Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4778
Peer-review started: January 5, 2021
First decision: March 27, 2021
Revised: April 1, 2021
Accepted: April 23, 2021
Article in press: April 23, 2021
Published online: June 26, 2021
Processing time: 156 Days and 15.1 Hours
Intralenticular foreign body is rarely encountered in ophthalmic practice. In most cases, subsequent traumatic cataract requires cataract surgery for visual rehabilitation.
A 35-year-old man was injured by iron filings in his left eye. After the injury, the patient tried to draw the object out by himself using a magnet; however, the foreign body (FB) was pushed to the equator of the lens. The FB was removed by a magnet through the anterior chamber accessed through the original capsular wound. Since most of the lens was transparent and only partially opaque after the operation, the lens was kept under close observation. After the surgery, the patient’s visual acuity reached 20/20 from 2/20, visual function recovered very well, and local opacity of the lens remained stable.
For intralenticular FB in the anterior cortex under the capsule, magnet may be a more advantageous way to remove the object.
Core Tip: Intralenticular foreign body is rarely encountered in ophthalmic practice. In most of these studies, the lens was either preserved without intraocular foreign body removal or removed together with intraocular foreign bodies. The present case report is about successful retrieval of a foreign body from the lens while the lens is preserved, with resultant stable visual function.
- Citation: Xue C, Chen Y, Gao YL, Zhang N, Wang Y. Disappeared intralenticular foreign body: A case report. World J Clin Cases 2021; 9(18): 4778-4782
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4778.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4778
Intralenticular foreign body is rarely encountered in ophthalmic practice. It only accounts for approximately 5% to 10% of all intraocular foreign bodies (IOFBs)[1]. In some cases, subsequent traumatic cataract requires cataract surgery for visual rehabilitation[2,3]. Conservative management of intralenticular foreign bodies has also been successful in other patients who have minimal lens opacities and stable visual function[3,4]. In most of these studies, the lens was either preserved without intraocular foreign body removal or removed together with intraocular foreign bodies[5].
However, in clinical practice, the condition is various, and sometimes it is rare and complicated. For rare cases, we should think carefully and try our best to get a good prognosis with optimized treatment. The present case report is about successful retrieval of a foreign body from the lens of the eye of a 35-year-old man, with resultant stable visual function. It was a rare and special case due to the patient’s own incorrect treatment. In this case, the lens was preserved while the foreign body was removed.
A 35-year-old man who was injured by iron filings in his left eye visited our emergency room 1 d after the injury. He was admitted to the hospital.
The man was injured by iron filings in his left eye 1 d before visiting our emergency room.
The history of past illness was unremarkable.
There was nothing special about personal and family history.
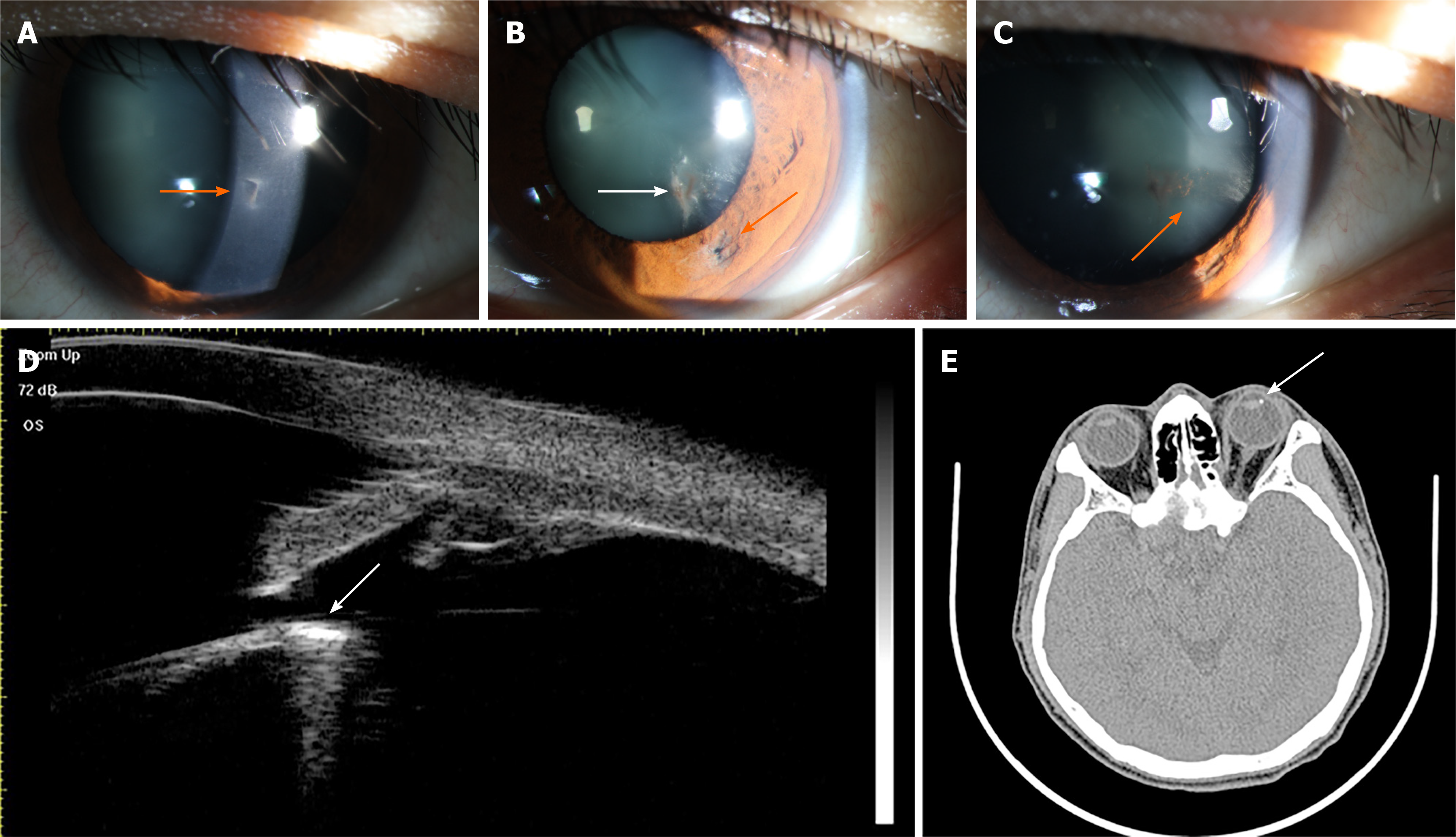
On local examination, the visual acuity was 20/20 in the right eye and 2/20 in the left eye. The intraocular pressure was 14 mmHg in the right eye and 13 mmHg in the left eye. Slit-lamp examination of the left eye showed a well-closed full-thickness corneal perforation wound (Figure 1A), an iris hole (Figure 1B, orange arrow), and only a localized lens opacity (Figure 1B, white arrow) at the corresponding positions. There were no cells, flare, or keratic precipitates. Despite dilating the pupil fully, we could not see the foreign body under direct vision. A band of a cloudy area was seen instead extending toward the equator of the lens (Figure 1C, orange arrow). We asked the patient about further events before he reported to us when we came to know about his attempts to remove the object by himself using a magnet. The patient had once successfully removed a foreign body from his arm; on another occasion, therefore, he tried attempting the same for his eye.
The band of the cloudy area towards the equator of the lens made us feel that the foreign body might be lying somewhere behind the iris. Computed tomography (CT) confirmed the presence of the foreign body around the equator of the lens (Figure 1D). An ultrasound biomicroscopic (UBM) examination was performed to check the relative positions of the foreign body and the lens, considering that the cornea wound was well closed (Figure 1E).
Nothing abnormal was showed in the laboratory examinations.
CT and UBM was performed to confirm the presence and positions of the foreign body.
From the medical history, clinical signs, examinations, and findings in the operation, it was clearly that the final diagnosis was intralenticular foreign body. It was a rare and special case for the patient’s attempts to remove the object by himself using a magnet.
During the procedure, a self-sealing 3.2 mm clear corneal major incision was made at the 11 o’clock position. Then, viscoelastic material was used to fill the anterior chamber. The iris was pushed away, revealing the position of the foreign body at the superficial layer of the lens equator. A magnet was inserted to the anterior chamber through the major corneal incision, and the foreign body was removed through the original capsular wound. Fortunately, the operation was smooth and did not cause any additional laceration of the anterior capsule of the lens after the removal of the object. As most of the lens was transparent and only partially opaque, we decided not to perform any further surgical intervention to the lens, but to observe the progression of traumatic cataract during follow-up.
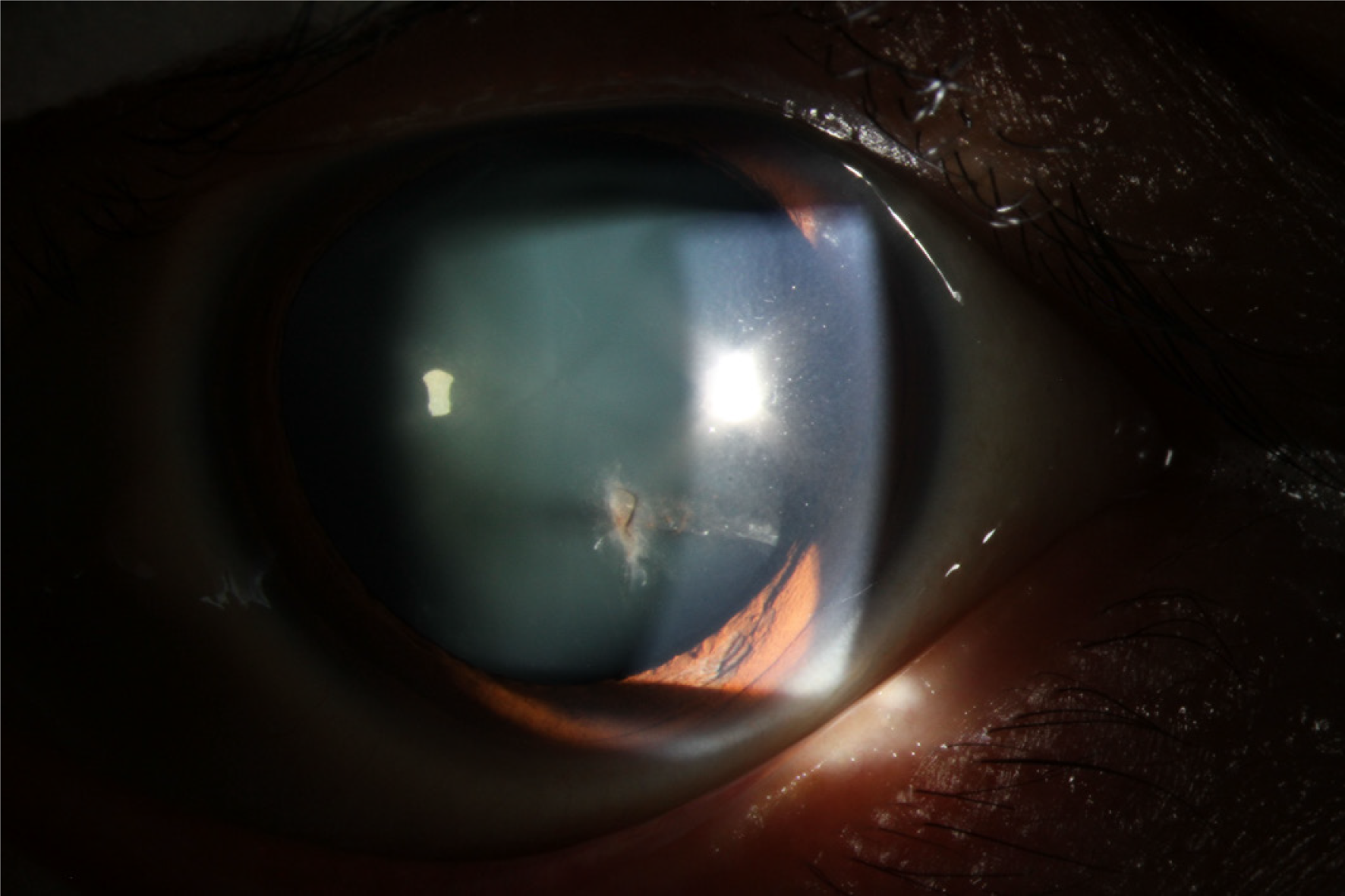
Postoperative recovery was extremely good. On the 2nd day of the surgery, the visual acuity of the left eye was 20/20, and there was no sign of any cells or flare in the anterior chamber. The lens in the pupil area was transparent, with only local opacity. One week after the surgery, the best-corrected visual acuity was 20/20 in the left eye, the lens in the pupil area was still transparent, and the local opacity did not expand (Figure 2). One month after the surgery, the best-corrected visual acuity was maintained at 20/20, the lens in the pupil retained transparency, and the local opacity region did not expand more. Three months after the surgery, during a follow-up call, the patient reported excellent visual acuity and did not feel any eye discomfort, indicating no further progression in the opacity.
