. Updates in the pathogenesis, diagnosis and management of ectopic varices. Hepatol Int. 2008;2:322-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 133] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Sato T, Akaike J, Toyota J, Karino Y, Ohmura T. Clinicopathological features and treatment of ectopic varices with portal hypertension. Int J Hepatol. 2011;2011:960720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (35)] |
| 4. | Sano K, Shuin T, Takebayashi S, Sugawara T, Moriyama M, Kinoshita Y, Kubota Y, Hosaka M. A case of vesical varices as a complication of portal hypertension and manifested gross hematuria. J Urol. 1989;141:369-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Gaspar Y, Detry O, de Leval J. Vesical varices in a patient with portal hypertension. N Engl J Med. 2001;345:1503-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Herden U, Seiler CA, Candinas D, Schmid SW. Bladder tamponade due to vesical varices during orthotopic liver transplantation. Transpl Int. 2008;21:1105-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Kim M, Al-Khalili R, Miller J. Vesical varices: an unusual presentation of portal hypertension. Clin Imaging. 2015;39:920-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Bruet A, Fingerhut A, Lopez Y, Bergue A, Taugourdeau P, Mathe C, Hillion D, Fendler JP. Ileal varices revealed by recurrent hematuria in a patient with portal hypertension and Mekong Schistosomiasis. Am J Gastroenterol. 1983;78:346-350. [PubMed] |
| 9. | Hallamore SL, Grills RJ, Neerhut G, Lawrentschuk N. Submucosal vesical varicosities causing hematuria and retention of urine in pregnancy: cystovarix. Am J Obstet Gynecol. 2007;196:e29-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Suzuki K, Tsugawa K, Oki E, Morio T, Ito E, Tanaka H. Vesical varices and telangiectasias in a patient with ataxia telangiectasia. Pediatr Nephrol. 2008;23:1005-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Rinnab L, Paiss T, Küfer R. [Klippel-Trénaunay syndrome. A rare cause of recurrent macrohematuria: case report]. Urologe A. 2006;45:739-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Koshy CG, Govil S, Shyamkumar NK, Devasia A. Bladder varices--rare cause of painless hematuria in idiopathic retroperitoneal fibrosis. Urology. 2009;73:58-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Lipsich J, Rojas L, Alonso J, Teplisky D, Halac A, Alvarez F, Sierre S. Massive hematuria due to portal hypertension in a child with bladder augmentation for vesical exstrophy. J Pediatr Urol. 2008;4:236-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Lim DH, Kim DH, Kim MS, Kim CS. Balloon-occluded percutaneous transhepatic obliteration of isolated vesical varices causing gross hematuria. Korean J Radiol. 2013;14:94-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Bawany FA, Ghirano RA, Bayabani SR. Primary vesical varices: a cause of gross haematuria. J Pak Med Assoc. 2009;59:332-334. [PubMed] |
| 16. | Hou Y, Xue Y, Yang Y, Sun RG. Vesical varices causing gross hematuria in a four-year-old girl. Urology. 2012;79:902-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Sato T. Transabdominal color Doppler ultrasonography for the diagnosis of small intestinal and vesical varices in a patient successfully treated with percutaneous transhepatic obliteration. Clin J Gastroenterol. 2010;3:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Sivalingam S, Manikam R, Razack MPdH, Mohamad N. Endoscopic Injection of Histoacryl® in the Treatment of Recurrent Hematuria Secondary to Bladder Varices. Int J Case Rep Imag. 2011;2. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Parmar K, Rathi S, Khanna A, Gupta M, Singh A, Singh SK, Singh V. Portal Hypertensive Vesiculopathy: A Rare Cause of Hematuria and a Unique Management Strategy. Urology. 2018;115:e7-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |