Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4754
Peer-review started: December 17, 2020
First decision: March 11, 2021
Revised: April 7, 2021
Accepted: May 7, 2021
Article in press: May 7, 2021
Published online: June 26, 2021
Processing time: 175 Days and 13.7 Hours
Pheochromocytomas are rare endocrine tumors with various clinical manifestations, and few of them might present with profound, life-threatening conditions.
We report the case of a 65-year-old man who complained of sudden dyspnea and hemoptysis for half a day. There was no obvious cause for the patient to have dyspnea, coughing, or coughing up to approximately 100 mL of fresh blood. Finally, he was diagnosed with pheochromocytoma crisis (PCC), coexisting with an abdominal aortic aneurysm (AAA).
We report a case of pheochromocytoma presenting with recurrent hemoptysis, dyspnea and hypotension coexisting with an AAA. It not only proved the uncommon manifestations of pheochromocytoma but also directed clinicians to consider PCC among the possible diagnoses when meeting similar cases. Moreover, surgical excision is the most beneficial method for the treatment of pheochromocytoma coexisting with AAA when the situation is stable.
Core Tip: We report a case of pheochromocytoma presenting with recurrent hemoptysis, dyspnea, and hypotension coexisting with an abdominal aortic aneurysm. It not only proved the uncommon manifestations of pheochromocytoma but also directed clinicians to consider pheochromocytoma crisis among the possible diagnoses when meeting similar cases.
- Citation: Zhao HY, Zhao YZ, Jia YM, Mei X, Guo SB. Pheochromocytoma with abdominal aortic aneurysm presenting as recurrent dyspnea, hemoptysis, and hypotension: A case report. World J Clin Cases 2021; 9(18): 4754-4759
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4754.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4754
Pheochromocytomas are rare endocrine tumors with various clinical manifestations, and a small number of them might present with profound, life-threatening conditions. We report a case of pheochromocytoma presenting with recurrent hemoptysis, dyspnea, and hypotension, coexisting with an abdominal aortic aneurysm, and with a positive outcome. We discuss the management and treatment of the patient in this case report and the proposed mechanisms.
A 65-year-old man was taken to our emergency department, complaining of sudden dyspnea and hemoptysis for half a day. There was no obvious cause for the patient to have dyspnea, coughing, or coughing up to approximately 100 mL of fresh blood.
The patient had four episodes of similar symptoms in the past 10 years. The first three episodes had dyspnea accompanied by hypertension, without hemoptysis, and only the symptoms were treated; the cause had not been identified. Dyspnea, hemoptysis, and hypotension occurred 5 years ago. He was hospitalized at our hospital, and a left adrenal mass and an abdominal aortic aneurysm (AAA) were found. An abdominal computed tomography (CT) scan showed a left adrenal mass measuring 3.2 cm × 3.6 cm and an AAA with a maximum diameter of 5.3 cm. Surgical treatment was not performed because the patient worried about the risks of surgery.
The patient was healthy.
The patient had a disease-free personal and family history.
On physical examination, the patient was dyspneic, in distress, and sweating profusely. His blood pressure was 87/50 mmHg, heart rate was 107 beats/min, respiratory rate was 35 breaths/min, body temperature was 36 °C, and oxyhemoglobin saturation was 88% while breathing a 50% oxygen concentration with a face mask.
Initial laboratory tests demonstrated leukocytosis (25.73 × 109/L, with 93.6% neutrophils) and significantly increased serum procalcitonin at 58.4 ng/mL (normal value: < 0.05 ng/mL). Blood gas analysis revealed lactate 11.0 mmol/L, pH 7.31, PaO2 72.1 mmHg, PaCO2 32.3 mmHg, and HCO3– 18.9 mmol/L while breathing 100% oxygen concentration with noninvasive positive pressure ventilation (NIPPV). His liver and renal function was also abnormal (alanine transaminase 145 U/L, glutamic-oxaloacetic transaminase 156 U/L, and creatinine 126 µmol/L), and D-dimer was 28.85 mg/L (normal value: ≤ 0.55 mg/L). Electrocardiogram showed sinus tachycardia and ST segment depression in the V2-V6 leads.