The management of intralenticular foreign body involves an initial assessment of its size, site, material, any potential for infection, and degree of lenticular and other intraocular damage[6]. In this case, the foreign body was of the medium size, and it may cause a higher risk of complication(s) if not be removed. The foreign body embedded in the anterior cortex under the capsule, so a magnet was applied to remove it from the original capsular wound. In younger patients because of the accommodation, age plays a vital factor in the extraction of the lens during removal of the intraocular foreign body[7,8]. In this case, the patient was 35 years old, so we tried out best to retain his lens. Fortunately, the operation did not cause any additional laceration of the anterior capsule of the lens and most of the lens was transparent and only partially opaque; thus, we decided not to extract the lens. The reason for conservative observation was to avoid further damage to the eye, and more importantly, to maintain accommodation of the eye.
Despite a capsular breach, most of the lens was clear and only partial opaque in this case. If the capsular breach is small, the anterior capsule retains its healing capacity. The presence of the subcapsular epithelium makes it heal quickly by rapid epithelial proliferation, restoring its continuity and limiting the free passage of ions and fluid that may progress to the development of cataract formation[9,10].
From examinations and medical history, we could infer that the IOFB passed through the cornea, iris, and anterior capsule of the lens successively, and finally stayed at the superficial layer of the cortex in the middle part of the lens at the time of the primary injury. However, after the patient’s attempts to remove the object by himself using a magnet, the IOFB was drawn to the equator of the lens.
The problem encountered in the process of treatment was that the foreign body might enlarge capsular breach, in which situation the development of traumatic cataract might accelerate and the cataract surgery might be necessary in this process. The foreign body was relatively tiny and was at the superficial layer of the lens. We inferred that the force between the magnet and the foreign body might not be strong. Probably, drawing the foreign body from the lens with magnet would not cause additional damage. We were very careful in the process and fortunately the operation was smooth and did not cause any additional laceration of the anterior capsule. The lens could be preserved while the foreign body was removed at the same time.
The critical aspect of this case was the patient’s own attempt to retrieve the foreign object using a magnet before he reported to us. This made the case difficult during operation as the object was pushed to the equator of the lens and it may cause additional damage and increase opacity of the lens. Fortunately, with surgery, the patient’s visual function recovered well, and local opacity of the lens remained stable without further progress. In summary, patients should not attempt any self-treatment particularly when it involves delicate structures such as the eyes as it might lead to further damage. The clinicians should take all possible considerations to preserve the physiological function when dealing with embedded intraocular foreign bodies. The limitation of this case report was a relatively short follow-up time, however, we can infer a good long-time outcome from the 3-mo follow-up result.
In conclusion, for intralenticular foreign body in the anterior cortex under the capsule, magnet may be a more advantageous way to remove the object. It is recommended to keep the lens if only partially opaque and maintain a close follow-up after retrieval of the foreign body, especially in younger patients, to maintain the accommodation of the eye.
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Xu X S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Li JH
| 1. | Coleman DJ, Lucas BC, Rondeau MJ, Chang S. Management of intraocular foreign bodies. Ophthalmology. 1987;94:1647-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 76] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Kumar A, Kumar V, Dapling RB. Traumatic cataract and intralenticular foreign body. Clin Exp Ophthalmol. 2005;33:660-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Dhawahir-Scala FE, Kamal A. Intralenticular foreign body: a D-Day reminder. Clin Exp Ophthalmol. 2005;33:659-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Lebowitz HA, Couch JM, Thompson JT, Shields JA. Occult foreign body simulating a choroidal melanoma with extrascleral extension. Retina. 1988;8:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Lin YC, Kuo CL, Chen YM. Intralenticular foreign body: A case report and literature review. Taiwan J Ophthalmol. 2019;9:53-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Reddy SC. Intralenticular metallic foreign body: a case report. Int J Ophthalmol. 2011;4:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 7. | Cazabon S, Dabbs TR. Intralenticular metallic foreign body. J Cataract Refract Surg. 2002;28:2233-2234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Surv Ophthalmol. 2016;61:582-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 9. | Fagerholm PP, Philipson BT. Human traumatic cataract. A quantitative microradiographic and electron microscopic study. Acta Ophthalmol (Copenh). 1979;57:20-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Keeney AH. Intralenticular foreign bodies. Arch Ophthalmol. 1971;86:499-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 0.6] [Reference Citation Analysis (0)] |