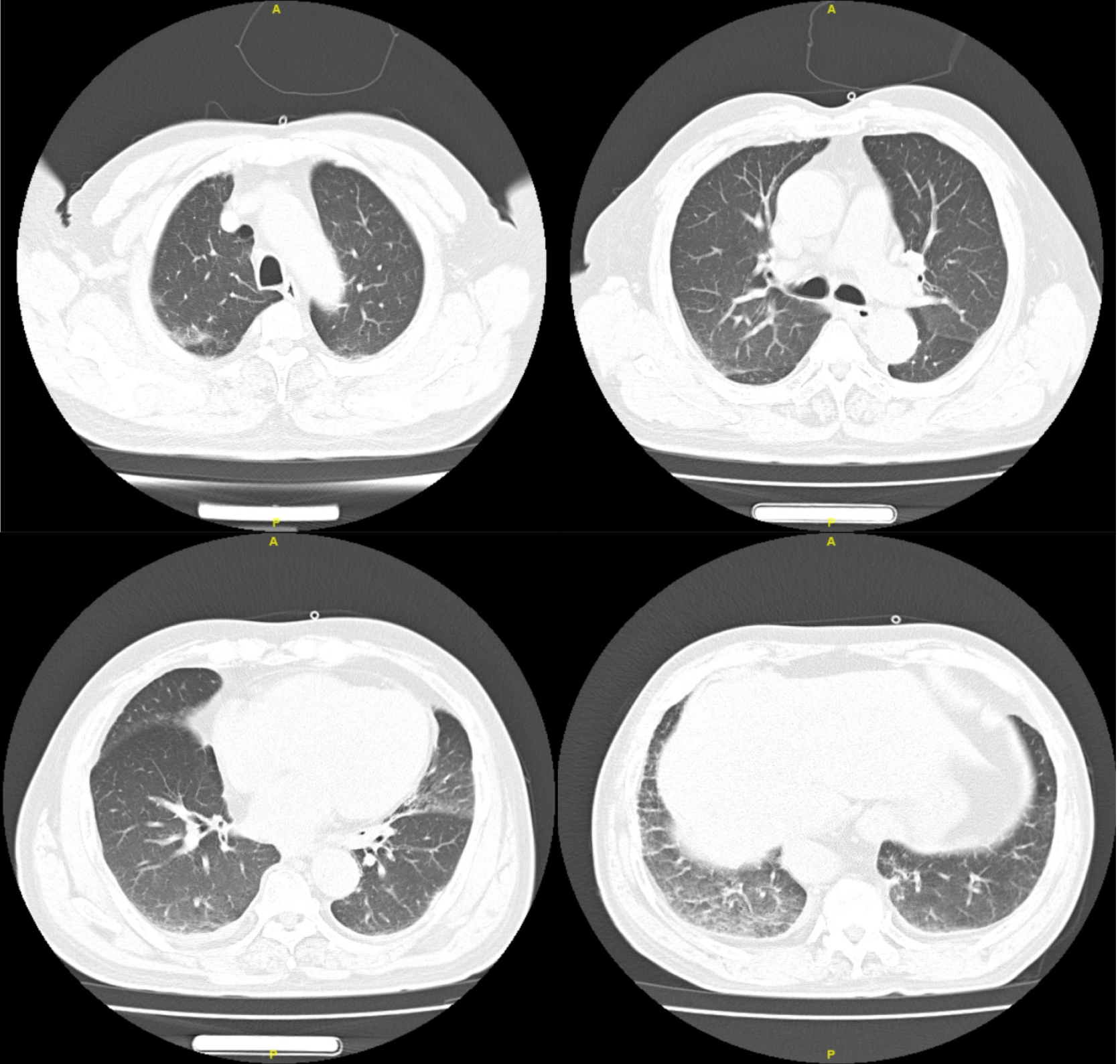
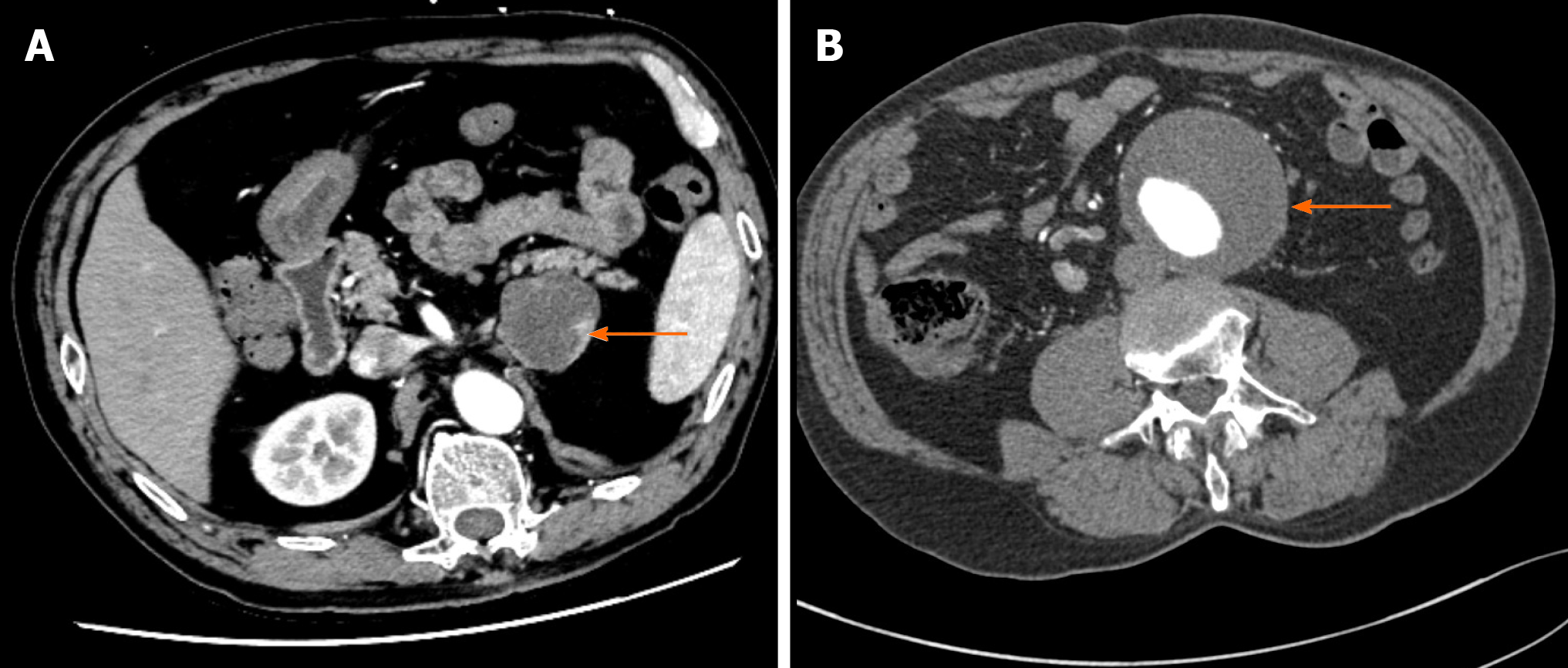
The patient’s chest X-ray manifestations were characterized by multiple plaques in both lungs, chest CT scans showed little ground glass shadow under the pleura of both lungs (Figure 1), and abdominal CT scans showed a left adrenal mass measuring 4.4 cm × 4.3 cm and an AAA with a maximum diameter of 7.3 cm (Figure 2). Echocardiography showed enlargement of the left atrium, aortic sinus, and ascending aorta. Systolic left ventricular function was impaired (ejection fraction 55%), but there was no pulmonary hypertension and no sign of diastolic dysfunction (left ventricular end diastolic diameter 55 mm).
The final diagnosis of the present case was pheochromocytoma crisis (PCC) and abdominal aortic aneurysm.
Although PCC was considered, septic shock cannot be excluded. After treatment with antibiotic (imipenem), fluid resuscitation, and NIPPV for relieving dyspnea, the patient’s condition improved on the second day, except for blood pressure. Dopamine (5-10 μg/kg/min) was used to support blood pressure. On the third day, the patient completely stopped hemoptysis and the leukocyte count recovered to normal. Considering that there was no evidence of infection and no fever, which did not fit with the diagnosis of sepsis, step-down treatment was adopted for anti-infection. Tests of plasma and urine catecholamines and metabolites were performed. The levels of dopamine and methoxyepinephrines were increased in both the urine and 24-h urine. To our surprise, the level of plasma adrenocorticotropic hormone (ACTH) was decreased (Table 1). In addition, the blood cortisol level was slightly reduced. Magnetic resonance imaging of the pituitary gland was normal. The levels of angiotensin II, aldosterone, and renin were normal. One week later, the patient had no obvious discomfort, and blood pressure returned to normal. He was discharged. The repeated tests were performed 7 d after discharge (Table 1). Persuaded by us and his family, the patient finally made up his mind to undergo operation. The abdominal aortic aneurysm was repaired first by endovascular exclusion of abdominal aortic aneurysm, and 1 mo later, he underwent laparoscopic left adrenal tumor resection. Pathological examination confirmed the diagnosis of left adrenal pheochromocytoma.
| Laboratory test | On admission | Seven days out of hospital | Normal range |
| Serum catecholamine | |||
| AD (pg/mL) | 31.77 | 47.95 | 0.00-100.00 |
| NA (pg/mL) | 141.48 | 600.53 | 0.00-600.00 |
| DOP (pg/mL) | 243.55 | 52.09 | 0.00-100.00 |
| Serum methoxyepinephrines | |||
| 3-MT (nmol/L) | 55.89 | < 0.08 | < 0.18 |
| NMN (nmol/L) | 0.66 | 0.71 | ≤ 0.50 |
| MN (nmol/L) | 1.95 | 3.64 | ≤ 0.90 |
| 24-h urinary catecholamine | |||
| 24 h AD(μg/d) | 11.65 | 8.38 | 0.00-20.00 |
| 24 h NA (μg/d) | 24.55 | 48.34 | 0.00-90.00 |
| 24h DOP (μg/d) | 1448.71 | 53.57 | 0.00-600.00 |
| 24-h urinary methoxyepinephrines | |||
| 24 h 3-MT (nmol/d) | 14443 | 266 | < 216 |
| 24 h NMN (nmol/d) | 579 | 682 | < 216 |
| 24 h MN (nmol/d) | 276 | 169 | < 382 |
| ACTH (pg/mL) | 5.0 | 26.0 | 7.2-63.3 |
The patient was followed for 5 mo and showed no signs of recurrence.
Pheochromocytomas are catecholamine-secreting tumors arising from chromaffin cells of the adrenal medulla and the sympathetic ganglia. The typical clinical presentation consists of episodic headache, diaphoresis, and tachycardia accompanied by paroxysmal or essential hypertension[1]. However, PCC has dramatic and fulminant clinical expression and is usually associated with significant mortality. PCC as an endocrine emergency has been defined as the acute severe presentation of catecholamine-induced hemodynamic instability causing end-organ damage or dysfunction, usually associated with significant mortality[2]. However, due to catecholamine overrelease, PCC can mimic other common conditions and thus frequently is initially misdiagnosed[3]. As the clinical manifestations of the present case were featured by hypotension, hemoptysis, dyspnea, and multiple organ dysfunction syndrome on admission, we may easily miss the diagnosis of pheochromocytoma. Many patients choose surgery after the first attack of PCC. In this case, the patient did not undergo surgery; therefore, he had recurrent PCC. The patient’s medical history contributed to our diagnosis. However, hemoptysis, dyspnea, and hypotension were nonspecific signs. Bedside echocardiography helped us rule out heart disease and pulmonary embolism. Due to the widespread actions of catecholamines, pheochromocytomas may present with numerous conditions or diseases. Massive hemoptysis can be the main manifestation[4,5]. Pulmonary venous hypertension secondary to severe paroxysmal hypertension was thought to be a possible cause of hemoptysis[4]. In addition, Kimura et al[6] reported that increased activation of the coagulation cascade and endothelial or platelet stimulation, evidenced by increased plasma von Willebrand factor, may have contributed to hemoptysis. The patient had recurrent PCC five times; the first three had hypertension, but the next two had sustained hypotension. Whitelaw et al[7] suggest that a PCC without sustained hypotension is classified as a type A crisis, whereas a severe presentation with sustained hypotension, shock, and multiorgan dysfunction is classified as a type B crisis. However, the pathological processes of hypotension are not well understood. Norepinephrine and epinephrine are hypothesized to be the primary causes of tumor-induced alterations in hypotension. The primary mechanism seems to be excess plasma epinephrine stimulating β2 receptors to cause vasodilation[8], and norepinephrine is thought to be related to myocardial dysfunction, hypovolemia, and desensitization of baroreflexes[9,10]. In addition, ACTH secretion should increase under stress, but the ACTH and cortisol levels in this case were relatively reduced. We suspect that the reason may be related to ischemia-reperfusion after the severe contraction of pituitary blood vessels caused by pheochromocytoma hormone storm. Such insufficient stress may also be one of the reasons for hypotension. Many reports describe the use of various inotropes and vasopressors (including adrenaline, noradrenaline, dopamine, dobutamine, vasopressin, and levosimendan) to manage sustained hypotension and circulatory compromise[11-13]. We used dopamine for a week. The results of related tests might be affected by the use of this drug. It is unclear if any of these provide significant benefit in the circumstances, but the literature more generally supports the use of vasopressin[14]. The coexistence of pheochromocytoma and AAA poses certain problems, and surgical intervention in these patients carries a significant risk of myocardial infarction, cerebrovascular accident, and cardiovascular collapse. In the preoperative period, there is an increased risk of rupture of the aneurysm, caused by excess catecholamine and hypertension[15]. Also, resecting the pheochromocytoma places the aneurysm at an increased risk of rupture in the postoperative period. Taking these factors into consideration, our patient was subjected to endovascular exclusion of abdominal aortic aneurysm first, and 1 mo later, the patient underwent laparoscopic left adrenal tumor resection. Further studies are needed to determine whether it is possible to repair adrenal tumors and aneurysms at the same time, and the intraoperative management will be a challenging issue.
We report a case of pheochromocytoma presenting with recurrent hemoptysis, dyspnea, and hypotension coexisting with an abdominal aortic aneurysm. It not only proved the uncommon manifestations of pheochromocytoma but also directed clinicians to consider PCC among the possible diagnoses when meeting similar cases. Moreover, surgical excision is the most beneficial method for the treatment of pheochromocytoma coexisting with AAA when the situation is stable.
Manuscript source: Unsolicited manuscript
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shorrab AA S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016;175:G1-G34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1045] [Cited by in RCA: 1018] [Article Influence: 113.1] [Reference Citation Analysis (0)] |
| 2. | Mittendorf EA, Evans DB, Lee JE, Perrier ND. Pheochromocytoma: advances in genetics, diagnosis, localization, and treatment. Hematol Oncol Clin North Am. 2007;21:509-25; ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Lee TW, Lin KH, Chang CJ, Lew WH, Lee TI. Pheochromocytoma mimicking both acute coronary syndrome and sepsis: a case report. Med Princ Pract. 2013;22:405-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Yoshida T, Ishihara H. Pheochromocytoma presenting as massive hemoptysis and acute respiratory failure. Am J Emerg Med 2009; 27: 626.e3-626. e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Frymoyer PA, Anderson GH Jr, Blair DC. Hemoptysis as a presenting symptom of pheochromocytoma. J Clin Hypertens. 1986;2:65-67. [PubMed] |
| 6. | Kimura Y, Ozawa H, Igarashi M, Iwamoto T, Nishiya K, Urano T, Goto S. A pheochromocytoma causing limited coagulopathy with hemoptysis. Tokai J Exp Clin Med. 2005;30:35-39. [PubMed] |
| 7. | Whitelaw BC, Prague JK, Mustafa OG, Schulte KM, Hopkins PA, Gilbert JA, McGregor AM, Aylwin SJ. Phaeochromocytoma [corrected] crisis. Clin Endocrinol (Oxf). 2014;80:13-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 8. | Ueda T, Oka N, Matsumoto A, Miyazaki H, Ohmura H, Kikuchi T, Nakayama M, Kato S, Imaizumi T. Pheochromocytoma presenting as recurrent hypotension and syncope. Intern Med. 2005;44:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | de Leeuw PW, Waltman FL, Birkenhäger WH. Noncardiogenic pulmonary edema as the sole manifestation of pheochromocytoma. Hypertension. 1986;8:810-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Graillon T, Fuentes S, Régis J, Metellus P, Brunel H, Roche PH, Dufour H. Multidisciplinary management of giant functional petrous bone paraganglioma. Acta Neurochir (Wien). 2011;153:85-9; discussion 89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Chao A, Yeh YC, Yen TS, Chen YS. Phaeochromocytoma crisis--a rare indication for extracorporeal membrane oxygenation. Anaesthesia. 2008;63:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Park SM, Kim DH, Kwak YT, Jeong IK, Cho JM, Jin ES, Kim CJ. Pheochromocytoma-induced cardiogenic shock rescued by percutaneous cardiopulmonary bypass system. Circ J. 2009;73:1753-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Westaby S, Shahir A, Sadler G, Flynn F, Ormerod O. Mechanical bridge to recovery in pheochromocytoma myocarditis. Nat Rev Cardiol. 2009;6:482-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin vs norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358:877-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1191] [Cited by in RCA: 1183] [Article Influence: 69.6] [Reference Citation Analysis (0)] |
| 15. | van der Horst-Schrivers AN, Kerstens MN, Wolffenbuttel BH. Preoperative pharmacological management of phaeochromocytoma. Neth J Med. 2006;64:290-295. [PubMed] |